Abstract
Purpose
Vaccination against HPV plays a crucial role in preventing cervical cancer and related health issues. This study aimed to (1) assess knowledge, awareness, intentions, and attitudes regarding HPV and vaccination among Jordanian parents, and (2) evaluate the efficacy of two intervention strategies in promoting knowledge, awareness, and attitudes towards HPV vaccinations.
Methods
In study one, a web-based survey was used to collect data from Jordanian parents. In study two, participants were allocated into three groups: video-based intervention, lecture-based intervention, and a control group. Pre-post tests were conducted to evaluate the efficacy of the intervention strategies in promoting knowledge, awareness, and attitudes toward HPV vaccination among Jordanian parents.
Results
A total of 572 participants took part in the survey. Knowledge levels about HPV and its vaccine were generally low. Intentions regarding HPV vaccination were uncertain for the majority of participants, with 92 % reported as not receiving any guidance from medical professionals about administering the HPV vaccine to themselves or their children. Only 22 % agreed that their children might get infected with HPV at any time in their lives. The pilot randomized clinical trial revealed an improvement in knowledge, awareness, and attitudes towards HPV vaccination in both intervention groups compared to the control group with large effect sizes (eta squared between 0.29 and 0.68).
Conclusions
Findings highlight the need for increased knowledge and awareness regarding HPV and vaccination. It also supported the potential effectiveness of basic educational efforts in significantly improving knowledge, awareness, and attitudes towards the HPV vaccine.
1. Introduction
Human papillomaviruses (HPVs) represent a diverse group of pathogens within the papillomaviruses family, characterized by their non-enveloped, double-stranded circular DNA structure. With over 200 identified types, HPVs exhibit a remarkable affinity for infecting squamous epithelial tissues, including both cutaneous and mucosal surfaces.1,2 HPV stands out as the most prevalent sexually transmissible infection worldwide, significantly impacting individuals' social lives.3 While frequently associated with sexual contact, HPV can also spread through non-sexual means, including skin-to-skin, skin-to-mucosa, or mucosa-to-mucosa contact.4 HPV types are categorized into high-risk and low-risk groups, based on their oncogenic potential.2 Notably, the high-risk genotypes are responsible for nearly 99.7 % of invasive cervical cancers worldwide5 and emerge as the primary risk factor for the subsequent development of nearly all cervical cancers in women.6 In fact, HPV is identifiable in 99.7 percent of cervical cancer cases.7 Additionally, it serves as the predominant cause of and significantly contributes to carcinomas across the anogenital tract in both sexes, and head and neck squamous cell carcinomas.8, 9, 10
Vaccination against HPV plays a crucial role in preventing cervical cancer and other related health issues caused by HPV infection11,12 Crucially, the safety profile of these vaccines is excellent, with no major safety concerns identified. It is important to emphasize that the vaccine achieves its highest effectiveness when administered prior to an individual's initiation of sexual activity, as its primary goal is to provide protection before exposure to HPV.13 Ten to fourteen years old adolescents produce a significantly greater quantity of antibodies after HPV vaccination compared to girls and women aged 18–53 years.14 Further, HPV vaccines generate a much stronger antibody response than what naturally occurs in response to HPV infection.15 Recent studies and reviews have also indicated that administering adjuvant HPV vaccination following the treatment of HPV-related diseases is linked to a decreased risk of recurrence of cervical intraepithelial neoplasia (CIN).16
Suboptimal HPV vaccination rates have been associated with a multitude of determinants, including familial social dynamics, parental knowledge gaps, parental attitudes towards vaccines, safety apprehensions, absence of healthcare provider endorsements, restricted accessibility to preventive healthcare services, and vaccine hesitancy.17,18 According to Ndejjo et al.,19 parental awareness and attitudes regarding HPV vaccines constitute pivotal determinants in the uptake of HPV vaccination among children. Vaccine efficacy depends highly on the degree of acceptability and adoption, factors predominantly contingent upon parental consent for the vaccination of their eligible offspring.
2. Study context
In Jordan, the absence of a national cervical cancer screening program reveals a significant healthcare gap. Annually, 115 women are diagnosed, and 71 die due to cervical cancer, ranking it 11th among Jordanian women and 10th among those aged 15 to 44. In terms of mortality, it stands as the 12th most deadly cancer overall and the 9th for the 15 to 44 age group.20 Over 90 % of cases are attributed to HPV.21 Since 1979, mandatory routine immunization has been established in Jordan, currently encompassing vaccination against 12 diseases: tuberculosis, diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, Haemophilus influenza type b, measles, mumps, rubella, rotavirus, and hepatitis A. Immunization services are universally provided to children, irrespective of their citizenship, through a network comprising approximately 700 comprehensive, primary, and peripheral health centers.22 Jordan's commendable vaccine coverage rate, reaching 95 % in 2021, has significantly contributed to a decline in both mortality rates and incidents of vaccine-preventable diseases.23 Notably, the National Immunization Programme in Jordan does not include the HPV vaccine.
Data is not yet available on the HPV burden in the general population of Jordan. However, in Western Asia, the region Jordan belongs to, about 2.5 % of women in the general population are estimated to harbor cervical HPV-16/18 infection at any given time, and 72.4 % of invasive cervical cancers are attributed to HPV 16 or 18.20 Regarding HPV vaccination profile, only one study looked into this area revealing that among female university students in health schools with previous knowledge of HPV (n = 524), only 19 students reported receiving HPV vaccination (3.63 %).24 This study also found that higher vaccine conspiracy beliefs were significantly correlated with a higher likelihood of HPV vaccine rejection.24 In a comprehensive multicountry study encompassing women from Jordan, Qatar, the United Arab Emirates, and Iraq, a mere 3.0 % (n = 84) of participants reported having received the HPV vaccine.25 The major barriers against receiving or recommending the vaccine in Jordan were inadequate information (68 %) and fear of side effects (46 %).25
The primary objective of our research was to comprehensively investigate the multifaceted aspects of HPV vaccination in Jordan. Our approach comprised two distinct studies: The first study encompassed a survey, exploring existing levels of knowledge, awareness, and attitudes regarding HPV and its vaccination within the Jordanian population and examining differences across demographic levels and participant characteristics. The second study involved a pilot randomized clinical trial, designed to evaluate and compare the effectiveness of two intervention strategies — short informational videos and interactive lectures — in promoting knowledge, awareness, and positive attitudes towards HPV vaccination among Jordanian residents. Our findings hold the potential to offer evidence-based recommendations for healthcare practitioners and policymakers, guiding the formulation of targeted strategies to augment HPV vaccination uptake in Jordan.
3. Methods
3.1. Study one: descriptive survey
A web-based survey collected data on the following domains: 1) knowledge, 2) awareness, 3) intentions, and 4) vaccination attitudes. The survey link was shared with parents through online invitation letters on various social media platforms and free messaging services, such as Facebook, Instagram, and WhatsApp. These communications comprehensively described the study objectives, emphasized voluntary participation, assured confidentiality, provided details on the survey's length, and outlined potential benefits and risks. An online consent form was developed, and returning the questionnaire was considered a tacit form of consent. The study received approval from the Institutional Review Board at the University of Jordan.
The survey included different sections assessing knowledge, awareness, intentions, attitudes towards vaccinations, as well as demographic characteristics: (1) The HPV Knowledge Scale26 includes ten questions aimed at assessing the participants' understanding of HPV infection and vaccination, including the modes of transmission, related diseases, preventive aspects, and the sources of information accessed by the participants. (2) The Awareness Scale27 includes eight statements targeting the participants' awareness and concerns regarding HPV infection and vaccination. Additionally, two items were included to evaluate the influence of medical advice and recommendations from important individuals on the decision to get the HPV vaccine for their children. The Awareness Scale incorporated six Likert 5-level scale statements, enabling participants to express their level of agreement or disagreement (1 = Strongly disagree to 5 = Strongly agree). Two subsequent items were based on a ternary scale (1 = Yes, I was advised to get it, 2 = I was advised not to get it, 0 = No, I have not received any advice about the vaccine). (3) The intention subscale of the Carolina HPV Immunization Attitudes & Beliefs Scale28 includes five items gauging participant willingness and readiness to have their children receive the HPV vaccine within the coming year. These items included considerations of cost and willingness to pay for the vaccine, the potential financial commitment, and the influence of the vaccine's availability free of charge. (4) The General Vaccination Attitudes Scale29 includes fifteen statements that explore the participant attitudes and beliefs regarding vaccination, emphasizing aspects such as safety, effectiveness, trust in public health authorities, and participant individual decision-making processes concerning vaccination. The scale was rated on a 7-level Likert scale across various statements, allowing participants to express their degree of agreement with the provided statements (from 1 = Strongly disagree to 7 = Strongly agree). Assuming that 50 % of participants would have high HPV vaccination knowledge, this assumption, along with a desired 5 % margin of error and 95 % confidence level, resulted in an estimated sample size of 385. The assumed proportion allowed for the largest possible sample size.
3.2. Study two: pilot randomized clinical trial (RCT)
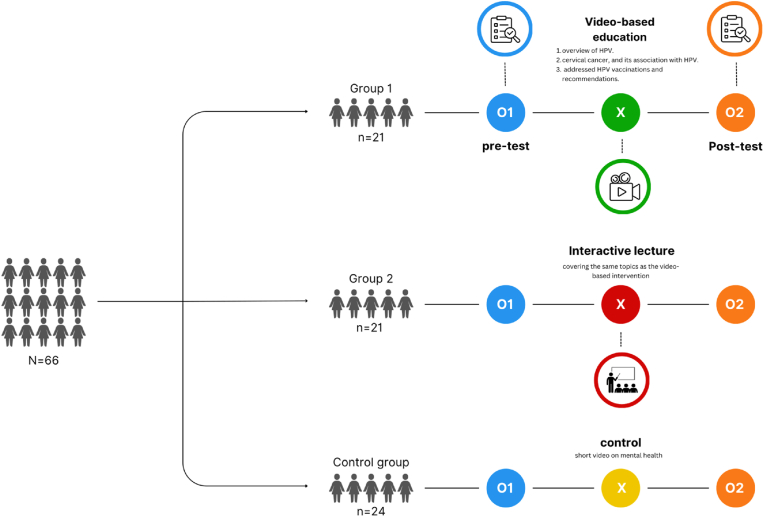
A three-arm pilot RCT was implemented with a total of 66 adult participants, who were randomly assigned to one of three intervention groups: a short-video-based education group (n = 21), a conventional lecture group (n = 21), and a control group (n = 24), as illustrated in Fig. 1. To participate, individuals had to be at least 18 years old and possess basic literacy skills. All intervention sessions were conducted in a uniform setting at a high school located in Amman, the capital city. Participants, primarily parents of high school students, were initially gathered at an open health day event. From 81 attendees, 66 were chosen through a random drawing of lots, thereby guaranteeing an unbiased selection. In alignment with the CONSORT statement, the random allocation of participants to the trial's three arms was performed using a computer-generated list, ensuring a 1:1 allocation ratio. This step was carried out by a research team member who was not involved in data collection. Given the nature of the intervention, it was not feasible to blind participants or the researchers administering the intervention.
Fig. 1.
The pilot ranomized control trial method.
The sample size for this pilot study was calculated using the G*Power statistical program. This calculation was based on an ANOVA: fixed effects, omnibus, one way. Drawing from prior studies26,30 on educational interventions targeting knowledge, attitudes, and practices enhancement, the effect size was estimated to be large. Setting an alpha level at 0.05, a power level of 0.8, and adopting 0.4 as the convention for a large effect size, we determined the required sample size to be 66. This estimation ensured the study was adequately powered to detect significant differences, should they exist, across the different intervention arms.
Regarding the educational content, the first group received a video-based intervention, which consisted of three brief animation videos, each lasting approximately 2 min. The first video provided an overview of HPV, its pathology, and transmission routes. The second one focused on cervical cancer, its incidence, and its association with HPV, while the third one addressed HPV vaccinations and recommendations. The second group received information covering the same topics as the video-based intervention but using traditional lecturing. In the third control group, participants received no interventions, but were instructed to watch a short video on mental health and were required to fill out the same questionnaire administered to the other groups at baseline and after the interventions were completed. Participants underwent a pretest-posttest using the identical set of measures previously outlined in the survey to assess changes in these domains. The research protocol received full review and approval from the institutional review board of the corresponding author's institution, as well as the recruitment setting.
4. Results
4.1. Study one: descriptive survey
4.1.1. HPV knowledge
A total of 572 participants filled out and returned the online survey. Table 1 details all participant characteristics. Among the surveyed participants, 28 % acknowledged familiarity with HPV infection, while 19 % reported being aware of HPV vaccination. When asked about modes of HPV transmission, only 22 % of the respondents were aware that HPV could be transmitted sexually, while direct transmission was recognized by 21 %. Only four responders (0.7 %) demonstrated awareness of all transmission routes, including direct contact, sexual transmission, breastfeeding, and transmission from mother to fetus during pregnancy. Notably, over half of the samples (57.2 %) lacked awareness of any HPV transmission routes. The survey also revealed poor knowledge regarding diseases associated with HPV infection, with almost 61 % of the sample not recognizing any.
Table 1.
Participant characteristics (N = 572).
| Characteristics | n (%) |
|---|---|
| Gender | |
| Male | 147 (25.7 %) |
| Female | 425 (74.3 %) |
| Marital status | |
| Married | 529 (92.5 %) |
| Divorced | 17 (3 %) |
| Widower | 26 (4.5 %) |
| Educational level | |
| Uneducated | 2 (0.3 %) |
| Less than secondary school | 41 (7.2 %) |
| high school | 98 (17.1 %) |
| University education | 431 (75.3 %) |
| Field of study | |
| Health | 63 (11 %) |
| Science | 195 (34.1 %) |
| Humanities | 153 (26.7 %) |
| None | 161 (28.1 %) |
| Number of male children between 9–18 y | |
| 0 | 156 (27.3 %) |
| 1–3 | 377 (65.9 %) |
| >3 | 39 (6.8 %) |
| Number of female children between 9–18 y | |
| 0 | 198 (34.6 %) |
| 1–3 | 349 (61 %) |
| >3 | 25 (4.3 %) |
4.1.2. HPV vaccination knowledge
The survey revealed diverse perceptions regarding HPV vaccination. For the statement "Vaccination is one way to prevent HPV infection," 42 % of respondents correctly identified this as true. However, for the statement "HPV vaccine gives protection from cervical cancer," 26.9 % correctly affirmed this, and 67.3 % were unsure. Regarding the belief that "HPV vaccine can be given to females and males," 32.2 % responded affirmatively and 59.8 % were uncertain. Furthermore, 13.1 % correctly recognized that "HPV vaccine is given to children," while 28.7 % acknowledged "HPV vaccine is given to adolescents," as true. When inquired about primary channels for acquiring information about HPV, responses recorded social media platforms (Facebook, Instagram, Twitter) and electronic media outlets (radio, TV, websites), collectively accounting for 43.2 %. Family and friends constituted 9.6 % and 11.2 %, respectively, as sources of information. A total of 40 respondents (7 %) reported obtaining their information from healthcare workers, while 10 % relied on university faculty for their HPV-related information. We looked into differences in knowledge levels based on participant characteristics. The results revealed that knowledge was significantly contingent upon age with older participants having less knowledge about HPV and its vaccine.
4.1.3. HPV awareness
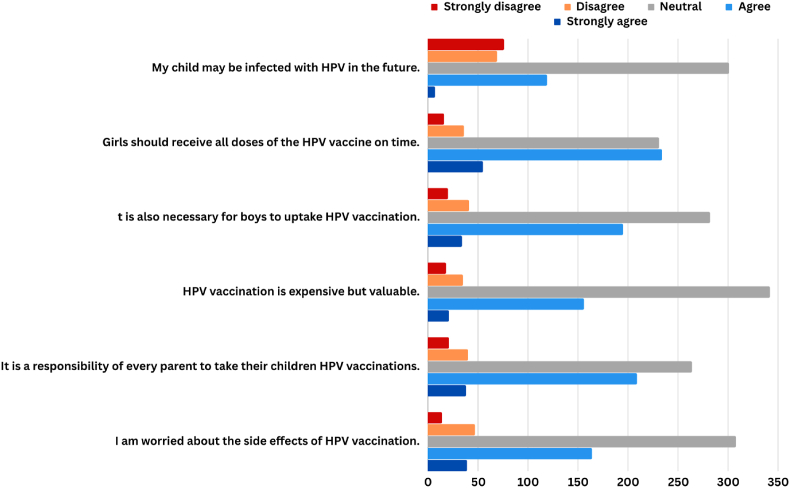
The mean score for the total awareness responses was 19.51 ± 3.28 ranging from 6 to 30. A significant proportion of respondents (92 %) reported not receiving any advice from healthcare professionals regarding administering the HPV vaccine to their children. Only 22 % of the sample agreed with the statement that their children might get infected with HPV at any time of their lives. Notably, 36 % expressed concerns regarding potential side effects of HPV vaccination. Participant characteristics had no impact on their awareness. Fig. 2 displays more responses.
Fig. 2.
HPV awareness among Jordanian parents.
4.1.4. HPV intentions
When asked about their feelings regarding obtaining the HPV vaccine in the next year, 73 % indicated uncertainty, categorizing themselves as "undecided”. A minority, accounting for 13 %, conveyed a negative stance, while 14.3 % expressed a positive inclination. When considering the scenario of personally covering the cost of the HPV vaccine for their children (which costs around 688 USD for three doses), 41.8 % expressed an inclination towards unlikeliness. However, a notable shift in perspective occurred when the cost factor was removed, as 47.9 % of respondents (274 individuals) indicated a likelihood of getting the HPV vaccine for their children.
4.1.5. Vaccination attitudes
Only 25 % of participants disagreed with the statements that vaccines are safe. Regarding trust in public authorities on vaccines, 45.7 % agreed. Notably, about 22 % agreed with the statement that vaccination is unnecessary because vaccine-preventable diseases are not common anymore, while about 41 % agreed that it is unnecessary to get vaccinated when everyone else does, and 23 % agreed that their immune system alone protects them against diseases. Finally, perceiving vaccination as a collective action to prevent disease spread resulted in 10.0 % disagreement, 18.7 % neutrality, and 71.3 % agreement among participants. Table 2 displays the complete responses.
Table 2.
Participant attitudes towards vaccination (N = 572).
| Item | Disagree n (%) | Neutral n (%) | Agree n (%) |
|---|---|---|---|
| I am completely confident that vaccines are safe. | 144 (25.2 %) | 188 (32.9 %) | 240 (41.9 %) |
| Vaccinations are effective | 96 (16.8 %) | 177 (30.9 %) | 299 (52.3 %) |
| Regarding vaccines, I am confident that public authorities decide in the best interest of the community. | 114 (19.9 %) | 197 (34.4 %) | 261 (45.7 %) |
| Vaccination is unnecessary because vaccine-preventable diseases are not common anymore. | 248 (43.4 %) | 199 (34.8 %) | 125 (21.8 %) |
| My immune system is so strong, it also protects me against diseases. | 284 (49.6 %) | 151 (26.4 %) | 137 (23 %) |
| Vaccine-preventable diseases are not so severe that I should get vaccinated. | 334 (58.4 %) | 166 (29 %) | 72 (12.6 %) |
| Everyday stress prevents me from getting vaccinated. | 280 (48.9 %) | 164 (28.7 %) | 128 (22.4 %) |
| For me, it is inconvenient to receive vaccinations | 197 (34.4 %) | 137 (24 %) | 238 (41.6 %) |
| Visiting the doctor's makes me feel uncomfortable; this keeps me from getting vaccinated | 279 (48.8 %) | 127 (22.2 %) | 161 (28 %) |
| When I think about getting vaccinated, I weigh benefits and risks to make the best decision possible. | 51 (8.9 %) | 111 (19.4 %) | 410 (71.7 %) |
| For each and every vaccination, I closely consider whether it is useful for me | 47 (8.2 %) | 106 (18.5 %) | 419 (73.3 %) |
| It is important for me to fully understand the topic of vaccination before I get vaccinated. | 44 (7.7 %) | 92 (16.1 %) | 436 (76.2 %) |
| When everyone is vaccinated, I don't have to get vaccinated, too. | 198 (34.6 %) | 139 (24.3 %) | 235 (41.1 %) |
| I get vaccinated because I can also protect people with a weaker immune system. | 68 (11.9 %) | 136 (23.8 %) | 368 (64.3 %) |
| Vaccination is a collective action to prevent the spread of diseases. | 57 (10 %) | 107 (18.7 %) | 408 (71.3 %) |
4.1.6. Factors affecting vaccination attitudes
Hierarchal multiple regression analysis was used to explore factors that may shape parents' attitudes toward vaccination. The results revealed that the first model (containing parents' characteristics) could not predict parents' attitude scores (F 5, 566 = 0.238, p = .946, R2 = 0.002). This model explained less than 1 % of the variance in the outcome. However, the second model (containing parents’ characteristics as well as their knowledge and awareness regarding HPV) significantly predicted parents' attitudes but was able to explain only 9 % of the variance in this outcome (F 7, 564 = 7.98, p < 0.001, AdjR2 = 0.088). In other words, about 9 % of the variability in parents' attitudes could be explained by their demographic characteristics as well as levels of awareness and attitudes. The individual betas in the second model indicate that parents' attitudes are significantly related to being more aware of the possibility of getting future infections, and the need for a vaccine.
4.2. Study two: pilot RCT
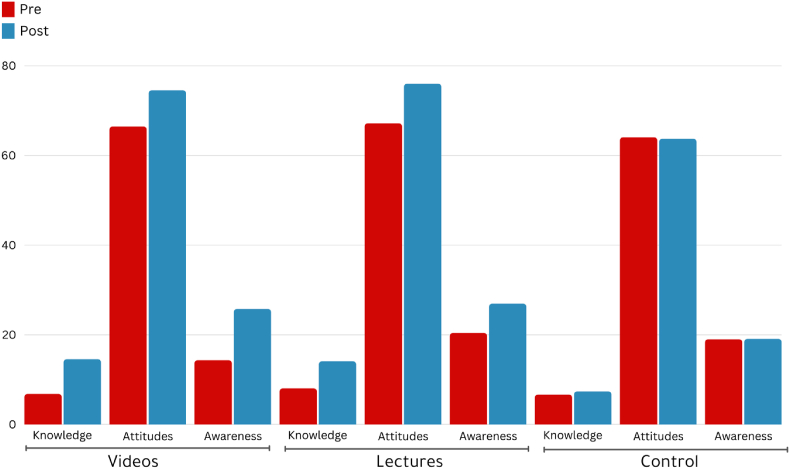
To examine the study primary outcomes, we initially conducted an ANOVA test to compare baseline mean scores of knowledge, awareness, and attitudes between the intervention and control groups. The results revealed no statistically significant differences (all p > 0.05), implying comparable baseline conditions. We then performed ANOVA tests to assess mean differences in the three outcomes following the educational sessions. The analysis disclosed significant differences in knowledge scores (F2,63 = 68.25, p < 0.001), with both the short-video and lecture groups showing significantly better knowledge and awareness and more positive attitudes towards HPV vaccination compared to the control group (all p < 0.001). Eta-squared sores indicated very large effect sizes (Table 3). Fig. 3 shows the post-intervention mean scores of the outcomes.
Table 3.
Between-group differences in knowledge, awareness, and attitudes after the educational sessions.
| ANOVA |
Eta Squared | Scheffe |
|||||
|---|---|---|---|---|---|---|---|
| Outcome | (1) Lecture |
(2) Short-Videos |
(3) Control |
F | Significant comparison | P value | |
| (n = 21) |
(n = 21) |
(n = 24) |
|||||
| M (SD) | M (SD) | M (SD) | |||||
| Knowledge | 14.09 (1.17) | 14.57(0.97) | 7.37(3.64) | 68.25* | 0.684 | 1 vs 3 | <0.001 |
| 2 vs 3 | <0.001 | ||||||
| Awareness | 26.95(2.41) | 25.76 (2.96) | 19.08(3.32) | 47.42* | 0.601 | 1 vs 3 | <0.001 |
| 2 vs 3 | <0.001 | ||||||
| Attitudes | 76.00(10.78) | 74.52(8.65) | 63.70(6.59) | 13.45* | 0.299 | 1 vs 3 | <0.001 |
| 2 vs 3 | <0.001 | ||||||
Fig. 3.
Post-intervention mean scores of knowledge, awareness and attitudes.
5. Discussion
Despite the high level of education reported by the study sample, there was still substantial lack of knowledge about this vaccine The study showed that only a minority of participants demonstrated adequate knowledge about HPV, its transmission routes, associated diseases, and the HPV vaccine. These knowledge gaps were particularly pronounced when it came to understanding the modes of HPV transmission and diseases associated with HPV infection. Findings also highlighted limited awareness of the HPV vaccine with a significant proportion of parents unsure about the vaccine's effectiveness, target population, or its role in preventing cervical cancer. To state the obvious this lack of knowledge and awareness can significantly impact vaccination decisions, as informed choices depend on understanding the benefits and risks associated with vaccines.31,32
Our investigation indicates that the educational attainment of participants does not exert a significant influence on their attitudes regarding HPV vaccination. This might be attributed to the absence of comprehensive public recommendations and policies pertaining to HPV vaccination. Additionally, this observation may signify a discernible lack of interest within the educational framework in Jordan concerning HPV and HPV vaccination.
The low level of knowledge and awareness of the HPV vaccine in this study mirrors trends observed in several Arab countries.33,34 These findings collectively emphasize the urgent need for region-specific awareness campaigns tailored to address information gaps, eliminate misconceptions, and enhance comprehension about the importance of HPV vaccination in preventing cervical cancer. In our study, only 6.3 % of participants received a positive recommendation from a healthcare provider regarding HPV vaccination. This aligns with a study conducted in Qatar, where 4 % of parents reported that their children's primary care physicians had mentioned the HPV vaccine,35 highlighting a significant communication gap between healthcare providers and the public.
Conspiracy theories against vaccines spread unfounded beliefs about their safety and efficacy, often suggesting a sinister plot by governments or pharmaceutical companies. These theories contribute to vaccine hesitancy, leading individuals to refuse vaccination and posing risks to public health.36, 37, 38, 39 This study also examined general vaccination attitudes among Jordanian parents, revealing a mixed perception. In terms of trusting public authorities, only 45.7 % of respondents expressed confidence, and there were concerns about vaccine safety and the necessity of vaccines, highlighting a crucial factor in vaccine decision-making. Studies show that high trust in public health authorities correlates with positive attitudes toward vaccination.
Overall, the current HPV knowledge profile suggests a pressing need for comprehensive educational campaigns and interventions aimed at increasing HPV-related knowledge and awareness and promoting positive attitudes among parents in Jordan. Improving understanding of HPV and its vaccine is essential for making informed decisions about vaccination, which, in turn, can lead to higher vaccination uptake and better public health outcomes. The pilot RCT results informed this recommendation by indicating that educational interventions can significantly enhance knowledge and awareness and promote positive attitudes toward HPV vaccination. In our study, the interventions although brief, did affect changes in knowledge and attitudes. Short video interventions demonstrated efficacy comparable to interactive lectures, emphasizing the potency of dynamic public health strategies. Leveraging reels on platforms like Instagram and TikTok, these visually engaging videos enhance accessibility, rendering health information easily shareable.40,41 The interactive nature of social media facilitates real-time communication, community building, and rapid dissemination of information by health institutions.42 Despite these advantages, challenges like combating misinformation and navigating demographic variances require careful consideration. In essence, integrating reels and social media into public health interventions represents a nimble, influential approach, fostering engagement and efficiently disseminating vital information. However, further research is needed to explore the long-term effects of such interventions and their potential scalability in a broader population.
The cost of the HPV vaccine appeared to be a significant factor influencing parents' intentions, with a substantial shift in willingness to vaccinate when the cost barrier was removed. Ensuring that the vaccine is affordable and accessible to all socioeconomic groups promotes health equity. It means that vaccination decisions are based on medical recommendations and informed choices rather than financial constraints.43,44 Wider vaccine coverage contributes to the prevention of HPV-related cancers, such as cervical cancer, and reduces the associated healthcare costs.45, 46, 47 This, in turn, has a positive impact on public health and healthcare system sustainability.
6. Limitations
One limitation of our study is that we did not question participants about their access to healthcare services, which is a well demonstrated barrier to vaccination.48 Another limitation is the high percentage of college-educated participants, potentially introducing a selection bias. However, Jordan has reported youth and adult literacy rates exceeding 96 %, and similar high levels of internet accessibility, indicating that our sample was reflective of the general population.49,50 Further, the impact and generalizability of the interventions might be limited due to the small sample size used in the study.
7. Conclusions
This study provides valuable insights into the current state of HPV knowledge, attitudes, and intentions among Jordanian parents. By addressing knowledge gaps and misconceptions through targeted educational efforts and improving vaccine accessibility, Jordan can take significant steps towards increasing HPV vaccination rates and reducing the burden of HPV-related diseases. Public health authorities, healthcare providers, and educators should collaborate to implement evidence-based strategies to achieve these goals.
CRediT authorship contribution statement
Ahmad Al-leimon: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. Obada Al-leimon: Conceptualization, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Bayan Abdulhaq: Investigation, Methodology, Writing – original draft, Writing – review & editing. Fadi Al-salieby: Investigation, Methodology, Writing – original draft, Writing – review & editing. Abdul-Raheem Jaber: Investigation, Methodology, Writing – original draft, Writing – review & editing. Mohammed Saadeh: Investigation, Methodology, Writing – original draft, Writing – review & editing. Abdel Rahman Jaber: Investigation, Methodology, Writing – original draft, Writing – review & editing. Omer Aziziye: Methodology, Writing – original draft, Writing – review & editing. Latefa Ali Dardas: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We acknowledge Mohammadnour Amr for his contribution to collecting data for this research.
Contributor Information
Bayan Abdulhaq, Email: bayan.abdulhaq@sit.edu.
Latefa Ali Dardas, Email: L.dardas@ju.edu.jo.
Data availability
Data will be made available on request.
References
- 1.National Institutes of Health . Human Papilloma Virus Database. 2019. Human papilloma virus subtypes. NIH: Bethesda, MA, USA. [Google Scholar]
- 2.Li Y., Xu C. Human papillomavirus-related cancers. Adv Exp Med Biol. 2017;1018:23–34. doi: 10.1007/978-981-10-5765-6_3. [DOI] [PubMed] [Google Scholar]
- 3.Kombe Kombe AJ., Li B., Zahid A., et al. Epidemiology and burden of human papillomavirus and related diseases, molecular pathogenesis, and vaccine evaluation. Front Public Health. 2021;8 doi: 10.3389/fpubh.2020.552028. Published 2021 Jan 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sabeena S., Bhat P., Kamath V., Arunkumar G. Possible non-sexual modes of transmission of human papilloma virus. J Obstet Gynaecol Res. 2017;43(3):429–435. doi: 10.1111/jog.13248. [DOI] [PubMed] [Google Scholar]
- 5.Athanasiou A., Bowden S., Paraskevaidi M., et al. HPV vaccination and cancer prevention. Best Pract Res Clin Obstet Gynaecol. 2020;65:109–124. doi: 10.1016/j.bpobgyn.2020.02.009. [DOI] [PubMed] [Google Scholar]
- 6.Stanley M. Pathology and epidemiology of HPV infection in females. Gynecol Oncol. 2010;117(2 Suppl):S5–S10. doi: 10.1016/j.ygyno.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 7.Walboomers J.M., Jacobs M.V., Manos M.M., et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol. 1999;189(1):12–19. doi: 10.1002/(SICI)1096-9896(199909)189:1<12::AID-PATH431>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 8.Stanley M. HPV vaccination in boys and men. Hum Vaccines Immunother. 2014;10(7):2109–2111. doi: 10.4161/hv.29137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McLaughlin-Drubin M.E. Human papillomaviruses and non-melanoma skin cancer. Semin Oncol. 2015;42(2):284–290. doi: 10.1053/j.seminoncol.2014.12.032. [DOI] [PubMed] [Google Scholar]
- 10.Brianti P., De Flammineis E., Mercuri S.R. Review of HPV-related diseases and cancers. New Microbiol. 2017;40(2):80–85. [PubMed] [Google Scholar]
- 11.Wang R., Pan W., Jin L., et al. Human papillomavirus vaccine against cervical cancer: opportunity and challenge. Cancer Lett. 2020;471:88–102. doi: 10.1016/j.canlet.2019.11.039. [DOI] [PubMed] [Google Scholar]
- 12.Yousefi Z., Aria H., Ghaedrahmati F., et al. An update on human papilloma virus vaccines: history, types, protection, and efficacy. Front Immunol. 2022;12 doi: 10.3389/fimmu.2021.805695. Published 2022 Jan 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization . second ed. World Health Organization; 2014. Comprehensive Cervical Cancer Control: A Guide to Essential Practice.https://apps.who.int/iris/handle/10665/144785 [PubMed] [Google Scholar]
- 14.Nicoli F., Mantelli B., Gallerani E., et al. Effects of the age of vaccination on the humoral responses to a human papillomavirus vaccine. NPJ Vaccines. 2022;7(1):37. doi: 10.1038/s41541-022-00458-0. Published 2022 Mar 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stanley M., Pinto L.A., Trimble C. Human papillomavirus vaccines--immune responses. Vaccine. 2012;30(Suppl 5):F83–F87. doi: 10.1016/j.vaccine.2012.04.106. [DOI] [PubMed] [Google Scholar]
- 16.Di Donato V., Caruso G., Petrillo M., et al. Adjuvant HPV vaccination to prevent recurrent cervical dysplasia after surgical treatment: a meta-analysis. Vaccines (Basel) 2021;9(5):410. doi: 10.3390/vaccines9050410. Published 2021 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holman D.M., Benard V., Roland K.B., Watson M., Liddon N., Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brewer N.T., Gottlieb S.L., Reiter P.L., et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ndejjo R., Mukama T., Musinguzi G., Halage A.A., Ssempebwa J.C., Musoke D. Women's intention to screen and willingness to vaccinate their daughters against cervical cancer - a cross sectional study in eastern Uganda. BMC Publ Health. 2017;17(1):255. doi: 10.1186/s12889-017-4180-4. Published 2017 Mar 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The HPV Information Centre Jordan: human papillomavirus and related cancers, fact sheet 2023. https://hpvcentre.net/statistics/reports/JOR_FS.pdf Available online.
- 21.Centers for Disease Control and Prevention HPV. Cdc. 2019. https://www.cdc.gov/hpv/parents/cancer.html 19.12.23.
- 22.Routine Childhood Immunizations. www.unicef.org. https://www.unicef.org/jordan/stories/routine-childhood-immunizations, (accessed 19.12.23).
- 23.Increase in Routine Childhood Immunization Coverage to over 95%. Ministry of Health/Jordan; 2021. https://moh.gov.jo/Ar/NewsDetails/ 19.12.23. [Google Scholar]
- 24.Sallam M., Al-Mahzoum K., Eid H., et al. Attitude towards HPV vaccination and the intention to get vaccinated among female university students in health schools in Jordan. Vaccines (Basel) 2021;9(12):1432. doi: 10.3390/vaccines9121432. Published 2021 Dec 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alsous M.M., Ali A.A., Al-Azzam S.I., et al. Knowledge and awareness about human papillomavirus infection and its vaccination among women in Arab communities. Sci Rep. 2021;11(1):786. doi: 10.1038/s41598-020-80834-9. Published 2021 Jan 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sitaresmi M.N., Rozanti N.M., Simangunsong L.B., Wahab A. Improvement of Parent’s awareness, knowledge, perception, and acceptability of human papillomavirus vaccination after a structured-educational intervention. BMC Publ Health. 2020;20(1):1836. doi: 10.1186/s12889-020-09962-1. Published 2020 Dec 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou M., Qu S., Zhao L., Campy K.S., Wang S. Parental perceptions of human papillomavirus vaccination in central China: the moderating role of socioeconomic factors. Hum Vaccines Immunother. 2019;15(7-8):1688–1696. doi: 10.1080/21645515.2018.1547605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McRee A.L., Brewer N.T., Reiter P.L., Gottlieb S.L., Smith J.S. The Carolina HPV Immunization Attitudes and Beliefs Scale (CHIAS): scale development and associations with intentions to vaccinate. Sex Transm Dis. 2010;37(4):234–239. doi: 10.1097/OLQ.0b013e3181c37e15. [DOI] [PubMed] [Google Scholar]
- 29.Betsch C., Schmid P., Heinemeier D., Korn L., Holtmann C., Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0208601. Published 2018 Dec 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dixon B.E., Zimet G.D., Xiao S., et al. An educational intervention to improve HPV vaccination: a cluster randomized trial. Pediatrics. 2019;143(1) doi: 10.1542/peds.2018-1457. [DOI] [PubMed] [Google Scholar]
- 31.Romijnders K.A.G.J., van Seventer S.L., Scheltema M., van Osch L., de Vries H., Mollema L. A deliberate choice? Exploring factors related to informed decision-making about childhood vaccination among acceptors, refusers, and partial acceptors. Vaccine. 2019;37(37):5637–5644. doi: 10.1016/j.vaccine.2019.07.060. [DOI] [PubMed] [Google Scholar]
- 32.Patty N.J.S., van Dijk H.M., Wallenburg I., et al. To vaccinate or not to vaccinate? Perspectives on HPV vaccination among girls, boys, and parents in The Netherlands: a Q-methodological study. BMC Publ Health. 2017;17(1):872. doi: 10.1186/s12889-017-4879-2. Published 2017 Nov 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alsaad M.A., Shamsuddin K., Fadzil F. Knowledge towards HPV infection and HPV vaccines among Syrian mothers. Asian Pac J Cancer Prev. 2012;13(3):879–883. doi: 10.7314/apjcp.2012.13.3.879. [DOI] [PubMed] [Google Scholar]
- 34.Alhusayn K.O., Alkhenizan A., Abdulkarim A., Sultana H., Alsulaiman T., Alendijani Y. Attitude and hesitancy of human papillomavirus vaccine among Saudi parents. J Family Med Prim Care. 2022;11(6):2909–2916. doi: 10.4103/jfmpc.jfmpc_2377_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hendaus M.A., Hassan M., Alsulaiti M., et al. Parents attitudes toward the human papilloma virus (HPV) vaccine: a new concept in the State of Qatar. J Family Med Prim Care. 2021;10(7):2488–2493. doi: 10.4103/jfmpc.jfmpc_1122_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al Alawi S., Al Zaabi O., Heffernan M.E., et al. Knowledge, attitudes and acceptance toward Human papillomavirus (HPV) vaccination: perspectives of Muslim women and men. Vaccine. 2023;41(13):2224–2233. doi: 10.1016/j.vaccine.2023.02.063. [DOI] [PubMed] [Google Scholar]
- 37.Pertwee E., Simas C., Larson H.J. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28(3):456–459. doi: 10.1038/s41591-022-01728-z. [DOI] [PubMed] [Google Scholar]
- 38.Larson H.J., Clarke R.M., Jarrett C., et al. Measuring trust in vaccination: a systematic review. Hum Vaccines Immunother. 2018;14(7):1599–1609. doi: 10.1080/21645515.2018.1459252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ullah I., Khan K.S., Tahir M.J., Ahmed A., Harapan H. Myths and conspiracy theories on vaccines and COVID-19: potential effect on global vaccine refusals. Vacunas. 2021;22(2):93–97. doi: 10.1016/j.vacun.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wojtara M.S. Use of social media for patient education in dermatology: narrative review. JMIR Dermatol. 2023;6 doi: 10.2196/42609. Published 2023 Apr 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thang C.J., Garate D., Thang J., Lipoff J.B., Barbieri J.S. Short-form medical media: a multi-platform analysis of acne treatment information in TikTok videos, Instagram reels, and YouTube shorts. JMIR Dermatol. 2023;6 doi: 10.2196/48140. Published 2023 Aug 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen J., Wang Y. Social media use for health purposes: systematic review. J Med Internet Res. 2021;23(5) doi: 10.2196/17917. Published 2021 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Radisic G., Chapman J., Flight I., Wilson C. Factors associated with parents' attitudes to the HPV vaccination of their adolescent sons : a systematic review. Prev Med. 2017;95:26–37. doi: 10.1016/j.ypmed.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 44.Zhu L., Zhai S., Siu P.T., et al. Factors related to Chinese parents' HPV vaccination intention for children. Am J Health Behav. 2019;43(5):994–1005. doi: 10.5993/AJHB.43.5.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rees C.P., Brhlikova P., Pollock A.M. Will HPV vaccination prevent cervical cancer? J R Soc Med. 2020;113(2):64–78. doi: 10.1177/0141076819899308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brisson M., Kim J.J., Canfell K., et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395(10224):575–590. doi: 10.1016/S0140-6736(20)30068-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lei J., Ploner A., Elfström K.M., et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383(14):1340–1348. doi: 10.1056/NEJMoa1917338. [DOI] [PubMed] [Google Scholar]
- 48.Newman P.A., Dinh D.A., Nyoni T., et al. Covid-19 vaccine hesitancy and under-vaccination among marginalized populations in the United States and Canada: a scoping review. J Racial Ethn Health Disparities. 2023 Dec;20 doi: 10.1007/s40615-023-01882-1. Epub ahead of print. PMID: 38117443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nusair L., Palmer R. Weak foundations in Arabic literacy: drivers of learning poverty in Jordan. Int J Educ Dev. 2023;99 10.1016/j.ijedudev.2023.102774 [Google Scholar]
- 50.Department of Statistics and ICF Jordan population and family and health survey 2017–18. Amman, Jordan, and Rockville, Maryland, USA: DOS and ICF. 2019. https://www.dhsprogram.com/pubs/pdf/FR346/FR346.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.