Short abstract
Despite worldwide efforts to prevent HIV infection, the number of people affected continues to rise. The authors of this article argue that a commonsense approach based on simple country by country analyses could improve the situation
Every year, the United Nations releases new estimates of the number of people living with HIV infection. Despite 20 years of experience with prevention programmes, this number continues to rise. To date, around 60 million people have been infected with this preventable, fatal viral infection—a sad indictment of the world's prevention efforts so far.1
Why have we not done better? Some people suggest that we have focused too much on the behaviours that spread the virus, rather than on the social and economic conditions that promote such behaviours.2 We believe, rather, that many countries are failing because they are not paying enough attention to who is becoming infected and how. Plans for prevention are often built on broad categorisations of type of epidemic rather than on a careful analysis of where new infections are occurring.
Countries do need to tackle the structural factors that support risky behaviour. Structural change takes time, however, so even this work must be focused on the factors that are most likely to enable people in a particular country to reduce their exposure to HIV. Almost all new HIV infections occur when an infected person shares body fluids with an uninfected person, so prevention programmes must focus on situations in which this is happening.3,4 This should be obvious, but many countries are being sold “off the peg” prevention packages based on arbitrary numerical thresholds: “If HIV is over 1% in pregnant women, do this; if not, do that.” This approach is no substitute for careful analysis of patterns of transmission within a country, and such analysis is rarely undertaken.5,6 Indeed, many countries do not even collect the information they need to determine which behaviours are responsible for most new HIV infections. We believe that relatively simple analyses can highlight the differences in categories of exposure between prevalent and incident cases of HIV, can point to important shifts in patterns of transmission, and can in turn lead to better prevention programming.
Methods
We examined current levels and trends in patterns of prevalence and incidence of HIV in five countries that differ by level, category, and age of epidemic: Cambodia, Indonesia, Honduras, Russia, and Kenya. We obtained information on prevalence of HIV and sexually transmitted infections from recent surveys completed in the five countries.7–17 The description of the analytical approaches and the software used for the analyses presented here are available at www.epidem.org.
Results
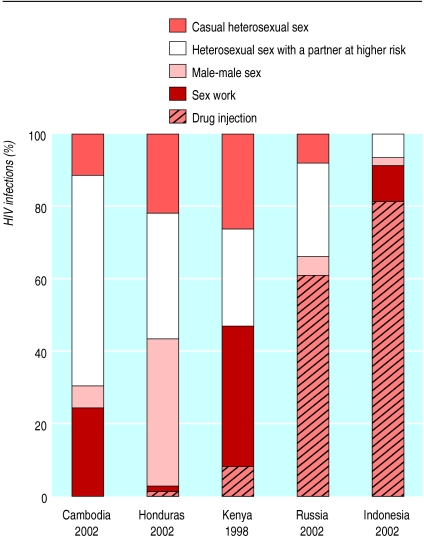
Incidence by category of exposure (fig 1) varied widely between countries, including countries considered to have the same “type” of epidemic, defined as low level, concentrated, or generalised. Kenya, Cambodia, and Honduras are all classified as having generalised epidemics, with a prevalence of HIV infection over 1% in the adult population. Cambodia and Honduras have similar levels of adult prevalence—2.7% and 1.6%.18 The three countries have very different patterns of exposure, however. Russia and Indonesia have concentrated epidemics, with prevalence in adults below 1%, but again there are clear differences in exposure.
Fig 1.
Distribution of new HIV infections by type of exposure in selected countries, 1998-2002. Data on behaviour and HIV prevalence drawn from references 7–17
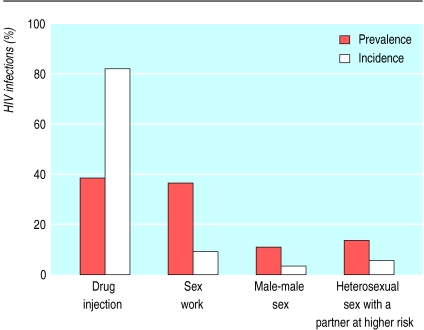
Many countries use prevalence data to guide planning of prevention, but as figure 2 illustrates huge differences can exist between prevalent and incident infections. Whereas drug injection and sex work accounted for roughly the same proportion of existing infections in Indonesia in 2002, a rapidly escalating epidemic of injecting drug use means that unsafe injecting will account for over 75% of new infections in 2003. Clearly, failure to examine current patterns of incidence can lead to inappropriate prevention efforts.
Fig 2.
Distribution of prevalent and incident HIV infections by type of exposure in Indonesia, 2002. Data on behaviour and HIV prevalence drawn from references 10, 11, and 17
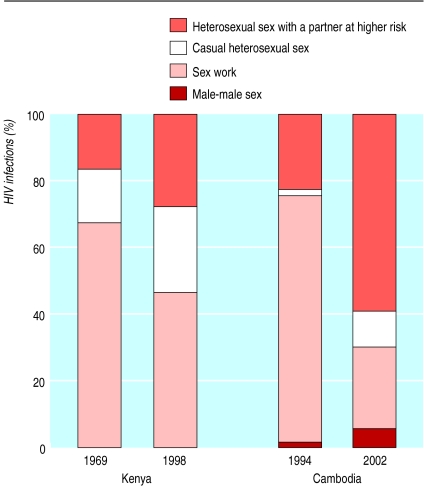
Current patterns of HIV incidence may differ from current patterns of prevalence but are clearly not independent of them. This is illustrated in figure 3, which shows the changing distribution of transmission in Kenya and Cambodia.
Fig 3.
Distribution of new HIV infections by type of exposure, Kenya 1989-98 and Cambodia 1994-2002. Data on behaviour and HIV prevalence drawn from references 8, 9, 15, and 16
In Cambodia, HIV infection was driven for years by an active sex industry. Prevention efforts focused on decreasing unprotected sex work transactions have been remarkably successful. The proportion of men in mobile occupations buying sex has dropped from 76% to 32% in the past five years, and condom use has doubled to 87% over the same period.6 This has had a dramatic impact on the total number of new infections, which plummeted from an estimated 40 000 in 1994 to 6500 in 2002. Because HIV infection acquired through sex work has fallen so radically the proportion of new infections transmitted within marriage has grown from 11% to 46%. Clearly, more attention should now be given to prevention strategies aimed at reducing transmission between spouses who may previously have been exposed to HIV through buying or selling sex, while sustaining existing prevention efforts focused on sex work.
Cambodia is classified as having a “generalised” epidemic, and indeed the current nexus of infection has shifted beyond groups with identifiable “high risk” behaviours; however, the epidemic is not necessarily spreading widely in the general population. People becoming infected are largely those in partnerships in which at least one partner had high risk behaviours in the past. If Cambodia maintains its success in reducing risk in sex work transactions while also cutting into transmission between spouses, HIV prevalence will probably fall to the very low endemic levels recorded in many industrialised nations.
Kenya—another country with a “generalised” epidemic—has had a radically different experience. The epidemic was already well advanced by 1989, when national prevalence of HIV in adults was nearly 4%. Prevalence of HIV infection among sex workers in Nairobi at that time was 60-70%.8 A substantial proportion of men bought sex, and, as figure 3 shows, as many as two thirds of new HIV infections were among sex workers and their clients. Kenya's prevention programme has increased in variety and scope over the years, but neither the proportion of men buying sex nor the proportion of men and women having sex outside marriage has changed much. Use of condoms at latest sexual intercourse with a non-marital partner had risen from very low levels in 1989 to 42% by 1998, but this has not been sufficient to reduce prevalence dramatically.9 The result is that the absolute number of new infections each year more than doubled over the decade in Kenya. The pattern of new infections has changed as the epidemic has evolved, as seen in figure 3, but transmission through commercial sex remains a key factor.
Discussion
Many approaches to the prevention of HIV infection exist. Recently, emphasis has been on altering structural factors such as poverty and sexual inequity that affect people's ability to protect themselves from HIV. In consequence, some public health officials have taken their attention off the virus and the specific behaviours that spread it. Yet an understanding of the dynamics of a country's HIV epidemic, how it changes over time, and who is currently at greatest risk is essential to guiding decisions about effective prevention. Long term structural changes are desirable, but they are often beyond the control of the public health community. In the short term, people planning HIV prevention programmes will make most difference by focusing where most new infections are occurring, while other partners such as religious and political leaders take the lead in changing the social and cultural factors that influence people's sexual and drug taking habits.
This approach should not allow the public health community to shirk responsibility. Indeed, it often means embracing difficulty, inasmuch as the bulk of new infections may, in many countries, be concentrated among some of the most marginalised and politically “untouchable” groups, such as drug injectors and male, female, and transvestite sex workers. We must collect the information we need to track HIV infection and risky behaviour in the populations that may be exposed and use that information to make sensible choices about which prevention efforts are most likely to reduce new infections in a particular country at a particular stage of epidemic.
Clearly, these simple analyses do not provide all the answers needed for a really effective HIV prevention plan at the country level. Like all analyses of national prevalence and incidence, those used here are only as good as the assumptions that inform them. In many cases, relatively few data points are available and these are being applied to very large populations; this is especially problematic for heterogeneous and decentralised countries such as Indonesia and Russia. As surveillance systems improve, however, this type of analysis should be possible at the regional or provincial level, and we would strongly encourage such a shift. However, even broad national analyses based on in-country data will provide a sounder basis for national prevention planning than an “off-the-peg” plan based on a simple global characterisation of epidemic type. As HIV surveillance systems expand to include biological and behavioural surveillance and focus more on the populations most likely to contribute to transmission of HIV, more countries can undertake this kind of analysis and act on it.19
Summary points
Patterns of transmission of HIV vary widely between countries
Patterns of transmission also change over time within a single country, partly because of the success or failure of past efforts at prevention
Simple analyses can indicate who is currently being infected and how
Improved biological and behavioural surveillance systems are providing reliable data for input into such analyses in a growing number of countries
A clearer focus on the behaviours that are responsible for most exposure to HIV in a country should lead to more effective prevention efforts
To say that countries cannot begin a sensible assessment of their prevention efforts without a proper analysis of who is becoming infected with HIV and how they were exposed seems almost too obvious, and yet we so rarely undertake this analysis. With five million new HIV infections to shame us over the past year, it is time to stop stating the obvious and to start doing it.
See also editorial by Ammann
We express our appreciation to the countries that have made their data publicly available. The analyses and estimates reported here do not represent the official estimates of any of the countries. The estimates and opinions expressed in this article are solely those of the authors.
Contributors: All the authors contributed to all aspects of the paper.
Funding: None.
Competing interests: None declared.
References
- 1.Joint United Nations Programme on HIV/AIDS (UNAIDS), World Health Organization. AIDS epidemic update, December 2002. Geneva: UNAIDS/WHO, 2002.
- 2.Barnett T, Whiteside A. AIDS in the twenty-first century: disease and globalisation. Houndsmill, England: Palgrave Global Publishing, 2002.
- 3.Global HIV Prevention Working Group. Global mobilization for HIV prevention: a blueprint for action. White River Junction, VT: Global Health Council, 2002.
- 4.Ainsworth M, Teokul W. Breaking the silence: setting realistic priorities for AIDS control in less-developed countries. Lancet 2000;356: 55-60. [DOI] [PubMed] [Google Scholar]
- 5.Jha P, Nagelkerke NJD, Ngugi EN, Prasada Rao JVR, Willbond B, Moses S, et al. Reducing HIV transmission in developing countries. Science 2001;292: 224-5. [DOI] [PubMed] [Google Scholar]
- 6.Creese A, Floyd K, Alban A, Guinness L. Cost-effectiveness of HIV/AIDS interventions in Africa: a systematic review of the evidence. Lancet 2002;359: 1635–42. [DOI] [PubMed] [Google Scholar]
- 7.Gorbach P, Sopheab H, Leng HB, Vonthanak S. BSS V: sexual behavior among urban sentinel groups: Cambodia 2001 (final report). Phnom Penh, Cambodia: National Center for HIV/AIDS, Dermatology and STDs, Ministry of Health, 2002.
- 8.Kitabu MZ, Maitha GM, Mungai JN, Plummer FA, Ndinya-Achola JO, Temmerman M. Trends and seroprevalence of HIV amongst four population groups in Nairobi in the period 1989 to 1991. VIII International Conference on AIDS, Amsterdam, 7/19-24, Poster PoC 4018.
- 9.National Council for Population and Development. Kenya demographic and health survey, 1998. Nairobi: Central Bureau of Statistics and Macro International, 1999.
- 10.National estimates of HIV infection 2002. Jakarta: Republic of Indonesia, Directorate of Communicable Disease Control and Environmental Health, 2002.
- 11.Behavioural surveillance among populations at risk for HIV, 2002. Jakarta: Republic of Indonesia, Directorate of Communicable Disease Control and Environmental Health, and Central Bureau of Statistics, 2002.
- 12.Rhodes T, Platt L, Filatov KA, Sarang A, Davis M, Renton A. Behavioural risk factors for HIV transmission in eastern Europe and central Asia: a review. Report prepared for UNAIDS and UNICEF, 2002.
- 13.Soto RJ, Padilla IS, Ghee A, Astete S, Alvarenga MA, Hughes JP, et al. Prevalence of HIV/STD and behavior in Honduran female sex workers—the Central American multicenter study of HIV/STD and behavior. XIV International AIDS Conference, Barcelona, July 2002. Abstract WePeC6133.
- 14.Ghee AE, Soto RJ, Padilla I, Alvarenga MA, Astete S, Hughes JP, et al. Prevalence of HIV/STD and behavior in Honduran men who have sex with men—the Central American multicenter study of HIV/STD and behavior. XIV International AIDS Conference, Barcelona, July 2002. Abstract WePeC6132.
- 15.Leng HB, Wantha SS, Sun LP, Sopheap S, Natpratan C, Stuer F, et al. Low prevalence of sexually transmitted infections in Cambodia supports recent behavioral and HIV seroprevalence trends: 2001 Cambodia STI prevalence survey final report. Phnom Penh, Cambodia: National Center for HIV/AIDS, Dermatology and STDs, Ministry of Health, 2002.
- 16.Leng HB. HIV Sentinel Surveillance 2002. Presented on 10 September 2002, Phnom Penh, Cambodia, National Center for HIV/AIDS, Dermatology and STDs, Ministry of Health.
- 17.Estimasi HIV di Indonesia, 2002: Laporan kegiatan estimasi populasi rawan terinfeksi HIV. Jakarta: Ministry of Health, Republic of Indonesia, in press.
- 18.Joint United Nations Programme on HIV/AIDS (UNAIDS). Report on the global HIV/AIDS epidemic 2002. Geneva: UNAIDS, 2002.
- 19.Joint United Nations Programme on HIV/AIDS (UNAIDS), World Health Organization. Guidelines for second generation HIV surveillance. Geneva: UNAIDS/WHO, 2000.