Abstract
Introduction
Determining limb length in gastric bypass procedures is a crucial step to ensure significant weight loss without risking malnutrition. This study investigated the effect of ex vivo training on the skills needed to determine limb lengths.
Materials and Methods
This was a single-center ex vivo training experiment in a teaching hospital in the Netherlands. We designed a training exercise with marked ropes in a laparoscopic trainer box. All ten surgical residents participated and practiced the skill of estimating limb length. Before and after the two-week period their results on a 150-centimeter limb length task were evaluated.
Results
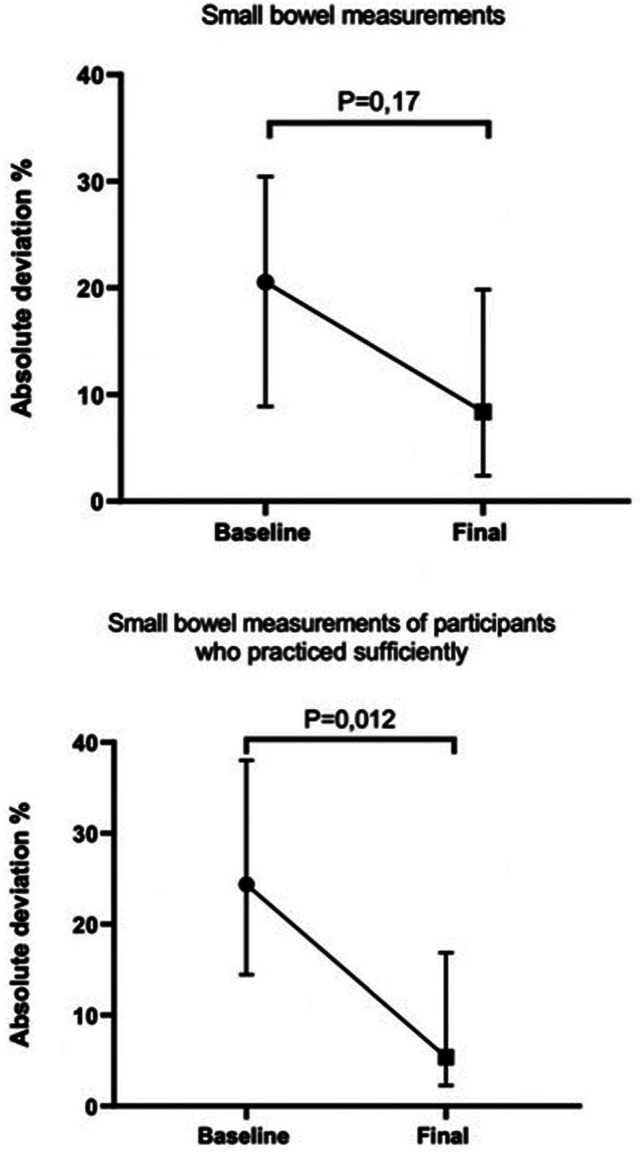
Before training, 10 surgical residents estimated 150 centimeters of small bowel with an absolute deviation of 21% [range 9-30]. After the training experiment, the residents measured with 8% [2-20] deviation (P = .17). The 8 residents who trained sufficiently improved statistically significantly to an absolute deviation of 5% [2-17] (P = .012). Over 70% of the participants felt their skills had improved.
Conclusions
With sufficient training, surgical residents’ skills in measuring small bowel length improved when tested in an ex vivo model. Residents became more confident in their laparoscopic measurement skills. This ex vivo training model is a alternative and addition to on-site training.
Keywords: gastric bypass, bowel measurement, small bowel length, laparoscopic training, technical skills
Introduction
Laparoscopic gastric bypass procedures such as Roux-en-Y gastric bypass (RYGB) and one anastomosis gastric bypass (OAGB) are common surgical procedures for patients with morbid obesity and metabolic disorders.1,2 Although these procedures are widely studied, still no consensus exists on the optimal lengths of the alimentary and biliopancreatic limbs in the RYGB and OAGB. Both too-long and too-short limb lengths may have clinical consequences and reduce the effect of the bypass or induce side effects, such as nutritional deficiencies and steatorrhea.3-5
Only a few studies investigated the accuracy of laparoscopic measurement of the small bowel, showing wide variability in the estimated lengths both in the hands of surgeons and residents. While the clinical implications of inaccurate bowel length measurements have not been investigated, studies have indicated that the magnitude of the discrepancies is noteworthy, with deviation ranging from 34 to 50 cm when the intended length is 150 cm.6,7 Research regarding limb length may produce inadequate or irreproducible results if bowel length measurements are not precise, emphasizing the relevance of this issue.
In many bariatric centers, a stepwise hand-over-hand technique is used to estimate limb lengths. With this technique, marked graspers are used as reference points to estimate the length of the bypassed bowel. 8 Recently, our bariatric center performed an ex vivo experiment to analyze the accuracy and variability of small bowel measurements in our bariatric surgeons and surgical residents. 9 Our study showed that bariatric surgeons measured bowel length with on average less than 10% deviation from the goal lengths, but surgical residents structurally underestimated limb lengths, with a much wider spread. These results support the study of Jackson et al, who also found residents underestimated laparoscopic measured limb lengths. 7
Several studies have been published on ex vivo training of laparoscopic bariatric skills, including augmented reality simulation, human cadaver and animal models, and box trainers.10-15 However, to our knowledge, no literature is available about how to practice or train these methods of laparoscopic small bowel measurement. As running the small bowel is a basic skill, used in other procedures as well, it is important for residents to acquire the skill of accurate estimation of bowel length. Handling the small bowel to make a measurement or estimate the length requires tissue handling skills, accuracy, and a certain speed to avoid delay in the procedure. Training of fellows and residents during gastric bypass procedures may affect the quality and costs of the operations.16-18 A sufficient ex vivo training method could result in a reduction of the learning curve in the operating room.
This emphasizes that research is necessary to investigate how accurate laparoscopic measurement of the small bowel can be practiced and learned. This study aimed to investigate if the accurate laparoscopic measurement of the small bowel length can be learned to surgical residents through an ex vivo training experiment.
Materials and Methods
A laparoscopic training exercise was designed to train the skill of laparoscopic bowel length measurement. Laparoscopic small bowel measurement was simulated using a laparoscopic box trainer with the intestine of a porcine cadaver. The use of animal by-products was approved by the Netherlands Food and Consumer Product Safety Authority. In the Netherlands, no ethical approval is required for animal cadaver studies.
Participants
Ten surgical residents were asked to participate and provided informed consent. Baseline data of all participants including age, gender, and laparoscopic and bariatric experience were collected. None of the participants performed a complete laparoscopic gastric bypass before entering the study, neither supervised nor unsupervised. To ensure adequate knowledge of the techniques used, the participants were sent an instruction video including a fragment of the bowel length measurement during laparoscopic gastric bypass surgery.
Study Design
This is a single-center ex vivo training experiment in a large peripheral teaching hospital, including all surgical residents working at the hospital during the study period from 2021 to 2022. For this type of study, no ethical approval is required in the Netherlands.
Laparoscopic Training Exercise
A laparoscopic box training system (Lapstar model 2, Camtronics B.V. Son, the Netherlands) with a fixed camera and two graspers was used to simulate the measurement of the small bowel. With a stepwise hand-over-hand technique using one marked grasper, the measurement was run in estimated steps of 5 cm. This method of bowel length measurement was described before by Slagter et al. 9
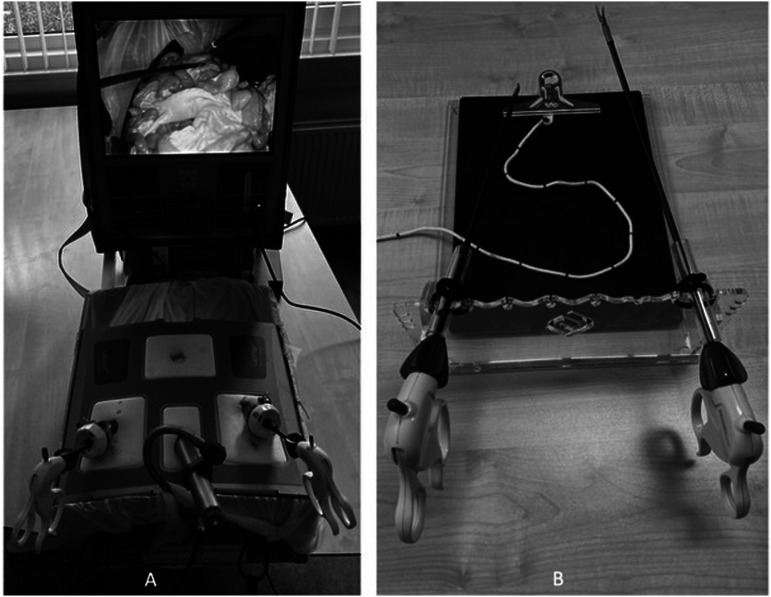
For the baseline measurement, the entire small bowel of a porcine cadaver including its mesentery was placed in the laparoscopic box (Figure 1A). All participants were asked to measure a small bowel segment of 150 cm on the porcine intestine three times in a row. Each endpoint of a measurement was used as a starting point for the next measurement, to blind participants from their previous results. Next, the participants repeated these three 150 cm measurements on an unmarked rope in the laparoscopic box trainer. For all measurements on the small bowel, the time spent on the task was recorded. After the measurements on both porcine intestine and rope, the actual length of the marked segments was determined by the observer, using a tape measure outside the laparoscopic box, avoiding any traction on the porcine bowel during this tape measurement. The length of the porcine intestine was measured twice, and the mean of the two tape measure lengths was used as the actual measured length. The participants received feedback about the estimated lengths they performed on the small bowel and rope. Next, the participants were given a mini box trainer rope model with two training exercises to train their skills for two weeks. They received both verbal instruction and an instruction video to train at least once, but preferably three times, for at least 15 minutes during each week of the training experiment.
Figure 1.
(A) Laparoscopic box trainer. (B) Mini box trainer to practice at home.
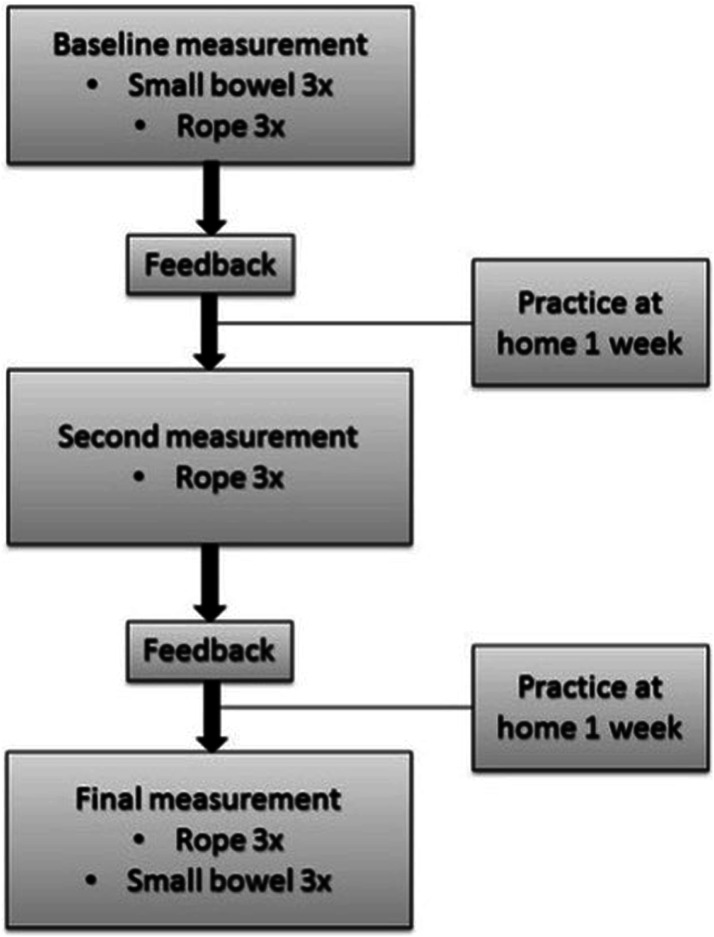
A second measurement evaluation was made after one week of practice. The participants were now asked to perform three repeated measurements of 150 cm on a rope in the laparoscopic box trainer. The participants again received feedback about their estimated lengths. After another week of practice at home, again three times a week, the final measurements were done on both porcine small bowel and rope in the laparoscopic box. This training model is summarized in Figure 2.
Figure 2.
Training protocol.
After completion of the training experiment, the participants were invited to give their opinion of the training method via a short questionnaire. The questionnaire comprised five statements that had to be rated on a 5-point Likert scale.
Mini Box Trainer Exercise
The plexiglass Alphatron Surgical box trainer without a camera was used as a base for two laparoscopic graspers (Medtronic). Two training exercises were designed to practice adequate length estimation. In both exercises a 3-meter-long rope was placed in the mini box, fixed at its starting point to simulate Treitz’s ligament. In the first exercise a marked rope was used (Figure 1B), marked every 5 cm in the first 50 cm, marked every 10 cm in the next 50 cm, and finally marked every 50 cm for the remainder of the rope. In the second exercise, an unmarked rope was used, with the instruction to estimate a 150 cm length and validate their measurement with a measuring tape, providing feedback on their estimation skills.
Statistics
Given the small sample size and skewed distribution, measured values were presented as median [interquartile range]. Individual percentages of absolute deviation from the goal length were calculated. Both rope and bowel measurements were repeated three times at each time point. The mean absolute deviation of these three measurements was used for analyses. The rope measurements were compared using the Friedman test. Wilcoxon Signed Rank test was used to conduct a paired difference test of the repeated bowel measurements and results are reported as P-value and Z statistics. To analyze the effect of the training experiment, a separate analysis was performed for the participants with sufficient practice. Participants who did not meet our minimum criteria of practice (one time a week for at least 15 minutes) were excluded from this analysis. Acceptable variation in small bowel length measurement was defined as between the lower and upper margin of 10% deviation from the actual bowel length. A two-sided P-value of ≤.05 was considered statistically significant. Statistical analyses were performed in SPSS version 24.
Results
Baseline characteristics of the participants are shown in Table 1. Two participants did not practice during the first week of the training experiment. As shown in Table 2, the residents estimated the baseline rope measurements with an absolute deviation of 10% [5-22] from the goal length. Second and final rope measurements showed similar results of 9 [6-21] and 11% [7-18] deviation (P = 1.0). The duration of the rope measurements was similar at the start, during, and after the training experiment (P = .5).
Table 1.
Participant Demographics.
| Sex | Age | Lap Experience | Days of training | Minutes of training | |
|---|---|---|---|---|---|
| Resident 1 | Male | 31 | 10 | 1 | 15 |
| Resident 2 | Male | 34 | 80 | 2 | 30 |
| Resident 3 | Female | 31 | 0 | 3 | 50 |
| Resident 4 | Female | 25 | 0 | 4 | 60 |
| Resident 5 | Female | 34 | 80 | 4 | 60 |
| Resident 6 | Male | 31 | 2 | 4 | 60 |
| Resident 7 | Male | 29 | 0 | 4 | 80 |
| Resident 8 | Female | 28 | 0 | 6 | 95 |
| Resident 9 | Female | 32 | 75 | 6 | 96 |
| Resident 10 | Male | 31 | 30 | 7 | 100 |
Lap experience, laparoscopic experience expressed as number of individually performed laparoscopic surgeries.
Table 2.
Measurements Laparoscopic Training Experiment.
| Rope Baseline | Rope second | Rope Final | Small Bowel Baseline | Small Bowel Final | |
|---|---|---|---|---|---|
| N | 10 | 10 | 10 | 10 | 10 |
| Absolute deviation, cm | 16 [7-33] | 14 [10-32] | 17 [11-28] | 31 [13-46] | 13 [4-30] |
| Absolute deviation, % | 10 [5-22] | 9 [6-21] | 11 [7-18] | 21 [9-30] | 8 [2-20] |
| Between margins 10% | 14 of 30 | 16 of 30 | 13 of 30 | 11 of 30 | 19 of 30 |
| Outside 15% margins | 10 of 30 | 10 of 30 | 9 of 30 | 18 of 30 | 9 of 30 |
| Time, min | 1:43 | 2:08 | 1:48 | 2:29 | 2:01 |
Values are median [interquartile range].
At baseline, surgical residents estimated small bowel length with an absolute deviation of 21% [9-30] (Figure 3). After completing the training experiment, all residents combined estimated bowel length with an absolute deviation of 8% [2-20]. However, this difference of 13% was not statistically significant (Z = −1.38, P = .17). As shown in Figure 3B, residents with sufficient practice of at least 15 minutes in each week of the study (n = 8) estimated the baseline bowel measurements with an absolute deviation of 24% [14-38]. These residents improved their measurements statistically significantly to 5% [2-17] deviation after the training experiment (Z = −2.5, P = .012). In total, the surgical residents estimated baseline measurements 11 of 30 times (37%) between the acceptable lower and upper margins of 10% deviation. After the training experiment, the residents estimated 19 of 30 times (63%) between the 10% margins. Baseline bowel measurement time was 2:29 minutes, which did not significantly differ from the time of 2:01 minutes after the training experiment (P = .28).
Figure 3.
The percentage absolute deviation of the baseline and final bowel measurements is expressed as median and interquartile range. (A) Measurement results before and after the training program were compared for all residents (Z = −1.38, P = .17). (B) Measurement results of the participants with sufficient practice (N = 8) before and after the training experiment were compared (Z = −2.5, P = .012). Sufficient practice was defined as practicing at least one time each week.
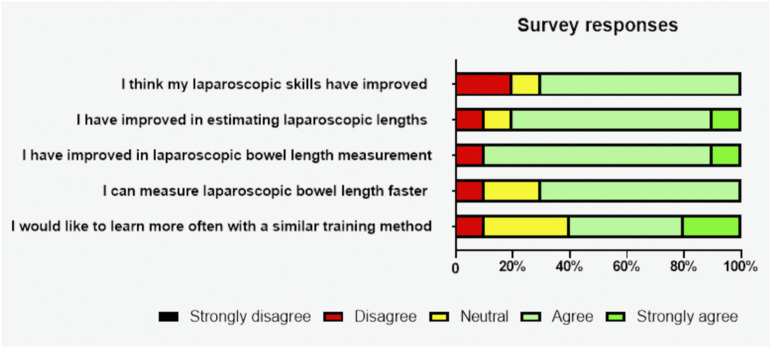
The results of the survey are shown in Figure 4. The survey shows that 70% of the participants agreed that their laparoscopic skills improved by the training experiment and that they were able to measure laparoscopic bowel length faster. Furthermore, 90% agreed that they improved in laparoscopic bowel length measurement after the training experiment. Of all participants, 60% would like to learn more often with a similar training method, while 30% answered neutrally on that question.
Figure 4.
Participant responses to the survey questionnaire by Likert scale.
Discussion
The results of this study show that after completing the training experiment, in total the surgical residents were able to improve their laparoscopic small bowel measurements by 13%, however, this difference was not statistically significant. Residents who practiced sufficiently improved significantly and were able to measure small bowel length with only 5% deviation from the goal length.
The lack of statistical significance of the 13% reduction is probably due to the small sample size. In a subgroup analysis of residents who did practice sufficiently, the reduction was significant, which strengthens the relevance of practice. In a previous study, a ten percent or less deviation of the goal length was defined as acceptable, as these differences may not have clinical implications. 9 With only 5% deviation, surgical residents measured small bowel length with an acceptable deviation from the goal length.
An earlier review by Thingaard et al showed that a take-home trainer box facilitated off-site training by making it accessible to residents. 19 Moreover, other research has shown that in obtaining procedural, including surgical, skills distributed practice leads to more and more durable training effects compared to massed practice.19-21 Participants in our experiment were therefore instructed to practice at least every week of the experiment.
Even with these low demands on training time, not all participants managed to find time for adequate practice. Clinical duties, on-call hours, and additional tasks during the COVID-19 outbreak interfered. However, even with these limited amounts of training a significant effect was found on the accuracy of limb length measurement. This may encourage residents to find a little time to practice their skills as even a small amount of practice shows to be beneficial. This is supported by the results of our questionnaire, in which over 70% of residents responded they feel their skills have improved during the study period.
A remarkable result of our study is that although the small bowel measurements on the porcine bowel specimen significantly improved, the measurements of the rope did not improve over time. This observation could be explained by the specific characteristics of the cord, its stiffness, length, and thickness. The pros of this small cord are its accessibility, low costs, and haptic feedback when grasping it compared to a lint for example. The use of a different exercise tool, such as the cotton bowel used by Wagner et al. may be subject of further research to not only exercise the task but also assess the trainee’s skills ex vivo. 14 As an alternative, the porcine small bowel model used in this experiment as well as other studies could be used to assess the residents’ skills. 12
The presented study focuses on the accuracy of the trainee’s measurement. However, handling the small bowel to estimate limb length requires multiple subskills; accuracy, tissue handling, and speed. Obtaining some speed may be a side-effect of this exercise, but it was not the goal. A reduction of the time needed to estimate 150 cm bowel length was observed, from circa 2.5 to 2 minutes, however this was not statistically significant. Tissue handling was not trained or measured, this part of the skill should still be trained in vivo or obtained otherwise.
To our knowledge, this is the first study creating a training experiment to train surgical residents in laparoscopic small bowel measurement. The learning curve of a gastric bypass procedure comprises 30-200 cases, depending on the definition of the endpoint of the learning curve. 22 During this learning curve operative times are longer and complication rates are higher. 17 However, the learning curve can be shorter if the different skills needed are already mastered. As Buchwald and Scopinaro have stated: all techniques needed in the sub-steps of the procedures can and have to be mastered in the surgical training program. 23 This ex vivo training method with box trainers is a simple, easy to implement, and low in costs method to train residents in laparoscopic small bowel measurements. It can be implemented in teaching hospitals to train surgical residents. With high demands on operative quality and costs, ex vivo training is a relevant alternative and addition to on-site training. Further research is necessary to optimize training methods to be able to train more of the gastric bypass sub-steps using an ex vivo model.
A limitation in the design is that the box trainer does not use a laparoscopic camera, but the graspers and cord are manipulated under direct sight. This excludes the magnification of the camera and gives 3D instead of 2D sight. However, the use of marked cords was designed to train the motoric memory in a hand-over-hand technique with 5 cm step intervals. These 5 cm difference in spatial position between the two graspers stays the same, regardless of the viewpoint of the trainee, in 2D, 3D, and different magnifications. Using a plexiglass assembly box makes it possible to be used multiple times, at low cost, and can be used to practice at home next to a laparoscopic box with a camera system. Another limitation was the small sample size of the study including only 10 surgical residents in the study. Nevertheless, due to the high percentage of improvement in the residents who adhered to the training this sample size was sufficient to show significant differences. Additionally, the actual clinical consequences of inaccurate bowel length measurements on the outcomes after gastric bypass have not been investigated. However, a comparison of the findings of this study with existing literature has revealed that small bowel length deviations range from 21 to 36%. Intended limb lengths of 150 or 180 cm can result in a final length that exceeds 200 cm. This might have clinical implications as studies have shown limb lengths of more than 200 cm are associated with a higher incidence of nutritional deficiencies. 24
Conclusion
This study shows that with sufficient training using an ex vivo model with a box trainer, surgical residents improved their skill of laparoscopic small bowel length measurement. Moreover, 70% of residents feel their skills have improved by practicing this specific task, which is a key step in gastric bypass procedures. With high demands on operative quality and costs, this ex vivo training experiment is a relevant alternative and addition to on-site training.
Footnotes
Author Contributions: All authors were involved in the conception and design of the study. NS and MK performed the study and wrote the manuscript. All authors critically read, revised, and approved the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Mirjam A. Kaijser https://orcid.org/0000-0003-1243-9603
References
- 1.DeMaria EJ, Pate V, Warthen M, Winegar DA. Baseline data from American society for metabolic and bariatric surgery-designated bariatric surgery centers of excellence using the bariatric outcomes longitudinal database. Surgery for Obesity and Related Diseases. 2010;6(4):347-355. doi: 10.1016/j.soard.2009.11.015 [DOI] [PubMed] [Google Scholar]
- 2.Ramos AC, Chevallier JM, Mahawar K, et al. IFSO (international federation for surgery of obesity and metabolic disorders) consensus conference statement on one-anastomosis gastric bypass (OAGB-MGB): results of a modified delphi study. Obes Surg. 2020;30(5):1625. doi: 10.1007/s11695-020-04519-y, Published online. [DOI] [PubMed] [Google Scholar]
- 3.Zorrilla-Nunez LF, Campbell A, Giambartolomei G, Lo Menzo E, Szomstein S, Rosenthal RJ. The importance of the biliopancreatic limb length in gastric bypass: a systematic review. Surgery for Obesity and Related Diseases. 2019;15(1):43-49. doi: 10.1016/j.soard.2018.10.013 [DOI] [PubMed] [Google Scholar]
- 4.Mahawar KK, Parmar C, Carr WRJ, Jennings N, Schroeder N, Small PK. Impact of biliopancreatic limb length on severe protein-calorie malnutrition requiring revisional surgery after one anastomosis (mini) gastric bypass. J Minim Access Surg. 2018;14(1):37-43. doi: 10.4103/jmas.JMAS_198_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahuja A, Tantia O, Goyal G, Chaudhuri T, Khanna S, Poddar A. MGB-OAGB : effect of biliopancreatic limb length on nutritional deficiency, Weight Loss, and Comorbidity Resolution; 2018;28:3439-3445. Published online. [DOI] [PubMed] [Google Scholar]
- 6.Gazer B, Rosin D, Bar-Zakai B, et al. Accuracy and inter-operator variability of small bowel length measurement at laparoscopy. Surg Endosc. 2017;31(11):4697-4704. doi: 10.1007/s00464-017-5538-5 [DOI] [PubMed] [Google Scholar]
- 7.Jackson HT, Zettervall SL, Teitelbaum EN, et al. Effects of experience and reference tools on laparoscopic length measurements. Surg Endosc. 2015;29(6):1297-1302. doi: 10.1007/s00464-014-3802-5 [DOI] [PubMed] [Google Scholar]
- 8.Isreb S, Hildreth A, Mahawar K, Balupuri S, Small P. Laparoscopic instruments marking improve length measurement precision. World Journal of Laparoscopic Surgery with DVD. 2009;2(December):57-60. doi: 10.5005/jp-journals-10007-1038 [DOI] [Google Scholar]
- 9.Slagter N, van Wilsum M, de Heide LJM, et al. Laparoscopic small bowel length measurement in bariatric surgery using a hand-over-hand technique with marked graspers: an ex vivo experiment. Obes Surg. 2022;32(4):1201-1208. doi: 10.1007/s11695-022-05918-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thuler FR, De Freitas WR, Ilias EJ, Kassab P, Malheiros CA. Laparoscopic bariatric surgery training program model: gastric bypass. BMC Surg. 2014;14(1):101. doi: 10.1186/1471-2482-14-101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giger U, Frésard I, Häfliger A, Bergmann M, Krähenbühl L. Laparoscopic training on Thiel human cadavers: a model to teach advanced laparoscopic procedures. Surgical Endoscopy and Other Interventional Techniques. 2008;22(4):901-906. doi: 10.1007/s00464-007-9502-7 [DOI] [PubMed] [Google Scholar]
- 12.Varas J, Mejía R, Riquelme A, et al. Significant transfer of surgical skills obtained with an advanced laparoscopic training program to a laparoscopic jejunojejunostomy in a live porcine model: feasibility of learning advanced laparoscopy in a general surgery residency. Surg Endosc. 2012;26(12):3486-3494. doi: 10.1007/s00464-012-2391-4 [DOI] [PubMed] [Google Scholar]
- 13.Zimmerman H, Latifi R, Dehdashti B, et al. Intensive laparoscopic training course for surgical residents: program description, initial results, and requirements. Surg Endosc. 2011;25(11):3636-3641. doi: 10.1007/s00464-011-1770-6 [DOI] [PubMed] [Google Scholar]
- 14.Wagner M, Mayer BFB, Bodenstedt S, et al. Comparison of conventional methods for bowel length measurement in laparoscopic surgery to a novel computer-assisted 3D measurement system. Obes Surg. 2021;31(11):4692-4700. doi: 10.1007/s11695-021-05620-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aggarwal R, Boza C, Hance J, Leong J, Lacy A, Darzi A. Skills acquisition for laparoscopic gastric bypass in the training laboratory - an innovative approach. Obes Surg. 2007;17(1):19-27. doi: 10.1007/s11695-007-9001-x [DOI] [PubMed] [Google Scholar]
- 16.Bridges M, Diamond DL. The financial impact of teaching surgical residents in the operating room. The american journal of surgery. 1999;177:28. [DOI] [PubMed] [Google Scholar]
- 17.Birkmeyer JD, Finks JF, O’Reilly A, et al. Surgical skill and complication rates after bariatric surgery. New England Journal of Medicine. 2013;369(15):1434-1442. doi: 10.1056/nejmsa1300625 [DOI] [PubMed] [Google Scholar]
- 18.Babineau TJ, Becker J, Gibbons G, et al. The “cost” of operative training for surgical residents. Arch Surg. 2004. Published online https://www.archsurg.com [DOI] [PubMed] [Google Scholar]
- 19.Thinggaard E, Kleif J, Bjerrum F, et al. Off-site training of laparoscopic skills, a scoping review using a thematic analysis. Surg Endosc. 2016;30(11):4733-4741. doi: 10.1007/s00464-016-4834-9 [DOI] [PubMed] [Google Scholar]
- 20.Cnossen F. Cognitive skills in medicine: an introduction. In: PanVascular Medicine. Berlin Heidelberg: Springer; 2015:4719-4752. doi: 10.1007/978-3-642-37078-6_181 [DOI] [Google Scholar]
- 21.Broekema TH, Talsma AK, Wevers KP, Pierie JPEN. Laparoscopy instructional videos: the effect of preoperative compared with intraoperative use on learning curves. J Surg Educ. 2017;74(1):91-99. doi: 10.1016/j.jsurg.2016.07.001 [DOI] [PubMed] [Google Scholar]
- 22.Wehrtmann FS, de la Garza JR, Kowalewski KF, et al. Learning curves of laparoscopic roux-en-Y gastric bypass and sleeve Gastrectomy in bariatric surgery: a systematic review and introduction of a standardization. Obes Surg. 2020;30(2):640-656. doi: 10.1007/s11695-019-04230-7 [DOI] [PubMed] [Google Scholar]
- 23.Buchwald H, Scopinaro N. Retiring the learning curve. Obes Surg. 2009;19(5):541-542. doi: 10.1007/s11695-009-9833-7 [DOI] [PubMed] [Google Scholar]
- 24.Tasdighi E, Barzin M, Mahawar KK, et al. Effect of biliopancreatic limb length on weight loss, postoperative complications, and remission of comorbidities in one anastomosis gastric bypass: a systematic review and meta-analysis. Obes Surg. 2022;32(3):892-903. doi: 10.1007/s11695-021-05848-2 [DOI] [PubMed] [Google Scholar]