Abstract
Objective:
Data on the practice of self-managed medication abortion are limited, in part because this practice takes place purposefully outside of established healthcare systems. Given this, we aimed to ascertain abortion providers’ familiarity with self-managed medication abortion and associated complications, compare regional differences, and evaluate provider attitudes.
Study Design:
We distributed an online survey to members of Society for Family Planning, Association of Reproductive Health Providers, and the Abortion Care Network between July and September 2017 querying experiences with and opinions about self-managed abortion.
Results:
Of 650 respondents, 359 (55.1%) were direct abortion providers. Two hundred and thirty of 335 providers (68.6%) had experience with women trying to interrupt pregnancies on their own, and of those, 153 (76.1%) had seen use of misoprostol and/or mifepristone, and 204 of 342 (59.6%) thought this practice increased in the past 5 years. One hundred and seventeen of 335 (34.9%), witnessed complications from self-managed abortion with misoprostol/mifepristone; most commonly incomplete abortion, and less often hemorrhage, sepsis and uterine rupture. Half of providers, 171 of 321 (53.3%), think that the use of misoprostol/mifepristone for the self-management of abortion is safe.
Conclusion:
Two thirds of respondents had experiences with women attempting to self-manage abortion and about a third witnessed complications related to self-managed medication abortion. About half of respondents agreed that self-managed abortion is safe.
Implications:
There is no consensus amongst providers about the safety of self-managed medication abortion likely due to a lack of rigorous study. However, this study does establish that self-managed abortion is a practice which a majority of respondents have seen amongst their patients and an area that warrants further research.
Keywords: medical abortion, misoprostol, self-managed abortion, provider attitudes, telemedicine
1. Introduction
The safety of medication abortion in a telemedicine or online consultation setting and no direct contact with a provider has been established with years of reassuring safety outcomes [1, 2]. Groups like Women on Web and Safe2Choose have successfully expanded access to abortion throughout the world by mailing medications after an online consultation, but do not currently operate in the United States due to the overall legality, albeit restricted, access to abortion. In an era of increasing restrictions on legal abortions in the United States, clinic closures and mandatory waiting periods have increased the burden on women seeking a legal abortion [3]. Furthermore, with states imposing more restrictions, the mean distance of women to the nearest abortion clinic is also increasing [4]. Murtagh et al. demonstrated that there are options for buying mifepristone and misoprostol online from pharmaceutical companies with the appropriate medications received [5]. However, self-sourcing these medications from potentially unreliable sources without instructions or follow up mechanism is not equivalent to the supervised telemedicine practices previously described. This is a particularly difficult area to study, given that most women who are able to obtain and successfully use these medications on their own will never contact a provider [6]. At the same time, those working in family planning could be the most likely to interact with these women if they are not successful or have complications with a self-managed abortion.
There is a paucity of data regarding abortion providers’ perspectives on the use of self-managed misoprostol and mifepristone for abortion, experience with complications of this technique, as well as the current prevalence of its use. The most recent estimate regarding lifetime prevalence of trying to end a pregnancy without a provider is 1.4% based on a probability based representative sample of US women [7], which is slightly lower than the previously described 1.7% in a 2009 national survey [8]. The difference in safety between these unassisted procedures and telemedicine outcomes has not been described. Given the increasing number of restrictions on obtaining legal abortions in many states, a reasonable hypothesis would be that an increasing number of patients would be turning to this method, especially with the ease of access to information spread on the internet. Our goal is to explore providers’ experiences with self-managed abortion and their opinion on the possibility of a more formalized out of clinic means of providing a medication abortion, given the difficulty women have in accessing abortion care.
2. Methods
After University of Iowa Institutional Review Board approval of all study activities, we sent a secure, web-based, anonymous survey to family planning providers querying abortion provider demographics, knowledge of the use of misoprostol and mifepristone to self-manage abortions and frequency of having patients report prior self-managed abortion attempts, complications witnessed from this practice, and why they think patients choose this to end their pregnancies. We asked about concerns with women self-managing medications and ways that the providers might gain comfort with women taking medications without direct provider involvement. We developed questions with input from each of the organizations involved in disseminating the survey. Most questions used a 5-point Likert scale or multiple choice, with minimal free text responses. The survey was approved by the Society for Family Planning (SFP), Association of Reproductive Health Providers (ARHP), and the Abortion Care Network (ACN) for distribution to their members, which includes physicians, nurse practitioners, nurse midwives, physician assistants, pharmacists, researchers, educators, and other professionals.
Recruitment emails were sent a total of three times at 2–4 week intervals between July and August 2017. A letter containing the elements of consent immediately displayed after the survey link was accessed via the recruitment email.
We collected and stored data in the REDCap (Research Electronic Data Capture) secure, web-based, electronic data capture tool. Statistical analysis was done using SAS version 9.3 (SAS Institute Inc. Base SAS®, Cary, NC, USA). A statistically significant result was defined as p-value <0.05. Comparisons between subject groups utilized Pearson-Chi square tests for categorical variables and Wilcoxon-Rank Sum for ordinal data. Logistic regression was performed to adjust for covariates when grouping into those who had seen self-managed abortion and by regions and states’ hostility towards abortion.
3. Results
3.1. Respondent characteristics
A total of 685 individuals accessed the email link and viewed the consent page, of whom 650 unique respondents started the survey (94.9%). Of the 650 respondents, 359 were direct abortion providers and were included in the full analysis, with demographic details in Table 1. Specifically, of those recruited via SFP, 191 of 501 (38.0%) responded via the link sent by that organization. It was not possible to calculate an exact response rate from the other organizations due to incomplete information about their email lists. Sixty-eight percent of respondents provided more than 100 abortions per year. The majority of providers responding were MD/DOs with completion of residency training (60.4%), with fewer still in training (26.2%) or advanced practice providers (12.0%). Forty-three percent of providers had completed a family planning fellowship.
Table 1.
Characteristics of providers participating in a 2018 online survey of members of reproductive health organizations (N=359).
| Seen self-managed abortion (n=230) | Not seen self-managed abortion (n=105) | p-value | |
|---|---|---|---|
| Abortion services | |||
| Surgical | 7 (3.0%) | 4 (3.8%) | 0.61 |
| Medical | 25 (10.9%) | 15 (14.3%) | |
| Both | 198 (86.1%) | 86 (81.9%) | |
| Number abortions provided per year | |||
| <10 | 12 (5.2%) | 8 (7.6%) | 0.02 |
| 11–100 | 54 (23.5%) | 30 (28.6%) | |
| 101–500 | 96 (41.7%) | 49 (46.7%) | |
| 501–1000 | 37 (16.1%) | 13 (12.4%) | |
| >1000 | 31 (13.5%) | 5 (4.8%) | |
| Provides >100 abortions per year | 164 (71.3%) | 67 (63.8%) | 0.17 |
| Highest level of training | |||
| MD/DO | 56 (24.4%) | 34 (32.4%) | 0.07 |
| MD/DO with completion of residency training | 147 (63.9%) | 56 (53.3%) | |
| ARNP/PA/CNM | 22 (9.6%) | 15 (14.3%) | |
| Other | 5 (2.2%) | 0 (0.0%) | |
| (n=103) | |||
| Completion of family planning fellowship | 112 (48.7%) | 33 (32.0%) | 0.02 |
| Setting | |||
| Hospital | 135 (58.7%) | 60 (57.1%) | 0.79 |
| Private Practice | 68 (29.6%) | 23 (21.9%) | 0.14 |
| Planned Parenthood | 111 (48.3%) | 49 (46.7%) | 0.79 |
| Independent Reproductive Health Clinic | 57 (24.8%) | 22 (21.0%) | 0.44 |
| Other | 23 (10.0%) | 14 (13.3%) | 0.37 |
| Gender | (n=214) | (n=95) | |
| Female | 177 (82.7%) | 83 (87.4%) | 0.12 |
| Male | 37 (17.3%) | 11 (11.6%) | |
| Other | 0 (0.0%) | 1 (1.0%) | |
| Age | (n=216) | (n=98) | |
| 20–30 | 7 (3.2%) | 9 (9.2%) | 0.58 |
| 31–40 | 102 (47.2%) | 45 (45.9%) | |
| 41–50 | 58 (26.8%) | 18 (18.4%) | |
| 51–60 | 26 (12.0%) | 10 (10.2%) | |
| >60 | 23 (10.6%) | 16 (16.3%) | |
| Years providing abortion care | (n=216) | (n=97) | |
| 0–5 | 55 (25.5%) | 37 (38.1%) | 0.02 |
| 6–10 | 57 (26.4%) | 27 (27.8%) | |
| 11–20 | 65 (30.1%) | 18 (18.6%) | |
| >20 | 39 (18.1%) | 15 (15.5%) | |
| Race/Ethnicity | (n=208) | (n=94) | |
| Caucasian | 160 (76.9%) | 65 (69.2%) | 0.56 |
| African American | 13 (6.2%) | 7 (7.4%) | |
| Asian | 23 (11.1%) | 16 (17.0%) | |
| Hispanic | 8 (3.8%) | 5 (5.3%) | |
| Other | 4 (1.9%) | 1 (1.1%) | |
| (n=185) | (n=83) | ||
| Hostile or Extremely hostile state* | 65 (35.1%) | 30 (36.1%) | 0.87 |
| Region | (n=185) | (n=83) | |
| Northeasta | 55 (29.7%) | 19 (22.9%) | 0.38 |
| Southb | 29 (15.7%) | 18 (21.7%) | |
| Midwestc | 32 (17.3%) | 11 (13.2%) | |
| Westd | 69 (37.3%) | 35 (42.2%) |
Defined by Guttmacher institute data year 2017 [3]
Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, Pennsylvania
Delaware, Florida, Georgia, Maryland, North Carolina, South Carolina, Virginia, District of Columbia, West Virginia, Alabama, Kentucky, Mississippi, Tennessee, Arkansas, Louisiana, Oklahoma, Texas
Illinois, Indiana, Michigan, Ohio, Wisconsin, Iowa, Kansas, Minnesota, Missouri, Nebraska, North Dakota, South Dakota
Arizona, Colorado, Idaho, Montana, Nevada, New Mexico, Utah, Wyoming, Alaska, California, Hawaii, Oregon, Washington.
Respondents were varied in practice setting and location, with 58.5% primarily working in hospital settings, 47.1% at a Planned Parenthood affiliate, and fewer in private practice (26.7%) or independent reproductive health clinics (24.2%). The largest number came from the West (39.1%), followed by the Northeast (27.4%), South (17.3%), and Midwest (16.2%). Using the Guttmacher Institute’s definitions of hostile states (4–5 types of major abortion restrictions enacted) and extremely hostile states (≥6 types of major abortion restrictions enacted) in 2017 [3], 35.3% of providers came from hostile or extremely hostile states.
3.2. Experiences with self-managed abortion
The primary outcome measured was if the respondent had taken care of a patient that tried to self-manage an abortion. Two hundred and thirty of 335 providers (68.6%) had experience with women trying to interrupt pregnancies on their own, and of those, 76.1% used misoprostol and/or mifepristone. Fifty-nine percent reported they felt that attempts at self-management by any means have been increasing in the past 5 years and similarly, 59.6% felt attempts with mifepristone and misoprostol have been increasing. Amongst respondents, 34.6% reported seeing an attempted or successful self-managed abortion with misoprostol or mifepristone between 1–4 times in the past year, 4.8% between 5–10 times, and 1.2% greater than 11 times. Those who had seen patients with self-managed abortion were significantly more likely to perform a higher volume of procedures (p=0.02) and to have completed a family planning fellowship (p<0.01). The internet was the most common source where women reported having found information on having an abortion without a provider. Ninety-three percent of respondents agreed that the current political climate (Fall 2017) would result in more women who choose to seek self-management of abortion with misoprostol (with or without mifepristone).
3.3. Complications with self-managed abortion and opinions on safety
Thirty-five percent of respondents had witnessed complications following self-managed abortion with misoprostol and/or mifepristone compared with 46.6% who had seen complications from any type of self-managed abortion. The most frequently observed complication was incomplete abortion and retained products of conception, which comprised 34.7% of the reported types of complication, with hemorrhage following at 25.8% (Figure 1). Serious complications, such as sepsis/shock, undiagnosed ectopic pregnancy, and uterine rupture were much rarer. For each of these circumstances, we are unable to identify if each was a separate incident, or if different providers sharing care of a single patient all reported the same complication.
Figure 1.
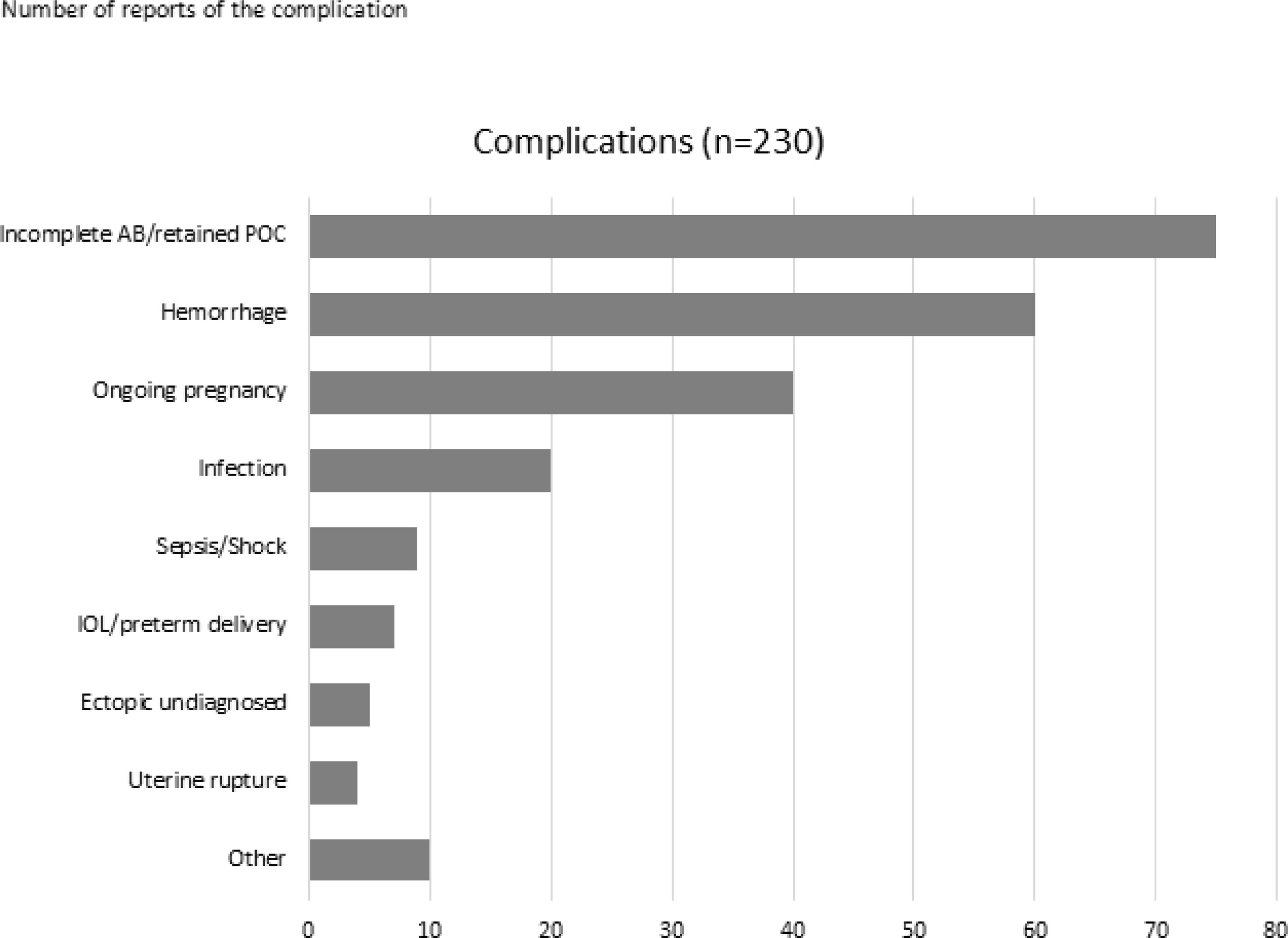
Number of participants reporting having seen each type of complication of a patient presenting after self-sourced medical abortion with mifepristone and/or misoprostol.
About half of providers responding to the survey (53.3%) think that the use of misoprostol (with or without mifepristone) for the self-management of abortion is safe (Figure 2). Those respondents with a higher volume of abortions (>100 per year), were more likely to agree that it is safe (55.1% vs 40.7%, p<0.01). Seventy-six percent felt that a provider/clinic should be able to mail or provide a prescription for medication abortion after a phone or online encounter with a patient/client. Nearly a third, 31.7%, felt that most women would prefer to obtain medication for their abortion from a provider via the mail or an electronic prescription. Even fewer were open to the idea of making medication abortion available over the counter without provider involvement, with 28.8% supporting this delivery model. When asked their top three concerns regarding self-managed abortion, the greatest concern that respondents noted is the possibility of missed or delayed diagnosis of an ectopic pregnancy (72.1%), followed by underestimation of gestational age (68.3%) and women not accessing other in-clinic services such as contraception and sexually transmitted infection testing (55.2%). The risk of incomplete abortion (37.8%) or retained products of conception (14.7%), possible anomalies with ongoing pregnancy (14.4%), and legal issues for women (27.6%) were of less concern.
Figure 2.
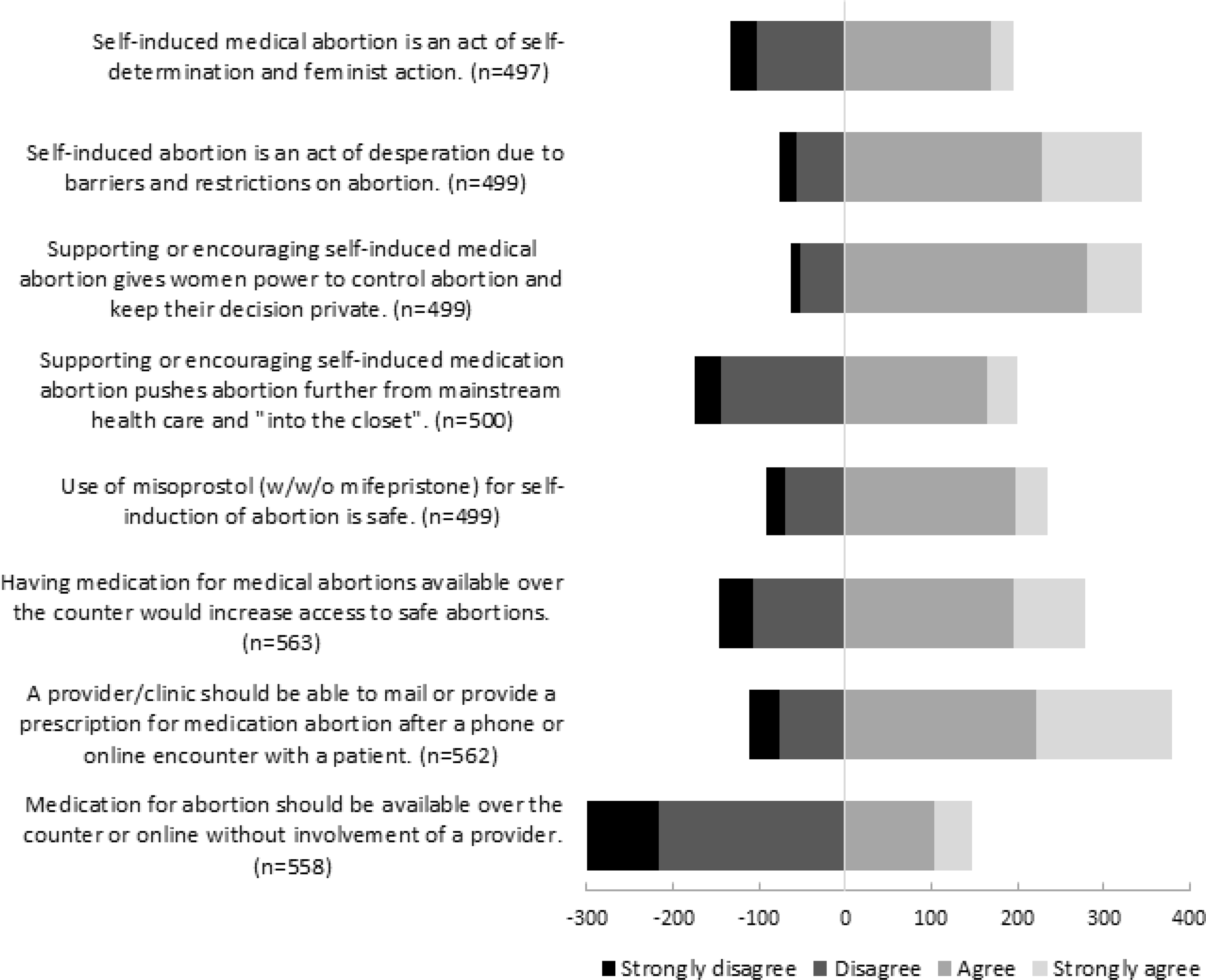
Opinions on safety, desirability, and alternatives to in-clinic medical abortion amongst all respondents.
A telephone hotline for patient questions (73.8%), provision of a clinic number for follow up (72.3%), a more supportive legal environment (65.7%), evidence of good ultrasound dating (61.7%), and reliability of medication sources (57.3%) were all cited to a similar extent as ways that would give respondents more comfort with supporting self-managed abortions. There was no significant difference between responders from states hostile to or supportive of abortion rights.
Looking at safety from a different perspective, respondents were asked if they would use self-managed medical abortion for themselves or their partner, or if they would recommend it to a friend. Only 29% would personally use it and 12% would recommend it to a friend, signifying while although they potentially see this method as safe, most respondents would not choose it.
3.4. Regional differences
With the exception of lower volume of abortions per provider in the West, there were no significant demographic differences regionally. Likewise, those in hostile states were more likely to perform greater than one hundred abortions per year than those in supportive states (79% vs 68%, p=0.049), but were otherwise demographically similar. Rates of seeing self-managed abortion and complications of such did not differ significantly by region or hostility. However, providers in supportive states were more likely to think that providers should be able to mail or provide a prescription for medication abortion after a phone or online encounter with a patient/client than those in hostile states (82% vs 68%, p=0.026). There were no significant differences regionally in opinions about safety of self-managed abortion with misoprostol with or without mifepristone.
4. Discussion
The family planning community is aware of the practice of self-managing abortions, and a majority of providers have had patients who presented after some attempt to end their pregnancy on their own. Respondents were split on whether this practice was increasing, which is potentially related to increased reports in news and the literature. Responses can only represent those women who saw a provider either due to a failed attempt at self-management or for care at a later time. It cannot capture those women who were able to successfully end their pregnancy on their own, or who chose not to reveal any attempts to their provider. Additionally, the response rate was low for the SFP members, and likely low amongst the other organizations as well, so we cannot generalize these data to all abortion providers. However, those responding were diverse in terms of age, experience, practice location, and type of practice, capturing a wide range of experiences. The population of women self-managing abortion is difficult to study directly given their limited contact with healthcare, however, we gained indirect insight into self-managed abortion by querying the providers with whom they are most likely to come into contact.
Over one third of providers had seen complications following self-managed abortion, and in most cases, complications were minor, such as incomplete abortion. However, there were reports of hemorrhage, missed ectopic pregnancies, sepsis and uterine rupture, all of which could be life-threatening. The reporting of frequency of complications is limited by the fact that multiple providers could have reported the same adverse event if multiple respondents were involved in a case. Another limitation with the relatively low response rate, as compared to the large number of members of the various groups, is that there may have been participation bias, potentially inflating the number that had seen complications, since those providers might be more apt to respond. At the same time, those trying to promote this method may also have responded at greater rates. Our sampling did not include emergency room and primary care providers, who may have more contact with women self-managing abortions, although patients may not openly tell those providers.
The greatest concerns of respondents involved missing an ectopic pregnancy and underestimation of gestational age. Both of these concerns would be alleviated if ultrasound documenting an intrauterine pregnancy was provided. However, ultrasound is not required for medical abortion and women are able to accurately estimate gestational age [9]. A model exists with the Tabbot Foundation in Australia providing medications and instructions by mail after an ultrasound is verified, but accurate gestational dating by LMP and provision of ectopic precautions also can suffice [10]. Further research into the feasibility of mailing medications from an existing abortion clinic instead of the multiple unregulated online pharmaceutical companies without provider involvement could be studied in areas where legal obstacles do not exist.
Expanding care delivery will be a legal challenge, with 34 states currently requiring that medication abortion be provided by a licensed physician and 19 states requiring that the prescribing physician must be in the physical presence of a patient [11]. However, this may be the care delivery model preferred by some patients. Over half of abortion providers responding to this survey think that self-managed abortions are safe and given the lack of access to traditional abortion care, this practice likely will continue. With the frequency at which self-managed abortion is encountered, further research involving self-managed medication abortion feasibility, fiscal saliency, safety, efficacy, and harm-reduction models are necessary, especially given likely increased restrictions on abortion in the current political climate.
Acknowledgements:
We would like to thank the Society for Family Planning, Association of Reproductive Health Providers, and Abortion Care Network for helping us in the design and distribution of the survey. REDCap for data capture was made available by the University of Iowa Institute for Clinical and Translational Science, supported by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002537, but the content is solely the responsibility of the authors.
Footnotes
Declarations of interest: none
References
- [1].Grossman D, Grindlay K. Safety of Medical Abortion Provided Through Telemedicine Compared With In Person. Obstetrics and gynecology. 2017;130:778–82. [DOI] [PubMed] [Google Scholar]
- [2].Aiken ARA, Digol I, Trussell J, Gomperts R. Self reported outcomes and adverse events after medical abortion through online telemedicine: population based study in the Republic of Ireland and Northern Ireland. Bmj. 2017;357:j2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Nash E, Gold RB, Mohammed L, Ansari-Thomas Z, Cappello O. Policy Trends in the States, 2017. Policy Analysis Guttmacher Institute; 2018. [Google Scholar]
- [4].Bearak JM, Burke KL, Jones RK. Disparities and change over time in distance women would need to travel to have an abortion in the USA: a spatial analysis. The Lancet Public Health.2:e493–e500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Murtagh C, Wells E, Raymond EG, Coeytaux F, Winikoff B. Exploring the feasibility of obtaining mifepristone and misoprostol from the internet. Contraception. 2017. [DOI] [PubMed] [Google Scholar]
- [6].Kapp N, Blanchard K, Coast E, et al. Developing a forward-looking agenda and methodologies for research of self-use of medical abortion. Contraception. 2018;97:184–8. [DOI] [PubMed] [Google Scholar]
- [7].Grossman D, Ralph L, Raifman S, et al. Lifetime prevalence of self-induced abortion among a nationally representative sample of U.S. women. Contraception. 2018;97:460. [Google Scholar]
- [8].Jones RK. How commonly do US abortion patients report attempts to self-induce? Am J Obstet Gynecol. 2011;204:23 e1–4. [DOI] [PubMed] [Google Scholar]
- [9].Bracken H, Clark W, Lichtenberg ES, et al. Alternatives to routine ultrasound for eligibility assessment prior to early termination of pregnancy with mifepristone-misoprostol. BJOG. 2011;118:17–23. [DOI] [PubMed] [Google Scholar]
- [10].Hyland P, Raymond EG, Chong E. A direct-to-patient telemedicine abortion service in Australia: Retrospective analysis of the first 18 months. The Australian & New Zealand journal of obstetrics & gynaecology. 2018. [DOI] [PubMed] [Google Scholar]
- [11].Medication Abortion. State Laws and Policies: Guttmacher Institute; 2018. [Google Scholar]


