Abstract
Background
The use of acupuncture for stress urinary incontinence is increasing in frequency, especially in Asian area. However, its effectiveness and side effects have not been evaluated.
Objectives
To assess the effectiveness and side effects of acupuncture for stress urinary incontinence in adults.
Search methods
We searched the Cochrane Incontinence Group Specialised Register (searched 28 January 2013), EMBASE, AMED, Chinese Biomedical Literature Database (CBM), Chinese Acupuncture Trials Register and China National Knowledge Infrastructure (CNKI) (all searched 20 February 2013). In addition, we searched the reference lists of relevant articles and contacted authors and trialists in the field.
Selection criteria
Randomised and quasi‐randomised controlled trials of acupuncture interventions without other treatments for the management of stress urinary incontinence for adults.
Data collection and analysis
Two review authors independently assessed eligibility, trial quality and extracted data. We meta‐analysed data where appropriate.
Main results
We identified 17 possibly eligible studies but only one small trial with 60 women met our inclusion criteria. The trial compared acupuncture versus midodrine, a drug for treating hypotension. The risk of bias was high as there was no concealment of randomised allocation, and there was no blinding of assessment of outcome. In addition, it was not possible to blind participants or health providers to the interventions. The statistical methods were not described.
More women improved in the acupuncture group (73% with acupuncture versus 33% with midodrine; risk ratio (RR) 2.20, 95% confidence interval (CI) 1.27 to 3.81) but the cure rates were low and not statistically significantly different (13% versus 7%; RR 2.00, 95% CI 0.40 to 10.11). There were adverse events in the drug group only.
Authors' conclusions
The effect of acupuncture for stress urinary incontinence for adults is uncertain. There is not enough evidence to determine whether acupuncture is more effective than drug treatment.
Keywords: Adult; Female; Humans; Acupuncture Therapy; Acupuncture Therapy/methods; Adrenergic alpha‐1 Receptor Agonists; Adrenergic alpha‐1 Receptor Agonists/therapeutic use; Midodrine; Midodrine/therapeutic use; Randomized Controlled Trials as Topic; Urinary Incontinence, Stress; Urinary Incontinence, Stress/therapy
Plain language summary
Acupuncture for stress urinary incontinence in adults
Stress urinary incontinence is a common disease among older people, especially women. The symptoms are leakage of urine when the person coughs, laughs or exercises. It affects social, psychological, physical and financial aspects of life. Acupuncture is used widely in Asian countries for this condition and frequency of use is increasing worldwide. From the viewpoint of traditional Chinese medicine, acupuncture could improve the symptoms of stress urinary incontinence by reinforcing qi (the vital substance constituting human body) and promoting recovery of the bladder's function. This review included only one small trial with 60 women. There was not enough evidence to assess the effects of acupuncture for stress urinary incontinence compared with drug treatment, and high‐quality randomised controlled trials are needed.
Background
Urinary incontinence can be classified as stress urinary incontinence (SUI), urgency urinary incontinence and mixed urinary incontinence (Haylen 2010; Mariappan 2005). SUI is the most common type in women (Wilson 1996). Prevalence of this disease is different in various parts of the world. A study conducted in Canada reported that an estimated 4% to 35% of adult women are effected by SUI (Luber 2004). In Beijing, the prevalence is 22.9% in adult women (Ge 2009). In a survery conducted in the USA 49.6% respondants reported urinary incontinence symptoms. Of those reporting incontinence symptoms; pure stress incontinence was reported by 49.8% (Reynolds 2011). The current prevalence of SUI in men is below 1% (Hampel 2004). SUI affects social, psychological, physical and financial aspects of life. Over 80% of women decline any treatment, and less than 1% undergo surgical management (Miller 2007).
Therapy for SUI includes behavioural therapy, physiotherapy, medications, devices and surgery (Rogers 2008). Duloxetine is the first licensed drug for the treatment of SUI, but it is poorly tolerated (overall 146/222 (66%) women discontinued therapy due to adverse effects or lack of efficacy) with high discontinuation rates (Duckett 2007; Mariappan 2005). The majority of women initially offered drug therapy will eventually undergo surgery for their incontinence (Vella 2008). Surgery is an effective option (Ogah 2009; Wu 2007). Pelvic floor muscle training (PFMT) is the recommended conservative therapy for SUI and it is more effective than no treatment, placebo drug or inactive control treatments for women with SUI (Dumoulin 2010). It is also the initial option in the treatment of post‐surgical SUI for men (Börgermann 2010; Campbell 2012). However, PFMT therapy needs long‐term adherence. There is a clinically unmet need and a mandate for effective, lower cost, non‐invasive treatment, especially for people living in low‐income regions. Acupuncture, as a minimally invasive treatment, is reported to be effective for SUI (Kim 2008), but its efficacy and safety have not been confirmed.
Description of the condition
The International Continence Society defines SUI as the complaint of involuntary loss of urine on effort or physical exertion, or on sneezing or coughing (Abrams 2002; Haylen 2010). Theoretically, two types of SUI are thought to exist: hypermobility of an otherwise healthy urethra and intrinsic deficiency of the sphincter itself (Hinoul 2009). Standard clinical assessment includes history taking, physical examination, frequency/volume charts and urine analysis. Some authors describe women with the symptoms of SUI alone (diagnosis made on clinical evaluation without urodynamics) (Ogah 2009). The cause of SUI in men is iatrogenic after prostate surgery or traumatic damage to the external urethral sphincter (Börgermann 2010). For women, recognised risk factors for SUI include white race, obesity, pregnancy and childbirth, particularly vaginal, as compared with caesarean, delivery (Rogers 2008).
Description of the intervention
Acupuncture is a branch of traditional Chinese medicine (TCM) and it has a history of thousands of years. It cures disease by stimulating points with needles.
Acupuncture, as a conservative method, includes many methods, such as body acupuncture, scalp acupuncture, electroacupuncture, warm acupuncture, fire needle, auricular acupuncture and elongated needle.
Body acupuncture: a generalised term for acupuncture and is in common use with reference to acupuncture therapy. It means treating disease by applying acupuncture to points along the channels of the human body.
Scalp acupuncture: a therapeutic method for treating diseases associated with the nerve system by using acupuncture needles along the surface of the head.
Electroacupuncture: a therapeutic method combining acupuncture with electrical stimulation (Peng 2007), where two electrodes from an electrical stimulator are attached to the needle handles.
Warm acupuncture: a needle with a firing moxa cylinder (a penetrating heat therapy which involves the burning of mugwort) attached to it, which can dispel coldness.
Fire needle: a needle is heated on a firing spirit lamp until the needle is red and hot, and then skin is pricked with the needle rapidly.
Auricular acupuncture: stimulates points on the ear with a needle or other instruments.
Elongated needle acupuncture: uses a needle that is usually longer than 5 cun (125 mm) (Gao 2002).
This review concentrates on body acupuncture, scalp acupuncture, electroacupuncture, warm acupuncture, fire needle and elongated needle. It excludes cupping, acupressure, laser acupuncture and dry needle as laser acupuncture and dry needle are not routine or traditional acupuncture methods in China, and cupping and acupressure are different therapies from acupuncture in TCM.
How the intervention might work
Although Western medicine does not recognise the mechanism of action, acupuncture is becoming increasingly popular in high‐income countries as a therapy for a wide variety of disorders, most of which are chronic and difficult to manage with conventional treatment (Langevin 2001). For SUI, it is not yet known how acupuncture produces its effects (e.g. whether on muscles, nerves, blood or energy). It is possible that it could desensitise the bladder through inhibition of capsaicin‐sensitive C‐fibre activation (Hino 2010).
According to TCM theory, SUI is mainly caused by deficiency of qi (also known as chi or ch'i and often translated as 'life force' or 'energy flow') of the kidneys, which will lead to the bladder's failure to control urine. There is a recording in Huangdi Neijing (also known as The Inner Canon of Huangdi or Yellow Emperor's Inner Canon, an ancient Chinese medical text) (Wang 2003), that "bladder's failure in controlling the urine leads to incontinence" and in Zhubing Yuanhoulun (General Treatise on Causes and Manifestations of All Diseases) (Ding 1992), "incontinence is due to deficiency of kidney qi". The working mechanism of acupuncture is thought to be in regulating qi and blood, and co‐ordinating yin and yang (used to describe how polar opposites or seemingly contrary forces are interconnected and interdependent in the natural world) (Xu 2002). By needling at some points on the bladder meridian and the kidney meridian, acupuncture can reinforce qi and promote recovery of the bladder's function, and finally improve the symptoms of SUI.
Why it is important to do this review
SUI is a common problem for women and also markedly impairs the quality of life of affected men. Surgery is an effective therapy; however, it has risks (such as injury to the bladder or urethra, urinary retention, incomplete cure of incontinence and severe infection) that some people may find unacceptable. Conservative therapy (i.e. PFMT) has long‐term adherence problems and its value remains uncertain for post‐prostatectomy incontinence in men (Hunter 2007). It is important to establish whether acupuncture is a good choice for people who do not want surgery, and whether it is as effective as other conservative or pharmacological therapies. Although there are reports showing that acupuncture is effective for SUI (Bi 2007; Lim 1995), the efficacy and safety of acupuncture for SUI has not been systematically reviewed. Another Cochrane review covers acupuncture for urinary incontinence after stroke (Thomas 2009).
Objectives
Determine the effects and safety of acupuncture for SUI in adults.
The following comparisons will be addressed:
acupuncture versus placebo or no treatment;
acupuncture versus any other treatment.
Methods
Criteria for considering studies for this review
Types of studies
Randomised and quasi‐randomised (allocating participants to different forms of care that is not truly random; e.g. allocation by date of birth, day of the week, medical record number, month of the year or the order in which participants are included in the study) controlled trials.
Types of participants
Participants of any age or ethnicity, with a diagnosis of SUI (according to the definition of the International Continence Society) were eligible for inclusion. People with SUI diagnosed with or without urodynamics were eligible for included in this review.
Types of interventions
Interventions include scalp acupuncture, body acupuncture, electroacupuncture, warm acupuncture, elongated needle, auricular acupuncture and fire needle.
Cupping, acupressure, laser acupuncture and dry needle acupuncture are excluded here, for laser acupuncture and dry needle acupuncture are not routine or traditional acupuncture methods in China, and cupping and acupressure are different therapies from acupuncture in TCM.
Comparison interventions include placebo, no treatment and any active treatment (i.e. conservative therapies, pharmacological therapies or surgery).
Types of outcome measures
Primary outcomes
Participant symptoms
Number of participants with incontinence.
Number of incontinent episodes over 24 hours (indicated by bladder charts, e.g. mean number of episodes).
Severity of incontinence (e.g. index score).
Perception of lack of improvement in continence (as reported by participant or carer).
Secondary outcomes
Physical measures
Pad tests of quantified leakage.
Volume of urine loss.
Total and mean number of pads used.
Clinicians' observations
Urodynamics.
Objective failure rates after treatment and at follow‐up (number not cured versus cured by objective test).
Quality of life
General health status measures (e.g. Short Form 36).
Specific instrument designed to assess urinary problems (such as distress, anxiety).
Socioeconomic measures
Costs of interventions.
Cost‐effectiveness of interventions.
Adverse events
Number of fainting episodes during acupuncture.
Number of haematomas during treatment.
Number of burns and local infection.
Search methods for identification of studies
We imposed no language or other restrictions on any of the searches.
Electronic searches
This review drew on the search strategy developed for the Cochrane Incontinence Group as a whole. We used the Cochrane Incontinence Group Specialised Register to identify relevant trials. The methods are described under the Group's module in The Cochrane Library. The register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE in Process, CINAHL, and handsearching of journals and conference proceedings. Appendix 1 lists the terms used when searching the Cochrane Incontinence Group Specialised Register. We searched the register on 28 January 2013.
We also searched EMBASE, AMED, Chinese Biomedical Literature Database (CBM), Chinese Acupuncture Trials Register and China National Knowledge Infrastructure (CNKI) on 20 February 2013. Appendix 1 lists the search terms used.
Searching other resources
We conducted the following additional searches: checking all reference lists of identified trials and other relevant articles; contacting authors and trialists in the field to identify any additional data or trials.
Data collection and analysis
Selection of studies
Two review authors considered titles and abstracts identified from the search for inclusion. We evaluated all possibly eligible studies for appropriateness for inclusion without prior consideration of the results. We listed all excluded studies in the Characteristics of excluded studies table with reasons for their exclusion.
Data extraction and management
Two review authors extracted data independently using a standard form containing prespecified outcomes. When data had been collected but not reported, we sought clarification from the trialists. We processed the included trial data as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved differences of opinions by discussion or consultation with a third review author.
Assessment of risk of bias in included studies
Two review authors independently used The Cochrane Collaboration's 'Risk of bias' tool to assess methodological quality. We classified studies as 'low', 'unclear' and 'high' risk of bias.
We considered the following six domains of bias:
sequence generation;
allocation concealment;
blinding (or masks);
incomplete data assessment;
selective outcome reporting;
other sources of bias.
We resolved differences of opinions by discussion or consultation with a third review author or the editorial team.
Measures of treatment effect
We based analyses on available data from the included trial relevant to the comparisons and outcomes of interest. For categorical outcomes, we related the numbers reporting an outcome to the numbers at risk in each group to calculate a risk ratio (RR) with 95% confidence interval (CI). For continuous variables, we used means and standard deviations to calculate a mean difference (MD) with 95% CI.
Unit of analysis issues
The individual participant was the unit of analysis (unit to be randomised for interventions to be compared).
Dealing with missing data
Trials using intention‐to‐treat analysis were included if the participants were analysed in the arms to which they had been randomised, irrespective of whether they received that management. For trials with missing data, we based primary analysis on available data.
Assessment of reporting biases
If there were more than 10 studies in the analysis, we would have used a funnel plot to assess publication bias.
Results
Description of studies
Results of the search
We identified 233 studies. All but 32 of the studies were published in Chinese. We identified 22 possibly eligible studies and we excluded 211 studies because they were not randomised controlled trials or they did not include acupuncture or the participants did not have SUI. Of the remaining 22 studies, we included one study (Characteristics of included studies), assigned one for further assessment (Characteristics of studies awaiting classification) and excluded 20 for other reasons (Characteristics of excluded studies). Figure 1 shows the flow of literature through the assessment process in a PRISMA flowchart.
1.
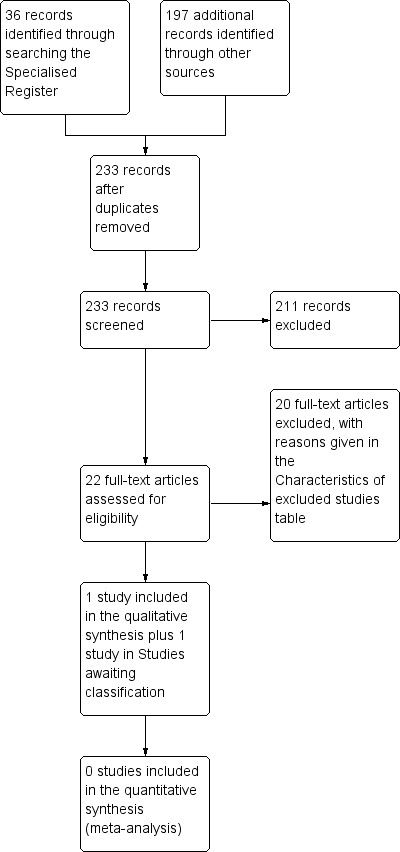
PRISMA study flow diagram.
Included studies
We included one study (Characteristics of included studies table).
Design
We included only one randomised controlled trial (Bi 2007). It compared electroacupuncture versus midodrine. A random number table was used, but there was no allocation concealment. It was not possible to blind the participants or the carers. The investigator who was in charge of outcome assessment and the statistician were not blinded to allocation. Another trial (Shen 2012) is awaiting assessment for inclusion.
Comparator
Midodrine is a vasopressor/antihypotensive agent with an action on the alpha‐adrenoceptors of the arteriolar and venous vasculature, producing an increase in vascular tone and elevation of blood pressure. It is not licensed for the treatment of SUI.
Location/setting
The trial was held in China.
Sample size
The trial enrolled 60 women and the sample size calculation was not reported.
Length of treatment
The length of treatment was 6 to 12 weeks.
Follow‐up and outcomes
The trial made assessments at the end of treatment but no follow‐up assessment was reported. Reported outcome measures included perception of cure and improvement in continence.
Excluded studies
We excluded 20 studies: 6 studies compared one type of acupuncture therapy versus another type; or there were 7 studies with several interventions in the treatment group or the control group, or both. Of the 20 studies, two compared acupuncture plus another therapy versus therapy alone. We excluded these trials, as the effect of acupuncture could not be assessed.
Risk of bias in included studies
Allocation
We judged randomisation concealment to be inadequate (high risk of bias).
Blinding
As the trial intervention was acupuncture and the comparator a drug, blinding of participants or doctors was not possible.
Incomplete outcome data
The trial reported no withdrawals or dropouts, and all participants completed the trial.
Selective reporting
We found no selective reporting.
Other potential sources of bias
The trial did not describe the statistics adequately and the trial was small.
Effects of interventions
Acupuncture versus placebo or no treatment
We found no trials.
Acupuncture versus active treatment
The one small included trial compared electroacupuncture versus a drug (midodrine) (Bi 2007).
Acupuncture seemed to be better than the drug alone in terms of number of women improved (73% with acupuncture versus 33% with midodrine; RR 2.20, 95% CI 1.27 to 3.81; Analysis 2.1; Figure 2), but not for cure rates (13% with acupuncture versus 7% with midodrine; RR 2.00, 95% CI 0.40 to 10.11; Analysis 2.2; Figure 3).
2.1. Analysis.
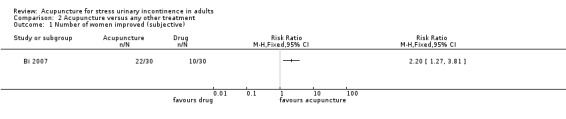
Comparison 2 Acupuncture versus any other treatment, Outcome 1 Number of women improved (subjective).
2.
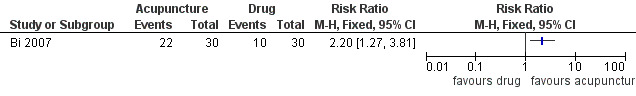
Forest plot of comparison: 2 Acupuncture versus any other treatment, outcome: 2.1 Number of women improved (subjective).
2.2. Analysis.
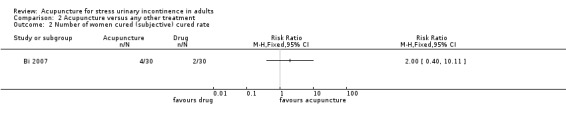
Comparison 2 Acupuncture versus any other treatment, Outcome 2 Number of women cured (subjective) cured rate.
3.
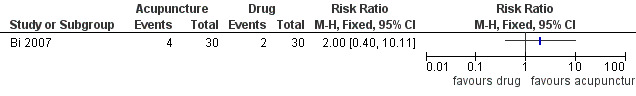
Forest plot of comparison: 2 Acupuncture versus any other treatment, outcome: 2.2 Number of women cured (subjective) cured rate.
The trial reported 23 adverse events (such as headache, dizziness and thirst) in the drug group compared with no adverse events in the acupuncture group.
There was no information about whether the effects of acupuncture persisted after the end of the course of treatment, as there was no follow‐up.
Discussion
Summary of main results
We identified 22 eligible trials but only one small trial met our inclusion criteria (Bi 2007). This was a small trial with 60 women, which compared acupuncture versus a drug midodrine. Acupuncture seemed to result in a higher improvement rate than the drug but few women were cured in either group and there was no statistically significant difference in the cure rate.
We classified one trial as awaiting assessment (Shen 2012), and we excluded 20 trials. The excluded trials in this review included comparisons of acupuncture with no treatment, drug, PFMT and another kind of acupuncture. In some trials, the interventions of the treatment group were acupuncture combined with foot massage, Chinese herb decoction or PFMT. However, none of them could be included because they were not randomised controlled trials or because acupuncture was combined with another treatment.
Overall completeness and applicability of evidence
The included trial does not provide enough evidence to assess the effects of acupuncture for SUI in adults.
Quality of the evidence
It is a randomised controlled trial with small sample size and no randomisation concealment or blind assessment of outcome. The results reported only numbers of participants cured/improved. The quality of the study was low and, therefore, the risk of bias was high.
The trial was at high risk of bias for randomisation procedure as there was no concealment of allocation, although a random number table was used to generate the randomised sequence. The author of this trial provided this information.
Because of the nature of acupuncture as an intervention, it was not possible to blind the participants or acupuncturists to the actual treatments received. This trial did not undertake blind assessments of outcome and allocation concealment. It did not provide a description of the statistical analysis used.
Potential biases in the review process
We considered there to be no potential biases in the review process.
Agreements and disagreements with other studies or reviews
We found no disagreements with other studies or reviews.
Authors' conclusions
Implications for practice.
The available data were too few to suggest that acupuncture is useful in the treatment of stress urinary incontinence compared with a drug (midodrine) and the cure rate was low.
Implications for research.
There are many acupuncture trials of stress urinary incontinence published in Chinese but their quality is not satisfactory. Larger randomised controlled trials of high quality are needed. Trials should use standardised methods of randomisation and adequate blinding of collection of outcome measures. In particular, trials should use standardised outcomes, such as validated questionnaires to assess participant's views of their incontinence and quality of life, pad tests of quantified leakage, volume of urine loss, total and mean number of pads, urodynamics, and objective failure rates after treatment and at follow‐up. Trials of acupuncture for male stress incontinence are rare and could be considered in future.
Acknowledgements
The author of one trial provided information about the randomisation process (Bi 2007).
Appendices
Appendix 1. Search terms used for the literature search
Cochrane Incontinence Group Specialised Register
The terms used to search the Cochrane Incontinence Group Specialised Register were:
(({DESIGN.CCT*} OR {DESIGN.RCT*}) AND {TOPIC.URINE.INCON*} AND ({INTVENT.PHYS.ACUPUNCTURE*} OR {INTVENT.COMPLEMENTARY.ACUPUNCTURE*}))
(All searches were of the keyword field of Reference Manager 12, Thomson Reuters). Date of last search: 28 January 2013.
Other sources:
Searches were run by the review authors for this review in: EMBASE, AMED, Chinese Biomedical Literature Database (CBM), Chinese Acupuncture Trials Register and China National Knowledge Infrastructure (CNKI). The search terms used were:
TOPIC.incontinence
and INTVENT. acupuncture /needling
and DESIGN clinical trials
In some Chinese databases, there are no randomised controlled trial or controlled clinical trial choices in the DESIGN section, so we used the term 'clinical trials'. The search date was 20 February 2013.
Data and analyses
Comparison 2. Acupuncture versus any other treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women improved (subjective) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Number of women cured (subjective) cured rate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bi 2007.
| Methods | Design: randomised controlled trial Allocation concealment: no Blinding procedures: no blinding Duration: 6‐12 weeks Follow‐up: no follow‐up Withdrawal/dropouts: none Intention‐to‐treat: yes |
|
| Participants | 60 women Inclusion criteria: stress urinary incontinence Exclusion criteria: no Mean age: 52.8 years |
|
| Interventions | A (30 women): electroacupuncture B (30 women): midodrine hydrochloride |
|
| Outcomes | Subjective cure rate: A) 13.3%, B) 6.7% Subjective improved rate: A) 73.3%, B) 33.3% Adverse effects: A 0/30, B 23/30 (headache, dizziness and thirst) |
|
| Notes | Small sample size | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | High risk | No concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No incomplete data |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Unclear risk | Small sample size |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bi 2011 | The intervention was warm acupuncture combined with foot massage and pelvic floor muscle training |
| Chen 2003 | Acupuncture versus another type of acupuncture |
| Chen 2010 | Acupuncture combined with treatment A versus acupuncture combined with treatment B |
| Gao 2011 | The intervention was acupuncture combined with another treatment |
| He 2011 | Not a randomised controlled trial |
| Jung 2008 | Some important data were absent |
| Le 2008 | Acupuncture combined with treatment B versus treatment B combined with C |
| Ni 2008 | Acupuncture plus herb, moxibustion and PFMT versus drug plus PFMT |
| Shang 2010 | Acupuncture compared with another kind of acupuncture |
| Sun 2011 | The intervention was acupuncture combined with another treatment |
| Tang 2009 | Acupuncture plus moxibustion and PFMT versus PFMT |
| Wang 2006 | Acupuncture compared with another kind of acupuncture |
| Xiong 2005 | Acupuncture plus PFMT versus herb |
| Yang 2004 | Acupuncture compared with another type of acupuncture |
| Yang 2008 | Not a randomised controlled trial |
| Yang 2010 | Acupuncture compared with another type of acupuncture |
| Yang B 2010 | Not a randomised controlled trial |
| Yang T 2004 | Acupuncture compared with another type of acupuncture |
| Yue 2008 | Acupuncture compared with another type of acupuncture |
| Zheng 1992 | Not a randomised controlled trial. Acupuncture compared with another type of acupuncture |
PFMT: pelvic floor muscle training.
Characteristics of studies awaiting assessment [ordered by study ID]
Shen 2012.
| Methods | Design: randomised controlled trial Allocation concealment: no Blinding procedures: no blinding Duration: 5‐7 days Follow‐up: no follow‐up Withdrawal/dropouts: none Intention‐to‐treat: yes |
| Participants | 120 men Inclusion criteria: transurethral resection of the prostate Exclusion criteria: yes Mean age: not reported |
| Interventions | A (30 men): electroacupuncture B (30 men): tolterodine tartrate C (30 men): electroacupuncture and tolterodine tartrate D (30 men): control (pethidine and anisodamine if necessary) |
| Outcomes | Bladder contraction: A) 0.58 (24 h); 1.82 (24‐48 h); 1.15 (48‐72 h) B) 0.59 (24 h); 1.80 (24‐48 h); 1.13 (48‐72 h) C) 0.46 (24 h); 1.55 (24‐48 h); 0.82 (48‐72 h) D) 0.76 (24 h); 2.82 (24‐48 h); 2.76 (48‐72 h) Bladder contraction duration: A) 6.81 (24 h); 7.65 (24‐48 h); 6.89 (48‐72 h) B) 6.54 (24 h); 7.27 (24‐48 h); 6.43 (48‐72 h) C) 5.43 (24 h); 4.40 (24‐48 h); 3.88 (48‐72 h) D) 8.46 (24 h);9.83 (24‐48 h); 10.87 (48‐72 h) Adverse effects: no |
| Notes |
Contributions of authors
All authors contributed to the writing of this review.
Yang Wang initiated the study and drafted the review. She unified differences of opinion and conducted quality assessment.
Weina Peng and Zhishun Liu provided methodological perspectives, quality assessment or data extraction.
Jie Zhao searched for trials, extracted and analysed data.
Baoyan Liu assessed the methodological quality of eligible trials.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Science and Technology Support Program, China.
The 'Twelfth Five‐Year Plan' of National Science and Technology Support Program, China
-
The National Institute for Health Research, UK.
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Incontinence Group.
Declarations of interest
None declared.
New
References
References to studies included in this review
Bi 2007 {published data only}
- Bi W. Clinical study on electroacupuncture treatment of female stress incontinence [电针治疗女性压力性尿失禁]. Cinese Archives of Traditional Chinese Medicine 2007;25(6):1284‐5. [Google Scholar]
References to studies excluded from this review
Bi 2011 {published data only}
- Bi K, Chi X, Song C. Warm acupuncture combined with foot massage and pelvic floor training for stress incontinence. [温针灸配合足底反射区按摩及盆底肌肉训练治疗压力性尿失禁的疗效观察]. International Journal of Traditional Chinese Medicine 2011;33(3):251‐3. [Google Scholar]
Chen 2003 {published data only}
- Chen Y‐L, Chen G‐M, Ge L‐B. Effect of acupuncture different points on unstable bladder. Journal of Acupuncture and Tuina Science 2003;1(3):22. [Google Scholar]
Chen 2010 {published data only}
- Chen L. Moxibustion with salt combined with electroacupuncture for female stress incontinence [隔盐灸加电针治疗女性压力性尿失禁]. Journal of External Therapy of TCM 2010;20(6):36‐7. [Google Scholar]
Gao 2011 {published data only}
- Gao X, Zhang L, Dong S, Xing Y. Medium frequency electro stimulant therapy combined with acupuncture for female stress incontinence [中频电刺激联合针刺治疗女性压力性尿失禁]. Journal of China Traditional Chinese Medicine Information 2011;3:200. [Google Scholar]
He 2011 {published data only}
- He Z, Li X. Electroacupuncture for mild and moderate female stress incontinence. [电针治疗女性中轻度压力性尿失禁]. Xinjiang Journal of Traditional Chinese Medicine 2011;29(1):19‐21. [Google Scholar]
Jung 2008 {published data only}
- Jung HK. Randomized control trial of hand acupuncture for female stress urinary incontinence. Acupuncture and & Electro‐therapeutics Research 2008;33:179‐92. [DOI] [PubMed] [Google Scholar]
Le 2008 {published data only}
- Le X, Wu H, Wang R. Clinical study of the treatment of female stress incontinence by combined electroacupuncture and pelvic floor muscle exercises [电针配合盆底肌锻炼治疗女性压力性尿失禁疗效观察]. Shanghai J Acu‐Mox 2008;27(10):18‐9. [Google Scholar]
Ni 2008 {published data only}
- Ni Y, Zhou Y. Needling at Baihui combined with Buzhong Yiqiwan for stress incontinence after childbirth. [针灸百会加补中益气丸治疗女性产后压力性尿失禁]. Chinese Community Doctors 2008;24:38. [Google Scholar]
Shang 2010 {published data only}
- Shang Y, Wang Z, Zhang Y, Jin C, Li X. Clinical observation of scalp and body acupuncture for 42 cases of female stress incontinence [头部透刺配合体针治疗42例女性压力性尿失禁的临床观察]. China's Naturopathy 2010;18(7):15. [Google Scholar]
Sun 2011 {published data only}
- Sun D, Xing Y, ZhangL, Dong S, Gao X. Acupuncture combined with low frequency electro stimulant therapy and biofeedback therapy for 32 cases of female stress incontinence. [针刺联合低频电刺激与生物反馈治疗女性压力性尿失禁32例]. Journal of China Traditional Chinese Medicine Information 2011;3(6):136. [Google Scholar]
Tang 2009 {published data only}
- TangCL, Dai DC, Zhu WF, Jin YY, Mei LF, Zhao GF. Observation on the therapeutic effect of dog‐day acupuncture and moxibustion combined with pelvic floor muscle exercises for treatment of female stress urinary incontinence. [三伏针灸联合盆底肌训练治疗女性压力性尿失禁疗效观察]. Chinese Acupuncture and Moxibustion 2009;29(11):879‐82. [PubMed] [Google Scholar]
Wang 2006 {published data only}
- Wang S, Chen G, Li L. 'Four sacral needles' therapy for female stress incontinence. [“骶四针”疗法治疗女性压力性尿失禁]. Shanghai Journal of Acupuncture and Moxibustion 2006;25(5):13‐5. [Google Scholar]
Xiong 2005 {published data only}
- Xiong X, Yao Q, Bi L, Yan B. Electroacupuncture combined with pelvic floor muscle training for stress incontinence [电针结合盆底肌肉锻炼治疗压力性尿失禁疗效观察]. Chinese Journal of Physical Medicine and Rehabilitation 2005;27(7):432‐3. [Google Scholar]
Yang 2004 {published data only}
- Yang P. Therapeutic effect of warming acupuncture‐moxibustion plus TDP radiation on stress urinary incontinence [温针灸加TDP照射治疗压力性尿失禁疗效观察]. Chinese Acupuncture and Moxibustion 2004;24(7):459‐60. [Google Scholar]
Yang 2008 {published data only}
- Yang J, Guo X, Yang J. Acupuncture and foot massage for 68 cases of female stress incontinence [针灸和足疗治疗女性压力性尿失禁68例]. Journal of the Fourth Military Medical University 2008;29(20):1850. [Google Scholar]
Yang 2010 {published data only}
- Yang X, Liang Y, Lu L. Clinical observation and nursing of warm acupuncture for stress incontinence. [温针灸治疗压力性尿失禁的疗效观察与护理]. Modern Nurses 2010;5:41. [Google Scholar]
Yang B 2010 {published data only}
- Yang BS, Ye DW, Yao XD, Peng JY, Zhang SL, Dai B, et al. The study of electrical acupuncture stimulation therapy combined with pelvic floor muscle therapy for postprostatectomy incontinence. Chung‐Hua Wai Ko Tsa Chih 2010;48(17):1325‐7. [PubMed] [Google Scholar]
Yang T 2004 {published data only}
- Yang T, Zhou, Zhao K. Electroacupuncture for female stress incontinence [电针治疗女性压力性尿失禁临床研究]. Journal of Sichuan of Traditional Chinese Medicine 2004;22(6):90‐1. [Google Scholar]
Yue 2008 {published data only}
- Yue J, Deng H, Zheng F. Electroacupuncture and warm acupuncture for female stress incontinence [电针加温和灸治疗女性压力性尿失禁临床观察]. Shandong Journal of Traditional Chinese Medicine 2008;27(10):688‐9. [Google Scholar]
Zheng 1992 {published data only}
- Zheng H, Sun Y, Xu Z, Hou M. Flow dynamics of urine in female patients with stress urinary incontinence treated by acupuncture and moxibustion. International Journal of Clinical Acupuncture 1992;3:243‐7. [Google Scholar]
References to studies awaiting assessment
Shen 2012 {published data only}
- Shen YZ, Lin X, Lin Q. Overactive bladder after transurethral resection of prostate treated with electroacupuncture therapy and tolterodine. Chinese Acupuncture and Moxibustion 2012;32(5):404‐8. [PubMed] [Google Scholar]
Additional references
Abrams 2002
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function. Report from the standardisation sub‐committee of the International Continence Society. Neurology and Urodynamics 2002;21(2):167‐78. [DOI] [PubMed] [Google Scholar]
Börgermann 2010
- Börgermann C, Kaufmann A, Sperling H, Stohrer M, Rubben H. The treatment of stress incontinence in men: part 2 of a series of articles on incontinence. Deutsches Arzteblatt International 2010;107(27):484‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2012
- Campbell SE, Glazener CMA, Hunter KF, Cody JD, Moore KN. Conservative management for postprostatectomy urinary incontinence. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD001843.pub4; CD001843] [DOI] [PubMed] [Google Scholar]
Ding 1992
- Ding G‐D. Collation and Explanation on Zhubing Yuanhoulun [Treatise on Causes and Symptoms of Diseases]. Beijing: People's Medical Publishing House, 1992. [Google Scholar]
Duckett 2007
- Duckett JR, Vella M, Kavalakuntla G, Basu M. Tolerability and efficacy of duloxetine in a nontrial situation. BJOG : an International Journal of Obstetrics and Gynaecology 2007;114(5):543‐7. [DOI] [PubMed] [Google Scholar]
Dumoulin 2010
- Dumoulin C, Hay‐Smith J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD005654.pub2] [DOI] [PubMed] [Google Scholar]
Gao 2002
- Gao X‐Y. Acupuncture Dictionary of China. 1. Zhengzhou: Henan Science and Technology Press, 2002. [Google Scholar]
Ge 2009
- Ge J, Lu Y‐X. Prevalence and impact on life quality of female urinary incontinence in China. Capital Journal of Public Health 2009;3(6):273‐6. [Google Scholar]
Hampel 2004
- Hampel C, Artibani W, Espuna Pons M, Haab F, Jackson S, Romero J, et al. Understanding the burden of stress urinary incontinence in Europe: a qualitative review of the literature. European Urology 2004;46(1):15‐27. [DOI] [PubMed] [Google Scholar]
Haylen 2010
- Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourology and Urodynamics 2010;29(1):4‐20. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S(editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from: www.cochrane‐handbook.org.
Hino 2010
- Hino K, Honjo H, Nakao M, Kitakoji H. The effects of sacral acupuncture on acetic acid‐induced bladder irritation in conscious rats. Urology 2010;75(3):730‐4. [DOI] [PubMed] [Google Scholar]
Hinoul 2009
- Hinoul P, Roovers J‐P, Ombelet W, Vanspauwen R. Surgical management of urinary stress incontinence in women: a historical and clinical overview. European Journal of Obstetrics, Gynecology and Reproductive Biology 2009;145(2):219‐25. [DOI] [PubMed] [Google Scholar]
Hunter 2007
- Hunter KF, Moore KN, Glazener CMA. Conservative management for postprostatectomy urinary incontinence. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD001843.pub3] [DOI] [PubMed] [Google Scholar]
Kim 2008
- Kim JH, Nam D, Park MK, Lee ES, Kim SH. Randomized control trial of hand acupuncture for female stress urinary incontinence. Acupuncture and Electro‐Therapeutics Research 2008;33(3‐4):179‐92. [DOI] [PubMed] [Google Scholar]
Langevin 2001
- Langevin HM, Churchill DL, Cipolla MJ. Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB Journal 2001;15(12):2275‐82. [DOI] [PubMed] [Google Scholar]
Lim 1995
- Lim FK, Razvi K, Tham KF, Ratnam SS. Current approach to the management of urinary stress incontinence. Singapore Medical Journal 1995;36(5):532‐7. [PubMed] [Google Scholar]
Luber 2004
- Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Reviews in Urology 2004;6 Suppl 3:S3‐9. [PMC free article] [PubMed] [Google Scholar]
Mariappan 2005
- Mariappan P, Alhasso AA, Grant A, N'Dow JMO. Serotonin and noradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004742.pub2] [DOI] [PubMed] [Google Scholar]
Miller 2007
- Miller D. Office management of stress incontinence: current and future role. Clinical Obstetrics and Gynecology 2007;50(2):376‐82. [DOI] [PubMed] [Google Scholar]
Ogah 2009
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006375.pub2] [DOI] [PubMed] [Google Scholar]
Peng 2007
- Peng WN, Zhao H, Liu ZS, Wang S. Acupuncture for vascular dementia. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD004987.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reynolds 2011
- Reynolds WS, Dmochowski RR, Penson DF. Epidemiology of stress urinary incontinence in women. Current urology reports 2011;12(5):31‐322. [DOI] [PubMed] [Google Scholar]
Rogers 2008
- Rogers RG. Urinary stress incontinence in women. New England Journal of Medicine 2008;358(10):1029‐36. [DOI] [PubMed] [Google Scholar]
Thomas 2009
- Thomas LH, Cross S, Barrett J, French B, Leathley M, Sutton CJ, et al. Treatment of urinary incontinence after stroke in adults. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD004462.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vella 2008
- Vella M, Duckett J, Basu M. Duloxetine 1 year on: the long‐term outcome of a cohort of women prescribed duloxetine. International Urogynecology Journal and Pelvic Floor Dysfunction 2008;19(7):961‐4. [DOI] [PubMed] [Google Scholar]
Wang 2003
- Wang B. Huangdi Neijing [Huang Di's Canon of Medicine]. 1st Edition. Beijing: Publishing House of Ancient Chinese Medical Books, 2003. [Google Scholar]
Wilson 1996
- Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. British Journal of Obstetrics and Gynaecology 1996;103(2):154‐61. [DOI] [PubMed] [Google Scholar]
Wu 2007
- Wu JM, Visco AG. Weidner AC, Meyers ER. Is Burch colposuspension ever cost‐effective compared with tension‐free vaginal tape for stress incontinence?. American Journal of Obstetrics and Gynecology 2007;197(1):62.e1‐5. [DOI] [PubMed] [Google Scholar]
Xu 2002
- Xu H‐Z. Acupuncture and Moxibustion. Beijing: People's Medical Publishing House, 2002. Chinese. [Google Scholar]


