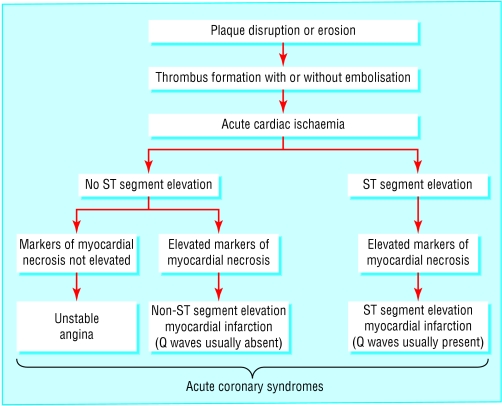
The term acute coronary syndrome refers to a range of acute myocardial ischaemic states. It encompasses unstable angina, non-ST segment elevation myocardial infarction (ST segment elevation generally absent), and ST segment elevation infarction (persistent ST segment elevation usually present). This article will focus on the role of percutaneous coronary intervention in the management of unstable angina and non-ST segment elevation myocardial infarction; the next article will address the role of percutaneous intervention in ST segment elevation infarction.
Although there is no universally accepted definition of unstable angina, it has been described as a clinical syndrome between stable angina and acute myocardial infarction. This broad definition encompasses many patients presenting with varying histories and reflects the complex pathophysiological mechanisms operating at different times and with different outcomes. Three main presentations have been described—angina at rest, new onset angina, and increasing angina.
Figure 1.
Spectrum of acute coronary syndromes according to electrocardiographic and biochemical markers of myocardial necrosis (troponin T, troponin I, and creatine kinase MB), in patients presenting with acute cardiac chest pain
Pathogenesis
The process central to the initiation of an acute coronary syndrome is disruption of an atheromatous plaque. Fissuring or rupture of these plaques—and consequent exposure of core constituents such as lipid, smooth muscle, and foam cells—leads to the local generation of thrombin and deposition of fibrin. This in turn promotes platelet aggregation and adhesion and the formation of intracoronary thrombus.
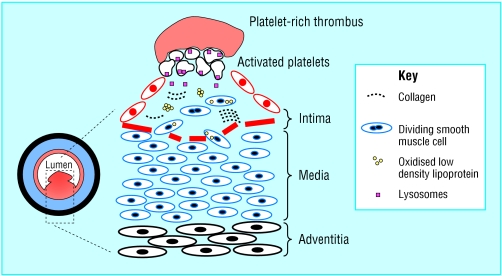
Figure 2.
Diagram of an unstable plaque with superimposed luminal thrombus
Unstable angina and non-ST segment elevation myocardial infarction are generally associated with white, platelet-rich, and only partially occlusive thrombus. Microthrombi can detach and embolise downstream, causing myocardial ischaemia and infarction. In contrast, ST segment elevation (or Q wave) myocardial infarction has red, fibrin-rich, and more stable occlusive thrombus.
Figure 3.
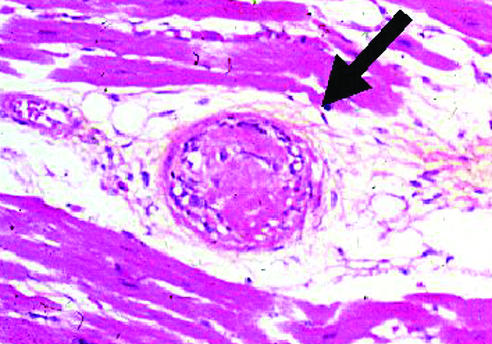
Distal embolisation of a platelet-rich thrombus causing occlusion of intramyocardial arteriole (arrow). Such an event may result in micro-infarction and elevation of markers of myocardial necrosis
Epidemiology
Unstable angina and non-ST segment elevation myocardial infarction account for about 2.5 million hospital admissions worldwide and are a major cause of mortality and morbidity in Western countries. The prognosis is substantially worse than for chronic stable angina. In-hospital death and re-infarction affect 5-10%. Despite optimal treatment with anti-ischaemic and antithrombotic drugs, death and recurrent myocardial infarction occur in another 5-10% of patients in the month after an acute episode. Several studies indicate that these patients may have a higher long term risk of death and myocardial infarction than do patients with ST segment elevation.
Table 1.
Three main presentations of unstable angina
| • Angina at rest—Also prolonged, usually > 20 minutes |
| • Angina of new onset—At least CCS class III in severity |
| • Angina increasing—Previously diagnosed angina that has become more frequent, longer in duration, or lower in threshold (change in severity by ≥ 1 CCS class to at least CCS class III) |
| CCS=Canadian Cardiovascular Society |
Diagnosis
Unstable angina and non-ST segment elevation myocardial infarction are closely related conditions with clinical presentations that may be indistinguishable. Their distinction depends on whether the ischaemia is severe enough to cause myocardial damage and the release of detectable quantities of markers of myocyte necrosis. Cardiac troponin I and T are the preferred markers as they are more specific and reliable than creatine kinase or its isoenzyme creatine kinase MB.
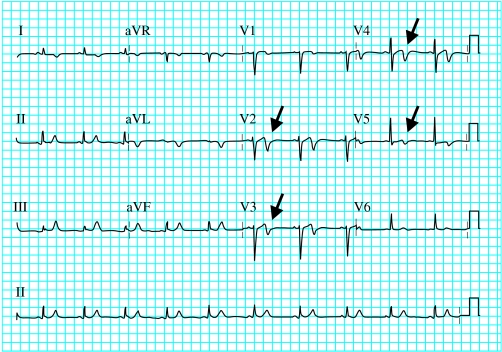
Figure 4.


Electrocardiogram of a 48 year old woman with unstable angina (top). Note the acute ischaemic changes in leads V1 to V5 (arrows). Coronary angiography revealed a severe mid-left anterior descending coronary artery stenosis (arrow, bottom left), which was successfully stented (bottom right)
An electrocardiogram may be normal or show minor non-specific changes, ST segment depression, T wave inversion, bundle branch block, or transient ST segment elevation that resolves spontaneously or after nitrate is given. Physical examination may exclude important differential diagnoses such as pleuritis, pericarditis, or pneumothorax, as well as revealing evidence of ventricular failure and haemodynamic instability.
Management
Management has evolved considerably over the past decade. As platelet aggregation and thrombus formation play a key role in acute coronary syndrome, recent advances in treatment (such as the glycoprotein IIb/IIIa inhibitors, low molecular weight heparin, and clopidogrel) and the safer and more widespread use of percutaneous coronary intervention have raised questions about optimal management.
As patients with unstable angina or non-ST segment elevation myocardial infarction represent a heterogeneous group with a wide spectrum of clinical outcomes, tailoring treatment to match risk not only ensures that patients who will benefit the most receive appropriate treatment, but also avoids potentially hazardous treatment in those with a good prognosis. Therefore, an accurate diagnosis and estimation of the risk of adverse outcome are prerequisites to selecting the most appropriate treatment. This should begin in the emergency department and continue throughout the hospital admission. Ideally, all patients should be assessed by a cardiologist on the day of presentation.
Figure 7.

Right coronary artery angiogram in patient with non-ST segment elevation myocardial infarction (top left), showing hazy appearance of intraluminal thrombus overlying a severe stenosis (arrow). Abciximab was given before direct stenting (top right), with good angiographic outcome (bottom)
Medical treatment
Medical treatment includes bed rest, oxygen, opiate analgesics to relieve pain, and anti-ischaemic and antithrombotic drugs. These should be started at once on admission and continued in those with probable or confirmed unstable angina or non-ST segment elevation myocardial infarction. Anti-ischaemic drugs include intravenous, oral, or buccal nitroglycerin, β blockers, and calcium antagonists. Antithrombotic drugs include aspirin, clopidogrel, intravenous unfractionated heparin or low molecular weight heparin, and glycoprotein IIb/IIIa inhibitors.
Conservative versus early invasive strategy
“Conservative” treatment involves intensive medical management, followed by risk stratification by non-invasive means (usually by stress testing) to identify patients who may need coronary angiography. This approach is based on the results of two randomised trials (TIMI IIIB and VANQWISH), which showed no improvement in outcome when an “early invasive” strategy was used routinely, compared with a selective approach.
These findings generated much controversy and have been superseded by more recent randomised trials (FRISC II, TACTICS-TIMI 18, and RITA 3), which have taken advantage of the benefits of glycoprotein IIb/IIIa inhibitors and stents. All three studies showed that an early invasive strategy (percutaneous coronary intervention or coronary artery bypass surgery) produced a better outcome than non-invasive management. TACTICS-TIMI 18 also showed that the benefit of early invasive treatment was greatest in higher risk patients with raised plasma concentrations of troponin T, whereas the outcomes for lower risk patients were similar with early invasive and non-invasive management.
Table 2.
Names of trials
| • TIMI IIIB—Thrombolysis in myocardial infraction IIIB |
| • VANQWISH—Veterans affairs non-Q-wave infraction strategies in hospital |
| • GUSTO IV ACS—Global use of strategies to open occluded arteries-IV in acute coronary syndromes |
| • RITA 3—Randomised intervention treatment of angina |
| • FRISC II—Fast revascularisation during instability in coronary artery disease |
| • TACTICS-TIMI 18—Treat angina with Aggrastat and determine cost of therapy with an invasive or conservative strategy-thrombolysis in myocardial infraction |
Identifying higher risk patients
Identifying patients at higher risk of death, myocardial infarction, and recurrent ischaemia allows aggressive antithrombotic treatment and early coronary angiography to be targeted to those who will benefit. The initial diagnosis is made on the basis of a patient's history, electrocardiography, and the presence of elevated plasma concentrations of biochemical markers. The same information is used to assess the risk of an adverse outcome. It should be emphasised that risk assessment is a continuous process.
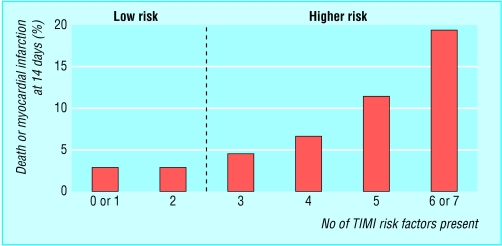
Figure 10.
Rates of death from all causes and non-fatal myocardial infarction at 14 days, by TIMI risk score. Note sharp rate increase when score ≥ 3
The TIMI risk score
Attempts have been made to formulate clinical factors into a user friendly model. Notably, Antman and colleagues identified seven independent prognostic risk factors for early death and myocardial infarction. Assigning a value of 1 for each risk factor present provides a simple scoring system for estimating risk, the TIMI risk score. It has the advantage of being easy to calculate and has broad applicability in the early assessment of patients.
Figure 11.
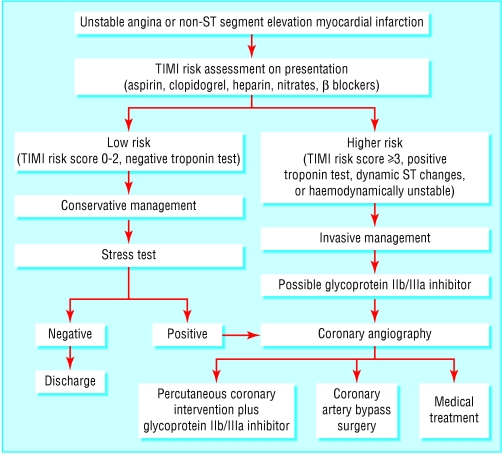
Simplified management pathway for patients with unstable angina or non-ST segment elevation myocardial infarction
Applying this score to the results in the TACTICS-TIMI 18 study indicated that patients with a TIMI risk score of ≥3 benefited significantly from an early invasive strategy, whereas those with a score of ≤2 did not. Therefore, those with an initial TIMI score of ≥3 should be considered for early angiography (ideally within 24 hours), with a view to revascularisation by percutaneous intervention or bypass surgery. In addition, any patient with an elevated plasma concentration of troponin marker, ST segment changes, or haemodynamic instability should also undergo early angiography.
Table 3.
The seven variables for the TIMI risk score
| • Age ≥65 years |
| • ≥3 risk factors for coronary artery disease |
| • ≥50% coronary stenosis on angiography |
| • ST segment change >0.5 mm |
| • ≥2 anginal episodes in 24 hours before presentation |
| • Elevated serum concentration of cardiac markers |
| • Use of aspirin in 7 days before presentation |
Conclusion
The diagnosis of unstable angina or non-ST segment elevation myocardial infarction demands urgent hospital admission and coronary monitoring. A clinical history and examination, 12 lead electrocardiography, and measurement of troponin concentration are the essential diagnostic tools. Bed rest, aspirin, clopidogrel, heparin, antianginal drugs, and opiate analgesics are the mainstay of initial treatment.
Early risk stratification will help identify high risk patients, who may require early treatment with glycoprotein IIb/IIIa inhibitors, angiography, and coronary revascularisation. Those deemed suitable for percutaneous intervention should receive a glycoprotein IIb/IIIa inhibitor and stenting as appropriate. There seems to be little merit in prolonged stabilisation of patients before percutaneous intervention, and an early invasive strategy is generally preferable to a conservative one except for patients at low risk of further cardiac events. This approach will shorten hospital stays, improve acute and long term outcomes, and reduce the need for subsequent intervention.
In the longer term, aggressive modification of risk factors is warranted. Smoking should be strongly discouraged, and statins should be used to lower blood lipid levels. Long term treatment with aspirin, clopidogrel (especially after stenting), β blockers, angiotensin converting enzyme inhibitors, and antihypertensive drugs should also be considered. Anti-ischaemic drugs may be stopped when ischaemia provocation tests are negative.
The ABC of interventional cardiology is edited by Ever D Grech and will be published as a book in summer 2003.
The picture of a microthrombus occluding an intramyocardial arteriole was provided by K MacDonald, consultant histopathologist, St Boniface Hospital, Winnipeg.
Competing interests: None declared.
Further reading
- •.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol 2002;40: 1366-74 [DOI] [PubMed] [Google Scholar]
- •.Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW, McFadden E, et al. Management of acute coronary syndromes: acute coronary syndromes without persistent ST segment elevation. Recommendations of the Task Force of the European Society of Cardiology. Eur Heart J 2000;21: 1406-32 [DOI] [PubMed] [Google Scholar]
- •.Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, et al. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA 2000;284: 835-42 [DOI] [PubMed] [Google Scholar]
- •.Ramsdale DR, Grech ED. Percutaneous coronary intervention unstable angina and non-Q-wave myocardial infarction. In: Grech ED, Ramsdale DR, eds. Practical interventional cardiology. 2nd ed. London: Martin Dunitz, 2002: 165-87