Abstract
Background
Due to the high burden of mortality from acute communicable and non-communicable diseases, emergency department’s mortality has become one of the major health indices in Ethiopia that should be evaluated regularly in every health institution. However, there are inconsistencies between studies, and there is no systematic review or meta-analysis study about the prevalence of mortality in the emergency department. Therefore, this study aimed to determine the pooled prevalence of mortality and identify its determinants in the emergency departments of Ethiopian hospitals.
Methods
This systematic review was conducted according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and has been registered with PROSPERO. A structured search of databases (Medline/PubMed, Google Scholar, CINAHL, EMBASE, HINARI, and Web of Science) was undertaken. All observational studies reporting the prevalence of mortality of patients in emergency departments of Ethiopian hospitals, and published in English up to December 16, 2023, were considered for this review. Two reviewers independently assess the quality of the studies using the Joanna Briggs Institute (JBI) critical appraisal tool. A meta-analysis using a random-effects model was performed to estimate the pooled prevalence. The heterogeneity of studies was assessed using I2 statistics, and to identify the possible causes of heterogeneity, subgroup analysis and meta-regression were used. Egger’s test and funnel plots were used to assess publication bias. STATA version 17.0 software was used for all the statistical analyses. A p-value less than 0.05 was used to declare statistical significance.
Results
A total of 1363 articles were retrieved through electronic search databases. Subsequently, eighteen studies comprised 21,582 study participants were included for analysis. The pooled prevalence of mortality among patients in the Emergency Department (ED) was 7.71% (95% CI: 3.62, 11.80). Regional subgroup analysis showed that the pooled prevalence of mortality was 16.7%, 12.89%, 10.28%, and 4.35% in Dire Dawa, Amhara, Oromia, and Addis Ababa, respectively. Moreover, subgroup analysis based on patients’ age revealed that the pooled prevalence of mortality among adults and children was 8.23% (95% CI: 3.51, 12.94) and 4.48% (95% CI: 2.88, 6.08), respectively. Being a rural resident (OR; 2.30, 95% CI: 1.48, 3.58), unconsciousness (OR; 3.86, 95% CI: 1.35, 11.04), comorbidity (OR; 2.82, 95% CI: 1.56, 5.09), and time to reach a nearby health facility (OR; 4.73, 95% CI: 2.19, 10.21) were determinants of mortality for patients in the emergency departments.
Conclusion and recommendations
This study found that the overall prevalence of mortality among patients in emergency departments of Ethiopian hospitals was high, which requires collaboration between all stakeholders to improve outcomes. Being a rural resident, unconsciousness, comorbidity, and time elapsed to reach health facilities were determinants of mortality. Improving pre-hospital care, training healthcare providers, early referral, and improving first-line management at referral hospitals will help to reduce the high mortality in our country.
Keywords: Associated factors, Emergency department, Ethiopia, Meta-analysis, Mortality
Background
The emergency department provides services for patients with conditions that are life-threatening or potentially life-threatening over 24 h a day and 365 days a year [1]. It is considered the backbone of health facilities and the general public by providing the first line of care upon arrival [2]. Patient mortality in Emergency Departments (ED) is a major public health problem that has aggravated in recent years [3].
The global estimate of ED mortality was 15–16%, and most of the ED deaths occur in low- and middle-income countries with scarce resources [4, 5]. The major causes of this mortality are traffic accidents, cardiovascular disease, trauma, and respiratory problems [3, 6–8]. Most emergency department mortality occurred within the first three days; the majority of these deaths are avoidable with proper intervention [8].
The World Health Organization (WHO) recommends all countries, regardless of resources or economic development, to start by establishing a comprehensive emergency care system and to monitor progress on a regular basis [9]. Because of this, emergency services are receiving more attention in Africa, where the burden of mortality from acute communicable and non-communicable diseases is still significant [10].
According to the Ethiopian Hospital Services Transformation Guideline, emergency patients should be able to access the triage area without the hindrance of their financial capacity and/or security guard [1]. Furthermore, the Ethiopian Federal Ministry of Health (EMOH) has striven to improve access to emergency care through sustainable, effective, and quality care provided by trained healthcare providers [1, 11]. Emergency room mortality has to be one of the emergency medical services indicators in Ethiopia, which should be lower than 1.5% by 2024 [1]. However, there are inconsistencies between studies, and there is no systematic review or meta-analysis study that reveals the pooled prevalence of mortality among emergency department patients. Therefore, this review and meta-analysis aimed to synthesize relevant and reliable evidence on the prevalence and determinant factors of mortality in emergency departments in Ethiopia.
Methods
Protocol and registration
The plan for conducting this review has been pre-registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the unique identification number (UIN): review registry CRD42023493897 (https://www.crd.york.ac.uk/prospero/#myprospero). This systematic review and meta-analysis has been reported in line with the preferred Reporting Item for Systematic Review and Meta-analysis (PRISMA) 2020 guideline [12].
Eligibility criteria
Observational studies (prospective and retrospective cohort, and cross-sectional) that reported the outcome (prevalence of mortality) in all emergency departments (adults, pediatrics, and obstetrics), conducted in Ethiopia, and published in English up to December 16, 2023, or grey literature sources were included in this review. Case control studies were included only for identifying the determinants of mortality, but they were omitted while determining the prevalence of mortality because, by their nature, they do not report the prevalence. Moreover, articles that didn’t report the outcome variable and studies with small sample size were excluded from this review. Once attempts were made to contact the corresponding authors of the studies to obtain the full texts, articles that did not provide full access and didn’t report the outcome (prevalence of mortality of patients in emergency departments) were excluded.
Searching strategy
Following the PRISMA guideline, studies were searched using PubMed, Google Scholar, CINAHL, EMBASE, HINARI, and Web of Science without publication year restriction up to December 16, 2023. All published and grey literature was retrieved, critically evaluated, and assessed for inclusion in this study. Search terms used to access studies using PECO (Population (patients), Exposure (attending in emergency departments), Context (Ethiopian hospitals), Outcome (mortality)) strategy are the following: “mortality”, “mortalities”, “crude death rate”, “crude mortality rate”, “death”, “Ethiopia”, Federal Democratic Republic of Ethiopia”, “emergency department”, ‘emergency departments”, emergency “department”, “emergency ward”, “emergency hospital”, “emergency class”, “emergency units”, and “emergency unit”. These search strategies were developed using “AND” and/or “OR” Boolean operators.
Outcomes
This review and meta-analysis primarily focus on determining the pooled prevalence of mortality in emergency departments in Ethiopia, expressed as a percentage with frequency. The calculation entails dividing the total number of patients who died by the overall number of patients visited in emergency departments, multiplied by 100. The authors utilized the Odds Ratio (OR) as an outcome measure to pinpoint determinants of mortality in emergency departments. Factors reported in at least two studies were considered for pooled analysis to increase the validity of this study.
Data extraction
The articles identified in the literature search were first screened by title and abstracts for inclusion in the systematic review by independent reviewers (M.A.M, T.A, and B.T.A). Those studies that passed the title and abstract screening processes were eligible for full-text review. The independent reviewers (M.A.M, T.A, B.T.A, A.G, and G.B) evaluated the full text of the eligible studies for inclusion in the final analysis. The disagreement was handled based on the inclusion and exclusion criteria, and the third reviewer (T.A.D) was involved in the final decision.
Microsoft Excel 2019 was used to extract data encompassing the author name, publication year, region of the study, prevalence of mortality, sample size, study design, and population group. Two independent reviewers (M.A.M and T.A) extracted and cross-checked the extracted data for potential variations, and the discrepancies were handled by re-evaluating the full text. A third review (B.T.A) examined the extracted data to ensure its accuracy and identify any errors.
Risk of bias assessment
The Joanna Briggs Institute (JBI) quality assessment tool [13] for prevalence studies was used to assess the quality of the included studies. The criteria were: (1) sample representativeness; (2) sample size adequacy; (3) using valid measurements; (4) using appropriate statistical analysis methods; and (5) response rates. Two reviewers (M.A.M. and T.A) assessed the quality of the included studies. The procedure was repeated whenever a disagreement occurred. Studies that scored greater than or equal to 50% of the assessment criteria were considered to have a low risk of bias.
Data analysis
Endnote X-8 reference manager software was used to manage the selection process. STATA version 17 was used for data analysis. Potential publication bias was checked by the funnel plot [14] and Egger’s test [15]. The heterogeneity of articles was assessed using I2 statistics, and scores of 75%, 50%, and 20% correspond to high, moderate, and low levels of heterogeneity, respectively [16]. DerSimonian and Laird’s random effects model was used to estimate the pooled prevalence with a 95% CI of mortality of patients in emergency departments. Subgroup analysis was done using region, type of population, and age group. A meta-regression analysis using the sample size and publication year was conducted to identify the possible source of heterogeneity. The sensitivity test was done to check the effect of individual studies on the pooled estimate.
Results
Article selection
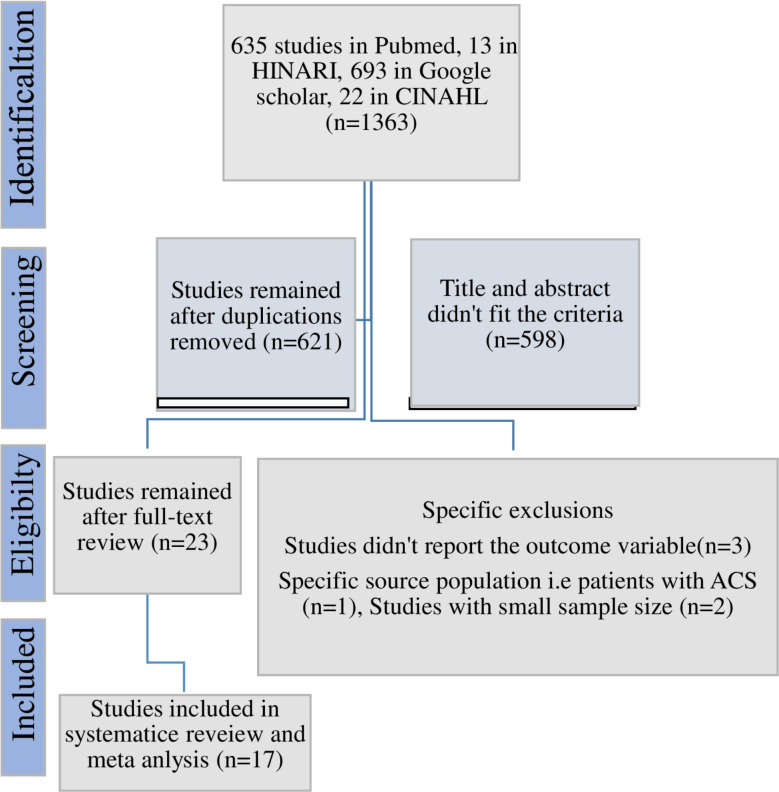
Using the PRISMA flow diagram, a total of 1363 potentially eligible studies were identified. After removing duplications and conducting a full-text review, 23 studies were retrieved. Finally, 17 studies were included for the final review and Meta-analysis [8, 17–32] (Fig. 1).
Fig. 1.
PRISMA flow-chart depicting the selection process of studies in Ethiopia
Study characteristics
Studies included in this review and meta-analysis were conducted in Ethiopia and published in indexed journals and/or found as grey literature. Fifteen studies were cross-sectional [8, 18–27, 29–32], and the remaining two were case-control [17, 28]. These studies are conducted in Addis Ababa [8, 18, 19, 21–25, 32], Amhara [20, 27, 30], Oromia [17, 26, 29], South Nation and Nationalities (SNN) [28], and Dire Dawa [31]. The sample size ranged from 175 to 9956. A quality assessment was performed using JBI appraisal tool and studies scored ≥ 50% has considered as low risk of bias. Subsequently, all studies included in this review and meta-analysis have a low risk of bias (Table 1).
Table 1.
General characteristics of the included studies
| Author | Publication year | Region | Age group | Sample size | Prevalence | Study design | Type of population |
|---|---|---|---|---|---|---|---|
| Tsegaye et al. [28] | 2023 | SNNP | Pedi | 333 | 11.4 | Case control | All |
| Abebe T et al. [18] | 2022 | AA | Adult | 362 | 3.6 | Cross sectional | All |
| Hanna D et al. [8] | 2021 | AA | Adult | 506 | 2.8 | Cross sectional | All |
| Tarkie et al. [27] | 2023 | Amhara | Adult | 5232 | 1.4 | Cross sectional | All |
| Hunchak et al. [24] | 2015 | AA | Adult | 9956 | 1.9 | Cross sectional | All |
| Woyessa A et al. [29] | 2019 | Oromia | Adult | 889 | 8.5 | Cross sectional | All |
| Abebe F et al. [17] | 2023 | Oromia | Adult | 261 | 28.2 | Case control | All |
| Dode et al. [21] | 2022 | AA | Adult | 388 | 3.02 | Cross sectional | All |
| Jofira et al. [25] | 2018 | AA | Pedi | 338 | 4.1 | Cross sectional | All |
| Habte T et al. [19] | 2023 | AA | Pedi | 303 | 5 | Cross sectional | All |
| Agerie et al. [30] | 2022 | Amhara | Adult | 567 | 4.6 | Cross sectional | All |
| Fitsumbirhan et al. [23] | 2015 | AA | Adult | 711 | 3.9 | Cross sectional | All |
| Fikadu A et al. [22] | 2021 | AA | Adult | 331 | 14.2 | Cross sectional | Fall injury |
| Birhan et al. [20] | 2023 | Amhara | Adult | 415 | 33 | Cross sectional | Trauma |
| Mamo et al. [26] | 2023 | Oromia | Adult | 357 | 12.6 | Cross sectional | RTI |
| Tesfaye et al. [32] | 2020 | AA | Adult | 324 | 3.4 | Cross sectional | TBI |
| Nigussie et al. [31] | 2022 | Dire Dawa | Adult | 175 | 16.7 | Cross sectional | Poisoning |
AA; Addis Ababa, RTI; Road Traffic Injury, SNNP; Southern Nation Nationalities and People of Ethiopia, TBI; Traumatic Brain Injury
Quality and risk of bias assessment
Using the JBI critical appraisal checklist for analytical cross sectional studies, the quality and risk bias of each article included in this review were assessed. All included studies have a low risk of bias as they scored greater than or equal to 50% of the assessment criteria were considered (Table 2).
Table 2.
Quality and risk of bias assessment of individual studies
| No | Checklists | Were the samples representative? | Was the sample size adequate? | Was the exposure measured in a valid and reliable way? | Was appropriate statistical analysis used? | Were confounding factors identified? | Were strategies to deal with confounding factors stated? | Were the outcomes measured in a valid and reliable way? | Was the response rate acceptable | Overall appraisal score |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Tsegaye et al. [28] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 2 | Abebe T et al. [18] | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 6 |
| 3 | Hanna D et al. [8] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| 4 | Tarkie et al. [27] | 1 | 1 | 1 | 1 | N/A | N/A | 1 | N/A | 5 |
| 5 | Hunchak et al. [24] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | N/A | 7 |
| 6 | Woyessa A et al. [29] | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | 6 |
| 7 | Abebe F et al. [17] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 8 | Dode et al. [21] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 9 | Jofira et al. [25] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 10 | Habte T et al. [19] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 11 | Agerie et al. [30] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 12 | Fitsumbirhan et al. [23] | 1 | 1 | 1 | 1 | N/A | N/A | 1 | N/A | 5 |
| 13 | Fikadu A et al. [22] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 14 | Birhan et al. [20] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 15 | Mamo et al. [26] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 16 | Tesfaye et al. [32] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| 17 | Nigussie et al. [31] | 1 | 1 | 1 | 1 | N/A | N/A | 1 | 1 | 6 |
Note 1 = Yes 0 = No U = Unclear N/A = Not applicable
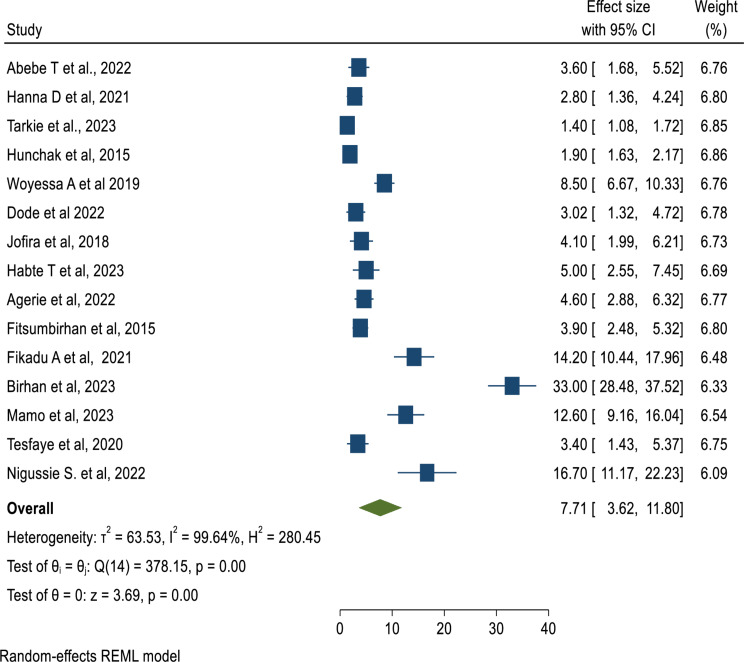
Prevalence of mortality in the ED
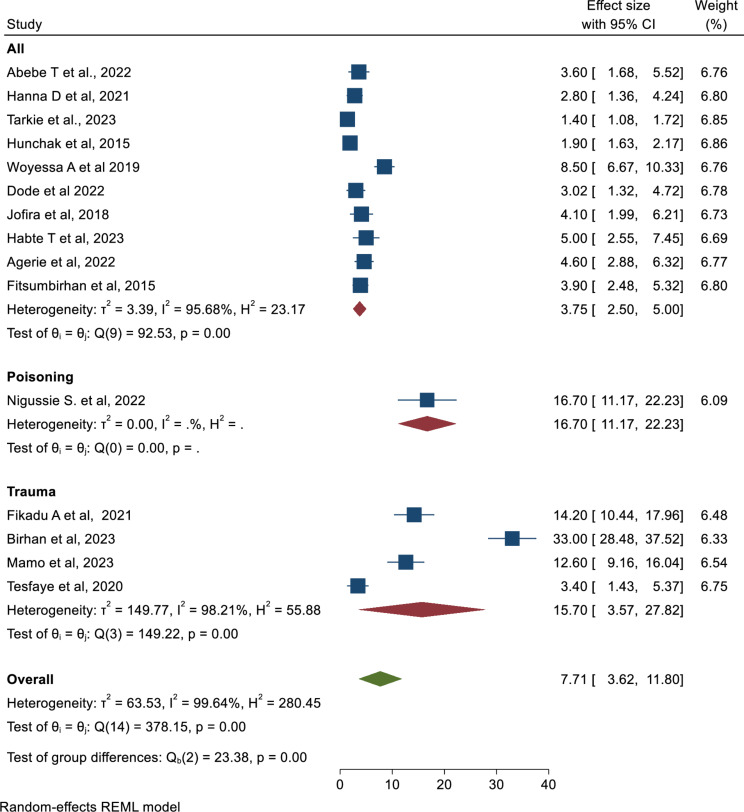
In this systematic review and meta-analysis study using a forest plot, the pooled prevalence of mortality of patients in the ED in Ethiopia was found to be 7.71% (95%CI: 3.62, 11.80) which is estimated by a random-effect model (Fig. 2).
Fig. 2.
Forest plot to depict the pooled prevalence of mortality in Emergency departments in Ethiopia
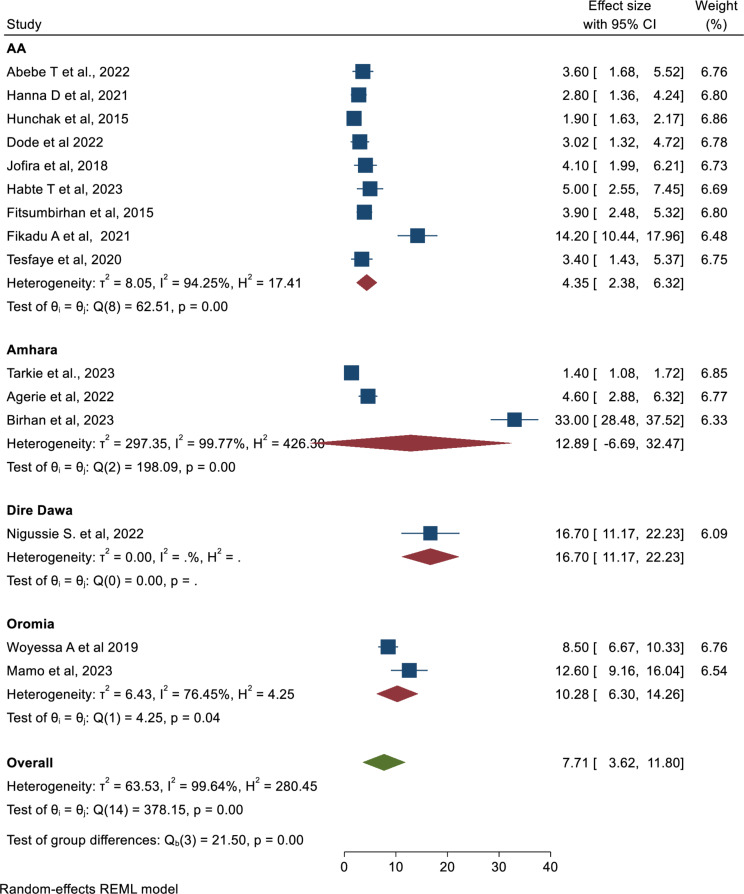
Subgroup analysis
The subgroup analysis using regions of the country showed that the highest mortality of patients in the ED was observed in Dire Dawa (16.70; 95% CI: 11.17, 22.23), followed by the Amhara region (12.89%; 95% CI: 6.69, 32.47) (Fig. 3).
Fig. 3.
Forest plot to depict the pooled prevalence of mortality in Emergency department by regions in Ethiopia
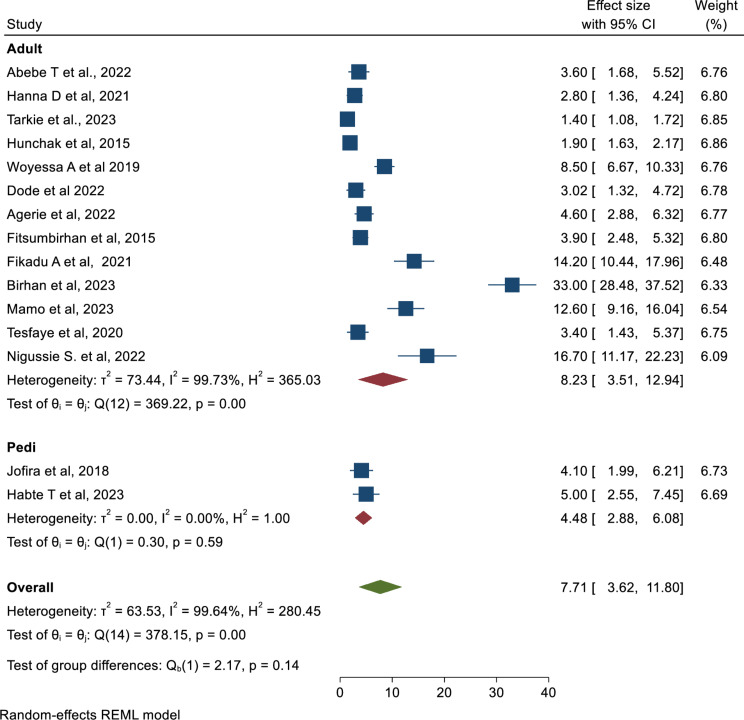
Similarly, another subgroup analysis using the age of the study population revealed that mortality of patients in the ED among the adults population is higher (8.23; 95% CI: 3.51, 12.94) as compared to pediatrics (4.48%; 95% CI: 2.88, 6.08) (Fig. 4).
Fig. 4.
Forest plot to illustrate the pooled prevalence of mortality in Emergency departments by age group in Ethiopia
Furthermore, the subgroup analysis using the type of population studied showed that the highest mortality of patients in the ED was encountered among trauma patients (15.70; 95%CI: 3.57, 27.82) (Fig. 5).
Fig. 5.
Forest plot to illustrate the pooled prevalence of mortality in Emergency department by type of population in Ethiopia
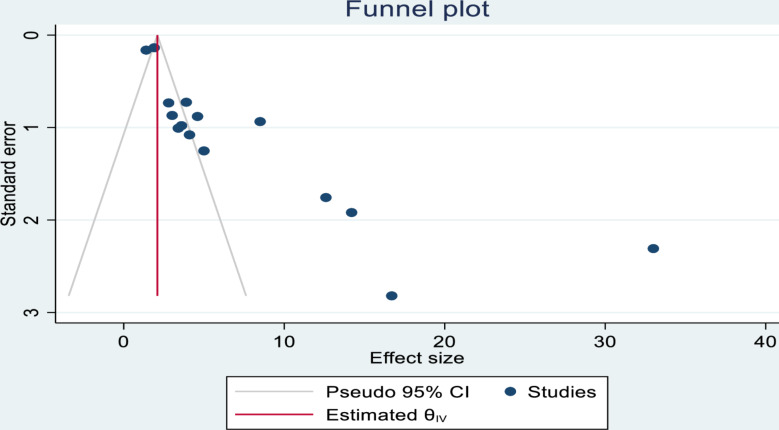
Publication bias evaluation
The presence of publication bias was evaluated using Egger’s (p = 0.000) and Begg’s tests (p = 0.003) which showed that there is a significant publication bias. In addition to the statistical tests, a funnel plot was used, and it is asymmetrical. The vertical line indicates the effect size, whereas the diagonal lines indicate the precision of individual studies with a 95% CI (Fig. 6).
Fig. 6.
Funnel plot to illustrate the presence of publication bias
Investigation of heterogeneity
A meta-regression analysis using the sample size and publication year was conducted to identify the possible source of heterogeneity. However, none of these factors showed significant heterogeneity. Therefore, the source of heterogeneity remains unknown (Table 3).
Table 3.
Meta-regression of mortality of patients in the ED with publication year and sample size to detect heterogeneity
| Source of heterogeneity | Coefficients | Standard error | p-value |
|---|---|---|---|
| Publication year | 1.230673 | 0.8908009 | 0.167 |
| Sample size | − 0.0004325 | 0.0009301 | 0.642 |
Factors associated with mortality of patients in the ED
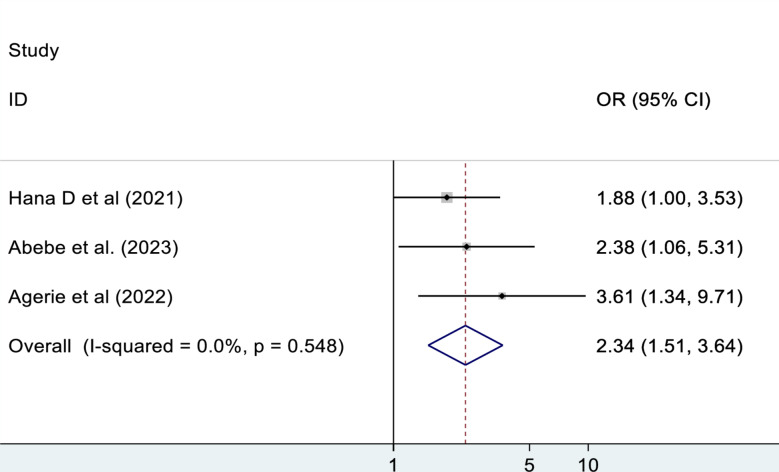
Residence
The pooled effect of three studies were reported on the association between residence and mortality of patients in the ED. This meta-analysis study revealed that being a rural resident has 2.3 times higher odds of mortality as compared to being an urban resident (OR: 2.30, 95% CI: 1.48, 3.58). There is no observed heterogeneity, I2 = 0% (Fig. 7).
Fig. 7.
The association between residence and mortality of patients in the ED
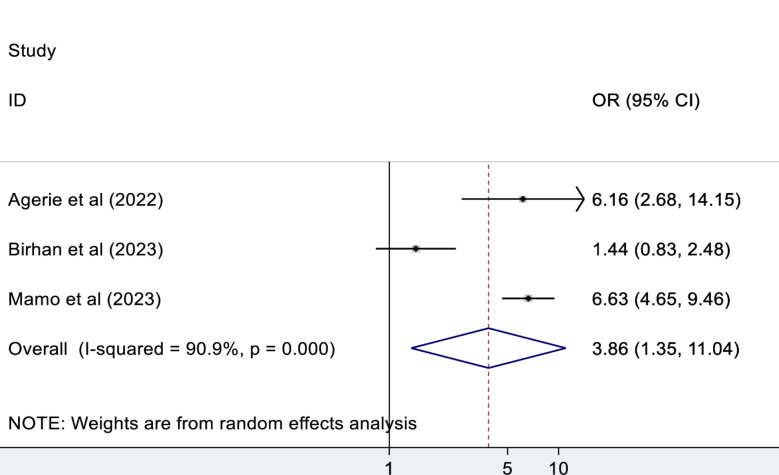
Unconsciousness
According to this meta-analysis, those patients who were unconscious during admission were 3.9 times more likely to die as compared to their counterparts (OR: 3.86, 95% CI: 1.35, 11.04) (Fig. 8).
Fig. 8.
The association between unconsciousness and mortality of patients in the ED
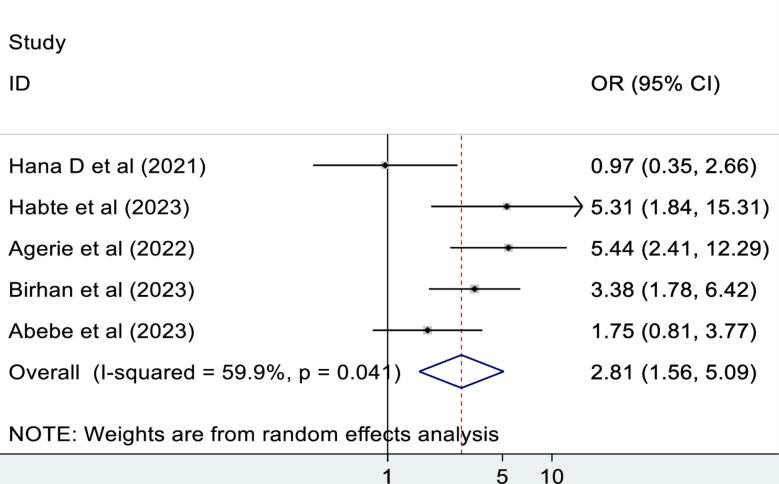
Comorbidity
The pooled effect of five studies showed that those patients who had comorbidity were 2.8 times more likely to die as compared to those who hadn’t comorbidity (OR: 2.82, 95% CI: 1.56, 5.09). There is a moderate heterogeneity between studies, I2 = 59.9% (Fig. 9).
Fig. 9.
The association between comorbidity and mortality of patients in the ED
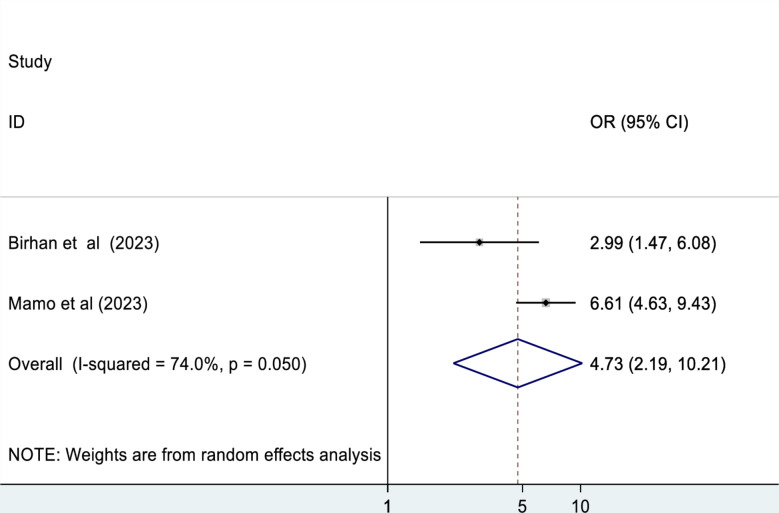
Time to reach at health facilities
This meta-analysis revealed that the time to reach at the nearby health facilities was another determinant factor associated with mortality of patients in the ED. Those patients who weren’t reached at nearby health facilities within one hour are 4.7 times more likely to die as compared to their counterparts (OR: 4.73, 95% CI: 2.19, 10.21) (Fig. 10 ).
Fig. 10.
The association between times elapsed to reach health facilities and mortality of patients in the ED
Sensitivity analysis
A sensitivity analysis using the random effect model showed that the single study didn’t affect the pooled prevalence of mortality (Table 4).
Table 4.
The sensitivity analysis to estimate the effect of a single study on the combined prevalence of mortality of patients in the ED in Ethiopia
| Study omitted | Prevalence (95% CI) |
|---|---|
| Tsegaye et al. [28] | 6.06 (4.85, 7.27) |
| Hana D. et al. [8] | 6.65 (5.37, 7.93) |
| Hunchak et al. [24] | 7.38 (5.52, 9.18) |
| Woyessa A. et al. [29] | 6.12 (4.92, 7.32) |
| Dode et al. [21] | 6.62 (5.34, 7.89) |
| Jofira et al. [25] | 6.52 (5.26, 7.78) |
| Habte T. et al. [19] | 6.45 (5.19, 7.70) |
| Agerie et al. [30] | 6.49 (5.23, 7.75) |
| Fitsumbirhan et al. [23] | 6.56 (5.29, 7.84) |
| Fikadu et al. [22] | 5.93 (4.74, 7.12) |
| Birhan et al. [20] | 5.94 (4.75, 7.12) |
| Mamo et al. [26] | 5.99 (4.79, 7.19) |
| Tesfaye et al. [32] | 6.57 (5.31, 7.84) |
| Nigussie S. et al. [31] | 6.01 (4.1, 7.20) |
| Combined | 7.71 (3.62, 11.8) |
Discussion
Emergency departments’ mortality is one of the major health indices in Ethiopia that should be evaluated monthly in every health institution. Therefore, this systematic review and meta-analysis study is important to generate comprehensive evidence about the prevalence of mortality among patients in EDs and its associated factors in Ethiopia. According to the findings of our study, the pooled prevalence of mortality in the ED was 7.71%. This finding is in line with the studies conducted in England [33] and Nigeria [34], which reported that the overall crud death rate in ED was 8.7% and 7.61%, respectively. However, it is higher as compared to the study conducted in Uganda (2%) [35], Switzerland (0.26%) [36], Sweden (0.88%) [37], England (2.2%) [38], Bulgaria (2.4%) [2], and Denmark (4%) [39]. The possible reasons for this discrepancy might be in industrialized countries, where paramedics begin life-saving measures at the patient’s residence and transport them to the hospital in well-equipped ambulances. In contrast, most patients in our country are brought to the hospital in private cars and traditional ambulances, often without any life-saving interventions before arrival. As a result, many patients arrive with complications and have a little chance of survival [40]. Moreover, it could be due to the differences in the study population, study period, and settings.
According to the current review, the pooled prevalence of mortality among pediatric age groups was 4.48%, which is lower than the study conducted in Burkina Faso [41] (12.9%). The discrepancies might be due to the differences in the study population in terms of disease severity. In addition, it is also higher as compared to the study done in Mexico [42] (21.8%).
This systematic review and meta-analysis revealed that being a rural resident has 2.1 times higher odds of mortality as compared to being an urban resident. This result is supported by the study done in America, which revealed that residents of rural areas experience higher rates of emergency mortality as compared to residents of urban areas [43]. This might be due to the fact that people residing in rural areas have poor health care-seeking behavior and have been presented in the ED lately [44]. Moreover, long distances from health facilities may delay the time to get emergency care, which might potentially lead to high mortality [45].
This meta-analysis study revealed that those patients who were unconscious during admission were 3.9 times more likely to die as compared to their counterparts. This finding is in agreement with studies conducted in Korea [46] and Sweden [47, 48]. The possible reason could be that those unconscious patients are unable to protect their airway, have a high risk of aspiration, have compromised ventilator effort, and are at risk of developing intracranial hypertension, which reduces cerebral perfusion and leads to secondary cerebral attacks and death [49]. Maintaining oxygenation and preventing hypercarbia by preventing aspiration, providing supplemental oxygen, and supporting ventilation are critical in the ED, especially for those unconscious patients [50].
This meta-analysis study revealed that those patients who had comorbidity were 2.8 times more likely to die as compared to those who didn’t have comorbidity. This finding is in harmony with the studies conducted in Iran [3], Sweden [47], and Denmark [39]. This could be due to comorbidities, which have been shown to have a significant impact on clinical course, complications, and patient outcomes [51]. It is a scientific fact that comorbidities such as HIV/AIDS, Diabetes Mellitus (DM), and other comorbidities are immune-compromising diseases. An individual with an immune-compromised condition cannot handle any additional disease burden. In addition, as there is a comorbid disease, patients are more likely to have a greater risk of mortality due to the increased risk of drug side-effects, drug-drug interactions, and drug-disease interactions [52].
According to this meta-analysis, those patients who weren’t reached at nearby health facilities within one hour were 4.7 times more likely to die as compared to their counterparts. This finding is supported by the study conducted in England, which reported that as the time elapsed to reach the health facilities increased by 2 h, the risk of death increased by 1% [53]. Existing evidence indicates that a longer time to reach nearby health facilities leads to delayed presentation to the ED, which can be a detrimental factor for patient mortality [54].
Limitations of the study
Our study has limitations. We limited the search to English-language articles, so any relevant articles published in foreign languages were not included. We also acknowledge that the studies included in this meta-analysis are observational studies with possible residual confounding, since residual confounding cannot be eliminated in observational studies.
Conclusion
This study found that the pooled prevalence of mortality of patients in emergency departments of Ethiopian hospitals was high as compared to the Ethiopian Health Sector Transformation Plan II (HSTP II), putting a high healthcare burden on the country, which requires collaboration between all stakeholders to improve outcome. Being a rural resident, unconsciousness, comorbidity, and time elapsed to reach health facilities were significant predictors of mortality. Improving pre-hospital service, expansion of adequately equipped ambulance for patient transportation to point of care, training of health care providers working in the ED, early referral, and improving first line management at referral hospitals will help to reduce the high mortality in our country.
Abbreviations
- CI
Confidence Interval
- ED
Emergency Department
- OR
Odds Ratio
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- WHO
World Health Organization
Author contributions
MA, BT and TA involved in developing the protocol and study design, study selection, data extraction, statistical analysis, and editing of the final manuscript draft. AG and TA: involved in quality assessment, statistical analysis, and manuscript revision. GB, GK, HB, AE, OA, YT, ST, WT and SM: study selection and extraction; took part in drafting the manuscript or revising it critically for important intellectual content; agreed to submit it to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Funding
Not applicable.
Data availability
All data supporting the findings of this study are available within the paper.
Declarations
Ethical approval and consent to participate
Because it is a systematic review and meta-analysis, ethical approval is not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Health FDROEMO. Ethiopian hospital services transformation guidelines. 2016.
- 2.Stefanovski PH, Vladimir Radkov R, Lyubomir Ilkov T, Pencho Tonchev T, Yoana Mladenova T, Vihar Manchev K, et al. Analysis of mortality in the emergency department at a university hospital in Pleven. J Int Med Res. 2017;45(5):1553–61. 10.1177/0300060517707901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shahrami KH, Sabzghabaie A, Keikha S. Cause of Emergency Department Mortality: a case-control study Hossein Alimohammadi1, Farahnaz Bidarizerehpoosh2, Farzaneh Mirmohammadi1. Emergency. 2014;2(1):30–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Obermeyer Z, Abujaber S, Makar M, Stoll S, Kayden SR, Wallis LA, et al. Emergency care in 59 low-and middle-income countries: a systematic review. Bull World Health Organ. 2015;93:577–86. 10.2471/BLT.14.148338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Reynolds TA, Stewart B, Drewett I, Salerno S, Sawe HR, Toroyan T, et al. The impact of Trauma Care Systems in low- and Middle-Income Countries. Annu Rev Public Health. 2017;38:507–32. 10.1146/annurev-publhealth-032315-021412 [DOI] [PubMed] [Google Scholar]
- 7.Hsia R, Razzak J, Tsai AC, Hirshon JM. Placing emergency care on the global agenda. Ann Emerg Med. 2010;56(2):142–9. 10.1016/j.annemergmed.2010.01.013 [DOI] [PubMed] [Google Scholar]
- 8.Yosha HD, Tadele A, Teklu S, Melese KG. A two-year review of adult emergency department mortality at Tikur Anbesa specialized tertiary hospital, Addis Ababa, Ethiopia. BMC Emerg Med. 2021;21:1–9. 10.1186/s12873-021-00429-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burkholder TW, Hill K, Hynes EJC. Developing emergency care systems: a human rights-based approach. Bull World Health Organ. 2019;97(9):612. 10.2471/BLT.18.226605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Catalá López F, Tabarés Seisdedos R. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet, 2017. 2017. [DOI] [PMC free article] [PubMed]
- 11.Ababa A. Federal Democratic Republic of Ethiopia ministry of health. Ethiopia: Postnatal Care; 2003. [Google Scholar]
- 12.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 13.Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). JBI Evid Implement. 2019;17(1):36–43. [DOI] [PubMed] [Google Scholar]
- 14.Sterne JA, Becker BJ, Egger M. The funnel plot. Publication bias in meta-analysis: Prevention, assessment and adjustments. 2005:73–98.
- 15.Harbord RM, Harris RJ, Sterne JA. Updated tests for small-study effects in meta-analyses. Stata J. 2009;9(2):197–210. 10.1177/1536867X0900900202 [DOI] [Google Scholar]
- 16.Thorlund K, Imberger G, Johnston BC, Walsh M, Awad T, Thabane L, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PLoS ONE. 2012;7(7):e39471. 10.1371/journal.pone.0039471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abebe F, Habtamu A, Workina A. Risks of early mortality and associated factors at adult emergency department of Jimma University Medical Center. Open Access Emerg Med. 2023:293–302. [DOI] [PMC free article] [PubMed]
- 18.Abebe T, Boru Y, Belay E, Abebe A, Kefyalew M, Kifle F. Clinical profile and outcomes of trauma patients visiting the emergency department of a trauma center Addis Ababa, Ethiopia. Afr J Emerg Med. 2022;12(4):478–83. 10.1016/j.afjem.2022.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asinakew T, Habte T, Murugan R. Outcomes of emergency admissions and associated factors among children admitted to the pediatric emergency unit of public hospitals in Addis Ababa, Ethiopia, Retrospective cross-sectional study. 2023.
- 20.Birhan S, Gedamu S, Belay MZ, Mera Mihiretu M, Tadesse Abegaz N, Fissha Adem Y et al. Treatment outcome, pattern of injuries and Associated factors among traumatic patients attending Emergency Department of Dessie City Government hospitals, Northeast Ethiopia: a cross-sectional study. Open Access Emerg Med. 2023:303–12. [DOI] [PMC free article] [PubMed]
- 21.Dode W, Alemayehu G, Tebebe B, Getachew T, Tigistu S, Aklog E, et al. Pattern and predictors of mortality in emergency department of Saint Paul Hospital Millennium medical college Addis Ababa. Ethiopia: retrospective study; 2022. [Google Scholar]
- 22.Fikadu A, Sultan M, Michael M, Workina A. Pattern and outcomes of fall injuries and associated factors in emergency department at Addis Ababa Burn, Emergency and Trauma Hospital. Open Access Emerg Med. 2021:381–9. [DOI] [PMC free article] [PubMed]
- 23.Fitsumbirhan T. Pattern and Outcome of Adult Medical Emergency Department Admissions at Yekatit 12 Hospital. Addis Ababa: Addis Ababa University; 2015. [Google Scholar]
- 24.Hunchak C, Teklu S, Meshkat N, Meaney C, Puchalski Ritchie L. Patterns and predictors of early mortality among emergency department patients in Addis Ababa, Ethiopia. BMC Res Notes. 2015;8(1):1–9. 10.1186/s13104-015-1592-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jofiro G, Jemal K, Beza L, Bacha Heye T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: a 5 year retrospective case review study. BMC Pediatr. 2018;18(1):1–10. 10.1186/s12887-018-1287-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mamo DE, Abebe A, Beyene T, Alemu F, Bereka B. Road traffic accident clinical pattern and management outcomes at JUMC Emergency Department; Ethiopia. Afr J Emerg Med. 2023;13(1):1–5. 10.1016/j.afjem.2022.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarkie K, Altaye KD, Berhe YW. Current patterns of care at adult emergency department in Ethiopian tertiary university hospital. Int J Emerg Med. 2023;16(1):25. 10.1186/s12245-023-00502-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsegaye H, Demelash A, Aklilu D, Girma B. Determinants of pediatrics emergency mortality at comprehensive specialized hospitals of South nation nationalities and people region, Ethiopia, 2022: unmatched case-control study. BMC Pediatr. 2023;23(1):1–9. 10.1186/s12887-023-04011-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woyessa AH, Dibaba BY, Hirko GF, Palanichamy T. Spectrum, pattern, and clinical outcomes of adult emergency department admissions in selected hospitals of Western Ethiopia: a hospital-based prospective study. Emergency medicine international. 2019;2019. [DOI] [PMC free article] [PubMed]
- 30.Zerihun A. Mortality and its associated factors among adult patients admitted in the emergency department at Northwest AMHARA comprehensive specialized hospitals, Northwest Ethiopia, 2022: UOG; 2022.
- 31.Nigussie S, Demeke F, Getachew M, Amare F. Treatment outcome and associated factors among patients admitted with acute poisoning in a tertiary hospital in Eastern Ethiopia: a cross-sectional study. SAGE open Med. 2022;10:20503121221078155. 10.1177/20503121221078155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.al Te. Oucomes of Traumatic Brain Injury Patients (TBI) admitted in Emergency departments in Addis Ababa. 2020.
- 33.Jones S, Moulton C, Swift S, Molyneux P, Black S, Mason N, et al. Association between delays to patient admission from the emergency department and all-cause 30-day mortality. Emerg Med J. 2022;39(3):168–73. 10.1136/emermed-2021-211572 [DOI] [PubMed] [Google Scholar]
- 34.Olusegun-Joseph A, Akande O, Otrofanowei E, Nwoye E, Olopade O, Ajuluchukwu J. Medical mortality in an emergency department in Nigeria: the transition is obvious! Afr Health Sci. 2021;21(1):172–9. 10.4314/ahs.v21i1.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chamberlain S, Stolz U, Dreifuss B, Nelson SW, Hammerstedt H, Andinda J, et al. Mortality related to acute illness and injury in rural Uganda: task shifting to improve outcomes. PLoS ONE. 2015;10(4):e0122559. 10.1371/journal.pone.0122559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heymann EP, Wicky A, Carron P-N, Exadaktylos AK. Death in the emergency department: a retrospective analysis of mortality in a Swiss University Hospital. Emergency medicine international. 2019;2019. [DOI] [PMC free article] [PubMed]
- 37.Wretborn J, Wilhelms DB, Ekelund U. Emergency department crowding and mortality: an observational multicenter study in Sweden. Front Public Health. 2023;11:1198188. 10.3389/fpubh.2023.1198188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meacock R, Anselmi L, Kristensen SR, Doran T, Sutton M. Higher mortality rates amongst emergency patients admitted to hospital at weekends reflect a lower probability of admission. J Health Serv Res Policy. 2017;22(1):12–9. 10.1177/1355819616649630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bech CN, Brabrand M, Mikkelsen S, Lassen A. Risk factors associated with short term mortality changes over time, after arrival to the emergency department. Scand J Trauma Resusc Emerg Med. 2018;26(1):1–9. 10.1186/s13049-018-0493-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Denu ZA, Osman MY, Bisetegn TA, Biks GA, Gelaye KA. Barriers and opportunities of establishing an integrated prehospital emergency response system in North West Ethiopia: a qualitative study. Inj Prev. 2022. [DOI] [PMC free article] [PubMed]
- 41.Barro M, Ouattara CA, Sanogo B, Baby AA, Ouattara ABI, Nacro FS et al. Risk factors for mortality in an African pediatric emergency department: case of Sourô Sanou Hospital, a prospective, cross-sectional study. J Trop Pediatr. 2023;70(1). [DOI] [PubMed]
- 42.García-Peña C, Pérez-Zepeda MU, Robles-Jiménez LV, Sánchez-García S, Ramírez-Aldana R, Tella-Vega P. Mortality and associated risk factors for older adults admitted to the emergency department: a hospital cohort. BMC Geriatr. 2018;18(1):1–11. 10.1186/s12877-018-0833-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Greenwood-Ericksen MB, Tipirneni R, Abir M. An emergency medicine–primary care partnership to improve rural population health: expanding the role of emergency medicine. Ann Emerg Med. 2017;70(5):640–7. 10.1016/j.annemergmed.2017.06.025 [DOI] [PubMed] [Google Scholar]
- 44.Fan L, Shah MN, Veazie PJ, Friedman B. Factors associated with emergency department use among the rural elderly. J Rural Health. 2011;27(1):39–49. 10.1111/j.1748-0361.2010.00313.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fleet R, Turgeon-Pelchat C, Smithman MA, Alami H, Fortin J-P, Poitras J, et al. Improving delivery of care in rural emergency departments: a qualitative pilot study mobilizing health professionals, decision-makers and citizens in Baie-Saint-Paul and the Magdalen Islands, Québec, Canada. BMC Health Serv Res. 2020;20:1–10. 10.1186/s12913-020-4916-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lim J, Lee J. Factors associated with mortality of older adults hospitalized via emergency departments in Korea. Korean J Adult Nurs. 2020;32(3):273–82. 10.7475/kjan.2020.32.3.273 [DOI] [Google Scholar]
- 47.Olsson H, Karlson BW, Herlitz J, Karlsson T, Hellberg J, Prytz M, et al. Predictors of short-and long-term mortality in critically ill, older adults admitted to the emergency department: an observational study. BMC Emerg Med. 2022;22(1):15. 10.1186/s12873-022-00571-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ljunggren M, Castrén M, Nordberg M, Kurland L. The association between vital signs and mortality in a retrospective cohort study of an unselected emergency department population. Scand J Trauma Resusc Emerg Med. 2016;24(1):1–11. 10.1186/s13049-016-0213-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Agorogianni D, Michalopoulos E, Prantzou A, Liaskou C, Stamou A, Kapadochos T, et al. Clinical indicators as prognostic factors of multi-trauma patients in the Intensive Care Unit. Health Res J. 2021;7(4):206–18. 10.12681/healthresj.28191 [DOI] [Google Scholar]
- 50.Surgeons ACo. Advanced Trauma Life Support (ATLS). Introduction. Chicago, United States: American College of Surgeons; 2018. p. xxix. [Google Scholar]
- 51.Simpson A, Puxty K, McLoone P, Quasim T, Sloan B, Morrison DS. Comorbidity and survival after admission to the intensive care unit: a population-based study of 41,230 patients. J Intensive Care Soc. 2021;22(2):143–51. 10.1177/1751143720914229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Uslu MF, Yilmaz M, Atescelik M, Atilgan FA, Atilgan F. Effect of Comorbid diseases on hospitalization and In-Hospital mortality of Elderly patients who reapplied to the Emergency Department within 72 hours. Cureus. 2023;15(11). [DOI] [PMC free article] [PubMed]
- 53.Nicholl J, West J, Goodacre S, Turner J. The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007;24(9):665–8. 10.1136/emj.2007.047654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Knowles E, Shephard N, Stone T, Mason SM, Nicholl J. The impact of closing emergency departments on mortality in emergencies: an observational study. Emerg Med J. 2019;36(11):645–51. 10.1136/emermed-2018-208146 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data supporting the findings of this study are available within the paper.