Viruses are the most common cause of lower respiratory tract disease in infants and young children and are a major public health problem in this age group. The novel variant of coronavirus that is associated with the worldwide outbreak of severe acute respiratory syndrome and human metapneumovirus, a recently identified new respiratory pathogen, have stressed the continuing importance of viral respiratory infections over the whole age spectrum.
Costs attributable to viral lower respiratory tract infections in both outpatient and inpatient settings are an important burden on national healthcare budgets.1 Each year approximately 3% of all children less than 1 year of age need to be admitted to hospital with moderate or severe viral lower respiratory tract infection.2 This review gives an update of viral lower respiratory tract infection in infants and young children, with special emphasis on treatment and prevention.
Sources and selection criteria
We gathered information from our own experience and by reading relevant literature on viral respiratory infections in infants and children obtained by searching Medline and the Cochrane database. Much literature is available on the topic, so we based our review on well designed major observational studies, controlled trials, and systematic reviews. We consulted the websites of the World Health Organization and the Centers for Disease Control for the most recent information on severe acute respiratory syndrome.
Epidemiology
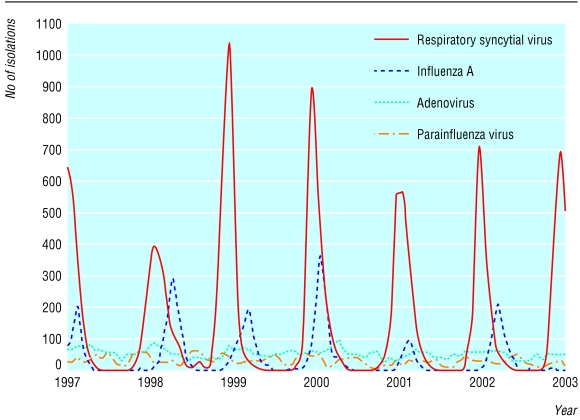
A great variety of viruses can cause lower respiratory tract disease in children—for example, respiratory syncytial virus, influenza viruses, parainfluenza viruses, rhinovirus, adenovirus, and the recently identified human metapneumovirus.3,w1,w2 Although most respiratory viral infections occur throughout the year, seasonal variation (in a worldwide comparable pattern) is obvious for certain viruses, such as respiratory syncytial virus and influenza virus (figure).
Figure 1.
Epidemiology of respiratory syncytial virus, influenza A, adenovirus, and parainfluenza virus in the Netherlands, 1997-2003
Respiratory syncytial virus and influenza viruses
Worldwide, respiratory syncytial virus is by far the most common cause of viral lower respiratory tract infection in infants and young children.4 Virtually all children have developed antibodies to respiratory syncytial virus by the age of 3 years.4 In addition, an estimated 75% of all admissions for bronchiolitis in children under 5 years of age are related to respiratory syncytial virus.3
Summary points
Respiratory syncytial virus is still by far the most common cause of viral lower respiratory tract infection in infants and children
Viral lower respiratory tract infections are self limiting in most cases, and no treatment is necessary
Passive immunisation against respiratory syncytial virus is effective in preventing admission to hospital, although there is doubt about its economic benefit
Debate is ongoing about whether influenza vaccination should be broadened to all age groups, including healthy children and adults
Development and implementation of practical guidelines and educational programmes are helpful in the control of viral lower respiratory tract infections
Influenza viruses also cause the most severe disease in the youngest age group. A recent study showed that infants and young children have a 12-fold increased risk of admission to hospital for respiratory tract infection caused by influenza virus compared with children aged 5-17 years.5
The concomitant circulation of respiratory syncytial virus and influenza during outbreaks has compromised the assessment of the relative contribution of each virus to viral lower respiratory tract infection in population based studies. The similarity in clinical syndromes caused by respiratory syncytial virus and influenza was shown in a recent community based observational study in the United Kingdom. This study showed that respiratory syncytial virus and influenza virus occur not only among people at the ends of the age spectrum but also among people aged 15-44 years and that in all age groups more than 20% of influenza-like illnesses are attributable to respiratory syncytial virus.6
Human metapneumovirus
Human metapneumovirus has recently been identified as a new paramyxovirus causing respiratory tract infections.7 It was isolated from nasopharyngeal aspirates from 28 children with symptoms of lower respiratory tract infection in the winter season in the Netherlands. Further serological studies revealed that virtually all children have been exposed to the virus by the age of 5 years. Studies from several other countries have confirmed its role in respiratory infections in both children and adults.8,9,w3,w4 The exact impact and epidemiology of human metapneumovirus in respiratory infections in infants and young children needs to be determined in prospective studies.
Severe acute respiratory syndrome
A worldwide outbreak of a life threatening febrile respiratory illness that has been named severe acute respiratory syndrome has recently started (box 1).w5 Hong Kong and the Guangdong province in China are the epicentres of the syndrome. By the beginning of May 2003 WHO had reported over 6500 cases in more than 25 countries. A causal association between severe acute respiratory syndrome and a newly identified coronavirus, distinct from the known human coronaviruses, has been shown.10 So far, infants and children do not seem to be a special risk group for the syndrome, and only a few cases have been reported among children under 15 years of age. Very recently, the clinical presentation and outcome in 10 children (aged 1.5-16.4 years) admitted to two hospitals in Hong Kong has been published.11 Whereas teenagers presented with the same symptoms as adults, young children presented mainly with signs of an upper respiratory tract infection without systemic symptoms such as chills, rigor, and myalgia. None of the children died. The clinical course seemed to be milder in young children than in teenagers and adults.
Box 1: Characteristics of severe acute respiratory syndrome
(see www.cdc.gov/ncidod/sars/casedefinition.htm for details of case definition)
Epidemiology
Most patients have been previously healthy adults aged 25-70 years
Only a few suspected cases have been reported in children
Signs and symptoms
Incubation time:2-7 days (may be up to 10 days)
Prodromal signs: fever (> 38°C), sometimes associated with headache, malaise, and myalgias
Lower respiratory signs: dry cough, dyspnoea potentially progressing to hypoxaemia, necessitating artificial ventilation in 10-20% of cases
Case fatality rate: around 9%, but may be much higher depending on host and viral factors
Milder course in young children than in teenagers and adults
Chest radiographs
Early focal infiltrates progressing to more generalised, patchy, interstitial infiltrates in a substantial proportion of patients
Abnormalities are indistinguishable from bronchopneumonia due to other causes
Laboratory abnormalities
Leukopenia with moderate lymphopenia
Elevated liver enzymes
Treatment
No efficacious treatment is yet known
Patients have been given a variety of antibiotics active against known bacterial agents of atypical pneumonia and antiviral agents such as oseltamivir or ribavirin in combination with steroids
Prevention
Standard, contact, and airborne precautions should be taken for infection control (see www.cdc.gov/ncidod/sars/infectioncontrol.htm for detailed information)
Bacterial co-infections
In addition to having a role as causative agents of respiratory disease, viral infections can predispose to bacterial superinfection.w6 Indeed, many experimental studies have shown that virus induced pathological and immunological phenomena may contribute to increased bacterial adhesion.w6 Despite this evidence for the important role of preceding viral infections in the aetiology of bacterial respiratory infections, the real incidence of clinically important bacterial superinfection after viral lower respiratory tract infection remains obscure. The proportion of children with mixed viral and bacterial respiratory tract infection found in studies using serology or antigen detection in serum or urine has been reported to be as high as 40%.12,w7 However, these methods are inadequate for assessing the clinical importance of the bacterial infection or the need for antimicrobial treatment. Other studies, using clinical methods, have shown that the risk of serious concurrent or secondary bacterial infection in patients with viral lower respiratory tract infection is very low.13,w8
Signs and symptoms
Respiratory viruses cause a similar spectrum of respiratory illness in children, ranging from pharingitis, otitis media, laryngitis subglottica, bronchitis, and tracheitis to bronchiolitis and pneumonia. It is difficult to distinguish clinically between the causative agents. Infections usually start with rhinorrhoea, cough and (non-obligate) fever. After one or two days the lower respiratory tract may become involved, with signs of respiratory distress, including tachypnoea, retractions, and cyanosis in severe cases. Life threatening apnoea may occur in very young infants, particularly in infections with respiratory syncytial virus. During infections with influenza virus systemic symptoms may be more prominent than signs in the respiratory tract.
Several patient groups are at high risk of a severe course of viral lower respiratory tract infection, especially in infections with respiratory syncytial virus. Examples are premature infants and patients with underlying pulmonary disease such as chronic lung disease or cystic fibrosis; patients with congenital heart disease, especially those with pulmonary hypertension, are also at risk. As well as these well known risk groups, previously healthy infants may also deteriorate severely during viral lower respiratory tract infection. Extreme tachypnoea and hypoxaemia are both associated with subsequent deterioration. Unfortunately, the sensitivity of these symptoms in identifying patients who will deteriorate is very low.w9
Bronchiolitis and pneumonia are the most common manifestations of viral lower respiratory tract infection in infants. Differentiation between these clinical syndromes is difficult as their definition is not based on standardised clinical criteria.w10 On the chest radiograph bronchiolitis is associated with air trapping and hyperinflation with or without focal and patchy atelectasis, whereas pneumonia lacks signs of hyperinflation and is characterised by interstitial thickening.w11 Overlap exists between the two clinical syndromes and they probably form both ends of a spectrum. The distinction between bronchiolitis and pneumonia is based on entangling clinical criteria and so far does not seem to be relevant in daily clinical practice. However, increasing insight into pathophysiological differences in the clinical manifestations of viral lower respiratory tract infection may eventually lead to specific treatment and preventive strategies in subgroups of patients, making an early specific diagnosis relevant.14 Additionally, the long term outcome of both groups might be different, eventually needing a differentiated therapeutic approach during initial disease.w12
Viral lower respiratory tract infection in immunocompromised patients
Respiratory viruses are a serious threat for immunocompromised patients.w2,w13 All community acquired respiratory viruses, especially adenovirus and respiratory syncytial virus, can cause severe infection in this high risk population, with considerable mortality. The presence of upper respiratory tract symptoms, wheezing, and interstitial or lobar consolidation on the chest radiograph may help in differentiating viral lower respiratory tract infection from other opportunistic respiratory pathogens, but definite diagnosis depends on demonstration of the virus in respiratory secretions by culture or polymerase chain reaction techniques. Pre-emptive treatment strategies are being explored in stem cell transplant recipients; these use routine polymerase chain reaction techniques to monitor viral load.
Children up to the age of 2 years infected with HIV have an almost fourfold increased risk of severe infection caused by respiratory syncytial virus, parainfluenza virus, influenza virus, and adenovirus than children not infected with HIV.15 In addition, HIV infected children more often present with pneumonia rather than bronchiolitis, more often have secondary bacterial infection, and have a higher mortality than uninfected children.16
Treatment
General considerations
Viral lower respiratory tract infections are usually self limiting. Preservation of adequate fluid intake and correction of hypoxaemia are mandatory in mild disease. Although medical treatment is rarely indicated in immunocompetent patients, great variability exists in the management of these patients.17,w14 Wilson et al showed that this variability does not affect clinical outcome but correlates significantly with costs associated with viral lower respiratory tract infections.18 No strict guidelines exist on when to admit or discharge children with a viral lower respiratory tract infection, but in daily practice physicians' discretion in decision making and factors associated with socioeconomic status are important determinants.19 Implementation of educational programmes and practical guidelines have been shown to be cost saving and may help in standardising treatment strategies for viral lower respiratory tract infections in children.20
Specific treatment strategies
Box 2 summarises the strategies available for treating viral lower respiratory tract infections.
Bronchodilator treatment
Despite unproved efficacy, bronchodilators are still often prescribed in patients with viral lower respiratory tract infection.17,w14 As in asthma, airway obstruction secondary to inflammation, oedema, and airway smooth muscle contraction are important in the pathophysiology of viral lower respiratory tract infection, especially that caused by respiratory syncytial virus. However, variations between patients in the response to bronchodilators indicate that differences might exist between patients in the contribution of these phenomena to airway obstruction. Future studies should focus on the identification of probable responders and non-responders to this form of treatment.
Corticosteroids
The efficacy of corticosteroids has been evaluated mainly in infants and children with respiratory syncytial virus disease, with disappointing results in mild disease. Very recently our group found that corticosteroids may be beneficial in artificially ventilated patients with severe bronchiolitis but had no effect in patients with pneumonia.14 These findings support the idea that corticosteroids may be beneficial in certain patients with a severe course of disease and that distinction between clinical manifestations of viral lower respiratory tract infection (bronchiolitis and pneumonia) is important in the evaluation of certain treatment strategies.
Antiviral treatment
Respiratory syncytial virus—Ribavirin is a synthetic nucleoside analogue with in vitro activity against respiratory syncytial virus.w31 However, on the basis of the currently available evidence, the routine use of ribavirin has no place in patients with respiratory syncytial virus infection.
Influenza virus—Although neuraminidase inhibitors are effective against influenza viruses, infections are relatively mild and self limiting in healthy children. On the other hand, costs attributable to influenza virus infections may be very high, particularly in infants and children.21 The goal of treatment with neuraminidase inhibitors therefore should be epidemiological control of disease rather than reducing the duration of disease in otherwise healthy individuals.
Antibiotics
Despite their lack of beneficial effects, antibiotics are often prescribed for patients with viral lower respiratory tract infection.17w14,w29,w32 In this era of increasing antimicrobial resistance this overuse should be reduced and future studies should focus on mechanisms and risk factors for bacterial superinfection in children with viral lower respiratory tract infection, as well as on accurate tests to differentiate viral from bacterial disease.
Prevention
Research into vaccination for viral lower respiratory tract infections in infants and children has mainly focused on respiratory syncytial virus and influenza virus. A recently published systematic review found no significant effect of vaccines against respiratory syncytial virus on preventing respiratory syncytial virus. The review included five controlled trials that evaluated the efficacy of subunit vaccines in children and adults mainly seropositive for respiratory syncytial virus.22 Although progress has been made during the past decade, particularly with live attenuated vaccines, it will take probably at least another 10 years before routine vaccination becomes available.w33
Disappointing results in the development of an active vaccine have forced research in the prevention of respiratory syncytial virus to focus on other strategies. Passive immunisation with intravenous hyperimmune globulins against respiratory syncytial virus has proved to be beneficial in preventing severe disease in children at high risk.23 However, practical problems have limited its use and further research and have led to the development of an intramuscular applicable IgG humanised monoclonal antibody directed against the F protein of respiratory syncytial virus (palivizumab). A controlled trial has shown that monthly injections with palivizumab reduce respiratory syncytial virus related hospital admissions in children at high risk by more than 50%.24 Several reports on experiences in the field have confirmed the trial results as well as the good safety profile of palivizumab. Although guidelines have been developed for use of palivizumab,w34 cost effectiveness studies in Europe have recommended that guidelines can not be generalised but should be based on national hospital admission data for respiratory syncytial virus.25,26
Inactivated intramuscular influenza vaccine as both cold adapted and live attenuated intranasal vaccines have been shown to be safe and effective in children from 1 year of age onwards,w35 but immunogenicity is poor in children younger than 6 months.27 Although influenza is usually a mild and self limiting disease, children with underlying chronic medical conditions are at risk of severe disease, and vaccination against influenza virus has mainly been focused on this patient group. In addition, although studies from the United States and western Europe have shown that vaccination is associated with economic benefits in all age groups, debate is ongoing about whether influenza vaccination should be broadened to all age groups, including healthy children and adults.28
Box 2: Treatment of viral lower respiratory tract infection
Bronchodilator agents
Studied in viral bronchiolitis irrespective of the viral cause
Most well designed trials show at best a minor beneficial effectw15-w17
Two meta-analyses have shown a statistically significant but clinically irrelevant beneficial effectw18,w19
Corticosteroids
Mainly studied in patients with (respiratory syncytial virus) bronchiolitis
Most well designed trials showed no beneficial effect of systemic or topical corticosteroids in patients with mild to moderate bronchiolitisw20-w22
A meta-analysis indicated a beneficial clinical effect of systemic corticosteroids in patients with moderate or severe bronchiolitisw23
A recent trial indicated a beneficial effect in a subgroup of patients with bronchiolitis14
Antiviral treatment
Respiratory syncytial virus
Ribavirin aerosol is not effective in immune competent patients and is restricted to immunocompromised patients with severe respiratory syncytial virus disease, although this practice is not supported by randomised controlled trials4
Parainfluenza virus and adenovirus
No specific treatment is available
Ribavirin has been used in immunodeficient patients, although this is mainly based on case reports and small series of heterogeneous patient populationsw24
Influenza virus
Ribavirin aerosol is not effective in immunocompetent patients,w25 and its efficacy in immunodeficient patients is unclear
Oral amantadine and rimantadine (M2 protein inhibitors) have been shown to shorten disease by one day in adults and children over 1 year of age with influenza A when given within 48 hours of the start of symptomsw26
Nasal zanamivir and oral oseltamivir (neuraminidase inhibitors) are effective in preventing and treating influenza A and B in adultsw27
Oseltamivir is also beneficial in children aged 1-12 yearsw28
The neuraminidase inhibitors are preferred to the M2 inhibitors as they have a broader antiviral activity, have less tendency for the development of resistance, and are better toleratedw27
Antibiotics
Antibiotics do not influence the course of viral lower respiratory tract infectionw29,w30
Additional educational resources
Useful articles
Nichol KL, Mallon KP, Mendelman PM. Cost benefit of influenza vaccination in healthy, working adults: an economic analysis based on the results of a clinical trial of trivalent live attenuated influenza virus vaccine. Vaccine 2003;21: 2216-26
Hall CB. Respiratory syncytial virus and parainfluenza virus. N Engl J Med 2001;344: 1917-28
Hament JM, Kimpen JL, Fleer A, Wolfs TF. Respiratory viral infection predisposing for bacterial disease: a concise review. FEMS Immunol Med Microbiol 1999;26: 189-95
Meissner HC. Uncertainty in the management of viral lower respiratory tract disease. Pediatrics 2001;108: 1000-3
Patel H, Platt R, Lozano JM, Wang EEL.
Glucocorticoids for acute viral bronchiolitis in hospitalized infants and young children (protocol for a Cochrane review). In: Cochrane Library, Issue 2. Oxford: Update Software, 2003
Information on SARS
Centers for Disease Control and Prevention: www.cdc.gov/ncidod/sars/
World Health Organization: www.who.int/csr/sars/en/
Information for patients
eMedicine (www.emedicine.com/): an online emergency textbook with extensive chapters on paediatrics and possibilities to search for patient education
Virtual Children's Hospital (www.vh.org/pediatric/index.html): gives information for patients on many paediatric topics, including infectious diseases
Progress has been made in the development of a parainfluenza virus vaccine. However, no effective human vaccine is yet available.w2
Conclusion
Viral lower respiratory tract infections in infants and children are an important medical and socioeconomic problem worldwide. Viral lower respiratory tract infections are mild and self limiting in most cases. Particular patient groups are at risk of a severe course of disease, although previously healthy infants with a viral lower respiratory tract infection may also develop severe disease.
Treatment for moderate viral lower respiratory tract infection is mainly supportive. Lack of means to control viral lower respiratory tract infection has led to great variation in management worldwide.17,w14 Development of practical guidelines and educational programmes in both clinical and outpatient settings may be helpful and cost saving in the control of viral lower respiratory tract infection in infants and children.
Supplementary Material
 Additional
references (w1-w35) are on
bmj.com
Additional
references (w1-w35) are on
bmj.com
Contributors: JBMvW drafted the original manuscript. All three authors jointly wrote the final paper.
Competing interests: JBMvW and JLLK have received fees for giving presentations at symposia organised by Abbot Laboratories, manufacturer of palivizumab.
References
- 1.Miedema CJ, Kors AW, Tjon a Ten WE, Kimpen JLL. Medical consumption and socioeconomic effects of infection with respiratory syncytial virus in the Netherlands. Pediatr Infect Dis J 2001;20: 160-3. [DOI] [PubMed] [Google Scholar]
- 2.Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, Anderson LJ. Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA 1999;282: 1440-6. [DOI] [PubMed] [Google Scholar]
- 3.Muller-Pebody B, Edmunds WJ, Zambon MC, Gay NJ, Crowcroft NS. Contribution of respiratory syncytial virus to bronchiolitis and pneumonia-associated hospitalizations in English children, April 1995-March 1998. Epidemiol Infect 2002;129: 99-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Simoes EA. Respiratory syncytial virus infection. Lancet 1999;354: 847-52. [DOI] [PubMed] [Google Scholar]
- 5.Izurieta HS, Thompson WW, Kramarz P, Shay DK, Davis RL, DeStefano F, et al. Influenza and the rates of hospitalization for respiratory disease among infants and young children. N Engl J Med 2000;342: 232-9. [DOI] [PubMed] [Google Scholar]
- 6.Zambon MC, Stockton JD, Clewley JP, Fleming DM. Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: an observational study. Lancet 2001;358: 1410-6. [DOI] [PubMed] [Google Scholar]
- 7.Van den Hoogen BG, de Jong JC, Groen J, Kuiken T, de Groot R, Fouchier RA, et al. A newly discovered human pneumovirus isolated from young children with respiratory tract disease. Nat Med 2001;7: 719-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peret TC, Boivin G, Li Y, Couillard M, Humphrey C, Osterhaus AD, et al. Characterization of human metapneumoviruses isolated from patients in North America. J Infect Dis 2002;185: 1660-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greensill J, McNamara PS, Dove W, Flanagan B, Smyth RL, Hart CA. Human metapneumovirus in severe respiratory syncytial virus bronchiolitis. Emerg Infect Dis 2003;9: 372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 2003;348: 1953-66. [DOI] [PubMed] [Google Scholar]
- 11.Hon K, Leung CW, Cheng W, Chan P, Chu W, Kwan YW, et al. Clinical presentations and outcome of severe acute respiratory syndrome in children. Lancet 2003;361: 1701-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Korppi M, Leinonen M, Koskela M, Makela PH, Launiala K. Bacterial coinfection in children hospitalized with respiratory syncytial virus infections. Pediatr Infect Dis J 1989;8: 687-92. [DOI] [PubMed] [Google Scholar]
- 13.Hall CB, Powell KR, Schnabel KC, Gala CL, Pincus PH. Risk of secondary bacterial infection in infants hospitalised with respiratory syncytial viral infection. J Pediatr 1988;113: 266-71. [PubMed] [Google Scholar]
- 14.Van Woensel JBM, van Aalderen WMC, de Weerd W, Jansen NJG, van Gestel JPJ, Markhorst DG, et al. The efficacy of dexamethasone in the treatment of patients mechanically ventilated for lower respiratory tract infection caused by respiratory syncytial virus: a randomized controlled trial. Thorax 2003;58: 383-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Madhi SA, Schoub B, Simmank K, Blackburn N, Klugman KP. Increased burden of respiratory viral associated severe lower respiratory tract infections in children infected with human immunodeficiency virus type-1. J Pediatr 2000;137: 78-84. [DOI] [PubMed] [Google Scholar]
- 16.Graham SM, Gibb DM. HIV disease and respiratory infection in children. Br Med Bull 2002;61: 133-50. [DOI] [PubMed] [Google Scholar]
- 17.Kimpen JLL, Schaad UB. Treatment of respiratory syncytial virus bronchiolitis: 1995 poll of members of the European Society for Paediatric Infectious Diseases. Pediatr Infect Dis J 1997;16: 479-81. [DOI] [PubMed] [Google Scholar]
- 18.Wilson DF, Horn SD, Hendley JO, Smout R, Gassaway J. Effect of practice variation on resource utilization in infants hospitalized for viral lower respiratory illness. Pediatrics 2001;108: 851-5. [DOI] [PubMed] [Google Scholar]
- 19.McConnochie KM, Roghmann KJ, Liptak GS. Hospitalization for lower respiratory tract illness in infants: variation in rates among counties in New York State and areas within Monroe County. J Pediatr 1995; 126: 220-9. [DOI] [PubMed] [Google Scholar]
- 20.Adcock PM, Sanders CL, Marshall GS. Standardizing the care of bronchiolitis. Arch Pediatr Adolesc Med 1998;152: 739-44. [DOI] [PubMed] [Google Scholar]
- 21.Neuzil KM, Mellen BG, Wright PF, Mitchel EF Jr, Griffin MR. The effect of influenza on hospitalizations, outpatient visits, and courses of antibiotics in children. N Engl J Med 2000;342: 225-31. [DOI] [PubMed] [Google Scholar]
- 22.Simoes EA, Tan DH, Ohlsson A, Sales V, Wang EE. Respiratory syncytial virus vaccine: a systematic overview with emphasis on respiratory syncytial virus subunit vaccines. Vaccine 2001;20: 954-60. [DOI] [PubMed] [Google Scholar]
- 23.Groothuis JR, Simoes EAE, Levin MJ, Hall CB, Long CE, Rodriguez WJ. Prophylactic administration of respiratory syncytial virus immune globulin to high-risk infants and young children. N Engl J Med 1993;329: 1524-30. [DOI] [PubMed] [Google Scholar]
- 24.The Impact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics 1998;102: 531-7. [PubMed] [Google Scholar]
- 25.Clark SJ, Beresford MW, Subhedar NV, Shaw NJ. Respiratory syncytial virus infection in high risk infants and the potential impact of prophylaxis in a United Kingdom cohort. Arch Dis Child 2000;83: 313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roeckl-Wiedmann I, Liese JG, Grill E, Fischer B, Carr D, Belohradsky BG. Economic evaluation of possible prevention of respiratory syncytial virus-related hospitalizations in premature infants in Germany. Eur J Pediatr 2003;162: 237-44. [DOI] [PubMed] [Google Scholar]
- 27.Clements ML, Makhene MK, Karron RA, Murphy BR, Steinhoff MC, Subbarao K, et al. Effective immunization with live attenuated influenza A virus can be achieved in early infancy. J Infect Dis 1996;173: 44-51. [DOI] [PubMed] [Google Scholar]
- 28.Nichol KL, Mallon KP, Mendelman PM. Cost benefit of influenza vaccination in healthy, working adults: an economic analysis based on the results of a clinical trial of trivalent live attenuated influenza virus vaccine. Vaccine 2003;21: 2216-26. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.