Short abstract
Although intestinal ischaemia is an infrequent event, early recognition and appropriate treatment can reduce the potential for a devastating outcome
Acute or chronic abdominal pain can be the result of many different pathophysiological processes. Many presentations are due to benign processes, whereas others may be life threatening if not recognised swiftly. Among the many possible causes, clinicians need to consider the possibility of intestinal ischaemic disorders. The variable vessels involved, location of bowel affected, and different levels of acuity of illness all result in multiple possible presentations. The detection of such a serious condition can be a diagnostic and therapeutic dilemma. This review aims to help clinicians to understand the features and management of acute and chronic mesenteric ischaemia, mesenteric venous thrombosis, and ischaemic colitis.
Sources and selection criteria
The information in this review is based on results of a Medline search for reviews and evidence based studies in major journals from the disciplines of gastroenterology, surgery, and radiology published between 1966 and 2003. The key words used included “intestinal ischemia,” “mesenteric ischemia,” “ischemic colitis,” “mesenteric venous thrombosis,” “mesenteric angiography,” “diagnosis,” “management,” and “treatment.”
Clinical features
Acute mesenteric ischaemia
The recognition of acute mesenteric ischaemia can be difficult, as most patients present with non-specific symptoms, particularly abdominal pain. Classically, pain is disproportionately exaggerated relative to the unremarkable physical findings and persists beyond two to three hours. However, signs of an acute abdomen with distension, guarding (rigidity), and hypotension may also occur, particularly when diagnosis has been delayed.1 Fever, diarrhoea, nausea, and anorexia are all commonly reported. Melena or haematochezia occurs in 15% of cases, and occult blood is detected in at least half of patients.2 The underlying process can involve emboli, arterial or venous thrombosis, vasoconstriction from low flow states, or vasculitis. Embolic occlusion of the superior mesenteric artery occurs in more than half of all cases.3 Most emboli originate in the heart and are potentiated by cardiac arrhythmias or depressed systolic function due to ischaemic heart disease (box 1).
Summary points
Acute intestinal ischaemia and infarction can result from impaired blood flow within the mesenteric arterial or venous systems and are most often caused by thrombotic or embolic disease
Chronic mesenteric ischaemia is often characterised by postprandial abdominal pain, sitophobia, and weight loss
Acute, subacute, or chronic mesenteric venous thrombosis can be the result of primary hypercoagulable disorders or can be secondary to drugs, portal hypertension, paraneoplastic states, or inflammatory abdominal processes
Ischaemic colitis results from conditions causing colonic hypoperfusion and embolic or thrombotic occlusion of the vascular supply of the colon
Computed tomography angiography and magnetic resonance imaging have developed into highly accurate and non-invasive methods of diagnosing mesenteric ischaemia
Surgical revascularisation remains the treatment of choice for mesenteric ischaemia, but thrombolytic medical treatment and vascular interventional radiological techniques have a growing role
In 25% of cases, thrombosis of pre-existing atherosclerotic lesions occurs. Many of these patients report chronic symptoms consistent with previous transient mesenteric ischaemia. Non-occlusive mesenteric ischaemia, which accounts for 20-30% of all cases of acute mesenteric ischaemia, presents similarly but occurs with patent mesenteric arteries. Microvascular vasoconstriction is the underlying process and is precipitated by splanchnic hypoperfusion due to depressed cardiac output or renal or hepatic disease.4
Mesenteric venous thrombosis
Primary or secondary thrombosis of the superior mesenteric vein accounts for 95% of cases and 5-15% of all intestinal ischaemic events. Primary thrombosis is most commonly due to hereditary or acquired hypercoagulation disorders. Deficiencies of protein C, protein S, anti-thrombin III, and factor V Leidin are discovered in some cases, but these proteins may be falsely low in patients with acute thrombosis.5 A variety of malignancies and inflammatory disorders, such as inflammatory bowel disease or pancreatitis, should also be considered as secondary causes. Mesenteric venous thrombosis can also occur postoperatively or as a result of trauma, cirrhosis, portal hypertension, previous endoscopic sclerotherapy for varices, or use of oral contraceptives.6 Clinically, thrombosis can present acutely, subacutely, or chronically as a segmental disease, usually affecting the small intestine rather than the colon. The recognition of acute venous thrombosis is essential, because of the risk of bowel infarction or peritonitis.
Box 1: Causes of acute mesenteric ischaemia
Arterial occlusion (50%)
-
Emboli to superior mesenteric artery:
Mural thrombi from cardiac hypokinesia or atrial fibrillation
Cardiac vavular lesions
Cholesterol embolisation
-
Thrombotic occlusion:
Pre-existing atherosclerotic vessel disease
Acute obstruction of chronic mesenteric ischaemia
Dissecting aortic aneurysm
Vasculitis or arteritis
Fibromuscular dysplasia
Direct trauma
Endotoxin shock
Non-occlusive mesenteric ischaemia (20-30%)
Systemic hypotension
Cardiac failure
Septic shock
Mesenteric vasoconstriction (sympathetic response)
Venous occlusion (5-15%)
-
Primary mesenteric vein thrombosis:
Deficiency of proteins C and S, antithrombin III, factor V Leiden
Antiphospholipid syndrome
Paroxysmal nocturnal haemoglobinuria
-
Secondary mesenteric vein thrombosis:
Paraneoplastic
Pancreatitis
Inflammatory bowel disease
Cirrhosis and portal hypotension
Previous sclerotherapy of varices
Splenomegaly or splenectomy
Postoperative state
Trauma
Oral contraceptives
Extravascular sources
Incarcerated hernia
Volvulus
Intussusception
Adhesive bands
Chronic mesenteric ischaemia
Chronic mesenteric ischaemia, also known as “intestinal angina,” should be considered when a patient reports generalised abdominal pain occurring usually in the postprandial state and persisting for one to three hours. Pain may be minimal at the onset but can progress over weeks or months into an incapacitating condition. Weight loss and sitophobia, the fear of eating, are often reported.3 Severe stenosis or complete obstruction of at least two of the three major splanchnic arteries usually occurs before symptoms are evident, because of the formation of a rich collateral vascular supply. One of the most feared complications is acute thrombosis and the consequent development of bowel infarction.7 Recognition of this can be difficult, as many patients are asymptomatic owing to extensive collateral veins. When thrombosis involves the portal or splenic veins the initial presentation may be variceal bleeding, splenomegaly, or ascites.8
Ischaemic colitis
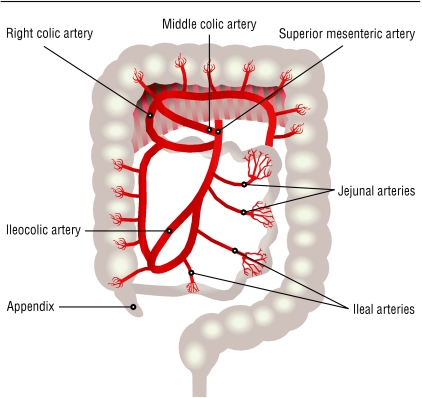
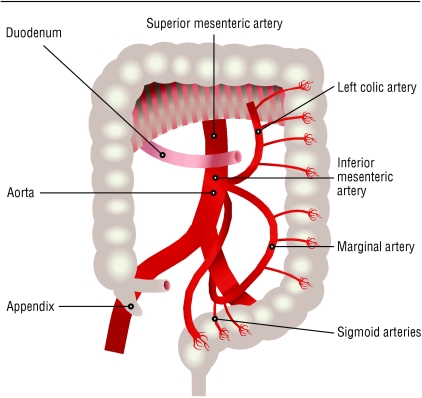
The most common form of ischaemic injury to the gastrointestinal tract is ischaemic colitis.9 The blood supply to the colon and small intestine comes from branches of the superior and inferior mesenteric arteries (fig 1 and fig 2). The rectum also receives blood from the inferior and middle haemorrhoidal arteries, which arise from the internal iliac artery.10 Colonic ischaemia may be precipitated by several conditions, although the cause is not clearly identified in most cases (box 2).
Fig 1.
Distribution of blood supply to the small intestine and colon from the superior mesenteric artery, branches of which include the middle, right, and ileocolic arteries as well as jejunal and ileal arteries and arterioles
Fig 2.
Distribution of blood flow to the colon originating from the inferior mesenteric artery, branches of which include the left colic, marginal, and sigmoid arteries and supply the left colon and superior portion of the rectum
Mesenteric artery emboli, thrombosis, or trauma may lead to occlusive vascular disease and impaired colonic perfusion. Many patients have underlying atherosclerosis.11 Hypoperfusion states due to congestive heart failure, transient hypotension in the perioperative period, and shock due to a variety of causes such as hypovolaemia or sepsis can result in ischaemic colitis.12 In younger patients, vasculitis, oestrogens, cocaine and methamphetamine misuse, psychotropic drugs, use of pseudoephedrine, sickle cell disease, and heritable disorders of coagulation should be considered.13 Most patients experience a sudden onset of mild, left sided lower abdominal pain. Mild haematochezia without haemodynamic instability may occur within 24 hours. The most susceptible areas of the colon to ischaemic damage are the “watershed regions,” which include the splenic flexure and the descending and sigmoid colon.14 Short segments of involved colon may suggest embolic or focal arterial disease, and longer segments are more typical of nonocclusive ischaemia.
Diagnosis
The diagnosis of intestinal ischaemia begins with the ability of the clinician to suspect and recognise it. The clinical history of abdominal pain and non-specific findings may be misleading. However, common clinical conditions should be quickly excluded and mesenteric vascular disease aggressively pursued in patients with the risk factors mentioned above.
The presence of metabolic acidosis, particularly from lactate production, may be a clue to severe bowel ischaemia. Findings on plain x ray films are usually non-specific in acute mesenteric ischaemia and are seen late in the course of illness; they include a non-specific ileus pattern and mesenteric thickening. Classic thumbprinting, seen also on barium studies, indicates submucosal haemorrhage or oedema resulting in focal mural thickening. Intramural pneumatosis and portal venous gas are also noted in acute mesenteric ischaemia but usually in advanced stages of bowel infarction.15 The role of plain films should be rapid identification of perforation or bowel obstruction to expedite surgical management. However, the clinician should also realise that findings might be non-specific for up to 12-18 hours after the onset of symptoms.16
Traditionally, conventional angiography has been regarded as the gold standard imaging method. This is accomplished by arterial injections into the superior mesenteric artery or celiac or splenic arteries and sometimes by direct transhepatic or transjugular portography for identification of venous thrombosis.17 Disadvantages include the highly invasive nature of the investigation, with potential nephrotoxicity and increased exposure to radiation. Advantages of angiography include the ability for concomitant endovascular treatment as described below. Additionally, digital subtraction angiography allows the best visualisation of peripheral splanchnic vessel disease.6,34 Colour Doppler ultrasonography has been used because it is non-invasive and inexpensive. However, it is limited by overlying bowel gas, operator dependent quality, and poor sensitivity for low flow vessel disease.18
Box 2: Conditions that predispose to ischaemic colitis
-
Thrombosis:
Inferior mesenteric artery thrombosis
-
Emboli:
Mesenteric arterial emboli
Cholesterol emboli
Decreased cardiac output or arrhythmias
Shock (sepsis, haemorrhage, hypovolaemia)
Trauma
Strangulated hernia or volvulus
-
Drugs:
Digitalis
Oestrogens
Antihypertensive drugs
Cocaine Methamphetamine
Vasopressin
Phenylephrine
Pseudoephedrine
Immunosuppressive agents
Psychotropic agents
-
Surgery:
Cardiac bypass
Aortic dissection and repair
Aortoiliac reconstruction
Colectomy with inferior mesenteric artery ligation
Gynaecological operations
-
Vasculitis:
Systemic lupus erythematosus
Polyarteritis nodosa (hepatitis B, C)
Thromboangiitis obliterans
Rheumatoid vasculitis
Sickle cell disease
-
Disorders of coagulation:
Protein C and S deficiency
Paroxysmal nocturnal haemoglobinuria
Activated protein C resistance
Antithrombin III deficiency
Long distance running
Colonoscopy or barium enema
Idiopathic
Axial computed tomography imaging has evolved over several years into a very useful modality for diagnosis of mesenteric ischaemia and is the test of choice in the diagnosis of acute mesenteric ischaemia. Findings include focal or segmental bowel wall thickening, submucosal oedema or haemorrhage, pneumatosis, and portal venous gas.19 Contrast enhanced computed tomography detects acute mesenteric ischaemia with sensitivity rates exceeding 90%. Helical computed tomography has improved image quality and scanning times as well as being able to detect non-vascular visceral abnormalities. Computed tomography angiography is also available, with a single breath hold technique to reduce motion artefact.20
Magnetic resonance imaging with angiography is another non-invasive modality that rivals conventional angiography. In mesenteric venous disease, excellent visualisation of the vascular anatomy is possible in addition to assessment of portal venous patency, flow direction, splanchnic thrombosis, and changes suggestive of portal hypertension. Three dimensional gadolinium enhanced reconstruction of vascular anatomy with a single breath hold and ultrafast scanning with digital subtraction angiography are also available.21 Magnetic resonance imaging with angiography has high sensitivity and specificity similar to those of computed tomography angiography, with the advantage of safer gadolinium agents and lack of ionising radiation. Although magnetic resonance imaging with angiography is an excellent tool for the evaluation of chronic mesenteric ischaemia, it should not be the first technique used in the diagnosis of acute mesenteric ischaemia, because of its potentially insufficient resolution to adequately identify non-occlusive low flow states or distal emboli.22,23
The diagnosis of ischaemic colitis depends on the recognition of clinical features. In patients in whom colonic ischaemia is suspected but no signs of peritonitis are present, a sigmoidoscopy should be performed to identify mucosal changes. Computed tomography imaging is usually non-specific and may only show thickening of the bowel wall. Mesenteric angiography usually has no role in the diagnosis of colon ischaemia, because the mesenteric vessels and arcades are usually patent. Damage from hypoperfusion is at the arteriolar level.24
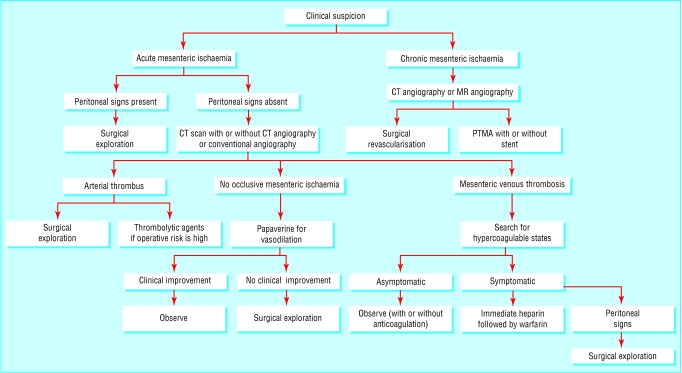
Management
Multiple therapeutic approaches are available for intestinal ischaemia, depending on acuity and extent of disease (fig 3). The presence of peritoneal signs mandates surgical exploration, as bowel infarction has probably occurred. Resection of infarcted bowel as well as embolectomy can be accomplished during this process. In the absence of peritoneal signs, surgical embolectomy is still considered the standard of care.25 However, an interventional radiological approach has been effectively used. Intra-arterial infusion of thrombolytic agents such as streptokinase, urokinase, or recombinant tissue plasminogen activator has been shown to be effective when used within 12 hours of onset of symptoms.26 For-going surgical embolectomy in favour of a less invasive approach may be appropriate in a patient with appreciable operative risk. In non-occlusive mesenteric ischaemia, infusion of an intra-arterial vasodilator such as papaverine into the superior mesenteric artery may be all that is needed to reverse vasoconstriction and prevent bowel infarction.27
Fig 3.
Management of mesenteric ischaemia. CT=computed tomography; MR=magnetic resonance; PTMA=percutaneous transluminal mesenteric angioplasty
In patients with mesenteric venous thrombosis, a search for an underlying hypercoagulable state is essential to preclude recurrent disease. The presence of peritoneal signs should prompt surgical exploration. In an asymptomatic patient, anticoagulation can be administered for three to six months followed by repeat evaluation. Several studies have shown that immediate heparinisation followed by warfarin treatment improves survival. Patients with certain medical conditions such as coagulation disorders and atrial fibrillation may need lifelong anticoagulation.6,28
Box 3: Indications for surgical management of ischaemic colitis
Peritoneal signs: perforation, fulminant colitis, gangrene
Massive haemorrhage
Recurrent fever or sepsis
Continuation of symptoms beyond two to three weeks
Chronic protein losing colopathy
Chronic segmental colitis with ulceration
Symptomatic ischaemic stricture
Additional educational resources
Review articles
Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. Gastroenterology 2000;118: 954-68
Gandhi SK, Hanson MM, Vernava AM, Kaminski DL, Longo WE. Ischemic colitis. Dis Colon Rectum 1996;39: 88-100
Greenwald DA, Brandt LJ, Reinus JF. Ischemic bowel disease in the elderly. Gastroenterol Clin North Am 2001;30: 445-73
Kumar S, Sarr MG, Kamath PS. Current concepts: mesenteric venous thrombosis. N Engl J Med 2001;345: 1683-8
Useful websites
Medline plus (www.nlm.nih.gov/medlineplus/ency/article/001151.htm)—describes symptoms, diagnostic tests, and management of intestinal ischaemia, including a few diagrams
First Principles of Gastroenterology (www.gastroresource.com/GITextbook/en/chapter8/8-2.htm)—provides a classification of intestinal ischaemic disorders and pertinent diagnostic tests and management
Patient resources
American College of Gastroenterology (www.acg.gi.org/patientinfo/gihealth/ischemia.html)—contains free information for patients, explaining briefly what intestinal ischaemia is and how it is recognised and managed
Merck Source (www.mercksource.com)—quick reference to help patients to understand the symptoms and signs of intestinal ischaemia and what to expect from their doctor
Surgical revascularisation has been shown to give long term symptom relief in up to 96% of patients with chronic mesenteric ischaemia suitable for surgery.29 The patency of the bypass graft, a more objective predictor of success, has been documented with rates of 78% at five years.30 In the past decade, however, percutaneous transluminal mesenteric angioplasty with or without a stent has become a viable alternative for selected patients.31 Initial studies have shown angioplasty to have similar outcomes to surgical bypass and embolectomy but have included only small numbers of patients. This alternative has been used most often in patients who are at high risk for surgical revascularisation.32
The variable presentations of ischaemic colitis dictate the management (box 3). In most cases, ischaemia resolves once the underlying cause of hypoperfusion to the colon has resolved. Most patients need bowel rest and supportive care.11 Prophylactic antibiotics have been advocated, but their benefit is unproved. Rarely, fulminant ischaemic colitis occurs with gangrene or perforation and needs urgent surgical exploration. In some cases, ischaemic colitis does not completely resolve and may develop into a chronic segmental colitis or stricture. If symptoms persist beyond two to three weeks a segmental colectomy is indicated. If ischaemic strictures are asymptomatic, observation is warranted as some will resolve within 12-24 months.33,34
Conclusion
The clinical spectrum of intestinal ischaemic disease is quite extensive. Timely recognition is essential for a favourable outcome. Compromise of the mesenteric blood flow, both arterial and venous disease, can result in acute ischaemia and infarction and needs an aggressive approach combining surgical and radiological expertise. Chronic mesenteric ischaemia should be considered as a source for abdominal pain after other more common causes are excluded. The outcome of ischaemic colitis can range from complete resolution to fulminant colitis.
Competing interests: None declared.
References
- 1.Edwards MS, Cherr GS, Craven TE, Olsen AW, Plonk GW, Geary RL, et al. Acute occlusive mesenteric ischemia: surgical management and outcomes. Ann Vasc Surg 2003;17: 72-9. [DOI] [PubMed] [Google Scholar]
- 2.Boley SJ, Sprayregan S, Vieth FJ, Siegelman SS. An aggressive roentgenologic and surgical approach to acute mesenteric ischemia. Surg Annu 1973;5: 355-78. [PubMed] [Google Scholar]
- 3.Brandt LJ, Boley SJ. AGA technical review on intestinal ischemia. Gastroenterology 2000;118: 954-68. [DOI] [PubMed] [Google Scholar]
- 4.Trompeter M, Brazda T, Remy CT, Vestring T, Reimer P. Non-occlusive mesenteric ischemia: etiology, diagnosis, and interventional therapy. Eur Radiol 2002;12: 1179-87. [DOI] [PubMed] [Google Scholar]
- 5.Kumar S, Sarr MG, Kamath PS. Current concepts: mesenteric venous thrombosis. N Engl J Med 2001;345: 1683-8. [DOI] [PubMed] [Google Scholar]
- 6.Abdu RA, Zakour BJ, Dallis DJ. Mesenteric venous thrombosis—1911 to 1984. Surgery 1987;101: 383-8. [PubMed] [Google Scholar]
- 7.Moawad J, Gewertz BL. Chronic mesenteric ischemia: clinical presentation and diagnosis. Surg Clin North Am 1997;77: 357-70. [DOI] [PubMed] [Google Scholar]
- 8.Bradbury MS, Kavanagh PV, Chen MY, Weber TM, Bechtold RE. Noninvasive assessment of portomesenteric venous thrombosis: current concepts and imaging strategies. J Comput Assist Tomogr 2002;26: 392-404. [DOI] [PubMed] [Google Scholar]
- 9.Gandhi SK, Hanson MM, Vernava AM, Kaminski DL, Longo WE. Ischemic colitis. Dis Colon Rectum 1996;39: 88-100. [DOI] [PubMed] [Google Scholar]
- 10.Harnsberger JR, Longo WE, Vernava AM. Vascular anatomy. Semin Colon Rectal Surg 1994;5: 2-13. [Google Scholar]
- 11.Greenwald DA, Brandt LJ. Colonic ischemia. J Clin Gastroenterol 1998;27: 122-8. [DOI] [PubMed] [Google Scholar]
- 12.Sakai L, Keltner R, Kaminski D. Spontaneous and shock-associated ischemic colitis. Am J Surg 1980;140: 755. [DOI] [PubMed] [Google Scholar]
- 13.Reinus JF, Brandt LJ, Boley SJ. Ischemic diseases of the bowel. Gastroenterol Clin North Am 1990;19: 319-43. [PubMed] [Google Scholar]
- 14.Hunter GC, Guernsey JM. Mesenteric ischemia. Med Clin North Am 1988;71: 1091-115. [DOI] [PubMed] [Google Scholar]
- 15.Greenwald DA, Brandt LJ, Reinus JF. Ischemic bowel disease in the elderly. Gastroenterol Clin North Am 2001;30: 445-73. [DOI] [PubMed] [Google Scholar]
- 16.Smerud MJ, Johnson CD, Stephens DH. Diagnosis of bowel infarction: a comparison of plain films and CT scans in 23 cases. AJR Am J Roentgenol 1990;154: 99-103. [DOI] [PubMed] [Google Scholar]
- 17.Lefkowitz Z, Cappell MS, Lookstein R, Mitty HA, Gerard PS. Radiologic diagnosis and treatment of gastrointestinal hemorrhage and ischemia. Med Clin North Am 2002;86: 1357-99. [DOI] [PubMed] [Google Scholar]
- 18.Roobottom CA, Dubbins PA. Significant disease of the celiac and mesenteric arteries in asymptomatic patients: predictive value of Doppler sonography. AJR Am J Roentgenol 1993;161: 985-8. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan SR. Acute mesenteric ischemia: recent advances in diagnosis and endovascular therapy. Emery Radiol 2000;7: 231-6. [Google Scholar]
- 20.Ha HK, Rha SE, Kim AY, Auh YH. CT and MR diagnoses of intestinal ischemia. Semin Ultrasound CT MR 2000;21: 40-55. [DOI] [PubMed] [Google Scholar]
- 21.Meaney JF, Prince MR, Nostrant TT, Stanley JC. Gadolinium-enhanced MR angiography of visceral arteries in patients with suspected chronic mesenteric ischemia. J Magn Reson Imaging 1997;7: 171-6. [DOI] [PubMed] [Google Scholar]
- 22.Laissy JP, Trillaud H, Douek P. MR angiography: noninvasive vascular imaging of the abdomen. Abdom Imaging 2002;27: 488-506. [DOI] [PubMed] [Google Scholar]
- 23.Gilfeather M, Holland GA, Siegelman ES. Gadolinium-enhanced ultrafast three-dimensional spoiled gradient-echo MR imaging of the abdominal aorta and visceral and iliac vessels. Radiographics 1997;17: 423-32. [DOI] [PubMed] [Google Scholar]
- 24.Fitzgerald SF, Kaminski DL. Ischemic colitis. Semin Colon Rectal Surg 1993;4: 222-8. [Google Scholar]
- 25.Endean ED, Barnes SL, Kwolek CJ, Minion DJ, Schwarcz TH, Mentzer RM. Surgical management of thrombotic acute intestinal ischemia. Ann Surg 2001;233: 801-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simo G, Echenagusia AJ, Camunez F, Turegano F, Cabrero A, Urbano J. Superior mesenteric arterial embolism: local fibrinolytic treatment with urokinase. Radiology 1997;20: 775-9. [DOI] [PubMed] [Google Scholar]
- 27.Rivitz SM, Geller SC, Hahn C. Treatment of acute mesenteric venous thrombosis with transjugular intramesenteric urokinase infusion. J Vasc Interv Radiol 1995;6: 219-28. [DOI] [PubMed] [Google Scholar]
- 28.Rhee RY, Gloviczki P. Mesenteric venous thrombosis. Surg Clin North Am 1997;77: 327-28. [DOI] [PubMed] [Google Scholar]
- 29.Kihara TK, Blebea J, Anderson KM, Freidman D, Atnip RG. Risk factors and outcomes following revascularization for chronic mesenteric ischemia. Ann Vasc Surg 1999;13: 37-44. [DOI] [PubMed] [Google Scholar]
- 30.Moaward J, McKinsey JF, Wyble CW, Bassiouny HS, Schwartz LB, Gewertz BL. Current results of surgical therapy for chronic mesenteric ischemia. Arch Surg 1997;132: 613-9. [DOI] [PubMed] [Google Scholar]
- 31.Loomer DC, Johnson SP, Diffin DC, DeMaioribus. Superior mesenteric artery stent placement in a patient with acute mesenteric ischemia. J Vasc Interv Radiol 1999;10: 29-32. [DOI] [PubMed] [Google Scholar]
- 32.Johnston KW, Lindsay T, Walker PM, Kalman PG. Mesenteric arterial bypass grafts: early and late results and suggested surgical approach for chronic and acute mesenteric ischemia. Surgery 1995;118: 1-7. [DOI] [PubMed] [Google Scholar]
- 33.Guttormson NL, Bubrick MP. Mortality from ischemic colitis. Dis Colon Rectum 1989;32: 469-72. [DOI] [PubMed] [Google Scholar]
- 34.Longo WE, Ballantyne GH, Gusberg RJ. Ischemic colitis: patterns and prognosis. Dis Colon Rectum 1992;35: 726-30. [DOI] [PubMed] [Google Scholar]