Abstract
Plants are a treasure trove of bioactive compounds. Kedrostis foetidissima (Jacq.) Cogn. has many important phytoconstituents like cucurbitacins, rutin, and quercitin compounds. Among these compounds, Quercetin-3-O- Rhamnoside (1) has antioxidant, anti-inflammatory, anticancer properties. Rutin (2) has anti-inflammatory, antioxidant, anti-diabetic, anti-microbial, antiviral properties, 7, 10—Hexa decadienoic acid methyl ester (3) has anti-inflammatory, antioxidant, hypocholesterolemia and anticancer activities. Docosanoic acid (4) has antioxidant, α-Glucosidase inhibitory activity. 3,7,11,15-Tetra methyl hexa decan-1-ol (5) has antiviral properties. Cucurbitacin-B (6) has antipyretic, analgesic, anti-inflammatory, antimicrobial, and antitumor activities. Performance of experimental studies on phytochemicals become more difficult as the availability of compounds in small quantities, hence the computational methods becomes important for drug discovery. Based on their biological activity, compounds 1–6 were tested for in silico ADMET (absorption, distribution, metabolism, excretion, and toxicity) profiling and drug-likeness properties using the Swiss ADME online web server and the pkCSM server. All the studied compounds obey Lipinski's rule of five except compounds 1 and 2 with two and three violations each. The entire selected compounds have a good bioavailability score in the recommended range of 0 to 1. Compound 4 has high (0.85) and compounds 1 and 2 have low (0.17) oral bioavailability scores. All the selected compounds from Kedrostis foetidissima have strong pharmacological activities. Supporting this, the selected plant methanol extracts of leaf, stem callus, and tuber have shown well in vitro antibacterial activity against Bacillus subtilis, Escherichia coli, and Proteus vulgaris. Therefore, these compounds may be developed into drug molecules with additional clinical research.
Keywords: Kedrostis foetidissima, ADMET, Antibacterial, In-silico
Introduction
Kedrostis foetidissima (Jacq.) Cogn is an important medicinal plant belonging to the Cucurbitaceae family. Kedrostis foetidissima is a climber in the family. It is a monoecious scandent shrub with a perennial rootstock that grows up to a height of 2 m. There are about 27 species in Kedrostis (Chakrvarty 1982). It is rich in regions of South Africa, Asia, India to Burma (John 2019). In India, it is distributed in warm and dry areas of Gujarat, Karnataka, Madhya Pradesh, Maharashtra, Tamil Nadu, and Andhra Pradesh (erstwhile). Kedrostis foetidissima had great medicinal value and uses in traditional and folklore systems of medicine (Siddha) for many years. This plant is used for curing various ailments such as cough, common cold, and measles, healing wounds, and treating bloats in cattle (Amutha 2017). It is also used for eczema, diarrhea in boils (https//www.wildturmeric.net), Asthma (Dogra et al. 2015), and hypertension and stomach-ache (Mugomeri et al. 2016).
Preliminary phytochemical analysis showed the presence of alkaloids, flavonoids, glycosides, phenols, saponins, steroids, and triterpenoids (Thenmozhi et al. 2014). GC–MS analysis of leaf extracts revealed 7,10-hexadecadienoic methyl ester, 2-hexadecen-1-ol, 3,7,11,15 Tetramethyl hexa decan-1 -ol, 1 H-1,2,4-triazole-3,5-dicarbaldehyde, and docosanoic acid as major components (Kalaisezhiyen and Sasikumar 2012). Phytochemical analysis of this plant through column chromatography revealed the presence of compounds like rutin, quercetin-o-rhamnoside, and cucurbitacin glycoside (Amutha 2017). The more interesting feature of this plant is the presence of cucurbitacins. Cucurbitacins B, D, E, and I were reported in this plant (Rios et al. 2005). Cucurbitacin C from stems and I from leaves were reported (Njoroge and Newton 1994 Jul).
Kedrostis foetidissima leaf extract showed anti-bacterial and antifungal activity (Priyavardhini et al. 2008, 2012), antidiarrheal activity (Sivaprakash 2016), antioxidant activity (Pavithra and Saravanan 2019), antiplasmodial, antileishmanial, and antitrypanosomal activity (Mothana et al. 2014), and wound healing property. Leaf, stem, and fruit extracts of this plant showed anticancer and anti-proliferative activity against human hepatocellular liver carcinoma cell lines (HEPG2), ethanol extracts, silver, and gold nanoparticles against the human osteosarcoma cell lines (MG-63), lung cancer cell lines A-549, and breast cancer cell lines MCF-7 and YMB-1 (Choene and Motadi 2012).
Drug development involves the assessment of the absorption, distribution, metabolism, and excretion (ADME) of a compound. Drug-likeness described as a complex balance of various molecular properties and structural features that can explain whether a compound is similar to the known drugs (Daina et al. 2017). Drug-likeness was evaluated by the Lipinski rule of five, which evaluates five simple physicochemical parameters. The performance of experimental studies becomes more difficult with the availability of compounds for physio-chemical screening in small quantities and using non-traditional techniques; hence, computational methods become important for drug discovery (Lipinski et al. 2001). Lipinski’s rule of five (RO5) was major in drug discovery. This rule used to determine the bioavailability of bulk materials to inspect their drug-like properties (Kavitha and Alivelu 2021).
An ideal drug administered orally has been absorbed from the gastrointestinal tract, distributed to its specific target, metabolized in the body without altering its properties, and excreted without any damage, or causing toxicity (Khan et al. 2017). Predictive tools for accessing the pharmacokinetic and toxicological properties, and the pharmacodynamic properties, are crucial for the early developmental stages of drug discovery processes. In silico methods are employed to estimate ADMET properties because in vivo and in vitro evaluations are becoming premium and laborious (Cheng et al. 2013).
Flavonoids are specialized metabolic compounds that possess antimicrobial properties, which include anti-viral activity (Rahman et al. 2021), antioxidants, and antidiabetic (Liu 2016). and anticancer activities (Raffa et al. 2017). Rutin and quercetin are flavonoid compounds. Which possess antiviral, antibacterial, anti-inflammatory, antioxidant, hepatoprotective, and anticancer activities (Gullón et al. 2017). Cucurbitacins are highly oxidized tetracyclic triterpenoids that are often present in the Cucurbitaceae family and have strong anticancer activity and antiviral, antibacterial, anti-hypertensive, anti-hyperglycemic, and anti-parasitic activities. They are also used in central nervous system disorders (Cai et al. 2015). Cucubitacin-B shows anticancer activity against the human leukemia cell line 562 (Chan et al. 2010), colorectal cancer cells (Chai et al. 2018), primary effusion lymphoma (PEL) (Ueno et al. 2021), and hepatocellular carcinoma cell line BEL-7402. 7, 10-hexa deca dienoic acid is an omega-6 fatty acid that has antioxidant, anti-inflammatory, hypocholesterolemic, and anti-cancer activities (Alqahtani et al. 2019). Docosanoic acid possesses antioxidant and α-glucosidase inhibitory activity (Zhang et al. 2020), 3,7,11,15-Tetramethyl-1-hexadecanol has antiviral properties (Sangeetha et al. 2017). Different biological activities are possessed by the Kedrostis foetidissima compounds that were chosen for drug-likeness analysis and ADMET profiling. Plant methanol and aqueous extracts of leaves, stem callus, and tubers have been investigated for them in vitro antibacterial activity against Proteus vulgaris, Escherichia coli, and Bacillus subtilis to substantiate this.
Materials and methods
Computational method
The structures of the biologically active compounds present in Kedrostis foetidissima were identified from the literature. Six compounds (Fig. 1) are selected for drug-likeness analysis and ADMET studies. They are Quercetin-3-O- Rhamnoside (1), Rutin (2), 7, 10—Hexa decadienoic acid methyl ester (3), Docosanoic acid (4), 3,7,11,15-Tetra methyl hexa decan-1-ol (5), and Cucurbitacin-B (6).
Fig. 1.
Structures of selected compounds of Kedrostis foetidissima
The Swiss ADME online web server (http://www.swissadme.ch/) is used to predict the drug-likeness properties and oral bioavailability of selected compounds. As per Lipinski’s rule of five (RO5), a drug-like compound should have a molecular weight (MW) ≤ 500 Da, Van der Walls topological polar surface area (TPSA) value of ≤ 120 A°, a hydrogen bond acceptor (HBAs) ≤ 10, a hydrogen bond donor (HBD’s) ≤ 5, a partition coefficient (log P) ≤ 5, and only one violation allowed. The bioavailability of selected compounds was analysed by the bioavailability RADAR. For each of the selected compounds, several pharmacokinetic parameters for absorption, distribution, metabolism, excretion, and toxicity (ADMET) were analyzed using the pkCSM server (Pires et al. 2015).
Antibacterial studies
Plant material
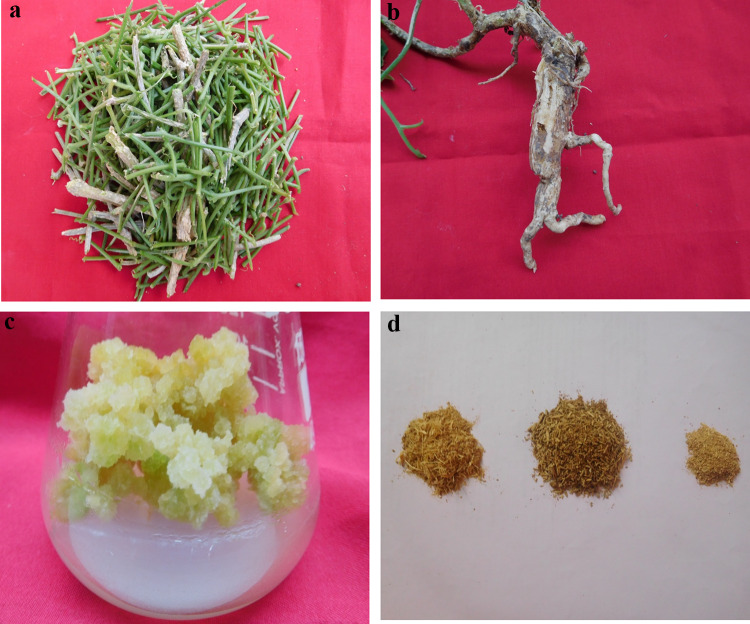
Kedrostis foetidissima plant material (tubers) was collected in the rainy season (July) from Hanumakonda district. The collected tubers were planted in the botanical garden of the Department of Botany, Kakatiya University, Hanumakonda. The plant material was authenticated by Dr. Mohammad Mustafa, Department of Botany, Kakatiya University, and Hanumakonda. Matured plant material is used for antimicrobial studies (Fig. 2a, b, c, and d).
Fig. 2.
a Plant stem meterial of Kedrostis foetidissima. b Plant tuber material of Kedrostis foetidissima. c Stem callus material of Kedrostis foetidissima. d Dried powders of tuber, stem and stem callus of Kedrostis foetidissima
Test microorganisms
The following three bacterial strains were received from the Dept. of Microbiology, Pingle Govt. College for Women (A), Hanumakonda, Telangana. They were maintained on agar slants in an incubator until the experiment. They are Gram-positive bacteria: Bacillus subtilis, Gram-negative bacteria: Escherichia coli, and Proteus vulgaris.
Nutrient media
Nutrient agar media prepared by using 15% agar, 5% peptone, 3% beef extract, and 3 gr. NaCl dissolved in 1L distilled water and sterilized by autoclaving. 15 ml of nutrient agar media was poured into Petri dishes (15 mm) to prepare agar test plates.
Materials and instruments
All of the chemicals and reagents used in this study are purchased from HiMedia Laboratories Private Limited Bioscience Company, India. The instruments used in the study are Autoclave (Indosurgicals-India), Laminar-air-flow (Bionics scientific- India), and Incubator (Bionics scientific- India).
Preparation of plant extract
About 100 g of shade-dried plant parts, like the stem, stem callus, and tuber of the experimental plant, were ground in a mortar and pestle to make a fine powder. These were extracted using methanol and aqueous solvents. Used the cold extraction method by continuously shaking plant material in solvent for 24 h. Then the solvent was filtered, and the filtrate was evaporated until it became semisolid. The extract was taken from plates and stored at 4 °C until use.
Agar-well diffusion method
Bacterial cultures were mixed with nutrient agar media when it was warm and in a melted state, and about 15 ml of media was poured into the Petri plates. Then the plates were closed and allowed to cool. After inoculation, wells were prepared with a 6 mm sterile cork borer. To the wells, 20 μl of plant extract solution was added by using a micropipette (Valgas et al. 2007). The test solution was prepared by dissolving the plant extract in dimethyl sulfoxide (DMSO). The plates were labeled, covered, inverted, and incubated in an incubator for 24 h. After that, the zone of inhibition was measured, and data were recorded. Mean of three replicates were taken.
Result and discussion
Drug-likeness and oral bioavailability analysis
The Swiss ADME tool (http://www.swissadme.ch/) was used to evaluate the drug-likeness properties and oral bioavailability of selected compounds from Kedrostis foetidissima. The obtained results are presented in Table 1. Lipinski’s rule of five (RO5) was major in drug discovery. All the studied compounds obey Lipinski's rule of five, except Compounds 1 and 2. It indicates that all the studied compounds can be easily carried away, diffused, and absorbed (Murugesan et al. 2020). Compound 1 violates the rule with 2 violations, i.e., HBA 11 and TPSA 269.43, and Compound 2 violates the rule with 3 violations, i.e., MW 620.25, HBA 16, and TPSA 190.28. Even though Compounds 1 and 2 violate Lipinski’s rule, a literature review revealed that two of the important limitations of Lipinski’s rule of five are that they exclude natural products and exaggerate oral bioavailability. Approximately 50% of the FDA-approved drugs in small compounds are known to either violate Lipinski’s rule or not be administered orally. Strictly Following these rules would lead to the overlooking of important lead compounds (Zhang and Wilkinson 2007). Hence, Compound 2 (Rutin) was considered a prospective lead molecule against SARS-CoV-2 (Zackria et al. 2022).
Table 1.
Drug likeness and oral bioavailability of selected compounds
| Compound | MW (mg) |
HBD | HBA | Nnor | TPSA | Fraction Csp3 | Log S (ESOL) | Log P (XlogP3) | RO5 Violations |
Bio availability score |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 448.38 | 7 | 11 | 3 | 269.43 | 0.29 | − 3.33 | 0.86 | 2 | 0.17 |
| 2 | 610.25 | 10 | 16 | 16 | 190.28 | 0.44 | − 3.3 | − 0.33 | 3 | 0.17 |
| 3 | 266.42 | 0 | 2 | 13 | 26.3 | 0.71 | − 4.25 | 5.74 | 1 | 0.55 |
| 4 | 340.58 | 1 | 2 | 20 | 37.3 | 0.95 | − 7.16 | 10.37 | 1 | 0.85 |
| 5 | 125.9 | 1 | 4 | 2 | 75.71 | 0 | − 0.63 | − 0.42 | 0 | 0.55 |
| 6 | 558.708 | 3 | 8 | 6 | 138.20 | 0.75 | − 4.57 | 2.64 | 1 | 0.55 |
MW molecular weight, HBD no. of hydrogen bond donors, HBA no. of hydrogen bond acceptor, Nnor no. of rotatable bonds, TPSA topological polar surface area, Fraction Csp3 ratio of sp3 hybridized carbons over the total carbon count of the molecule, Log S water solubility, Log P logarithm of compound partition coefficient between n-octanol and water
Various properties for oral bioavailability (size, polarity, insolubility, instauration, flexibility, and lipophilicity) of the compounds were analyzed by comparing the radar plots (Fig. 3). The pink area in the RADAR shows the most favourable zone for each of the bioavailability (Abdul-Hammed et al. 2022). Except for Compounds 2 and 6, all are in the recommended SIZE < 500 mg/compound. Polarity (POLAR) was assessed by the TPSA, and all the compounds except compounds 1, 2, and 6 were within the limit, i.e., 120 A°, which implies that compounds are fulfilling the optimal requirement for drug absorption and are following the Lipinski rule. Lipophilicity (LIPO) and insolubility (INSOLU) are one of the important criteria for bioavailability studies. All the compounds except compound 4 are in the recommended range of ESOL log S. This compound shows a 7.16 value of ESOL log S, which means it is poorly soluble. Poor aqueous solubility and a slow dissipation rate can lead to poor oral absorption and lower oral bioavailability (Waterbeemd and Gifford 2003). So it can be administered through an oral or parenteral route (Sepay et al. 2021). The value of FLEX (Flexibility) is evaluated using the number of rotatable bonds, which does not exceed 9. For this character, except compounds 3, 4, and 5, all are accepting this. The instauration (INSATU) was determined using Fraction Csp3. All the selected compounds also obey this property. The entire selected compounds have a good bioavailability score (Fig. 4) in the recommended range of 0 to 1 (Martin 2005), hence they can be used for drug development.
Fig. 3.
The bioavailability RADAR for the selected compounds
Fig. 4.
Comparison of bioavailability score of selected molecules of Kedrostis foetidissima
In silico ADMET profiling of selected compounds
The results for ADMET profiling of selected compounds retrieved from the pkCSM server (https://biosig.lab.uq.edu.au/pkcsm/prediction) are presented in Table 2. The pharmacokinetics of a drug or compound help us know about the metabolism and movement of a drug in the body.
Table 2.
The results of ADMET profiling given by PkCSM server
| Property | Model name | Unit | Predicted values for compounds | |||||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||
| Absorption | Water solubility | Numeric(log mol/L) | − 2.903 | − 2.892 | − 6.166 | − 7.584 | − 6.67 | − 5.149 |
| CaCO3 permeability | Numeric(log Papp in 10−6 cm/s) | 0.048 | − 0.949 | 1.072 | 1.513 | 1.614 | − 0.124 | |
| Human intestinal absorption |
Numeric (% absorbed) |
52.709 | 23.446 | 89.942 | 90.785 | 93.347 | 76.76 | |
| Skin permeability | Numeric( log Kp) | − 2.735 | − 2.735 | − 2.734 | − 2.625 | − 2.457 | − 3.315 | |
| P-glycoprotein substrate | Categorical(yes/no) | Yes | Yes | No | No | No | Yes | |
| P-glycoprotein inhibitor-I | Categorical(yes/no) | No | No | No | No | No | Yes | |
| P-glycoprotein inhibitor-II | Categorical(yes/no) | No | No | Yes | Yes | No | Yes | |
| Distribution | VDss (human) | Numeric(log L/kg) | 1.517 | 1.663 | − 0.554 | 0.468 | 0.277 | − 0.105 |
| Fraction unbound (human) | Numeric( Fu) | 0.13 | 0.187 | 0.009 | 0.502 | 0.079 | 0.221 | |
| BBB permeability | Numeric (log BB) | − 1.495 | − 1.899 | − 0.363 | 0.829 | 0.079 | − 1.207 | |
| CNS permeability | Numeric (log PS) | − 4.156 | − 5.178 | − 1.488 | − 1.62 | − 1.572 | − 3.279 | |
| Metabolism | CYP2D6 substrate | Categorical(yes/no) | No | No | No | No | No | No |
| CYP3A4 substrate | Categorical(yes/no) | No | No | Yes | Yes | Yes | Yes | |
| CYP1A2 inhibitor | Categorical(yes/no) | No | No | Yes | Yes | Yes | No | |
| CYP2C19 inhibitor | Categorical(yes/no) | No | No | No | No | No | No | |
| CYP2C9 inhibitor | Categorical(yes/no) | No | No | No | No | No | No | |
| CYP2D6 inhibitor | Categorical(yes/no) | No | No | No | No | No | No | |
| CYP3A4 inhibitor | Categorical(yes/no) | No | No | No | No | No | No | |
| Excretion | Total clearance | Numeric (log ml/min/kg) | 0.364 | − 0.369 | 1.967 | 1.616 | 1.968 | 0.093 |
| Renal OCT2 substrate | Categorical(yes/no) | No | No | No | No | No | No | |
| Toxicity | AMES toxicity | Categorical(yes/no) | No | No | No | No | No | No |
| Max. Tolerated dose (human) | Numeric( log mg/kg/day) | 0.495 | 0.452 | − 0.796 | 0.184 | 0.073 | − 0.863 | |
| hERG I inhibitor | Categorical(yes/no) | No | No | No | No | No | No | |
| hERG II inhibitor | Categorical(yes/no) | No | Yes | No | Yes | No | Yes | |
| Oral acute rat toxicity (LD50) | Numeric(mol/kg) | 2.586 | 2.491 | 1.369 | 1.607 | 1.579 | 2.185 | |
| Oral chronic rat toxicity (LOAEL) | Numeric (log mg/g bw/day) | 3.022 | 3.673 | 3.639 | 1.009 | 2.854 | 1.687 | |
| Hepatotoxicity | Categorical(yes/no) | No | No | Yes | No | No | No | |
| Skin sensitisation | Categorical(yes/no) | No | No | Yes | Yes | Yes | No | |
| T. pyriformis toxicity | Numeric(log ug/L) | 0.285 | 0.285 | 0.381 | 1.829 | 2.061 | 0.316 | |
Absorption of the compounds is predicted using parameters like water solubility, CaCO3 permeability, skin permeability, and a P-gp inhibitor or substrate. All the selected compounds except compounds 3, 4, and 5 are within the range of log S, which is water solubility. CaCO3 permeability > 0.9 indicates high permeability. Compounds 3, 4, and 5 show higher CaCO3 permeability than all other compounds. Skin permeability (log Kp) > − 2.5 is considered to have low skin permeability for compounds. Except for compound 5, all are showing good skin permeability. Human intestinal absorption (HIA) value < 30% is considered to be a low absorption rate. An HIA value of 70 to 100% shows good intestinal absorption. Except for compound 2, all are showing excellent absorption. The main function of P-glycoprotein is to act as a biological barrier to eliminate toxins and xenobiotics from cells (Flores-Holguín et al. 2021). Hence, only compounds 1 and 2 are substrates for P-glycoprotein. None of the compounds is an inhibitor of P-Glycoprotein-I. Only compounds 3 and 4 are inhibitors of P-glycoprotein-II.
Among the distribution parameters, VDss (Volume of distribution at steady state), blood–brain barrier (BBB), CNS (Central nervous system) permeability, and fraction unbound (human) are calculated. The structural and physicochemical properties of the compound determine the distribution rate in the body. Some drugs may cross the blood–brain barrier (BBB) and enter the brain and central nervous system. Finally, the drug will bind to its molecular target. VDss calculates that the total dose of the drug would need to be uniformly distributed in blood plasma. Except for compounds 3 and 6, all have high VDss > 0.45, which indicates all these compounds readily distribute in blood plasma. For the selected compounds, all cannot cross the BBB, except compound 5, which is showing poor distribution in the brain. This means they don’t show any side effects on the brain. For the CNS, except compound 3, 4, and 5, all are showing less permeability to the brain.
The metabolism of drugs is carried out by cytochrome P450 enzymes. Inhibition of these enzymes leads to an increase in the concentration of drugs in the blood and shows adverse effects on organs. Among all the CYPs, CYP3A4, CYP2D6, CYP2C9, CYP2C19, and CYP2C8 contribute over 50% of CYP-related drug metabolism (Zhao et al. 2021). For the metabolism parameters, compounds 3, 4, 5, and 6 are substrates for CYP3A4. Except for compounds 3, 4, and 5, all are inhibitors of CYP1A2, and the remaining compounds are non-inhibitors. All the compounds are non-inhibitors for CYP2AC19, CYP2AC9, CYP2D6, and CYP3A4. The inhibition of cytochrome proteins reduces the capacity and pharmacological effects of the drug (Kavitha et al. 2022). Hence, all studied compounds can metabolize excellently.
Excretion parameters include: Total clearance and renal OCT2 substrates were analyzed. Hydrophobicity and molecular weight of the compounds are the main criteria for drug elimination. For this, none of the compounds are substrates for all the renal OCT2. Except for compound 2, all the compounds showed a high (> 0.3) value of total clearance.
The AMES test (Salmonella mutagenicity assay) is a bacteria-based method to determine a compound’s mutagenic potential. When the test is positive, it shows that the substance is mutagenic and able to cause cancer (Flores-Holguín et al. 2021). For the AMES test, none of the compounds are positive. None of the compounds are inhibitors of hERG2-I. Compounds 2 and 4 are inhibitors of hERG II. MRDT (Maximum tolerated dose) is the maximum tolerated dose that predicts the values of the toxic dose threshold of chemicals in humans. The recommended value for MRDT is ≤ 0.477 log (mg/kg/day), which is considered low and high if > 0.477. Only Compound 6 shows a high (− 0.863) MRDT, and the remaining has a low. Many drugs cause liver injuries. Hence, it is a safety concern for drug development. Only compound 3 showed hepatotoxicity. Compounds 3, 4, and 5 are showing skin sensitization. Remaining, not showing any skin sensitization. T. pyriformis is a protozoan bacterium, and its toxicity is frequently used as a toxic endpoint. A value > − 0.5 log ug/L is considered toxic. All the selected compounds show toxicity to this.
Antibacterial studies
Methanol and aqueous extracts of stem and callus derived from stem and tuber extracts were screened for antibacterial activity against Bacillus subtilis, Escherichia coli, and Proteus vulgaris, and zones of inhibition were recorded after 24 h, as presented in Table 3 (Fig. 5a, b, c, d, e, f).
Table 3.
Growth of inhibition of various extracts of Kedrostis foetidissima against bacterial cultures
| S. No | Organism | Methanol extract (20 μL) | Aqueous extract (20 μL) | ||||
|---|---|---|---|---|---|---|---|
| SC | S | T | SC | S | T | ||
| 1 | Bacillus subtilis | 18 | 17 | 12 | 13 | 8 | 6 |
| 2 | Escherichia coli | 19 | 16 | 6 | 12 | 10 | 5 |
| 3 | Proteus vulgaris | 18 | 16 | 10 | 14 | 11 | 8 |
Values indicates zone of inhibition in mm
SC stem callus, S stem, T tuber
Fig. 5.
a Growth of inhibition with stem, stem callus and tuber extracts of Kedrostis foetidissima-Methanol extracts against Bacillus subtillis. b Growth of inhibition with stem, stem callus and tuber extracts of Kedrostis foetidissima-Aqueous extracts against Bacillus subtillis. c Growth of inhibition with stem, stem callus and tuber extracts of Kedrostis foetidissima-Methanol extracts against Escherichia coli. d Growth of inhibition with stem, stem callus and tuber extracts of Kedrostis foetidissima-Aqueous extracts against Escherichia coli. e Growth of inhibition with stem, stem callus and tuber extracts of Kedrostis foetidissima- Methanol extracts against Proteus vulgaris. f Growth of inhibition with stem, stem callus and tuber extracts of Kedrostis foetidissima-Aqueous extracts against Proteus vulgaris
Methanol and aqueous extracts of stem extracts showed the highest activity against Escherichia coli, with 16 mm and 10 mm zones of inhibition, respectively. In contrast to our results, ethanol extracts of stem and leaf showed less activity against Escherichia coli. This is because different solvent extracts have different chemical compounds. The highest zone of inhibition, about 17 mm, was achieved against Basillus subtilis in methanol extract. Whereas acetone and chloroform extracts showed less response to Basillus subtilis. 11 mm of zone of inhibition against Proteus vulgaris was observed in aqueous solvents.
The antibacterial activity of methanol extracts of stem callus against Escherichia coli is greater than the antibiotic activity of gentamicin and tetracycline (Raja et al. 2019). For Bacillus subtilis, the highest zone of inhibition was about 18 mm and 13 mm, respectively, for the ethanol and aqueous extracts recorded. Methanol and aqueous extracts of stem callus extracts showed the highest activity against Proteus vulgaris, with 18 mm and 14 mm zones of inhibition, respectively. Similarly, callus cultures showed a higher zone of inhibition against E. coli in Clitoria ternatea than root extracts (Malabadi et al. 2012). With our results, it is proven that the in vitro-derived calli tissue was more effective compared to the in vivo tissue in terms of antibacterial activity (Shariff et al. 2006).
Among all plant extracts studied, tuber extracts showed the least response against all the studied organisms. Highest activity against Bacillus subtilis and Proteus vulgaris with 12 mm and 10 mm zones of inhibition, respectively, in methanol extracts. This proves that aerial parts show the highest inhibition activity compared to underground parts against microbes. Similar results were achieved in Gentiana asclepiadea (Vladimir et al. 2011).
In our results, methanol extracts of stem callus, stem, and tuber extracts showed more inhibition of the growth of bacteria than aqueous extracts. Similar reports were achieved with extracts of Boerhaavia diffusa, Tinospora cardiofolia, and Eclipta alba (Girish and Satish 2008). In vitro-derived stem, callus proved more bacterial efficacy than in vivo plant material, i.e., stem and tuber.
In the present work, the six compounds of the Kedrostis foetidissima plant were tested for in silico ADMET profiling and drug-likeness properties using the Swiss ADME online web server and the pkCSM server. All the studied compounds are obeying Lipinski's rule of five except compounds 1 and 2, with two and three violations each. All the selected compounds from Kedrostis foetidissima have strong pharmacological activities. Supporting this, the selected plant methanol extracts of leaf, stem callus, and tuber have shown well in vitro antibacterial activity against Bacillus subtilis, Escherichia coli, and Proteus vulgaris.
Conclusion
Based on the physicochemical properties such as molecular weight and topological polar surface area (TPSA) whose upper limits are formulated by Lipinski’s rule of five and Veber’s filter. An orally active compound must pursue molecular weight under 500 g/mol, TPSA underneath 120 Å. The molecule 2 and 6 show more than 500 g/mol molecular weight and molecule 1,2 show more than 120 Å2 TPSA values. Compounds 3, 4, 5, and 6 obey Lipinski's rule of five except compound 1 and 2, with 2 and 3 violations each. Even though compound 1 and 2 can be used for drug development because they are biologically active natural products. The entire selected compounds have a good bioavailability score in a recommended range of 0 to 1. Compound 4 has high (0.85) and compounds 1 and 2 have low (0.17) oral bioavailability scores. Most of them show acceptable ADMET properties. Analysis of the Drug likeness and ADMET parameters for the selected compounds predicted good drug-like properties. Therefore, these compounds have agreeable pharmacological properties that can be developed as an oral drug candidate. In our results, among all the plant extracts studied, the methanol extract of stem callus showed the highest inhibition against all the selected organisms. This research also demonstrated the presence of medicinally significant bioactive components in the investigated plant, supporting their usage in traditional medicines for the treatment of various illnesses. These results suggest that they could be studied further for in vitro and in vivo studies for particular pharmacological activities and docking studies for specific proteins to develop as drug molecules.
Acknowledgements
The authors are thankful to Dr. G. Renuka, Assistant Professor of Chemistry, Department of Microbiology, Pingle Govt. College for Women (A), Hanumakonda, 506370, Telangana, India, for providing bacterial cultures.
Author contributions
Dr. Kommidi Saritha: Conceptualization, writing original draft, Investigation, Methodology, Writing. Dr. Muangala Alivelu: Software, Data curation, Formal analysis. Prof. Mustafa Mohammad: Review, Editing, Resources.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of interest
The authors declared that they have no known competing financial interests with respect to the research, authorship and/or publication of this article. The authors declare no competing interests.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abdul-Hammed M, Adedotun IO, Olajide M, Irabor CO, Afolabi TI, Gbadebo IO, Ramasami P (2022) Virtual screening, ADMET profiling, PASS prediction, and bioactivity studies of potential inhibitory roles of alkaloids, phytosterols, and flavonoids against COVID-19 main protease (Mpro). Nat Prod Res 36(12):3110–3116 10.1080/14786419.2021.1935933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alqahtani FY, Aleanizy FS, Mahmoud AZ, Farshori NN, Alfaraj R, Al-Sheddi ES, Alsarra IA (2019) Chemical composition and antimicrobial, antioxidant, and anti-inflammatory activities of Lepidium sativum seed oil. Saudi J Biol Sci 26(5):1089–1092 10.1016/j.sjbs.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amutha, M. (2017). (Doctoral thesis) Phytochemical biological pharmacological evaluation of Kedrostis foetidissima Jacq Cogn and plant mediated synthesis of metal nanoparticles. http://hdl.handle.net/10603/184784.
- Cai Y, Fang X, He C, Li P, Xiao F, Wang Y, Chen M (2015) Cucurbitacins: a systematic review of the phytochemistry and anticancer activity. Am J Chin Med 43(07):1331–1350 10.1142/S0192415X15500755 [DOI] [PubMed] [Google Scholar]
- Chai Y, Xiang K, Wu Y, Zhang T, Liu Y, Liu X, Si Y (2018) Cucurbitacin B inhibits the Hippo-YAP signaling pathway and exerts anticancer activity in colorectal cancer cells. Med Sci Monitor: Int Med J Exp Clin Res 24:9251–9258 10.12659/MSM.911594 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Chakrvarty HL (1982) Fascicles of flora of India. Botanical survey of India.
- Chan KT, Li K, Liu SL, Chu KH, Toh M, Xie WD (2010) Cucurbitacin B inhibits STAT3 and the Raf/MEK/ERK pathway in leukemia cell line K562. Cancer Lett 289(1):46–52 10.1016/j.canlet.2009.07.015 [DOI] [PubMed] [Google Scholar]
- Cheng F, Li W, Liu G, Tang Y (2013) In silico ADMET prediction: recent advances, current challenges and future trends. Curr Top Med Chem 13(11):1273–1289 10.2174/15680266113139990033 [DOI] [PubMed] [Google Scholar]
- Choene M, Motadi LR (2012) Anti-proliferative effects of the methanolic extract of Kedrostis foetidissima in breast cancer cell lines. Mol Biol 1(2):1–5 10.4172/2168-9547.1000107 [DOI] [Google Scholar]
- Daina A, Michielin O, Zoete V (2017) Swiss ADME: a free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci Rep 7(1):1–13 10.1038/srep42717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dogra KS, Chauhan S, Jalal JS (2015) Assessment of Indian medicinal plants for the treatment of asthma. J Med Plants Res 9(32):851–862 10.5897/JMPR2015.5890 [DOI] [Google Scholar]
- Flores-Holguín N, Frau J, Glossman-Mitnik D (2021) In silico pharmacokinetics, ADMET study and conceptual DFT analysis of two plant cyclopeptides isolated from rosaceae as a computational peptidology approach. Front Chem 9:708364 10.3389/fchem.2021.708364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girish HV, Satish S (2008) Antibacterial activity of important medicinal plants on human pathogenic bacteria-a comparative analysis. World Appl Sci J 5(3):267–271 [Google Scholar]
- Gullón B, Lú-Chau TA, Moreira MT, Lema JM, Eibes G (2017) Rutin: A review on extraction, identification and purification methods, biological activities and approaches to enhance its bioavailability. Trends Food Sci Technol 67:220–235 10.1016/j.tifs.2017.07.008 [DOI] [Google Scholar]
- (https://www.wildturmeric.net/home-remedy-for-abscess-appakovay-leaves/
- John Britto S (2019) The Flora of Central and North Tamil Nadu: Fabaceae - Loranthaceae (APG-IV) Part-2. The Rapinat Herbarium, St. Joseph’s College (Autonomous), Tiruchirappalli (India)
- Kalaisezhiyen P, Sasikumar V (2012) GC-MS evaluation of chemical constituents from methanolic leaf extract of Kedrostis foetidissima (Jacq.) Cogn. Asian J Pharm Clin Res 5(4):77–81 [Google Scholar]
- Kavitha N, Alivelu M (2021) Investigation of Structures, QTAIM, RDG, ADMET, and docking properties of SASC compound using experimental and theoretical approach. Comput Theor Chem 1201:113287 10.1016/j.comptc.2021.113287 [DOI] [Google Scholar]
- Kavitha N, Alivelu M, Konakanchi R (2022) Computational quantum chemical study, in silco ADMET, and molecular docking study of 2-Mercapto Benzimidazole. Polycyclic Aromat Compd 42(8):5534–5549 10.1080/10406638.2021.1939071 [DOI] [Google Scholar]
- Khan T, Dixit S, Ahmad R, Raza S, Azad I, Joshi S, Khan AR (2017) Molecular docking, PASS analysis, bioactivities score prediction, synthesis, characterization and biological activity evaluation of a functionalized 2-butanone thiosemicarbazone ligand and its complexes. J Chem Biol 10(3):91–104 10.1007/s12154-017-0167-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipinski CA, Lombardo F, Dominy BW, Feeney PJ (2001) Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Deliv Rev 46(3):3–26 10.1016/S0169-409X(00)00129-0 [DOI] [PubMed] [Google Scholar]
- Liu F (2016) Separation of flavonoids from stems and leaves of male plants in Trichosanthes kirilowii and study on their activity of scavenging DPPH free radical. Chin Tradit Herbal Drugs 24:4141–4145 [Google Scholar]
- Malabadi RB, Naik SL, Meti NT, Mulgund GS, Nataraja K, Kumar SV (2012) Silver nanoparticles synthesized by in vitro derived plants and callus cultures of Clitoria ternatea; evaluation of antimicrobial activity. Res Biotech 3(5):26–38 [Google Scholar]
- Martin YC (2005) A bioavailability score. J Med Chem 48(9):3164–3170 10.1021/jm0492002 [DOI] [PubMed] [Google Scholar]
- Mothana RA, Al-Musayeib NM, Al-Ajmi MF, Cos P, Maes L (2014) Evaluation of the in vitro antiplasmodial, antileishmanial, and antitrypanosomal activity of medicinal plants used in Saudi and Yemeni traditional medicine. Evid-Based Complementary Altern Med 2014:1–7 10.1155/2014/905639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugomeri E, Chatanga P, Raditladi T, Makara M, Tarirai C (2016) Ethnobotanical study and conservation status of local medicinal plants: towards a repository and monograph of herbal medicines in Lesotho. Afr J Tradit Complement Altern Med 13(1):143–156 10.4314/ajtcam.v13i1.20 [DOI] [Google Scholar]
- Murugesan S, Venkateswaran MR, Jayabal S, Periyasamy S (2020) Evaluation of the antioxidant and anti-arthritic potential of Zingiber officinale Rosc.by in vitro and in silico analysis. S Afr J Bot 130:45–53 10.1016/j.sajb.2019.12.019 [DOI] [Google Scholar]
- Njoroge GN, Newton LE (1994) Edible and poisonous species of cucurbitaceae in the central highlands of Kenya. J East Afr Nat Hist 83(2):101–115 10.2982/0012-8317(1994)83[101:EAPSOC]2.0.CO;2 [DOI] [Google Scholar]
- Pavithra K, & Saravanan G (2019) Antioxidant potential of crude phenolic fraction from Kedrostis foetidissima (Jacq.) Cogn. leaves. KS Rangasamy college of arts and science (autonomous), 15. Proceeding of National Conference on “Translating the Science of Nutrition into Art of Healthy Living” (TSNAHL) January 30th & 31st 2019
- Pires DE, Blundell TL, Ascher DB (2015) pkCSM: predicting small-molecule pharmacokinetic and toxicity properties using graph-based signatures. J Med Chem 58(9):4066–4072 10.1021/acs.jmedchem.5b00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priyavardhini S, Gowri SS, Vasantha K, Umadevi M (2008) Antibacterial activity of stem and leaf extract of Kedrostis foetidissima (Jacq.) Cogn. Ancient Sci Life 28(2):10 [PMC free article] [PubMed] [Google Scholar]
- Priyavardhini S, Vasantha K, Tresina Soris P, Mohan VR (2012) Antifungal activity of Kedrostis foetidissima (Jacq.) Cogn. Int J Pharm Tech Res 4(1):44–48 [Google Scholar]
- Raffa D, Maggio B, Raimondi MV, Plescia F, Daidone G (2017) Recent discoveries of anticancer flavonoids. Eur J Med Chem 142:213–228 10.1016/j.ejmech.2017.07.034 [DOI] [PubMed] [Google Scholar]
- Rahman F, Tabrez S, Ali R, Alqahtani AS, Ahmed MZ, Rub A (2021) Molecular docking analysis of rutin reveals possible inhibition of SARS-CoV-2 vital proteins. J Tradit Complement Med 11(2):173–179 10.1016/j.jtcme.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raja MJ, Arivuchelvan A, Jagadeeswaran A (2019) Evaluation of antibacterial activity of Kedrostis foetidissima (Jacq.) Cogn. plant extracts against pathogens causing bovine mastitis. J Pharmacogn Phytochem 8(1):452–455 [Google Scholar]
- Rios JL, Escandell JM, Recio MC (2005) New insights into the bioactivity of cucurbitacins. Stud Nat Prod Chem 32:429–469 10.1016/S1572-5995(05)80062-6 [DOI] [Google Scholar]
- Sangeetha K, Purushothaman I, Rajarajan S (2017) Spectral characterization, antiviral activities, in silico ADMET and molecular docking of the compounds isolated from tectona grandis to chikungunya virus. Biomed Pharmacother 87:302–310 10.1016/j.biopha.2016.12.069 [DOI] [PubMed] [Google Scholar]
- Sepay N, Sekar A, Halder UC, Alarifi A, Afzal M (2021) Anti-COVID-19 terpenoid from marine sources: a docking, admet and molecular dynamics study. J Mol Struct 1228:129433 10.1016/j.molstruc.2020.129433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shariff N, Sudarshana MS, Umesha S, Hariprasad P (2006) Antimicrobial activity of Rauvolfia tetraphylla and Physalis minima leaf and callus extracts. Afr J Biotech 5(10):946–950 [Google Scholar]
- Sivaprakash, V. (2016) Antidiarrheal activity of Kedrostis Foetidissima leaf extract on experimentally induced diarrhea in mice. (Doctoral dissertation, Nandha College of Pharmacy, Erode)
- Thenmozhi K, Karthika K, Manian S (2014) Pharmacognostical and preliminary phytochemical screening of the leaves of Kedrostis foetidissima (Jacq.) Cogn. Kongunadu Res J 1(2):112–115 10.26524/krj50 [DOI] [Google Scholar]
- Ueno M, Kariya R, Sittithumcharee G, Okada S (2021) Cucurbitacin B induces apoptosis of primary effusion lymphoma via disruption of cytoskeletal organization. Phytomedicine 85:153545 10.1016/j.phymed.2021.153545 [DOI] [PubMed] [Google Scholar]
- Valgas C, Souza SMD, Smânia EF, Smânia A Jr (2007) Screening methods to determine antibacterial activity of natural products. Braz J Microbiol 38(2):369–380 10.1590/S1517-83822007000200034 [DOI] [Google Scholar]
- Van De Waterbeemd H, Gifford E (2003) ADMET in silico modelling: towards prediction paradise? Nat Rev Drug Discovery 2(3):192–204 10.1038/nrd1032 [DOI] [PubMed] [Google Scholar]
- Vladimir M, Nenad V, Neda N, Slavica S, Milan M, Pavle MK, Milan SS (2011) Studies on the antimicrobial activity and chemical composition of the essential oils and alcoholic extracts of Gentiana asclepiadea L. J Med Plants Res 5(7):1164–1174 [Google Scholar]
- Zackria AA, Pattabiraman R, Murthy TP, Kumar SB, Mathew BB, Biju VG (2022) Computational screening of natural compounds from Salvia plebeia R. Br. for inhibition of SARS-CoV-2 main protease. Vegetos 35(2):345–359 10.1007/s42535-021-00304-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang MQ, Wilkinson B (2007) Drug discovery beyond the ‘rule-of-five.’ Curr Opin Biotechnol 18(6):478–488 10.1016/j.copbio.2007.10.005 [DOI] [PubMed] [Google Scholar]
- Zhang J, Zhou L, Cui L, Liu Z, Wei J, Kang W (2020) Antioxidant and α-glucosidase inhibitory activity of Cercis chinensis flowers. Food Sci Human Wellness 9(4):313–319 10.1016/j.fshw.2020.04.003 [DOI] [Google Scholar]
- Zhao M, Ma J, Li M, Zhang Y, Jiang B, Zhao X, Qin S (2021) Cytochrome P450 enzymes and drug metabolism in humans. Int J Mol Sci 22(23):12808 10.3390/ijms222312808 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.