Summary
Background
Approximately 20% of adults in Vietnam have hypertension, and management of this chronic condition remains challenging. This study aimed to assess the effectiveness of a multicomponent intervention in reducing blood pressure (BP) in adults with uncontrolled hypertension.
Methods
This cluster randomised controlled trial was conducted in sixteen communities (8 intervention and 8 comparison) in a rural setting in Vietnam (2017–2022). Consenting adults (aged ≥ 18 years) with uncontrolled hypertension were enrolled. Sixteen communities were equally randomised to an intervention or comparison group stratified by district. Consenting adults were assigned to study groups by community. The comparison arm received training sessions about hypertension prevention and management for health workers, and patient education materials. The intervention arm received training sessions about hypertension prevention and management for health workers, and patient education materials and three enhancement components including a storytelling intervention, home BP self-monitoring, and expanded community health worker services. The primary outcome was the difference in changes in patient's levels of systolic BP between the study groups over a 12-month follow-up period. Patients and outcome assessors were masked.
Findings
A total of 671 patients (340: intervention, 331: comparison) were enrolled in the trial. The mean age was 66 years and 45% were men. At the 12-month follow-up, the mean systolic BP declined by 18.4 mmHg in the intervention group and 3.7 mmHg in the comparison group (differential decline of 14.7 mmHg [95% CI: 11.8–17.6]). The intervention group also achieved better BP control and medication adherence than the comparison group. There were no serious adverse events related to study participation.
Interpretation
The results of this trial demonstrate that a multicomponent intervention can effectively reduce elevated BP in individuals with uncontrolled hypertension in Vietnam. Trial registration: This trial was registered at ClinicalTrials.gov, NCT03590691.
Funding
National Heart, Lung, and Blood Institute.
Keywords: Hypertension, Storytelling, Home blood pressure monintoring, Community health worker, Vietnam, Clinical trial
Research in context.
Evidence before this study
Vietnam is undergoing an epidemiological transition with the morbidity and mortality from non-communicable diseases having risen rapidly over the last several decades. This transition can be attributed to changes in population size, socio-demographic characteristics, and increases in life expectancy. Cardiovascular disease (CVD) is now the leading cause of death in Vietnam, accounting for 30% of all deaths annually in 2010. Major risk factors for CVD including hypertension, diabetes, unhealthy dietary practices, and overweight/obesity are either on the rise or at alarming levels in Vietnam. National data showed that the prevalence of hypertension was more than 40% for those 50–69 years old and the general population consumed high levels of sodium in their diet in 2016. Although anti-hypertensive medications are off-patent, widely available across the country, and are covered by public health insurance, the awareness and management of hypertension is far from optimal; this is due to many factors including lack of regular screening and patient self-management strategies (e.g., medication adherence, lifestyle modifications). Inasmuch, the burden of CVD will continue to increase in the Vietnamese population unless effective prevention and control measures are put in place.
Added value of this study
The results of this community-based trial provide important insights into the effectiveness and implementation of a multicomponent intervention in reducing elevated levels of systolic and diastolic blood pressure (PB) among adult Vietnamese men and women with uncontrolled hypertension. Although the intervention produced statistically significant reductions in participant's BP, the proportion of hypertensive patients whose BP was controlled, even in the intervention arm, was sub-optimal.
Implications of all the available evidence
To date published community-based interventions to improve hypertension control are still limited. Our intervention shows promise, but more work needs to be done to improve its effectiveness and more widespread dissemination. Additional work should be done to determine how the intervention components used in the present trial could be intensified or combined in a more optimal manner. Other community-based strategies for hypertension control in Vietnam are still needed.
Introduction
Vietnam has experienced a recent increase in the magnitude of, and mortality from, non-communicable diseases due to longer life expectancy, economic development, and increased urbanization.1,2 Non-communicable diseases now account for a significant percentage of all deaths in Vietnam, with cardiovascular disease being the leading cause of these deaths.1,3 High blood pressure is one of the primary risk factors for cardiovascular disease,4 and a recent systematic review and meta-analysis of ten studies published between 2005 and 2018 estimated that one in every five adults in Vietnam has hypertension,5 a prevalence estimate which is consistent with the results of three national surveys in this low to middle income country (LMIC).5 Despite the affordability and widespread availability of anti-hypertensive agents, managing hypertension in Vietnamese adults remains a considerable challenge due to low levels of awareness, less than optimal medication adherence, and failure to change adverse lifestyle practices.6
Storytelling has been identified as a promising and innovative intervention for promotion positive health behavior change among adults with chronic disease, especially for individuals with uncontrolled hypertension, that is adaptable to different communities and cultures.7,8 Our study team had previously conducted a feasibility trial in Hung Yen province, Vietnam which demonstrated that a storytelling intervention successfully reduced elevated levels of systolic blood pressure and improved medication adherence among Vietnamese adults with high blood pressure.9
Recent studies have also highlighted the positive impact of community health workers in improving blood pressure control by promoting home blood pressure monitoring and emphasizing the importance of medication adherence, making healthy lifestyle changes, and connecting patients with community health centres.10,11 Self-management strategies, such as home blood pressure monitoring, have also been shown to positively impact the control of elevated blood pressure.12,13
Building upon our earlier study findings,9 we conducted a cluster randomised controlled clinical trial of 671 adults residing in 16 rural communities in Hung Yen province of Northern Vietnam to assess the effectiveness and implementation outcomes at patient level of these three intervention modalities, namely storytelling, home blood pressure monitoring, and expansion of community health workers for managing high blood pressure among Vietnamese adults with uncontrolled hypertension.
Methods
Study design and participants
This cluster randomised controlled trial (RCT) was conducted in patients with uncontrolled hypertension in Vietnam. We selected the cluster RCT design to minimize individual-level contamination since several of the components of the intervention were delivered at community level. All study personnel and collaborating investigators were carefully trained in specific aspects of the study protocol and in conducting standardized measurement procedures, as described in detail previously.14 The protocol for this trial and supporting CONSORT checklist are included in Appendix 1.
The present study was conducted in Hung Yen province (2017–2022), which has a population of approximately 1.3 million (rural population: 83%) and is organized into 10 districts and 161 communities. A total of 16 eligible communities in 4 districts in Hung Yen province were randomly assigned to either an intervention (n = 8) or a comparison group (n = 8). Each of the selected communities satisfied the following criteria: (1) had a community health centre with a medical doctor; (2) were not currently participating in other studies of hypertension control; and (3) had a minimum geographic separation of 12 km (seven miles) from all other study communities to minimize possible contamination between the intervention and comparison sites.
Patient inclusion criteria
As previously described,14 consenting adult men and women needed to fulfill each of the following criteria to be enrolled in the trial: (1) be a resident of the selected community and have no plans for moving during the 12 months after trial enrollment; (2) be aged 25 years or older, a cutoff which is commonly used in population-based surveillance studies of hypertension in Vietnam6; (3) have a diagnosis of uncontrolled hypertension according to the 8th Joint National Commission of High Blood Pressure (JNC 8)15; (4) not be cognitively impaired (as assessed by study physicians); (5) not be a “storyteller” used to develop the intervention; (6) not be a family member of another participant in the study; and (7) not be pregnant.
Screening events to identify community residents satisfying our study eligibility criteria were conducted at participating local community health centres. Individuals diagnosed with elevated blood pressure (BP) at the time of their first clinic trial visit were invited for re-measurement of their BP over the next two weeks (a minimum of one week apart) at their local community health centre. If their average BP remained elevated (systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg) at the second screening visit, these persons were invited to participate in the trial. Trained study nurses at study sites obtained informed consent from eligible patients.
We included patients with uncontrolled hypertension (incident and prevalent cases) irrespective of whether they had received treatment for this condition. At the time of baseline study enrollment, if patients were newly diagnosed with hypertension (incident cases), they were immediately referred to their district health centres to receive prescribed anti-hypertensive medications. If they were diagnosed previously (prevalent cases) but their BP levels were still elevated (systolic BP ≥ 180 mmHg or/and diastolic BP ≥ 110 mmHg) they were referred to their district health centres to modify the treatments they were receiving as needed.
Study recruitment, randomisation and masking
The recruitment of participating communities and study subjects has been described in detail previously.14 A total of 16 communities in Hung Yen Province were randomly assigned to either the intervention or comparison condition using a computer program, stratified by district because randomisation was implemented at the community and not the patient level. In each district, two communities were randomly assigned to the intervention group and two communities were randomly assigned to the comparison group. Eligible and consenting trial participants with uncontrolled hypertension were assigned to intervention versus comparison status based on the community in which they resided. Patients and outcome assessors were masked to study group assignment. Individuals found to have elevated BP findings at the time of clinic screening and were not willing to participate in the study were referred for usual care at local district health centres. Participant recruitment was started in October 2019, and completed in April 2021.
Intervention content and delivery
The study intervention has been previously described in detail.14
Vietnam National Hypertension Program (at community level)
Both the intervention and comparison groups received the Vietnam National Hypertension Program which included several training sessions about hypertension prevention and management for physicians and nurses, and a comprehensive set of patient education materials. Two training sessions were organized in September 2019 and July 2020 for 54 physicians and nurses working at participating community health centres to update their knowledge and skills in diagnosing and treating patients with hypertension, and to provide guidance on screening, counseling, and managing patients with hypertension. Posters and leaflets providing educational information for patients to improve their hypertension control were distributed to patients at the local community health centres.
Storytelling intervention (intervention group only-at patient level)
Our team has previously designed, implemented, and pilot tested a storytelling intervention for improving hypertension control in Vietnam.9,16 The patient narratives included first-hand accounts from patients in their journey to gain control of their BP and the stories were complemented by additional formal information about how to control their high BP levels in Didactic Learn More section. We developed four digital storytelling DVDs with patient stories and a Didactic Learn More section at the end of the DVDs. The first DVD was delivered at the time of trial enrollment with viewing in the clinic, the second and third DVDs were delivered at the three- and six-month follow-up visits at their local community health centres, and the last one was delivered at the participant's home at nine months after trial enrollment. All intervention participants were provided with a DVD player and instructed in how to navigate the menu structure of the DVDs at baseline.
We developed two short DVDs with a Didactic Learn More section only for the comparison group. This included general recommendations for managing important risk factors for hypertension including the importance of having a healthy diet, quitting smoking, drinking less or no alcohol, and participation in regular physical exercise. Patients in the comparison group received a DVD player and two DVDs; the first DVD was delivered at baseline and the second DVD was provided at the six-month follow-up visit.
Home self-blood pressure monitoring (intervention group only-at patient level)
Home BP self-monitoring was the second enhancement for the intervention group who received free home Omron BP measurement devices at the time of trial enrollment. All BP measurement devices had the same calibration performed before study enrolment. A trained community health worker instructed patients on how to use the BP measurement devices at home and how to record their BP readings in a log. Readings were to be taken at least two times: in the morning after arising and again at night. Patients were advised about reading variability, cautioned about overreacting to a single elevated BP value, and given specific protocols for when to contact a health care provider should the need arise.
Expanded community health worker services (intervention group only-at community and patient levels)
A critical enhancement for the intervention group was implemented to support and strengthen the role of community health workers in motivating patients to more actively manage their hypertension through lifestyle changes and adherence to prescribed medication. We carried out a series of training sessions for community health workers which were delivered locally in collaboration with the Vietnam Ministry of Health.
Two training sessions were organized for 41 community health workers at the eight intervention communities to strengthen their motivational interviewing and structured problem solving to assist patients in setting realistic goals for several lifestyle changes, including salt and alcohol reduction, smoking cessation, increased physical activity, and enhanced medication adherence; they also developed problem-solving strategies to achieve these goals. The community health workers were taught how to use the storytelling intervention to begin conversations with their patients. After each DVD of the storytelling intervention was shown, the community health workers met with the patient to review the material, elicit possible barriers to lifestyle changes and medication treatment, and identified strategies to overcome recognized barriers. The community health workers made bi-weekly patient home visits to resolve difficulties related to viewing the DVDs and using BP measurement devices.
Follow-up activities
After obtaining informed patient consent and trial enrollment, a reminder letter was sent to all participants before each of the clinic follow-up visits. One week prior to the scheduled follow-up visit, local staff contacted study participants by phone. If patients missed their follow-up visit, local staff contacted them by phone to remind them to come into the local community health centre or visited their homes to measure their BP, if necessary. The study was paused two times due to the COVID-19 pandemic (February–April 2021 and July–October 2021), which resulted in considerable missing data at the three and six-month clinic follow-up visits.
Sample size
Detailed sample size calculations for this trial have been previously described.14 Sample size calculations were based on our primary trial hypothesis of between group differences in changes over time in systolic BP. Our previous pilot data suggests that it feasible to achieve an over-time improvement of 8 mmHg in systolic BP with a standard deviation (SD) of 18 mmHg. Pilot data revealed an intra-class correlation (ICC) of 0.011 for the clustering of patients in communities for change in systolic BP. We set alpha error at 0.05 and examined a range of power from 0.8 to 0.9 based on the two-sided t-test with a common SD of 18, assuming that the mean improvement in systolic BP is 8 mmHg for the intervention group and 3 mmHg for the comparison group. We then adjusted sample size to account for clustering and inflated the resulting sample size by approximately 10% for losses to follow-up. We arrived at a final total sample size of 671 patients which provided adequate power for testing the main study hypothesis.
Data collection
Data collection processes have been described previously.14
Blood Pressure and Anthropometric Measurements
Certified study nurses were trained to measure trial participant's BP according to a standardized protocol approved by the World Health Organization17 using Omron BP measurement device. Three measurements were separated by at least 1 min apart, and values from the last two measurements were averaged. According to Vietnam Health Ministry guidelines, patient's BP findings were classified into three categories: hypertension stage 1: systolic BP 140–159 mmHg and/or diastolic BP 90–99 mmHg; hypertension stage 2: systolic BP: 160–179 mmHg and/or diastolic BP 100–109 mmHg; and hypertension stage 3: systolic BP ≥ 180 mmHg and/or diastolic BP ≥ 110 mm Hg. Height and weight were measured in the absence of shoes and heavy clothing while waist and hip sizes were measured by placing the tape horizontally around the smallest part of the waist and the widest portion of the hips, respectively.
Participant surveys
All paper-based surveys were conducted by trained research staff. We collected information on patient's level of education, occupation, and economic circumstances using the WHO STEPs protocol which was also used to collect data on tobacco use, alcohol consumption, salt intake, and physical activity.18 Adherence to anti-hypertensive medications was measured using standardized forms.19
Post-DVD viewing interviews for both groups collected information about self-reported engagement with the DVDs, and specific segments that were viewed. Participants were asked to elaborate on what motivated/hindered their intervention engagement. At each of the follow-up interviews, participants in the intervention group were asked about how often and how confident they used their BP monitoring device and BP log at home, and how often they received consultation services from the community health workers.
Trial outcomes
The trial outcomes were at the patient level. The primary outcome was the differential change in mean systolic BP over the 12-month follow-up period for the intervention versus comparison groups. Secondary outcomes included changes in diastolic BP, proportion of patients who had their BP controlled, and extent of medication adherence at the time of the 12-month follow-up visit. Implementation outcomes were feasibility and acceptability.
Data analysis
All primary hypothesis testing was performed on an intent-to-treat basis. Data analyses were performed at the patient level. Categorical data are presented as frequency distributions and continuous variables are presented as means (standard deviation−SD). For the main study hypothesis, which was the continuous outcome of level of systolic BP (H1), we used generalized linear mixed regression models which included group assignment, time of assessment, and the interaction between study group and time to estimate changes over time in our principal study outcome, accounting for clustering of patients within the community and repeated within-person measurements by random effects. The random effect for the district was not included in the regression model due to the limited number of districts and model instability. The intervention effect was parameterized by the interaction coefficient, which represented differences in over-time change for the intervention versus comparison group. Each patient contributed data at two time points (baseline and 12 months after trial enrollment). We also used a generalized linear mixed model adjusting for potential covariate imbalances between the two primary comparison groups including age, sex, education, smoking, baseline anti-hypertensive medication use, marital status, and body mass index. For the secondary analysis, we examined differential over-time changes in diastolic BP and hypertension control using statistical approaches described above for testing the main study hypothesis. For these analyses, a dichotomous measure of BP control was constructed according to JNC-8.15 Given the importance of baseline anti-hypertensive medication use, we performed stratified analysis by this variable. We carried out exploratory analyses for possible heterogeneity of the intervention effect on the control of patient's BP at the time of the 12-month follow-up visit among patient sub-groups stratified by age (<70 vs.≥70 years), sex, stage of baseline hypertension level-commonly used in Vietnam, and presence of selected CVD comorbidities (e.g., elevated blood cholesterol, elevated blood glucose) and baseline anti-hypertensive medication use using Forest plots. These particular subgroups were selected because we wanted to observe whether there was a differential effect of the intervention in several important patient subgroups at risk for adverse health outcomes. In this paper, we focused on reporting results for the primary trial outcomes. Results from the analyses of our secondary outcomes (e.g., CVD risk factors, cost effectiveness analyses) and mediation analyses will be reported in other manuscripts. All analyses were performed using SAS 9.4 statistical software (SAS Institute Inc., Cary, NC, USA).
Ethical considerations
This randomised trial was approved by the Institutional Review Board at the Health Strategy and Policy Institute (HSPI) in Hanoi, Vietnam (Decision 171/QD-CLCSYT dated September 10, 2019). Written informed consent was obtained from all patients. This trial was registered at ClinicalTrials.gov (Registration number: NCT03590691, registration date May 31, 2018).
Role of the funding source
This funding agency had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Results
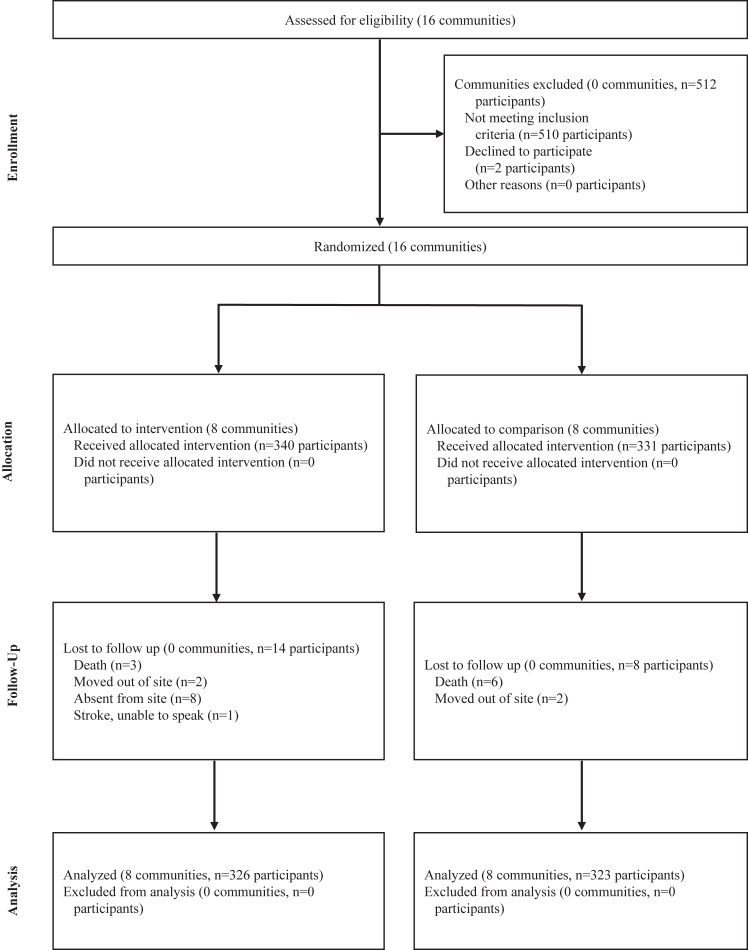
Details about the screening and follow-up process are shown in Fig. 1. A total of 671 eligible patients (340 in the intervention group and 331 in the comparison group) participated in the trial. At 12 months after trial enrollment, 97% (649 out of 671) of study patients were successfully followed up.
Fig. 1.
Consort figure- study scheme of cluster randomized controlled trial: conquering hypertension in vietnam (2017–2022).
The average age of the overall study population was 66 years, 45% were men, 11% were current smokers, and patients’ average body mass index was 23. The average baseline systolic and diastolic BP values were 161 mmHg and 92 mmHg, respectively.
Study participant characteristics
Patients in the intervention group were slightly younger, were more likely to have obtained a higher level of secondary school education and had slightly higher BP levels than those in the comparison group at the time of baseline trial enrollment. Patients in the intervention group were more likely to have elevated blood glucose findings or diabetes at baseline compared with those in the comparison group. There were no important differences in other characteristics for those randomised to either the intervention or comparison conditions at the time of trial enrollment (Table 1).
Table 1.
Baseline patient characteristics by study group: conquering hypertension in Vietnam (2017–2022).
| Intervention | Comparison | |
|---|---|---|
| Number of communities | 8 | 8 |
| Number of patients | 340 | 331 |
| Age (mean, SD, range), years | 65.7 (8.9, [38–84]) | 67.9 (9.0, [42–91]) |
| Body mass index, kg/m2 | 22.9 (3.0) | 23.1 (2.7) |
| Male (n,%) | 161 (42.6) | 141 (47.4) |
| Marital status (n,%) | ||
| Never married | 6 (1.8) | 3 (0.9) |
| Currently married | 277 (81.5) | 253 (76.5) |
| Separated/Divorced/Widowed | 57 (16.8) | 75 (22.7) |
| Level of Education (n,%) | ||
| Less than primary school | 40 (11.8) | 51 (15.5) |
| Primary school | 33 (9.7) | 48 (14.6) |
| Secondary school | 190 (55.9) | 164 (49.9) |
| High school | 43 (12.7) | 50 (15.2) |
| College/university | 34 (10.0) | 16 (4.9) |
| Work status (n,%) | ||
| Employed | 14 (4.1) | 7 (2.1) |
| Self-employed | 28 (8.2) | 14 (4.2) |
| Homemaker | 39 (11.5) | 41 (12.4) |
| Farmer | 109 (32.1) | 121 (36.6) |
| Retired | 78 (22.9) | 63 (19.0) |
| Other | 72 (21.2) | 85 (25.7) |
| Current smoker (n,%) | 105 (35.1) | 93 (31.4) |
| Self-reported cardiovascular comorbidity (n,%) | ||
| Elevated blood glucose/diabetes | 51 (15.0) | 31 (9.4) |
| Elevated blood cholesterol | 98 (28.8) | 85 (25.7) |
| Systolic blood pressure (mean, SD), mmHg | 161.8 (16.5) | 160.3 (15.2) |
| Diastolic blood pressure (mean, SD), mmHg | 92.5 (10.9) | 90.6 (11.2) |
SD: Standard deviation.
Intervention enhancement engagement and acceptability
In terms of the implementation of training activities, physicians and nurses working at participating community health centres (both intervention and control groups) stated that the study training sessions were very useful for them to update their knowledge and skills in screening, diagnosing, and treating patients with hypertension (based on our exit interviews).
With regards to enhancement of the storytelling intervention (intervention group only), the majority of patients stated that the patient stories used understandable words, attractive images, and were culturally acceptable, reliable, and encouraged patients to change their lifestyle and medication adherence habits (Table 2). With regards to the Didactic Learn More materials, the majority of patients in the comparison group stated that the materials provided were culturally acceptable and used understandable and reliable words; however, a considerable proportion of patients reported that the material was too short and they wanted more information.
Table 2.
Reports of patient acceptability and engagement for the Storytelling enhancement and Learn-more module at the 12-month clinic follow-up: conquering hypertension in Vietnam (2017–2022).
| Responses | Storytelling (Intervention group, n = 313) | Didactic (comparison group, n = 299) |
|---|---|---|
| Understandable words (n, %) | 294 (93.9) | 269 (90.0) |
| Culturally acceptable (n, %) | 298 (95.2) | 271 (90.6) |
| Reliable, (n, %) | 297 (95.2) | 274 (91.6) |
| Attractive images (n, %) | 283 (91.0) | 253 (84.6) |
| Telling story/health topic attractively (n, %) | 282 (90.4) | 282 (90.4) |
| Encouraged to change lifestyles (n, %) | 291 (93.3) | 262 (87.6) |
| Length (n, %) | ||
| Reasonable | 307 (98.4) | 241 (80.6) |
| Too long | 4 (1.3) | 3 (1.0) |
| Too short | 1 (0.3) | 55 (18.4) |
| Enough information provided (n, %) | 311 (99.7) | 264 (88.3) |
In terms of the home BP monitoring enhancement (intervention group only), almost all patients used the automated BP monitor at home, most of these individuals were confident in its usage, monitored their BP at the recommended twice a day, and used the pre-designed BP log to record their BP levels (Table 3).
Table 3.
Reports of patient acceptability and engagement for home blood pressure (BP) monitoring and expanded Community Health Workers enhancement at 12-month follow up visit (Intervention group only): conquering hypertension in Vietnam (2017–2022).
| n | % | |
|---|---|---|
| Used automated blood pressure monitor at home | 323 | 99.7 |
| Level of confidence in using BP monitor | ||
| Confident | 301 | 92.9 |
| Somewhat confident | 19 | 5.9 |
| Unconfident | 4 | 1.2 |
| Frequency of using automated blood pressure monitor | ||
| Twice a day | 270 | 83.3 |
| Once a day | 27 | 8.3 |
| 3–5 times/week | 10 | 3.1 |
| 1–3 times/week | 6 | 1.9 |
| Once a month | 11 | 3.4 |
| Used pre-designed blood pressure log | 320 | 98.9 |
| Used BP log by themselves | 279 | 86.1 |
| Frequency of using automated blood pressure log | ||
| Twice a day | 300 | 92.6 |
| Once a day | 7 | 2.1 |
| 3–5 times/week | 8 | 2.5 |
| Rarely/never | 9 | 2.8 |
| Quality of blood pressure log use (via study staff's observation) | ||
| Correct and sufficient | 186 | 58.1 |
| Insufficient | 64 | 20.0 |
| Incorrect | 34 | 10.6 |
| Insufficient and incorrect | 16 | 5.0 |
| Not using | 20 | 6.3 |
| Received extended Community Health Worker service | ||
| Home visits | 266 | 82.1 |
| Counselling via phone calls | 26 | 8.0 |
| No service | 33 | 9.9 |
With regards to the extended community health worker service enhancement (intervention group only), the community health workers provided in-person consultations for more than 80% of patients at their homes and via phone calls for 8% of patients during the study period (except during the COVID-19 pandemic when social distancing and lockdown measures were implemented) (Table 3). Community health workers commented that the study training sessions strengthened their counseling skills for patients to better manage their hypertension (exit interview).
Medication adherence
At the time of the 12-month follow-up survey at which time medication adherence was assessed, patients in the intervention group were significantly more likely to report using anti-hypertensive medications during the prior seven days compared with those who were randomly assigned to the comparison group (94% vs. 80%, p < 0.001).
Blood pressure outcomes
The average systolic and diastolic BP readings improved over time for both study groups (Table 4). However, significantly greater reductions in average blood pressure values were observed for patients in the intervention as compared with those in the comparison group (p for interaction term between study group and time <0.001) (Table 4).
Table 4.
Differential over-time change for intervention vs. comparison group (95% CIs) in blood pressure levelsa: conquering hypertension in Vietnam (2017–2022).
| Intervention | Comparison | Difference over time (95% CIs) |
||
|---|---|---|---|---|
| Unadjusted | Multivariable Adjusted | |||
| Number of communities | 8 | 8 | ||
| Number of patients | 326 | 323 | ||
| Systolic blood pressure (mean, SD) mmHg | ||||
| Baseline | 161.9 (16.6) | 160.2 (15.2) | – | – |
| 12 Months | 143.4 (13.9) | 156.5 (20.6) | – | – |
| Δ Baseline- 12 Months, mmHg | 18.4 (16.6) | 3.7 (20.8) | 14.7 (11.8–17.6) | 14.9 (8.1–21.7) |
| Diastolic blood pressure (mean, SD) mmHg | ||||
| Baseline | 92.5 (10.9) | 90.6 (11.2) | – | – |
| 12-Months | 83.6 (8.9) | 88.2 (13.1) | – | – |
| Δ Baseline- 12 Months, mmHg | 8.9 (10.4) | 2.4 (12.1) | 6.5 (4.0–9.1) | 6.2 (3.7–8.7) |
| Controlled blood pressureb(n,%) | Odds Ratio (95% CI) | |||
| 12 Months | 120 (36.8) | 58 (18.0) | 3.13 (1.35–7.25) | 3.29 (1.36–7.98) |
Results from generalized linear models that account for clustering patients within a community and repeated measures nested within patients and controlled for age, sex, education, smoking, baseline anti-hypertensive medication use, marital status, and body mass index. Intracluster correlation coefficients (ICCs) for systolic blood pressure were 0.08 and 0.122 for community and patient, respectively. ICCs for diastolic blood pressure were 0.011 and 0.36 for community and patient, respectively.
Based on guidelines from the Joint National Commission for the Management of High Blood Pressure in Adults. All patients had uncontrolled hypertension at baseline.
At the 12-month follow-up visit, patient's average systolic BP values had declined by 18.4 mmHg in the storytelling intervention group and by 3.7 mmHg in the comparison group (unadjusted difference over-time between two groups: 14.7 mmHg [95% CI: 11.8–17.6]; multivariable adjusted: 14.9 mmHg [95% CI: 8.1–21.7]). Similarly, patient's mean diastolic BP had declined by 8.9 mmHg in the intervention group and by 2.4 mmHg in the comparison group (unadjusted difference over-time between two groups: 6.5 mmHg [95% CI: 4.0–9.1]; multivariable adjusted difference: 6.2 mmHg [95% CI: 3.7–8.7]) (Table 4).
At baseline, all patients had uncontrolled BP. At the 12-month clinic follow-up visit, the proportion of patients whose BP was controlled in the intervention group was significantly higher than among those in the comparison group (37% vs. 18%). The odds for patients in the intervention group to have their BP controlled at the time of the 12-month clinic follow-up were three times greater (multivariable adjusted odds ratio (OR): 3.29 [95% CI: 1.36–7.98]) than that for those in the comparison group (Table 4).
The results of stratified analysis by baseline anti-hypertensive medication use showed that the intervention demonstrated a strong effect in reducing systolic BP pressure levels (adjusted difference over time between the two groups: 16.2 mmHg [95% CI: 9.9–22.5]) and diastolic BP levels (adjusted difference: 6.7 mmHg [95% CI: 4.3–9.1]) and in improving hypertension control among patients who were receiving medication (37.3% vs. 16.2%; p < 0.01, adjusted OR: 4.34 [95% CI: 1.35–13.99]) (Supplemental Table S1A). Similarly, the intervention demonstrated a beneficial effect among those who were not being treated with medication in reducing systolic BP pressure levels (adjusted difference: 12.8 mmHg [95% CIs: 4.4–21.2]), and diastolic BP levels (adjusted difference: 5.2 mmHg [95% CI: 1.9–8.5]) and in improving hypertension control (35.6% vs. 19.9%, p < 0.01, adjusted OR: 2.39 [95% CI: 0.89–6.41]) (Supplemental Table S1B).
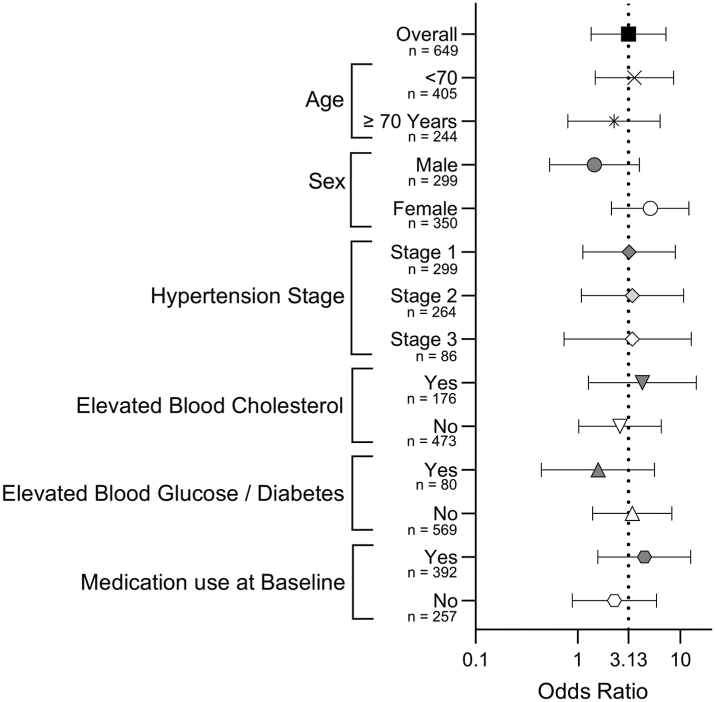
In examining possible heterogeneity of the intervention effects, we conducted several prespecified subgroup analyses for purposes of examining whether there were differences in the control of patient's hypertension at the time of the 12-month follow-up visit (Fig. 2). The forest plots suggested that there is no evidence of heterogeneity of the multi-component trial intervention.
Fig. 2.
Odds ratios (95% CI) for blood pressure control in selected subgroups: conquering hypertension in Vietnam (2017–2022).
Serious adverse events (SAEs)
During the study period, there were 3 deaths (0.9%) and 27 hospitalizations (7.9%) reported in the intervention group and 6 deaths (1.8%) and 9 hospitalizations (2.7%) in the comparison group. None of these SAEs were related to study participation.
Discussion
The results of this large clinical trial in middle-aged and older adults living in rural Northern Vietnam with uncontrolled hypertension demonstrate that a multicomponent intervention of storytelling, home BP monitoring, and expanded community health worker services can effectively reduce elevated BP in these at-risk individuals. The intervention revealed no harm to study patients.
Several multicomponent community-based interventions implemented in other LMICs have demonstrated their effectiveness in reducing patients' BP. A study in Nepal found that an educational intervention led by community health volunteers, combined with home BP monitoring, resulted in a reduction in systolic BP by almost 4 mmHg compared with a control group at a one-year follow-up.20 Similarly, a trial in Argentina21 evaluated the effectiveness of a community health worker-led home-based intervention, including text messages for promoting lifestyle changes and home BP monitoring. Patients in the intervention group experienced an average reduction of 6.6 mmHg more in their systolic BP than the control group by the 18-month follow-up visit. These results support community health worker-led multicomponent interventions for effectively lowering BP. A study conducted in Bangladesh, Pakistan, and Sri Lanka,22 which engaged government-trained community health workers to counsel patients on BP management strategies, showed a reduction in average systolic BP by more than 5 mmHg as compared with the non-intervention groups. This study and another trial from India,22,23 which used community health workers to counsel and educate patients on BP management strategies, also showed increased adherence to medications compared to the usual care groups. Similarly, home BP monitoring has also been shown to be an effective strategy for the management of hypertension.24,25 In a RCT conducted in Honduras and Mexico,26 patients in the intervention group received home BP monitoring devices and regular automated telephone reminders to check their BP, resulting in an average reduction in systolic BP by 4.2 mmHg compared with a standard care group. This modality has also been found to promote adherence to antihypertensive medication regimens.27,28 Compared with declines in BP observed in the context of other trials, the present trial demonstrated a marked decrease in systolic BP in patients who received our multifaceted intervention compared with those who received usual care. This marked reduction in BP may be attributed to several factors, including the rural setting, the inclusion of middle-aged and older participants who may be more receptive to lifestyle interventions,29,30 and the combination of culturally adaptive storytelling, home BP monitoring, and support provided by community health workers.
Storytelling is a method of communication that has been shown to be a promising intervention for controlling hypertension.8 Our storytelling intervention was adapted from a prior study conducted by our team in urban safety-net clinics in Alabama,8 and from our feasibility trial conducted in other rural communities in the same Vietnamese province, which observed similar positive results.9 Although the mechanisms for the beneficial effects of storytelling were not examined and can only be speculated upon, the use of impactful and culturally sensitive narratives has the potential to encourage patients to adhere to antihypertensive medications and adopt positive lifestyle changes, ultimately leading to improved BP control. The storytelling component was delivered via DVDs in this present study and can be easily transferred to smartphone apps as more than 80% of Vietnamese adults own a smartphone and have access to high-speed data. Thus, storytelling could be integrated into primary care settings in rural areas by employing this approach as a complementary educational tool during patient visits or as part of group education sessions.
Community health workers have long been recognized as a valuable resource in promoting healthy lifestyle practices and medication adherence, effectively controlling hypertension.10,11 Our study showed that community health workers, who are well integrated in the Vietnam healthcare system, can use the storytelling intervention to begin their conversations with patients more easily and effectively to assist patients in controlling their hypertension, an approach which has never have been implemented in Vietnam. In addition, home BP monitoring, as utilized in our intervention, may offer a cost-effective and sustainable approach to BP control, particularly in rural settings; use of this approach can be further strengthened with the guidance of community health workers who receive proper training in hypertension management.
Although the multiple intervention modalities used in the present trial produced significant reductions in systolic and diastolic BP among the intervention group as compared with the comparison group, fewer than two in every five patients in the intervention group had their hypertension controlled by the 12-month follow-up visit. Further efforts are, therefore, needed to improve hypertension control in this population. The challenge of achieving effective BP control may be attributed, in part, to the high baseline BP levels of trial participants.
Study strengths and limitations
To our knowledge, this study is the first cluster RCT to include a combination of storytelling, home BP monitoring, and expanded community health worker services to improve hypertension control in rural settings of a LMIC. The study included multiple communities in multiple distinct districts in Hung Yen province, which is a typical rural province in Northern Vietnam. Inasmuch, the findings of the study can be generalizable for residents of rural settings who are living in northern Vietnam.
Moreover, we used a longitudinal design to evaluate the effectiveness and sustainability of the intervention over one year. We adhered to rigorous and standardized methods to measure patients' BP and were able to track participants' progress with regards to their diligence in home BP monitoring, engagement with the intervention components, and adherence to prescribed antihypertensive medications.
This study also had limitations. The research was conducted in a specific province in Northern Vietnam, which may not be generalizable to other rural regions (central or southern). Furthermore, given the trial design, we could not test each intervention component separately since our focus was on evaluating the holistic effectiveness of a multi-modality intervention. This underlying premise is based on the intricate interplay of factors contributing to the control of hypertension which requires a multifaceted approach. We used the STEPS survey to obtain data for patients' socio-demographic characteristics and medical history, which could have potentially resulted in some biases in these self-reported data. The STEPS survey has, however, been used in a number of prior studies of NCDs in Vietnam and has been shown to have high reliability. Similarly, we used post-DVD viewing surveys to obtain patients’ opinions and ratings about the study storytelling intervention. This survey has been used in our previous studies in the US and Vietnam and has shown high reliability. Therefore, the magnitude of self-reporting bias is likely to be small and similar in both the intervention and comparison groups. Only 3% of patients were lost to follow-up at 12 months, and this rate did not significantly differ according to the intervention or comparison condition; inasmuch, it likely had a minimal, if any, effect on the principal study outcome. The present study was also not powered for our subgroup analyses. Finally, the follow-up period was limited to 12 months, which is not long enough to capture the long-term effects of our intervention approach on controlling patients' BP.
The results of this community-based trial provide important insights into the effectiveness and implementation of a multicomponent intervention in reducing elevated levels of systolic and diastolic BP among adult Vietnamese men and women with uncontrolled hypertension. A storytelling intervention, home BP monitoring, and expanded community health workers should be considered for integration into the revised National program for NCD prevention and control at the community level. Although the intervention produced statistically significant reductions in participant's BP, the proportion of hypertensive patients whose BP was controlled, even in the intervention arm, was sub-optimal. Therefore, our intervention shows promise, but more work needs to be done to improve its effectiveness and more widespread dissemination. Additional work should be done to determine how the intervention components used in the present trial could be intensified or combined in a more optimal manner.
Contributors
HN, DH, OT, RG, and JA conceptualized the study and obtained funding. GC, VP, GN, CN, TN and TL contributed to the study design. GC, VP, CN, GN, and TL supervised trial implementation. GC, VP, CN, GN, TN and TL supervised data collection. BW was the lead statistician and led the development of the statistical analysis plan. BW, HN and GN directly accessed and verified the underlying data reported in the manuscript and analyzed the data. HN, DH, OT, JA, RG, and BW led interpretation of the data, with support from GN, CN and ET. HN, ET and BW drafted the tables and figures, with input from GN and CN. HN, RG, GN, CN, ET, BW and JA wrote the first draft of the manuscript. HB contributed during the revision process of the manuscript. All authors reviewed the manuscript and approved the final draft. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. HN and JA have directly accessed and verified the underlying data reported in the manuscript.
Data sharing statement
De-identified participant data that were collected for this study can be obtained by contacting the corresponding author. Data with the dictionary will be made available, beginning with publication, after approval of a short proposal summarizing the analyses to be done.
Declaration of interests
We declare no competing interests.
Acknowledgements
The research reported in this article was supported by the U.S. National Heart, Lung, and Blood Institute of the National Institutes of Health under award number 1U01HL138631-01. The views expressed are those of the authors and do not necessarily represent those of the National Heart, Lung, and Blood Institute, the National Institutes of Health, the Department of Health and Human Services, or the U.S. Government.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2024.101123.
Appendix A. Supplementary data
References
- 1.Medical Statistics Yearbook 2019-2020. Ministry of Heatlh; Hanoi, Vietnam: 2021. [Google Scholar]
- 2.Vietnam Data . 2021. World bank data. [Google Scholar]
- 3.Nguyen T.T., Hoang M.V. Non-communicable diseases, food and nutrition in Vietnam from 1975 to 2015: the burden and national response. Asia Pac J Clin Nutr. 2018;27:19–28. doi: 10.6133/apjcn.032017.13. [DOI] [PubMed] [Google Scholar]
- 4.Vietnam global burden of disease study 2019 results. Institute for Health Metrics and Evaluation; 2019. [Google Scholar]
- 5.Meiqari L., Essink D., Wright P., et al. Prevalence of hypertension in Vietnam: a systematic review and meta-analysis. Asia Pac J Public Health. 2019;31:101–112. doi: 10.1177/1010539518824810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Son P.T., Quang N.N., Viet N.L., et al. Prevalence, awareness, treatment and control of hypertension in Vietnam-results from a national survey. J Hum Hypertens. 2012;26:268–280. doi: 10.1038/jhh.2011.18. [DOI] [PubMed] [Google Scholar]
- 7.Pardoel Z.E., Reijneveld S.A., Lensink R., et al. Core health-components, contextual factors and program elements of community-based interventions in Southeast Asia - a realist synthesis regarding hypertension and diabetes. BMC Publ Health. 2021;21:1917. doi: 10.1186/s12889-021-11244-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Houston T.K., Allison J.J., Sussman M., et al. Culturally appropriate storytelling to improve blood pressure: a randomized trial. Ann Intern Med. 2011;154:77–84. doi: 10.7326/0003-4819-154-2-201101180-00004. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen H.L., Ha D.A., Goldberg R.J., et al. Culturally adaptive storytelling intervention versus didactic intervention to improve hypertension control in Vietnam- 12 month follow up results: a cluster randomized controlled feasibility trial. PLoS One. 2018;13 doi: 10.1371/journal.pone.0209912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mbuthia G.W., Magutah K., Pellowski J. Approaches and outcomes of community health worker's interventions for hypertension management and control in low-income and middle-income countries: systematic review. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-053455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeet G., Thakur J.S., Prinja S., et al. Community health workers for non-communicable diseases prevention and control in developing countries: evidence and implications. PLoS One. 2017;12 doi: 10.1371/journal.pone.0180640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cappuccio F.P., Kerry S.M., Forbes L., et al. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004;329:145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Agarwal R., Bills J.E., Hecht T.J., et al. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57:29–38. doi: 10.1161/hypertensionaha.110.160911. [DOI] [PubMed] [Google Scholar]
- 14.Ha D.A., Tran O.T., Nguyen H.L., et al. Conquering hypertension in Vietnam-solutions at grassroots level: study protocol of a cluster randomized controlled trial. Trials. 2020;21:985. doi: 10.1186/s13063-020-04917-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whelton P.K., Carey R.M., Aronow W.S., et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Allison J.J., Nguyen H.L., Ha D.A., et al. Culturally adaptive storytelling method to improve hypertension control in Vietnam - "We talk about our hypertension": study protocol for a feasibility cluster-randomized controlled trial. Trials. 2016;17:26. doi: 10.1186/s13063-015-1147-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO STEPS survey. https://www.who.int/ncds/surveillance/steps/STEPS_Manual.pdf
- 18.Bonita R., De Counter M., Dwyer T., et al. Geneva: World Health Organization; Geneva: 2001. Surveillance of risk factors for noncommunicable disease: the WHO STEPwise approach. [Google Scholar]
- 19.Voils C.I., Maciejewski M.L., Hoyle R.H., et al. Initial validation of a self-report measure of the extent of and reasons for medication nonadherence. Med Care. 2012;50:1013–1019. doi: 10.1097/MLR.0b013e318269e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neupane D., McLachlan C.S., Mishra S.R., et al. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): an open-label, cluster-randomised trial. Lancet Global Health. 2018;6:e66–e73. doi: 10.1016/S2214-109X(17)30411-4. [DOI] [PubMed] [Google Scholar]
- 21.He J., Irazola V., Mills K.T., et al. Effect of a community health worker-led multicomponent intervention on blood pressure control in low-income patients in Argentina: a randomized clinical trial. JAMA. 2017;318:1016–1025. doi: 10.1001/jama.2017.11358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jafar T.H., Gandhi M., de Silva H.A., et al. A community-based intervention for managing hypertension in rural south asia. N Engl J Med. 2020;382:717–726. doi: 10.1056/NEJMoa1911965. [DOI] [PubMed] [Google Scholar]
- 23.Xavier D., Gupta R., Kamath D., et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4:244–253. doi: 10.1016/s2213-8587(15)00480-5. [DOI] [PubMed] [Google Scholar]
- 24.McManus R.J., Mant J., Haque M.S., et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312:799–808. doi: 10.1001/jama.2014.10057. [DOI] [PubMed] [Google Scholar]
- 25.Uhlig K., Patel K., Ip S., et al. Self-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysis. Ann Intern Med. 2013;159:185–194. doi: 10.7326/0003-4819-159-3-201308060-00008. [DOI] [PubMed] [Google Scholar]
- 26.Piette J.D., Datwani H., Gaudioso S., et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed J e Health. 2012;18:613–620. doi: 10.1089/tmj.2011.0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Onzenoort H.A., Verberk W.J., Kroon A.A., et al. Effect of self-measurement of blood pressure on adherence to treatment in patients with mild-to-moderate hypertension. J Hypertens. 2010;28:622–627. doi: 10.1097/HJH.0b013e328334f36b. [DOI] [PubMed] [Google Scholar]
- 28.Ralston J.D., Cook A.J., Anderson M.L., et al. Home blood pressure monitoring, secure electronic messaging and medication intensification for improving hypertension control: a mediation analysis. Appl Clin Inform. 2014;5:232–248. doi: 10.4338/ACI-2013-10-RA-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tibebu A., Mengistu D., Negesa L. Adherence to recommended lifestyle modifications and factors associated for hypertensive patients attending chronic follow-up units of selected public hospitals in Addis Ababa, Ethiopia. Patient Prefer Adherence. 2017;11:323–330. doi: 10.2147/ppa.S126382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang J., Moore L., Loustalot F., et al. Reporting of adherence to healthy lifestyle behaviors among hypertensive adults in the 50 states and the District of Columbia, 2013. J Am Soc Hypertens. 2016;10:252–262.e253. doi: 10.1016/j.jash.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.