Abstract
Introduction
Blood lactate is a marker of tissue hypoxia while capillary refill time (CRT) is a surrogate of tissue perfusion. Measuring these parameters is recommended for assessing circulatory status and guiding resuscitation. However, blood lactate is not widely available in African emergency departments. Additionally, CRT assessment faces challenges related to its precision and reproducibility. This study aims to evaluate the accuracy of visual CRT(V-CRT) compared to plethysmographic CRT (P-CRT) in predicting lactate levels among septic patients.
Methods
This prospective observational study enrolled consecutive patients with sepsis or septic shock over a 6-month period from a tertiary hospital in Marrakech, Morroco. V-CRT and P-CRT were evaluated upon admission, and simultaneous measurements of arterial lactate levels were obtained. The precision of V-CRT and P-CRT in predicting arterial lactate was assessed using ROC curve analysis.
Results
Forty-three patients aged of 64±15 years, of whom 70 % were male, were included in the study. Of these, 23 patients (53 %) had sepsis, and 20 patients (47 %) experienced septic shock. Both V-CRT and P-CRT demonstrated statistically significant correlations with arterial lactate, with correlation coefficients of 0.529 (p < 0.0001) and 0.517 (p = 0.001), respectively. ROC curve analysis revealed that V-CRT exhibited satisfactory accuracy in predicting arterial lactate levels >2 mmol/l, with an area under the curve (AUC) of 0.8 (95 % CI=0.65 – 0.93; p < 0.0001). The prediction ability of P-CRT was lower than V-CRT with an AUC of 0.73 (95 % CI: 0.57–0.89; p = 0.043). The optimal thresholds were determined as 3.4 s for V-CRT (sensitivity = 90 %, specificity = 58 %) and 4.1 s for P-CRT (sensitivity = 85 %, specificity = 62 %).
Conclusion
These findings suggest that the plethysmographic evaluation did not improve the accuracy of CRT for predicting lactate level. However, V-CRT may still serve as a viable surrogate for lactate in septic patients in low-income settings.
Keywords: Sepsis, Septic shock, Plethysmography, Capillary refill time, Lactate, Low-income setting
African relevance
▒
-
-
Lactate measurement is crucial for managing sepsis and septic shock, yet its availability in African emergency and intensive care departments is limited.
-
-
Capillary refill time (CRT) is a cost-effective, non-invasive marker of tissue perfusion that correlates with lactate levels. Some studies suggest using the plethysmographic curve to measure CRT for accurate lactate prediction.
-
-
This comparative study found that integrating the plethysmographic signal to assess CRT was not superior to the classical visual assessment in African septic patients, indicating limited relevance of investing in such devices in low-resource settings.
▒
Introduction
Lactate is a biological marker of tissue hypoxia and anaerobic metabolism [1,2]. Its measurement is recommended for both septic shock diagnosis and resuscitation guidance [3,4]. The Surviving Sepsis Campaign has recommended using serum lactate to screen for the presence of sepsis [3]. Serum lactate is associated with mortality, and reducing lactate levels is a resuscitation target [2,3]. However, its measurement requires invasive sampling and is not widely available in African emergency and intensive care units. A survey assessing the availability of resources for treating septic patients in Africa revealed that less than a quarter of physicians had access to serum lactate measurement [5].
In contrast, capillary refill time (CRT),1 a clinical marker of tissue perfusion, offers a non-invasive, cost-free alternative and is easily executed [6]. Prolonged CRT has been associated with increased morbidity and mortality in septic patients, and CRT-targeted resuscitation could be associated with improved outcomes [[6], [7], [8]]. Nevertheless, the traditional visual assessment of CRT introduces a certain level of subjectivity. Plethysmographic CRT, which utilizes the plethysmographic curve for measurement, could offer a more objective approach [9,10]. We hypothesized that integrating a simple plethysmographic evaluation could enhance the precision and objectivity of capillary CRT measurement. Thus, this study aims to compare the predictive accuracy of visual CRT (V-CRT) versus plethysmographic CRT (P-CRT) in estimating arterial lactate levels in septic patients.
Methods
This prospective observational single-center study was conducted in the Department of Emergency and Intensive Care Medicine (ICU) of Avicenna Military Hospital, Marrakech, Morocco. After approval by the Hospital ethical committee, written informed consent was obtained from patients or relatives.
During a 9-month period, adult patients consecutively admitted with suspicion of sepsis or septic shock, defined according to sepsis-3 criteria, were included [4]. Patients were excluded if they had an elevated lactate unrelated to sepsis due to factors such as epinephrine infusion, prolonged propofol infusion, seizures, acute regional ischemia, or if they were diabetic patients on metformin. Patients were also excluded if the plethysmographic signal from the pulse oximetry was absent (e.g., due to severe vasoconstriction or hypothermia).
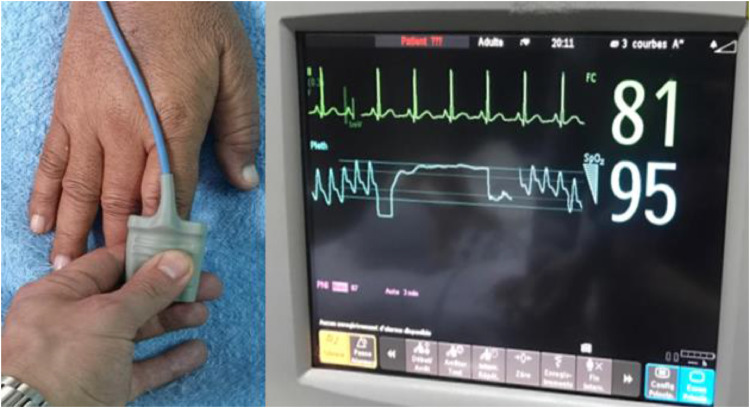
V-CRT and P-CRT were assessed during the first 6 h of ICU admission by a trained physician. V-CRT was measured by applying firm pressure for 10 s to the distal phalanx of one of the patient's three fingers: the index, middle, or ring finger [7]. The pressure applied was the minimum required to cause blanching of the physician's nail. The time taken for the normal color to return to the ventral surface of the patient's phalanx was recorded using a phone chronometer. P-CRT was determined using the plethysmographic curve of a pulse oximeter. Firm pressure was applied for 10 s to the distal phalanx, which was covered with a pulse oximeter sensor. The pressure applied was sufficient to cause the plethysmographic signal to disappear. The time taken for the plethysmographic signal to return to baseline corresponded to the P-CRT (Fig. 1). Blood gas analysis and lactate measurement were conducted using a point-of-care device. These measurements were performed immediately after CRT assessment to ensure that the physician assessing CRT was unaware of the lactate levels. Data collection included demographic characteristics, hemodynamic and perfusion characteristics, and biological data.
Fig. 1.
Measurement of plethysmographic capillary refill time.
Statistical analysis
Categorical variables were presented as numbers (percentages) and continuous variables were expressed as median (interquartile range). Between-group comparisons of continuous variables were performed using the Mann–Whitney test. Correlations were evaluated using Spearman's correlation coefficients. Receiver operating characteristic (ROC) curves, along with 95 % confidence intervals (CI), were constructed to assess the predictive ability of V-CRT and P-CRT for arterial lactate levels > 2 mmol/l. The areas under the ROC curves were compared using the DeLong test. The threshold value that maximized the Youden index (sensitivity + specificity - 1) was selected as the optimal cutoff.
Results
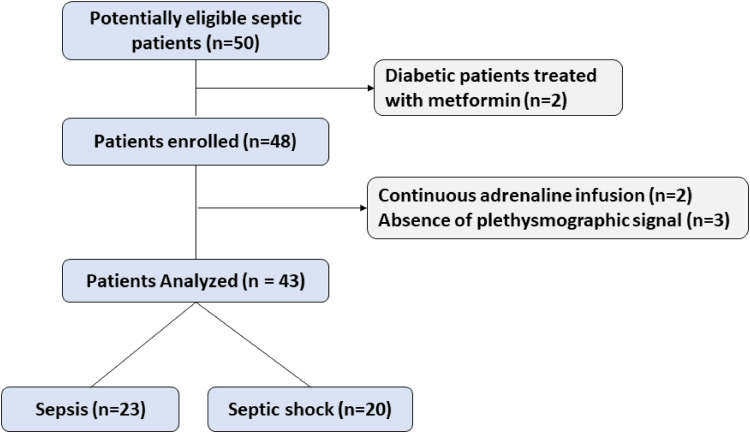
During the study period, 50 patients diagnosed with sepsis or septic shock were approached (Fig. 2). Seven patients were excluded from the study: two were taking metformin treatment, two were receiving continuous epinephrine infusion, and in three patients, a plethysmographic signal could not be recorded. Consequently, a total of 43 patients met the inclusion criteria, comprising 23 patients (53 %) with sepsis and 20 patients (47 %) with septic shock.
Fig. 2.
Flow chart of the study.
The demographic characteristics, biological, and hemodynamic variables are presented in Table 1. The median age of the patients was 65 years (range 59–73), and 30 % were female. The most prevalent comorbidities included diabetes and chronic arterial hypertension. The primary sources of sepsis were pneumonia, followed by abdominal and urinary tract infections.
Table 1.
Demographic characteristics, biological, and hemodynamic variables.
| Age (years) | 65 (59 - 73) |
| female / male | 13 (30 %) / 30 (70 %) |
| SAPS II | 41 (27 - 52) |
| SOFA | 5 (2 - 7) |
| Comorbidities | |
| Diabetes | 14 (33 %) |
| Arterial hypertension | 13 (30 %) |
| Chronic kidney disease | 8 (18 %) |
| Chronic respiratory disease | 8 (18 %) |
| Heart failure | 6 (14 %) |
| Source of sepsis | |
| Pneumonia | 25 (58 %) |
| Intra-abdominal infection | 7 (16 %) |
| Urinary tract infection | 3 (7 %) |
| Neuro-meningeal infections | 3 (7 %) |
| Other sources | 5 (11 %) |
| Biological data | |
| pH | 7.37 (7.3 – 7.42) |
| HCO3- (mmol/l) | 22 (15.7 – 27.3) |
| PaCO2 (mmHg) | 37 (26 −49) |
| PaO2 / FiO2 (mmHg) | 276 (221 – 335) |
| Hemoglobin (g/dl) | 127 (106 – 148) |
| Leucocytes (103/mm3) | 12.6 (8.8 – 1.7) |
| Neutrophiles (103/mm3) | 10 (5.9 – 1.4) |
| Lymphocytes (103/mm3) | 1.2 (0.6 – 1.7) |
| Platelets (103/mm3) | 238 (148 – 294) |
| Creatinine (µmol/l) | 141 (86 – 320) |
| Bilirubin (mmol/l) | 9 (7 −17) |
| International Normalized Ratio | 1.25 (1.13 – 1.29) |
| C-Reactive Protein (mg/l) | 230 (89 – 379) |
| Procalcitonin (ng/l) | 2.6 (0.7 – 28) |
| Arterial Lactates (mmol/l) | 2.3 (1.5 – 3.3) |
| Hemodynamic and perfusion data | |
| Heart rate (bpm) | 116 (97 – 132) |
| Systolic arterial blood pressure (mmHg) | 118 (100 – 140) |
| Diastolic arterial blood pressure (mmHg) | 69 (56 −81) |
| Mean arterial blood pressure (mmHg) | 87 (71 – 99) |
| Visual capillary refill time (seconds) | 4.1 (2.9 – 5.3) |
| Plethysmographic capillary refill time (seconds) | 4.7 (3.2 −5.9) |
Categorical variables as numbers (percentages), continuous variables are expressed as median (interquartile range), SOFA: Sequential Organ Failure Assessment, SAPS II: Simplified Acute Physiology Score II.
The median SOFA score was 5 (2 - 7). Twenty-four patients (56 %) exhibited a PaO2 / FiO2 ratio under 300 mmHg. Patients with hypoxemia received oxygen supplementation. None of the patients required mechanical ventilation at the time of the study. Twenty-eight (65 %) patients were categorized as having acute kidney injury according to the KDIGO classification. The median plasma creatinine level was 141 µmol/l (range 86–320). Acidemia (pH < 7.38) was found in 21 patients (49 %), with metabolic acidosis in 22 patients (51 %). Twenty-eight patients had arterial lactate levels >2 mmol/l. The median arterial lactate was 2.3 (1.5 – 3.3) mmol/l. The visual and plethysmographic CRT were, respectively, 4.1 (2.9 – 5.3) and 4.7 (3.2 −5.9) seconds.
Both V-CRT and P-CRT were significantly prolonged in patients with arterial lactate levels >2 mmol/l. The V-CRT was 3.3 s (2.1–4.3) in patients with lactate levels <2 mmol/l and 5.1 s (3.6–6.2) in patients with lactate levels >2 mmol/l (p = 0.001). Similarly, the P-CRT was 3.9 s (2.8–5.3) in patients with lactate levels <2 mmol/l and 5.2 s (4.6–6.5) in patients with lactate levels >2 mmol/l (p = 0.011). Moreover, both V-CRT and P-CRT demonstrated statistically significant correlations with arterial lactate levels. The correlation coefficient for V-CRT was rho=0.53 (95 % CI: 0.24 to 0.73; p < 0.001), and for P-CRT, it was rho=0.52 (95 % CI: 0.23 to 0.72; p = 0.001).
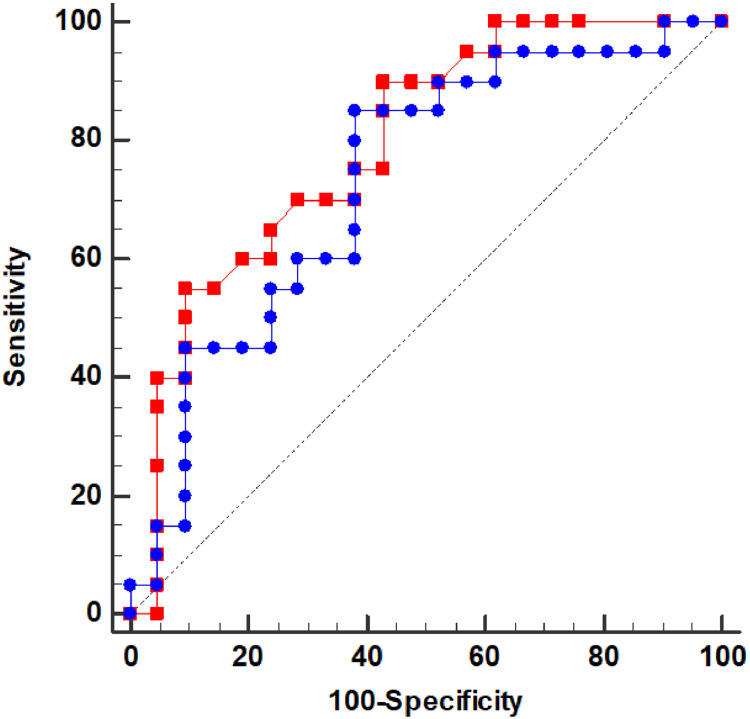
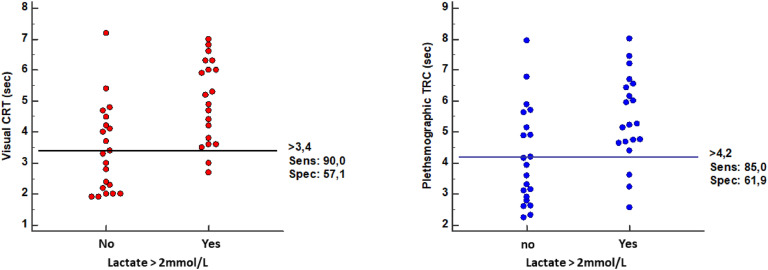
The ROC curve analysis (Fig. 3) revealed that V-CRT exhibited acceptable accuracy in predicting arterial lactate levels >2 mmol/l, with an area under the curve (AUC) of 0.8 (95 % CI=0.65–0.93; p < 0.001). In comparison, P-CRT showed a lower predictive accuracy: 0.73 (95 % CI: 0.57–0.89; p = 0.043). However, the difference in predictive accuracy between V-CRT and P-CRT was not statistically significant (p = 0.21). The optimal thresholds (Fig. 4) were determined as 3.4 s for V-CRT (sensitivity = 90 %, specificity = 58 %) and 4.1 s for P-CRT (sensitivity = 85 %, specificity = 62 %).
Fig. 3.
Receiver operating characteristic (ROC) curves evaluating the ability of visual capillary refill time (V-CRT, red curve) and of plethysmographic capillary refill time (P-CRT, blue curve) to predict an arterial lactate > 2 mmol/l in septic patients. The areas under the ROC curves were 0.8 (95 % CI=0.65–0.93; p < 0.0001) for V-CRT and. 0.73 (95 % CI: 0.57–0.89; p = 0.043) for P-CRT. CI: confidence interval.
Fig. 4.
Individual values of visual capillary refill time (V-CRT, left panel) and of plethysmographic capillary refill time (P-CRT, right panel) in patients with and without hyperlactatemia.
Discussion
In this study of 43 septic patients, the plethysmographic signal did not improve the accuracy of CRT in predicting lactate levels. In fact, a simple visual evaluation of CRT demonstrated a satisfactory and better predictive ability for arterial lactate levels > 2 mmol/l.
Sepsis involves complex changes in the microcirculation, which can lead to abnormalities in tissue oxygen delivery and consumption [11]. Lactate is traditionally considered a marker of tissue hypoxia and anaerobic metabolism [1,2]. The Surviving Sepsis Campaign recommend to target a decrease in lactate levels during resuscitation [3]. However, the lactate measurement is not widely available in low-resource settings. we hypothesized that CRT could be a surrogate for lactate and that incorporating the plethysmographic signal could improve the accuracy of CRT in predicting lactate levels. We selected a lactate threshold of 2 mmol/l as it is the recommended threshold for defining hyperlactatemia in septic shock [4].
Several reasons could explain the negative results of this study. Firstly, relying solely on visual assessment of the plethysmographic curve for P-CRT measurement may have contributed to these results. Integrating software that can automatically measure P-CRT could improve its accuracy. Secondly, lactate levels may not always reflect tissue hypoperfusion during sepsis, as there are other causes of hyperlactatemia unrelated to tissue hypoperfusion [2]. This discrepancy between tissue perfusion and lactate levels has been suggested to explain the findings of the ANDROMEDA-SHOCK trial, which compared CRT-based resuscitation with lactate-targeted resuscitation in septic shock. CRT-targeted resuscitation in that trial demonstrated lower mortality and faster resolution of organ dysfunction [8].
The idea of using the plethysmographic signal to measure CRT was explored by Morimura et al [9]. In a pilot study involving ICU patients, they attempted to establish a quantitative assessment of capillary refill time (Q-CRT) using the transmitted infrared light intensity of the pulse oximeter [9]. They found a satisfactory correlation between quantitative CRT and arterial lactate (rho=0.68). The ROC curve for the prediction of arterial lactate was superior to ours (AUROC=1; 95 % CI: 1–1). The cut-off value of Q-CRT for predicting a lactate level of ≥2.0 mmol/L was 6.8 s. However, this study included a large proportion of heterogeneous non-septic patients, and the sample size was small. Additionally, the algorithm and device used are not commercially available outside Japan. More recently, the same research team studied the predictive ability of Q-CRT for sepsis screening in the emergency department [10]. Q-CRT showed moderate accuracy for sepsis prediction with an AUROC of 0.74 and a cut-off value of 3.5 s, similar to the one found in our study. A duration of 3 s is usually defined as the upper normal limit of V-CRT [7].
Our study has several limitations. First, it is a monocentric study with a limited sample size. However, our goal was to gather preliminary data on the potential utility of P-CRT compared to V-CRT in predicting lactate levels in septic patients. Second, we did not collect data on patients' skin color, which could affect the generalizability of our results. Lastly, there was no follow-up beyond the first 6 h of admission. Further studies assessing V-CRT and P-CRT changes following resuscitation measures (fluids and vasopressors) are needed.
In conclusion, the integration of the plethysmographic signal did not improve the predictive accuracy of capillary refill time (CRT) for lactate levels in septic patients. However, our findings indicate that visual CRT (V-CRT) alone could effectively serve as a surrogate marker for arterial lactate. A V-CRT threshold of 3.4 s demonstrated good sensitivity and moderate specificity in predicting a lactate level greater than 2 mmol/L. This V-CRT threshold could potentially be used in lieu of lactate to redefine septic shock criteria, particularly in low-income countries.
Dissemination of results
This study was presented at the Moroccan Society of Anesthesiologists Annual Congress.
Author's contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of the data for the work; and the drafting or revising it critically for important intellectual content. CR and YA 40 % each, AB 20 %. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declare no conflicts of interest.
Acknowledgments
Acknowledgments
The authors would like to thank the nursing team in the Emergency and Intensive care Department of Avicenna Military Hospital.
Funding
None.
Footnotes
CRT : capillary refill time ; V-CRT: visual capillary refill time ; P-CRT : plethysmographic capillary refill time ; ICU : intensive care department ; CI : confidence intervals ; ROC : Receiver operating characteristic ; KDIGO : Kidney Disease Improving Global Outcomes ; AUC : area under the curve; Q-CRT : quantitative assessment of capillary refill time
References
- 1.Friedman G., De Backer D., Shahla M., Vincent J.L. Oxygen supply dependency can characterize septic shock. Intensive Care Med. 1998;24:118–123. doi: 10.1007/s001340050531. [DOI] [PubMed] [Google Scholar]
- 2.Hernandez G., Bellomo R., Bakker J. The ten pitfalls of lactate clearance in sepsis. Intensive Care Med. 2019;45(1):82–85. doi: 10.1007/s00134-018-5213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Evans L., Rhodes A., Alhazzani W., Antonelli M., Coopersmith C.M., French C., et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47:1181–1247. doi: 10.1007/s00134-021-06506-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D., Bauer M., et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baelani I., Jochberger S., Laimer T., Otieno D., Kabutu J., Wilson I., et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care. 2011;15(1):R10. doi: 10.1186/cc9410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lima A., Bakker J. Clinical assessment of peripheral circulation. Curr Opin Crit Care. 2015;21:226–231. doi: 10.1097/MCC.0000000000000194. [DOI] [PubMed] [Google Scholar]
- 7.Lara B., Enberg L., Ortega M., Leon P., Kripper C., Aguilera P., et al. Capillary refill time during fluid resuscitation in patients with sepsis-related hyperlactatemia at the emergency department is related to mortality. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0188548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zampieri F.G., Damiani L.P., Bakker J., Ospina-Tascón G.A., Castro R., Cavalcanti A.B., et al. Effects of a Resuscitation Strategy Targeting Peripheral Perfusion Status versus Serum Lactate Levels among Patients with Septic Shock. A Bayesian Reanalysis of the ANDROMEDA-SHOCK Trial. Am J Respir Crit Care Med. 2020;201:423–429. doi: 10.1164/rccm.201905-0968OC. [DOI] [PubMed] [Google Scholar]
- 9.Morimura N., Takahashi K., Doi T., Ohnuki T., Sakamoto T., Uchida Y., et al. A pilot study of quantitative capillary refill time to identify high blood lactate levels in critically ill patients. Emerg Med J. 2015;32:444–448. doi: 10.1136/emermed-2013-203180. [DOI] [PubMed] [Google Scholar]
- 10.Yasufumi O., Morimura N., Shirasawa A., Honzawa H., Oyama Y., Niida S., et al. Quantitative capillary refill time predicts sepsis in patients with suspected infection in the emergency department: an observational study. J Intensive Care. 2019;7:29. doi: 10.1186/s40560-019-0382-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hotchkiss R.S., Moldawer L.L., Opal S.M., Reinhart K., Turnbull I.R., Vincent J.L. Sepsis and septic shock. Nat Rev Dis Primers. 2016;2:16045. doi: 10.1038/nrdp.2016.45. [DOI] [PMC free article] [PubMed] [Google Scholar]