Abstract
Background
This study aimed to evaluate the effectiveness of conservative treatment in selected patients with atraumatic medial sesamoid pain (MSP) that developed during sports activities. The secondary aim was to determine the detailed underlying pathology in patients who did not respond to conservative treatment using magnetic resonance imaging (MRI).
Methods
From March 2015 to August 2022, we prospectively followed 27 patients who presented to our outpatient clinic with atraumatic sports-related MSP. The conservative treatment protocol for MSP included the use of oral analgesics, activity restriction, insole modification, local corticosteroid injections, and boot walker application with crutches. MRI was performed for all patients who experienced persistent pain despite the completion of conservative treatment.
Results
After the completion of the conservative treatment protocol, 48.1% of the patients reported a reduction in pain. Patients with younger age at pain onset (p = 0.001), higher body mass index (p = 0.001), and a bipartite medial sesamoid (p = 0.010) were more likely to experience persistent pain after conservative treatment. The type of sports activity was also a factor since running- and dancing-related MSP tended to respond better to conservative treatment compared to MSP originating from golf, futsal, and weightlifting with squatting. On MRI, 42.8% of patients showed no specific abnormal findings, with signal changes in soft tissues such as the subcutaneous fat and bursa being the most common, followed by intraosseous signal changes of the medial sesamoid bone and chondral or subchondral lesions of the medial sesamoid metatarsal joint (28.6% each).
Conclusions
Conservative treatment was successful in less than half of the patients who experienced MSP due to sports activity. Practitioners should be aware of the numerous possible causes of conservative treatment failure, such as bursitis, medial sesamoiditis, stress fracture, or chondral lesions between the medial sesamoid and metatarsal. MRI evaluation may be helpful in MSP patients who do not respond to conservative treatment.
Keywords: Conservative treatment, Forefoot, Medial sesamoid pain, Medial sesamoiditis, Medial sesamoid osteochondritis
Medial sesamoid pain (MSP) is an irritating and debilitating medical condition that typically occurs during the toe-off phase of gait.1,2) It is commonly associated with traumatic events, such as hyperextension injury of the first metatarsophalangeal (MTP) joint, fractures of the medial sesamoid bone, or damage to the plantar capsuloligamentous complex (turf toe), as it lies directly under the first metatarsal head. Conversely, MSP can be a chronic and atraumatic problem associated with repetitive axial loading in the plantar or dorsiflexed position of the first MTP joint.1,3) In this situation, several pathologic conditions may be hidden, such as bursitis around the medial sesamoid bone, medial sesamoid stress fracture,4,5) osteoarthritis, osteochondritis of the medial sesamoid-first metatarsal (mSM) joint,6) avascular osteonecrosis (AVN),7,8) or medial sesamoiditis.2)
To date, the results of conservative treatment for MSP arising without specific traumatic events have not been well established as they have not been widely studied. In this study, we specifically focused on atraumatic unilateral MSP that occurs during certain sports activities, as we have encountered difficulties in treating these patients at the outpatient clinic of our institution due to a lack of relevant studies. Therefore, we aimed to determine the effectiveness of conservative treatment by applying a uniform conservative treatment protocol to a group of selected MSP patients and determining the number of patients who responded to each treatment modality. Furthermore, we examined the nature of the medial sesamoid bone and its surrounding anatomy by performing magnetic resonance imaging (MRI) on patients in whom the conservative treatment had failed.
METHODS
Ethical Considerations
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Institutional Ethics Review Committee of Inje University Ilsan Paik Hospital (IRB No. 2023-03-016). Written informed consent was obtained from all enrolled patients.
Patient Selection
In this study, we prospectively followed patients who presented with pain around the medial sesamoid bone resulting from sports activities without a specific traumatic event between March 2015 and August 2022. We enrolled participants who met the following inclusion criteria: (1) a certain sports enthusiasm with repetitive training (2 or more times per week) and (2) individuals who developed pain without any specific acute traumatic event around the forefoot during sports activities. The exclusion criteria were as follows: (1) individuals who showed moderate to severe arthritic changes of the first MTP joint on radiographs; (2) individuals with systemic inflammatory diseases such as rheumatoid arthritis or gout; (3) individuals with a previous history of bony or soft-tissue trauma that could have affected foot alignment; and (4) individuals with MSP that developed from a specific traumatic event.
Initial Evaluation, Conservative Treatment Protocol, and Judgment of Treatment Success
Initially, a thorough physical examination was conducted to diagnose MSP. MSP was diagnosed by the presence of pain when the medial sesamoid bone was pressed directly. Maximally dorsiflexing the first MTP can be helpful in accurately identifying the tender point. Radiographic evaluation was performed at the first visit, including standing foot anteroposterior and lateral views, as well as a sesamoid axial view using the apparatus developed by Suzuki et al.,9,10) which simulates the heel-off to toe-off motion that occurs during walking.
Conservative treatment was initiated immediately after MSP diagnosis and involved 3 weeks of activity restriction, oral nonsteroidal anti-inflammatory drugs, and wearing stiffened offloading insoles to limit the bending motion of the MTP joint. If the initial conservative treatment failed, a local injection of triamcinolone (40 mg) mixed with 1% lidocaine (1 mL) was administered around the medial sesamoid bone under ultrasound guidance coupled with maintenance of the initial conservative treatment modality. If the pain persisted for 3 weeks after the injection, another injection with the same agents was attempted at a 3-week interval (maximally 3 times, including the first injection) when the patient agreed. If the pain was still unacceptable after the third injection or if the patient did not agree to the injection, we recommended the application of a boot walker for 3 weeks to limit the ankle and MTP joint motion. During the boot walker application period, the patients were advised to use crutches and avoid bearing weight on their forefoot (to practice a heel gait). This regimen would require a minimum of 12 weeks and up to a maximum of 18 weeks if all 3 injections are administered to the patient. If the injection was performed once or twice, activity restriction, oral painkillers, and insole modification were continued after the boot walker application until 3 months from the commencement of the initial conservative treatment. Treatment success was evaluated by assessing patient satisfaction with pain relief following the completion of conservative treatment. In patients who did not respond to conservative treatment, continuation of activity limitation, occasional use of painkillers, and insoles were recommended. During this period, operative treatment (medial sesamoidectomy) was recommended for patients who did not respond to conservative treatment and when the MRI results showed definite abnormal findings. The final interview was performed approximately 6 months from the onset of pain through phone calls or outpatient clinic visits. We specifically focused on the existence of the remaining MSP in sports or daily activities.
Assessments
First, we collected demographic data, including age at pain onset, sex, body mass index (BMI), and affected side (right or left) from the medical records of the patients. We also gathered information about sports activities that caused MSP. Additionally, we used objective clinical measures such as the visual analog scale (VAS; 0, no pain; 10, maximal pain), Foot and Ankle Ability Measure (FAAM)-activities of daily living (ADL), and Sports subscales11,12) to assess the clinical outcomes of the patients at the initial visit and after the completion of the conservative treatment protocol.
Radiographic evaluations were performed to determine whether the patient had a bipartite medial sesamoid13) and to assess the degree of hallux valgus and pes planus or cavus. The hallux valgus angle (HVA), first to second intermetatarsal angle (IMA), talo-first metatarsal angle (Meary’s angle), and calcaneal pitch angle (CPA) were measured. The position of the medial sesamoid was evaluated using 2 different methods: Hardy and Clapham’s method in the standing foot anteroposterior view9) and the Choi et al.’s method in the sesamoid axial view.14) These radiographic parameters were measured by 2 orthopedic surgeons (JYC and THS). To determine interobserver reliability and intraobserver reproducibility, all cases were reviewed twice, with a 2-month interval between readings. Intraclass correlation coefficients were used for data analysis.
Finally, MRI was performed for all patients who experienced persistent pain despite the completion of conservative treatment. The purpose of MRI was to determine the nature of the medial sesamoid and surrounding structures. We specifically focused on 3 aspects: (1) intraosseous signal changes of the medial sesamoid, (2) chondral or subchondral lesions on the mSM joint, and (3) signal changes in soft tissues, including subcutaneous fat and the intermetatarsal or adventitial bursa.
Statistical Analyses
Descriptive statistics were performed using SPSS version 21 (IBM Corp.) to calculate the means and standard deviations of all dependent parameters. Data normality was assessed using the Kolmogorov-Smirnov test. Patients were categorized into 2 groups based on the success of conservative treatment: group 1, which had persistent pain despite conservative treatment; and group 2, which had pain relief after conservative treatment. The Mann-Whitney U-test was used to compare continuous numeric parameters between the 2 groups, while the chi-square test was used to compare proportional parameters. Statistical significance was set at p < 0.05. Additionally, we calculated an appropriate effect size for the Mann-Whitney U-test using the formula, (r, effect size; z, the standardized test statistic; n, the number of pairs).
RESULTS
Characteristics of Included Patients in This Study
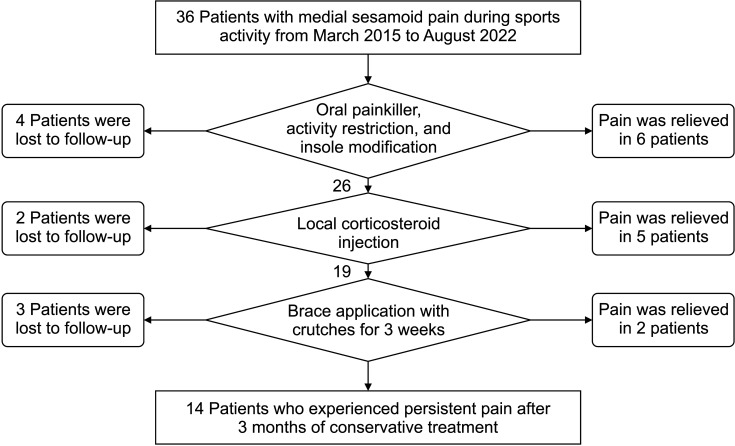
During the study period, 36 patients were initially enrolled; however, only 27 patients completed the conservative treatment protocol and were included in this study (Fig. 1). Patient characteristics are summarized in Table 1, showing a mean age of 40.0 years and mean BMI of 24.5 kg/m2. MSP during sports activity was more prevalent in men (77.8%), and pain developed regardless of foot dominance (15 of 27 patients [55.6%] experienced pain in the non-dominant feet). Running was the most common cause of MSP (29.6%), followed by golf, weightlifting with squatting, dancing (18.5% each), and futsal (indoor soccer, 14.9%). Radiographically, a bipartite medial sesamoid on the affected side was observed in 33.3% of the patients (9/27). The mean HVA and IMA did not meet the criteria for hallux valgus deformity, and the mean Meary’s angle and CPA were within normal ranges. The medial sesamoid was mostly located in an appropriate position without lateral subluxation on either the standing foot anteroposterior view or the sesamoid axial view. The mean initial VAS, FAAM-ADL, and FAAM sports scores were 8.3, 51.9, and 14.7, respectively.
Fig. 1. A structured treatment algorithm used in this study and the number of patients who responded to each treatment modality.
Table 1. Patient Characteristics.
| Characteristics | Value | |
|---|---|---|
| Total feet (patients) | 27 Feet (27) | |
| Age at pain onset (yr) | 40.0 ± 11.5 (24 to 67) | |
| Male : female (% of women) | 21 : 6 (22.2) | |
| Body mass index (kg/m2) | 24.5 ± 2.4 (20.2 to 28.9) | |
| Side (right : left) | 12:15 | |
| Related sports activity | ||
| Running | 8 (29.6) | |
| Golf | 5 (18.5) | |
| Weightlifting with squatting | 5 (18.5) | |
| Sports dancing | 5 (18.5) | |
| Futsal | 4 (14.9) | |
| Bipartite medial sesamoid on radiographs | 9 (33.3) | |
| HVA (°) | 12.6 ± 7.3 (4.8 to 23.4) | |
| IMA (°) | 9.6 ± 2.0 (7.0 to 12.0) | |
| Meary’s angle (°) | 0.5 ± 10.8 (–23.5 to 11.6) | |
| CPA (°) | 25.7 ± 5.1 (15.0 to 32.4) | |
| Medial sesamoid position by Hardy and Clapham on anteroposterior foot radiographs9) | ||
| 1 | 12 (44.4) | |
| 2 | 6 (22.2) | |
| 3 | 5 (18.5) | |
| 4 | 4 (14.8) | |
| 5, 6, 7 | 0 | |
| Medial sesamoid position by Choi et al. on forefoot axial radiographs14) | ||
| 1 | 19 (70.4) | |
| 2 | 8 (29.6) | |
| 3 | 0 | |
| Initial VAS score | 8.3 (6 to 10) | |
| Initial FAAM-ADL score | 51.9 (42 to 63) | |
| Initial FAAM-Sports score | 14.7 (12 to 21) | |
Values are presented as mean ± standard deviation (range), number (%), or mean (range).
HVA: hallux valgus angle, IMA: intermetatarsal angle, CPA: calcaneal pitch angle, VAS: visual analog scale, FAAM: Foot and Ankle Ability Measure, ADL: activities of daily living.
The statistical results of interobserver reliability and intraobserver reproducibility for 2 radiographic parameters are presented in the Supplementary Table 1.
Group Comparison According to the Treatment Success
After the completion of conservative treatment, pain reduction was achieved in 48.1% of the patients (13/27 patients). A comparison between groups 1 and 2 (Table 2) showed that younger age at pain onset (p = 0.001), higher BMI (p = 0.001), and a more frequent occurrence of bipartite medial sesamoid (p = 0.010) were notable characteristics of patients who continued to experience pain after conservative treatment. Furthermore, MSP related to running tended to respond well to conservative treatment (8 of 13 patients [61.5%] experienced pain relief after conservative treatment). Among several radiographic parameters, only the Meary’s angle demonstrated a statistically significant difference between the 2 groups (p = 0.010), with group 1 exhibiting a more pronounced cavus deformity compared to group 2. The final VAS was significantly lower in group 2, while FAAM-ADL and FAAM-Sports scores were significantly greater in group 2 (all p < 0.05).
Table 2. Patient Characteristics and MRI Findings of Patients with Persistent Pain after Conservative Treatment.
| Characteristics | Group 1: persistent pain after the conservative treatment (n = 14) | Group 2: relieved pain after the conservative treatment (n = 13) | p-value | |
|---|---|---|---|---|
| Age at pain onset (yr) | 33.2 ± 7.2 (24 to 40) | 47.5 ± 10.8 (38 to 67) | 0.001 | |
| Male : female (% of women) | 11 : 3 (21.4) | 10 : 3 (23.1) | 0.892 | |
| Side (right : left) | 5 : 9 | 7 : 6 | - | |
| Body mass index (kg/m2) | 26.3 ± 1.6 (23.8 to 28.9) | 22.9 ± 1.8 (20.2 to 25.7) | 0.001 | |
| Related sports activity | Weightlifting with squatting: 5 (35.7), futsal: 4 (28.6), golf: 4 (28.6), sports dancing: 1 (7.1) | Running: 8 (61.5), sports dancing: 4 (30.8), golf: 1 (7.7) | - | |
| Bipartite medial sesamoid on radiographs | 7 (50.0) | 2 (16.7) | 0.010 | |
| HVA (°) | 12.0 ± 7.6 (4.8 to 19.2) | 13.0 ± 7.3 (7.8 to 23.4) | 0.648 | |
| IMA (°) | 9.5 ± 2.6 (7.0 to 12.0) | 9.6 ± 1.4 (8.3 to 11.4) | 0.856 | |
| Meary’s angle (°) | 4.9 ± 10.1 (–4.7 to 14.4) | –4.7 ± 9.8 (–11.6 to 23.5) | 0.010 | |
| CPA (°) | 26.2 ± 4.7 (21.7 to 30.6) | 25.3 ± 5.6 (15.0 to 32.4) | 0.778 | |
| Medial sesamoid position by Hardy and Clapham on anteroposterior foot radiographs9) | - | |||
| 1 | 9 (77.6) | 3 (23.1) | ||
| 2 | 0 | 6 (46.2) | ||
| 3 | 5 (22.4) | 0 | ||
| 4 | 0 | 4 (30.7) | ||
| Medial sesamoid position by Choi et al. on forefoot axial radiographs14) | - | |||
| 1 | 9 (64.3) | 9 (69.2) | ||
| 2 | 5 (35.7) | 4 (30.8) | ||
| 3 | 0 | 0 | ||
| Final VAS score | 6.7 (5 to 9) | 2.3 (1 to 5) | 0.010 | |
| Final FAAM-ADL score | 52.1 (42 to 64) | 73.4 (68 to 79) | 0.001 | |
| Final FAAM-Sports score | 14.3 (11 to –22) | 26.6 (23 to 32) | 0.005 | |
| MRI findings | - | |||
| Nonspecific | 6 (42.8) | NA | ||
| mSM joint chondral defect | 4 (28.6) | |||
| Intra-osseous signal change | 4 (28.6) | |||
Values are presented as mean ± standard deviation (range), number (%), or mean (range).
MRI: magnetic resonance imaging, HVA: hallux valgus angle, IMA: intermetatarsal angle, CPA: calcaneal pitch angle, VAS: visual analog scale, FAAM: Foot and Ankle Ability Measure, ADL: activities of daily living, NA: not applied, mSM: medial sesamoid-first metatarsal.
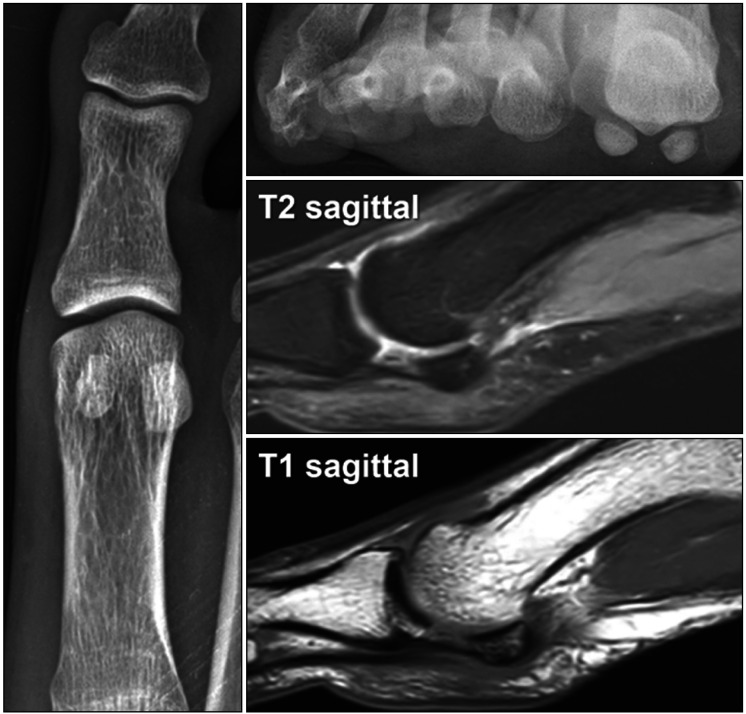
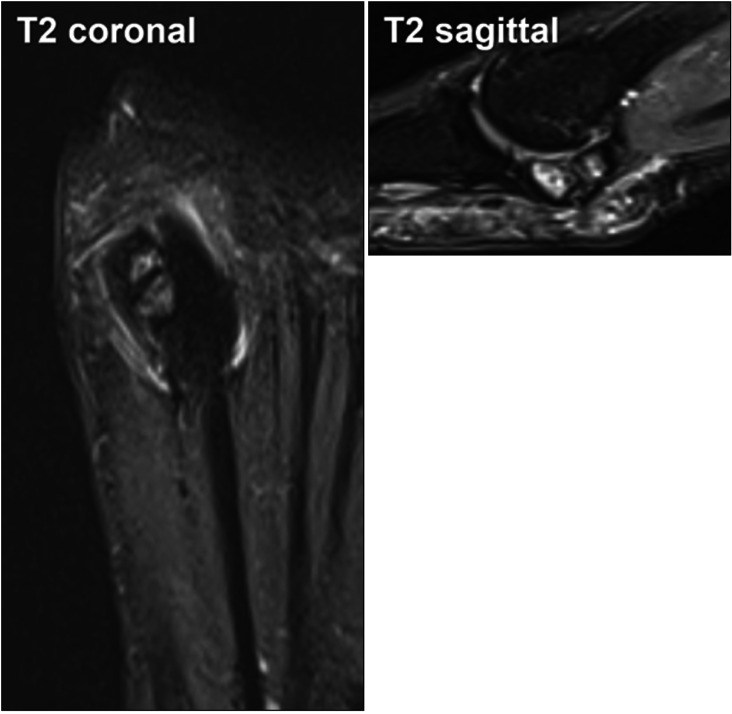
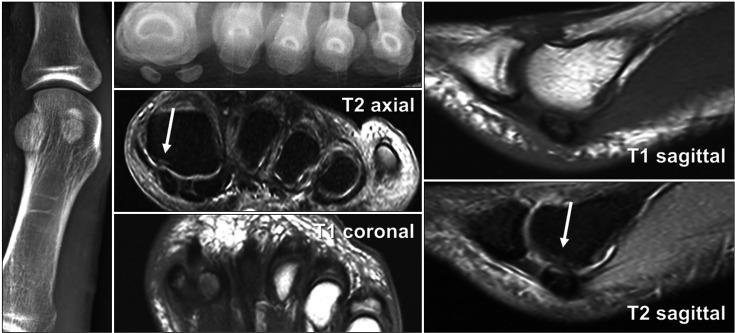
The MRI evaluation in group 1 showed that 42.8% of the patients (6/14) had nonspecific abnormalities (signal changes in soft tissues, such as subcutaneous fat and bursa) (Fig. 2). Four patients (28.6%) showed intraosseous signal changes (low on T1 and high on T2) in the medial sesamoid bone (Fig. 3), and chondral or subchondral lesions of the mSM joint were observed in the remaining 4 patients (Fig. 4).
Fig. 2. In 42.8% of the patients who did not respond to conservative treatment (6 / 14), no discernible pathological abnormalities were observed except for signal changes in soft tissues, such as subcutaneous fat and bursa.
Fig. 3. Intraosseous signal changes of the medial sesamoid bone were observed in 28.6% of the patients with persistent pain after completing the treatment protocol.
Fig. 4. A male patient, 43 years of age, who continued to experience medial sesamoid pain after conservative treatment, exhibited a subchondral signal change adjacent to the medial sesamoid bone with a cartilage defect in the first metatarsal bone (indicated by arrows).
After the completion of conservative treatment, medial sesamoidectomy was performed in only 1 patient in group 1, who showed an intraosseous signal change in the medial sesamoid bone. The final interview at 6 months was successfully completed by 12 and 11 patients in groups 1 and 2, respectively. The status of MSP with regard to sports or daily activities is summarized in Table 3. Notably, 3 patients in group 1, who were able to participate in sports but experienced mild post-activity pain, were those whose MRI findings showed no discernible pathological abnormalities except for signal changes in soft tissues. The effect size calculation for the difference in ΔFAAM-ADL between the 2 groups was calculated as 0.639, implying a more than medium effect size (> 0.5).
Table 3. Number of Patients Categorized According to the Nature of Pain and with Regard to Sports or Daily Living Activities at the Final Interview (around 6 Months after Pain Onset).
| Characteristics | Group 1 (n = 12) | Group 2 (n = 11) |
|---|---|---|
| Ability to attain prior level of sports activity without pain | 0 | 5 (45.4) |
| Possible to participate in sports, but experiencing mild post-sports MSP | 3 (25) | 4 (36.4) |
| Able to perform activities of daily living, but experiencing MSP during sports activities and unable to engage in sports | 5 (41.7) | 2 (18.2) |
| Experiencing residual MSP during activities of daily living | 4 (33.3) | 0 |
Values are presented as number (%).
Group 1: persistent pain after 3 months of conservative treatment, Group 2: relieved pain after 3 months of conservative treatment, MSP: medial sesamoid pain.
DISCUSSION
Our study found that conservative treatment was effective in only 48.1% of patients who experienced sports-related MSP. The conservative treatment protocols used in this study included oral analgesics, activity restriction, insole modification, local corticosteroid injections, and boot walker application. Notably, our data revealed that younger age at pain onset, higher BMI, and a more frequent occurrence of bipartite medial sesamoid were significant findings in patients who did not respond to conservative treatment compared to those who experienced pain reduction. Through MRI evaluations, we found that less than half of the patients who did not respond to conservative treatment had no specific abnormal findings, except for signal changes in the surrounding soft tissues, while 57.2% of these patients had significant pathological findings. Of the pathological MRI findings, signal changes in the medial sesamoid bone itself and chondral/subchondral lesions around the mSM joint occurred in equal proportions (28.6% each).
The term “sesamoid” refers to the shape of the bone resembling sesame seeds. The 2 sesamoids of the great toe (medial and lateral) are contained within the flexor hallucis brevis tendon and are connected to the plantar aspect of the proximal phalanx through the plantar plate. The function of these sesamoids consists of reducing friction at the first MTP joint, cushioning the first MTP joint, and increasing the plantar flexion moment of the first MTP joint during the toe-off phase of gait.15) Furthermore, it should be emphasized that the healing process of any kind of sesamoid injury might be delayed or halted because the blood supply from the first plantar artery can be tenuous to the distal sesamoids.16,17,18)
Based on the results of this study, practitioners may consider possible pathologic conditions that lead to a failure of the conservative treatment, including bursitis around the medial sesamoid bone, medial sesamoid stress fracture, osteoarthritis, or osteochondritis of the mSM joint, AVN, and medial sesamoiditis. In this context, we aimed to thoroughly analyze our MRI data. For patients who did not respond to conservative treatment, the most remarkable MRI findings were the intraosseous signal change of the medial sesamoid (low in T1 and high in T2), interpreted as fluid collection inside the bone, which implied sesamoiditis, osteomyelitis, or a possible stress fracture. Regarding stress fractures, the medial sesamoid is at risk of stress-related injury because of its location under the first metatarsal head, its larger size, and its biomechanical function.15,19,20) Richardson21) insisted that sesamoid stress fractures were more common than acute fractures and occurred most commonly in long-distance running and sports requiring rapid acceleration and deceleration.
Furthermore, medial sesamoiditis can be caused by repetitive stress on the great toe during sports activities and may be a source of pain. Players can acquire it from over-practicing movements that transfer weight to the padded portion of the sole between the toes and the arch underneath the heads of the metatarsal bones. Sugimoto et al.22) reported that hallucal sesamoiditis was the most common, followed by stress and acute sesamoid fracture by reviewing the medical chart of 683 young athletes with sesamoid injury. In our clinical experience, it was difficult to distinguish stress fractures from medial sesamoiditis when medial sesamoiditis was combined with bipartite sesamoid and so the operative treatment should be carefully considered in these situations.
Our data emphasize the importance of osteochondral lesions of the mSM joint23) as a possible cause of atraumatic MSP related to sports activities. In general, the mSM joint osteochondral lesion or osteoarthritis is believed to be related to severe hallux valgus24) and the lateral subluxation of the medial sesamoid on forefoot axial radiographs in hallux valgus patients.14) Other studies25,26) have insisted that severe trauma and prior stress fracture would be related to mSM osteochondral lesions, although the true etiology remains unclear. Unlike osteochondral lesions related to hallux valgus, the mean HVA and IMA of our patients were within the normal range, and the position of the medial sesamoid was medial to the intersesamoid ridge in all cases. Therefore, we reiterate that the osteochondral lesion of the mSM joint related to sports activities might have a different disease mechanism (repetitive stress in a certain position) from that of hallux valgus patients (malposition of the medial sesamoid bone); therefore, greater attention to these aspects would be highly recommended for practitioners.26)
Importantly, AVN of the medial sesamoid might also be considered a potential cause of persistent pain after conservative treatment, although we could not find any of these cases in this study. AVN of the hallucal sesamoid bones is a rare diagnosis and can be derived from isolated vascular perfusion deficit or mechanical overload or caused secondary to acute fracture.7) Stress fracture with subsequent nonunion might also evolve into avascular necrosis.7) Changes that are visible on plain radiographs are often delayed so that bone scintigraphy, computed tomography, or MRI would be more useful as a diagnostic tool. In cases with AVN, MRI will show low signal intensity on both T1- and T2-weighted images of the affected sesamoid bone as fibrous tissue replaces fat and hematopoietic tissue.27) Given the low prevalence of AVN, the success rate of conservative treatment for AVN is unknown.7)
Another novel finding of our present study is that 42.8% of MSP patients refractory to conservative treatment showed no significant abnormal findings on the medial sesamoid itself but showed signal changes in the surrounding soft tissues. These signal changes in the soft tissues might be either a result of prior local steroid injection or remaining inflammatory changes, such as bursitis. Furthermore, inflammation of peritendinous structures caused by the overuse of tendons that interact with the hallux sesamoid bones can persist. For these patients, we recommend observation without operative treatment, as we have found that the symptoms are alleviated slowly over a period of 6 months without further intervention.
Additionally, alternative conservative treatment options may include other injectional agents (i.e., platelet-rich plasma,3) intra-articular hyaluronic acid, or polydeoxyribonucleotide28)), custom orthotics (Morton’s extension or cut-out over the medial sesamoid), or extracorporeal shock waves.29) Future studies including these options with a large number of patients would help determine the best treatment combination for intractable MSP.
Lastly, the results of this study indicated that patients with persistent pain even after conservative treatment had a greater Meary’s angle compared to those whose pain was relieved through conservative treatment. In other words, we can hypothesize that a higher arch caused by pes cavus may increase the pressure on the medial sesamoid, making pain relief more difficult to achieve. Additionally, it is also possible that the presence of first-ray hypermobility may influence the occurrence of MSP, even among patients with similar degrees of foot arch. Whilst the importance of first-ray hypermobility has been extensively discussed in conditions such as hallux valgus and metatarsalgia,30,31,32) its association with MSP warrants further investigation in future studies including pedobarography.
The current study is subject to several limitations, notably a limited sample size, a significant number of excluded participants, a wide variety of sports activities leading to MSP, no assessment of ankle and first MTP joint range of motion as well as first ray hypermobility, and the lack of MRI evaluations conducted before starting conservative treatment. Comparing the MRI findings between groups 1 and 2 would have provided more detail on the causative factors that reduce the efficacy of conservative treatment. Furthermore, comparing the outcomes of conservative treatment with those of early surgical treatment could have provided more clinically meaningful data. Nevertheless, to our knowledge, this is the first study to determine the effectiveness of conservative treatment for MSP using a uniform treatment protocol for a group of selected patients along with MRI evaluations in the treatment failure group.
In conclusion, a conservative treatment protocol, including oral painkillers, activity restriction, insole modification, local corticosteroid injections, and boot walker application, was effective in less than half of the patients who experienced MSP during sports activities. Surgeons should be aware of numerous possible causes of the treatment failure, such as soft-tissue inflammation around the medial sesamoid, stress fracture, medial sesamoiditis, osteoarthritis/osteochondral lesion of the mSM joint, or AVN so that the MRI evaluation might be helpful. We found that less than half of the patients who did not respond to conservative treatment had nonspecific abnormalities (signal changes in soft tissues, such as subcutaneous fat and bursa), whereas 57.2% of these patients had significant pathological findings.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
SUPPLEMENTARY MATERIAL
Supplementary material is available in the electronic version of this paper at the CiOS website, www.ecios.org.
Statistics for Interobserver Reliability and Intraobserver Reproducibility in the 27 Patients
References
- 1.Chan BY, Markhardt BK, Williams KL, Kanarek AA, Ross AB. Os conundrum: identifying symptomatic sesamoids and accessory ossicles of the foot. AJR Am J Roentgenol. 2019;213(2):417–426. doi: 10.2214/AJR.18.20761. [DOI] [PubMed] [Google Scholar]
- 2.Sims AL, Kurup HV. Painful sesamoid of the great toe. World J Orthop. 2014;5(2):146–150. doi: 10.5312/wjo.v5.i2.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le HM, Stracciolini A, Stein CJ, Quinn BJ, Jackson SS. Platelet rich plasma for hallux sesamoid injuries: a case series. Phys Sportsmed. 2022;50(2):181–184. doi: 10.1080/00913847.2021.1964006. [DOI] [PubMed] [Google Scholar]
- 4.Bichara DA, Henn RF, Theodore GH. Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int. 2012;33(9):704–706. doi: 10.3113/FAI.2012.0704. [DOI] [PubMed] [Google Scholar]
- 5.Robertson GA, Goffin JS, Wood AM. Return to sport following stress fractures of the great toe sesamoids: a systematic review. Br Med Bull. 2017;122(1):135–149. doi: 10.1093/bmb/ldx010. [DOI] [PubMed] [Google Scholar]
- 6.Perez Carro L, Echevarria Llata JI, Martinez Agueros JA. Arthroscopic medial bipartite sesamoidectomy of the great toe. Arthroscopy. 1999;15(3):321–323. doi: 10.1016/s0749-8063(99)70043-5. [DOI] [PubMed] [Google Scholar]
- 7.Bartosiak K, McCormick JJ. Avascular necrosis of the sesamoids. Foot Ankle Clin. 2019;24(1):57–67. doi: 10.1016/j.fcl.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Shin EH, Kwon WH, Dujela MD, Kim BS. Arthroscopic synovectomy and excision of a sesamoid in the management of an atypical presentation of avascular necrosis of bone: a case report. J Foot Ankle Surg. 2020;59(3):594–597. doi: 10.1053/j.jfas.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 9.Hardy RH, Clapham JC. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 1951;33(3):376–391. doi: 10.1302/0301-620X.33B3.376. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki J, Tanaka Y, Takaoka T, Kadono K, Takakura Y. Axial radiographic evaluation in hallux valgus: evaluation of the transverse arch in the forefoot. J Orthop Sci. 2004;9(5):446–451. doi: 10.1007/s00776-004-0800-9. [DOI] [PubMed] [Google Scholar]
- 11.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 12.Saarinen AJ, Uimonen MM, Suominen EN, Sandelin H, Repo JP. Structural and construct validity of the Foot and Ankle Ability Measure (FAAM) with an emphasis on pain and functionality after foot surgery: a multicenter study. J Foot Ankle Surg. 2022;61(4):872–878. doi: 10.1053/j.jfas.2021.12.011. [DOI] [PubMed] [Google Scholar]
- 13.Favinger JL, Porrino JA, Richardson ML, Mulcahy H, Chew FS, Brage ME. Epidemiology and imaging appearance of the normal Bi-/multipartite hallux sesamoid bone. Foot Ankle Int. 2015;36(2):197–202. doi: 10.1177/1071100714552484. [DOI] [PubMed] [Google Scholar]
- 14.Choi JY, Ahn HC, Baek HS, Park JH, Suh JS. Factors influencing medial sesamoid arthritis in patients with hallux valgus deformity: magnetic resonance imaging evaluation. Foot Ankle Surg. 2019;25(5):612–617. doi: 10.1016/j.fas.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 15.Kane JM, Brodsky JW, Daoud Y. Radiographic results and return to activity after sesamoidectomy for fracture. Foot Ankle Int. 2017;38(10):1100–1106. doi: 10.1177/1071100717717265. [DOI] [PubMed] [Google Scholar]
- 16.Chamberland PD, Smith JW, Fleming LL. The blood supply to the great toe sesamoids. Foot Ankle. 1993;14(8):435–442. doi: 10.1177/107110079301400802. [DOI] [PubMed] [Google Scholar]
- 17.Pretterklieber ML, Wanivenhaus A. The arterial supply of the sesamoid bones of the hallux: the course and source of the nutrient arteries as an anatomical basis for surgical approaches to the great toe. Foot Ankle. 1992;13(1):27–31. doi: 10.1177/107110079201300105. [DOI] [PubMed] [Google Scholar]
- 18.Rath B, Notermans HP, Frank D, et al. Arterial anatomy of the hallucal sesamoids. Clin Anat. 2009;22(6):755–760. doi: 10.1002/ca.20843. [DOI] [PubMed] [Google Scholar]
- 19.Biedert R, Hintermann B. Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int. 2003;24(2):137–141. doi: 10.1177/107110070302400207. [DOI] [PubMed] [Google Scholar]
- 20.Peng J, He JK, Christie M, et al. Tibial sesamoidectomy: indications and outcomes. Ann Joint. 2019;4(4):48 [Google Scholar]
- 21.Richardson EG. Injuries to the hallucal sesamoids in the athlete. Foot Ankle. 1987;7(4):229–244. doi: 10.1177/107110078700700405. [DOI] [PubMed] [Google Scholar]
- 22.Sugimoto D, Gearhart MG, Kobelski GP, Quinn BJ, Geminiani ET, Stracciolini A. Hallux sesamoid injury characteristics in young athletes presented to the sports medicine clinic. Clin J Sport Med. 2022;32(3):e276–e280. doi: 10.1097/JSM.0000000000000902. [DOI] [PubMed] [Google Scholar]
- 23.Kliman ME, Gross AE, Pritzker KP, Greyson ND. Osteochondritis of the hallux sesamoid bones. Foot Ankle. 1983;3(4):220–223. doi: 10.1177/107110078300300408. [DOI] [PubMed] [Google Scholar]
- 24.Doty JF, Coughlin MJ, Schutt S, et al. Articular chondral damage of the first metatarsal head and sesamoids: analysis of cadaver hallux valgus. Foot Ankle Int. 2013;34(8):1090–1096. doi: 10.1177/1071100713481461. [DOI] [PubMed] [Google Scholar]
- 25.Garrido IM, Bosch MN, Gonzalez MS, Carsi VV. Osteochondritis of the hallux sesamoid bones. Foot Ankle Surg. 2008;14(4):175–179. doi: 10.1016/j.fas.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Richardson EG. Hallucal sesamoid pain: causes and surgical treatment. J Am Acad Orthop Surg. 1999;7(4):270–278. doi: 10.5435/00124635-199907000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Toussirot E, Jeunet L, Michel F, Kantelip B, Wendling D. Avascular necrosis of the hallucal sesamoids update with reference to two case-reports. Joint Bone Spine. 2003;70(4):307–309. doi: 10.1016/s1297-319x(03)00061-7. [DOI] [PubMed] [Google Scholar]
- 28.Lee DO, Yoo JH, Cho HI, Cho S, Cho HR. Comparing effectiveness of polydeoxyribonucleotide injection and corticosteroid injection in plantar fasciitis treatment: a prospective randomized clinical study. Foot Ankle Surg. 2020;26(6):657–661. doi: 10.1016/j.fas.2019.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Thompson D, Malliaropoulos N, Padhiar N. Sesamoid osteonecrosis treated with radial extracorporeal shock wave therapy. BMJ Case Rep. 2017;2017:bcr2017219191. doi: 10.1136/bcr-2017-219191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Biz C, Maso G, Malgarini E, Tagliapietra J, Ruggieri P. Hypermobility of the first ray: the Cinderella of the measurements conventionally assessed for correction of hallux valgus. Acta Biomed. 2020;91(4-S):47–59. doi: 10.23750/abm.v91i4-S.9769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glasoe WM. An operational definition of first ray hypermobility. Foot Ankle Spec. 2022;15(5):494–496. doi: 10.1177/19386400221093864. [DOI] [PubMed] [Google Scholar]
- 32.Singh D, Biz C, Corradin M, Favero L. Comparison of dorsal and dorsomedial displacement in evaluation of first ray hypermobility in feet with and without hallux valgus. Foot Ankle Surg. 2016;22(2):120–124. doi: 10.1016/j.fas.2015.05.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Statistics for Interobserver Reliability and Intraobserver Reproducibility in the 27 Patients