RESUME
Le syndrome du lobe moyen est une entité rare qui doit faire rechercher une cause locale obstructive ou inflammatoire. La broncholithiase, représente une de ses rares causes. Il s’agit d’une pathologie, peu décrite dans la littérature, aux aspects radio cliniques trompeurs.Nous rapportons l’observation d’une jeune patiente consultant pour une hémoptysie récidivante. L’imagerie montrait une atélectasie du lobe moyen. Le diagnostic de broncholithiase a été suggéré en objectivant, au sein du lobe collabé, une calcification siégeant dans la lumière bronchique. La fibroscopie bronchique était peu contributive. La persistance des hémoptysies et un doute avec une néoplasie pulmonaire sous-jacente a conduit à une lobectomie diagnostique et thérapeutique.Le diagnostic de broncholithiase doit être évoqué, devant un syndrome du lobe moyen, en cas de présence de calcification endobronchique à l’imagerie. La chirurgie doit être envisagée, dans les cas litigieux, afin de ne pas méconnaitre une néoplasie sous-jacente.
ABSTRACT
Middle lobe syndrome is a rare but important clinical entity worth investigating in local obstructive or inflammatory cause. One of its rare etiologies is broncholithiasis. We report the observation of a young female patient who presented with recurrent hemoptysis. Chest CT scan showed atelectasis of the middle lobe and suggested the diagnosis of broncholithiasis by objectifying, within the collapsed lobe, a calcification located in the bronchial lumen. Bronchial fibroscopy was of little help. Recurrent hemoptysis and doubt about pulmonary neoplasia led to a diagnostic and therapeutic lobectomy. In front of MLS, broncholithiasis should be suspected in the presence of calcifications on imaging. Surgery may be required in case of uncertain cases to not ignore an underlying tumor.
1. INTRODUCTION
Middle lobe syndrome (MLS) is a rare entity characterized by recurrent or chronic collapse of the middle lobe of the right lung. It was abundantly described in the 80s. From the early 90s, the literature became less abundant. MLS should, then, be investigated for a local obstructive or inflammatory cause. Tuberculosis represents one of its main etiologies in developing countries, notably through mediastinal adenopathies or, much less frequently, through broncholithiasis, which is defined by the presence of calcified material in the bronchial lumen. This last pathological entity is rare with misleading radio clinical aspects (1, 2).
Here, we report an interesting case of MLS caused by broncholithiasis.
OBSERVATION
A 38- years-old woman, without any notable medical history, presented to our pneumology department for recurrent hemoptysis. She reported a chronic cough evolving for 6 months. The clinical examination did not reveal anything remarkable. Chest CT scan identified centimetric mediastinal adenopathies and middle lobe atelectasis. This examination suggested the diagnosis of broncholithiasis by showing calcification in the bronchial lumen of the collapsed lobe (Figure 1). Bronchoscopic revealed an inflammatory change with mucosal oedema of the middle lobar bronchus but did not visualize any endobronchial calcification. No signs of malignancy were found on bronchial biopsies. Sputum and bronchial aspirate were negative for tuberculosis.
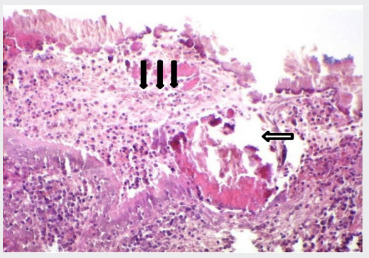
Despite medical treatment, hemoptysis has persisted. Thus, a middle lobectomy was performed for diagnostic purposes and in order not to miss an underlying lung tumor. Anatomopathological examination of the surgical specimen confirmed the diagnosis of broncholithiasis by showing Broncholithiasis 8 yellowish stones in the bronchi on gross examination and intra-bronchial lithiasis debris on microscopic study (Figure 2). The bronchial lymph nodes were reactive on histology.
Figure 1. Axial chest CT image demonstrates a broncholith (arrow) and middle lobe atelectasis .
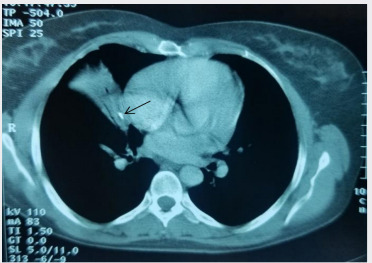
Figure 2. Histopathology images of broncholiths into the bronchial lumen (hollow arrow) .
DISCUSSION
MLS is a rare clinical entity poorly described in the literature. It is characterized by recurrent or chronic collapse of the middle lobe of the right lung (2). This syndrome can be divided pathophysiologically into obstructive and nonobstructive types.
Broncholithiasis is a rare cause of obstructive MLS. In our case, the diagnosis of MLS was made in front of the chronic collapse of the middle lobe on chest CT scan. This examination revealed intrabronchial calcified materiel. The diagnosis of broncholithiasis was confirmed by anatomopathological study. Broncholithiasis is a rare pathology that corresponds to the presence of calcareous concretions in the bronchial lumen.
It is secondary to the migration of calcified mediastinal adenopathy contents into the bronchi (1). Lymph node calcification is secondary, most often, to granulomatous disease, in particular tuberculosis in developing countries, histoplasmosis in the tropical zone and silicosis. Other less common causes of broncholithiasis include calcified endobronchial tumor, intrabronchial calcified foreign body, cryptococcosis, nocardiosis, coccidioidomycosis, actinomycosis and endobronchial aspergillosis (3,4). In our patient’s case, the endemicity of tuberculosis in our country and the evidence of mediastinal adenopathies on the thoracic CT suggested a post-primary tuberculosis infection inflammatory process.
Broncholithiasis may be asymptomatic or it may be revealed by non-specific signs of bronchial irritation. It is most often a dry cough, more rarely recurrent hemoptysis or bronchopulmonary infection. Lithoptysis is pathognomonic of this condition but it is rare, occurring in 6 to 26% of Broncholithiasis 9 cases depending on the series (3). Fistulization in the aorta or esophagus, acute bronchial obstruction or massive hemoptysis may sometimes complicate its evolution and exceptionally lead to death in 0 to 3% of cases (5). Chest CT scan suggests the diagnosis of broncholithiasis by demonstrating endobronchial calcified material. Bronchoscopy is often indicated to confirm the diagnosis (6). In our patient’s case, bronchial fibroscopy could not show any stone. Indeed, the inflammation of the mucosa hindered the visualization of the bronchial distality. According to previous studies, bronchial endoscopy fails to visualize the stone in approximately 50% of cases because of its peribronchial location or airway distortion. PET-CT Scan may be useful to rule out endobronchial neoplasms, which may rarely be calcified and can be mistaken for a broncholith ( 3,7).
Conservative management is warranted in asymptomatic patients. For cases involving complications, therapeutic bronchoscopy may be useful in the removal of endobronchial broncholiths. Surgical treatment is needed when the bronchoscopic extraction fails or if the diagnosis of broncholiths is unclear such is the case of our patient (7).
CONCLUSION
In front of MLS, broncholithiasis should be suspected in the presence of calcifications on imaging. In doubtful cases, surgical resection with removal of the middle lobe may be needed in order not to ignore an underlying tumor amcinolone acetonide at 2-month interval, using a 25-gauge needle, in the involved eyelid subcutaneous tissue, with a considerable reduction of the palpebral lesions at 24-month follow-up (Figure 3). No complications occurred especially no ocular hypertonia or skin discoloration.
References
- Attia S, Boussoffara L, Fkih L, Belhabib D, Fenniche S, Megdiche ML. Broncholithiasis. Rev Mal Respir. 2006;23:348–352. doi: 10.1016/s0761-8425(06)71601-1. [DOI] [PubMed] [Google Scholar]
- Gudbjartsson T, Gudmundsson G. Middle Lobe Syndrome: A Review of clinicopathological features, diagnosis and treatment. Respiration. 2012;84:80–86. doi: 10.1159/000336238. [DOI] [PubMed] [Google Scholar]
- Alshabani K, Ghosh S, Arrossi AV, Mehta AC. Broncholithiasis: A Review. Chest. 2019;156:445–455. doi: 10.1016/j.chest.2019.05.012. [DOI] [PubMed] [Google Scholar]
- Maalej S, Kwas H, Aouadi S, Zidi A, Ismail O, Drira I. Endobronchial aspergillosis associated with broncholithiasis. Presse Med. 2010;39:1331–1333. doi: 10.1016/j.lpm.2010.07.012. [DOI] [PubMed] [Google Scholar]
- Menivale F, Deslee G, Vallerand H, et al. Therapeutic Management of Broncholithiasis. Ann Thorac Surg. 2005;79:1774–1776. doi: 10.1016/j.athoracsur.2003.10.124. [DOI] [PubMed] [Google Scholar]
- Joon Beom S, Koun-Sik S, Jin Seong L, et al. Broncholithiasis: Review of the Causes with Radiologic-Pathologic Correlation. Radiographics. 2002;22:199–213. doi: 10.1148/radiographics.22.suppl_1.g02oc07s199. [DOI] [PubMed] [Google Scholar]
- So YL, Kyung JL, Kyeongman J, et al. Classification of broncholiths and clinical outcomes. Respirology. 2013;18:637–642. doi: 10.1111/resp.12060. [DOI] [PubMed] [Google Scholar]


