Short abstract
For truly informed decision making, patients need access to high quality information on treatments. Trevor Jones of the Association for the British Pharmaceutical Industry (ABPI) and Wendy Garlick of the Consumers' Association debate whether drug advertising direct to the public would help the quest for such information
Increasingly, patients have been seeking to learn more about their health and about treatments available. A symptom of the demand for this greater awareness and choice has been the growth of patient organisations. They provide information—often in great detail—to patients and therefore require a full understanding of, and information about, the diseases in which they specialise and the appropriate treatments. But they do not have the same level of information about medicines as a manufacturer.
Figure 1.
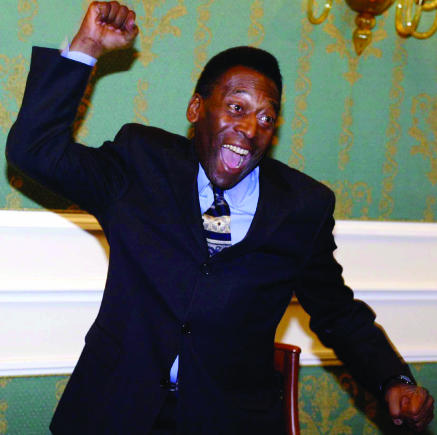
A talent for selling: Pfizer has employed ex-Brazilian football star Pele to advertise its impotence cures
FERRINI/AP RENATO
Until now, other than through patient information leaflets, legal restrictions have made it difficult for pharmaceutical manufacturers to provide information to patients about the medication they take. But patient information leaflets—contained in medicine packs—have essentially become part of the regulatory dossier and, in many cases, cannot practicably provide comprehensive information about medicines to patients. Nor do patients, carers, and the public have direct access to factual, non-promotional information from pharmaceutical companies on diseases and treatment options—despite the fact that companies are well qualified to meet many of these needs.
Pharmaceutical companies spend an average of 10-12 years developing a new medicine, which gives them unparalleled knowledge and experience of their products that many patients and carers would find invaluable. Yet, it remains the only industry where companies are forbidden from communicating with their individual customers about their products.
Ensuring that patients and carers have access to accurate information is of real concern. Existing sources of information contain much that is of poor quality. But let us make it crystal clear, it is information that the UK based pharmaceutical industry wants to be able to give patients. Some opponents confuse the provision of information with US-style media and television product advertising campaigns. While these do bring benefits, they are not on the agenda in Europe.
Poor information is often supplied, especially on the internet, by various parties, whereas, ironically, the manufacturers are severely restricted from providing information on the medicines they have researched and developed with patients and carers. Pharmaceutical companies wish to respond to patients seeking help by providing accurate, balanced, scientifically based, and ethically sound information about their medicines and the treatment of their illness.
All stakeholders, including the pharmaceutical industry, have a part to play in the provision of information to the public. All health information providers should adopt best practice guidelines to ensure consumers understand the context in which information is being provided. The ABPI accepts that the quality of information is important and supports the need for effective self regulation and the principles of good practice. Indeed, at present, the work of the Prescription Medicines Code of Practice Authority shows the industry's ability to self regulate drug promotion to healthcare professionals. The authority's rigorous implementation of the code demonstrates that the industry can be trusted to provide reliable information, but it also shows that confidence can also be maintained in the industry's ability to regulate itself.
The government has shown its recognition of the value in encouraging patients to become better informed by launching the Expert Patient initiative in 2001.1 In addition, the Wanless report, published in April 2002, outlines information as a crucial factor in determining future health outcomes for Britain.2 Provision of information should enhance the relationship and understanding between doctors and patients and should not, as some critics suggest, prejudice a doctor's behaviour or professional judgment. Ultimately, the doctor is still responsible for prescribing decisions and the choice of treatment. Encouraging and assisting patients to have greater knowledge and involvement in their own health care can often lead to earlier diagnosis, early intervention, and ultimately better health outcomes. Better diagnosis and treatment of illness can, in the long run, save the NHS money, but, more importantly, it is a welcome result for patients.
The fact this is being discussed at European level is a clear indication that the need for greater communication with patients is widely accepted. Though these proposals are a step in the right direction, they need to be much less restrictive if they are to have a real and swift impact on patients' access to more and better information. It is no longer acceptable to keep patients in the dark and to expect them to be happy relinquishing control of their health care in order to avoid difficult decisions on availability of treatment and affordability. Informed patients can lead to better health outcomes, a reduction in hospitalisations and other health related costs, as well as an increase in the number of patients complying with their prescribed courses of medication. In fact, the benefits far outweigh the risks and will lead to improved health care.
The few who oppose allowing the industry to communicate quality information suggest that such a move would lead to a large increase in the NHS drugs bill. It's certainly true that, thanks to “postcode prescribing,” patients are not always given information about appropriate treatments that are deemed “too expensive.” If we can help them find out about what is available, and how it can help them deal with their condition better, it might cost more—but would be a price well worth paying.
But the NHS medicines bill will not soar. Patients with a greater understanding of their medicines and the benefits that they obtain from taking them as prescribed will inevitably have better health outcomes. This then leads to more effective and efficient health care for the population as a whole.
Competing interests: TJ is director general of the Association of the British Pharmaceutical Industry, which represents around 80 UK based companies which research, develop, manufacture, and supply more than 90% of the medicines prescribed through the NHS. He is also a non-executive director of Merlin Bioscience Fund and the stem cell company ReNeuron.
Listen to the BMJ Round Table Debate: "Doctors as Sherpas"
References
- 1.Department of Health. “Patients to become the key decision-makers in their own care,” press release, 14 September 2001. www.info.doh.gov.uk/doh/intpress.nsf/page/2001-0421?OpenDocument (accessed 15 May 2003).
- 2.Wanless D. Securing our future health: taking a long-term view—Final report. London: HM Treasury, 2002. (Wanless report.)