Percutaneous coronary intervention has become a more common procedure than coronary artery bypass surgery in many countries, and the number of procedures continues to rise. In one day an interventionist may treat four to six patients with complex, multivessel disease or acute coronary syndromes. Various balloons, stents, and other devices are delivered by means of a 2 mm diameter catheter introduced via a peripheral artery. The success rate is over 95%, and the risk of serious complications is low. After a few hours patients can be mobilised, and they are usually discharged the same or the next day. Even the spectre of restenosis is now fading.
Refinements of existing techniques
The present success of percutaneous procedures is largely because of refinement of our “basic tools” (intracoronary guidewires and low profile balloons), which have greatly contributed to the safety and effectiveness of procedures. However, the greatest technological advance has been in the development of stents. These are usually cut by laser from stainless steel tubes into a variety of designs, each with different radial strength and flexibility. They are chemically etched or electropolished to a fine finish and sometimes coated.
Digital angiography is a great advance over cine-based systems, and relatively benign contrast media have replaced the toxic media used in early angioplasty. Although magnetic resonance and computed tomographic imaging may become useful in the non-invasive diagnosis of coronary artery disease, angiography will remain indispensable to guide percutaneous interventions for the foreseeable future.
Table 1.
Interventional devices and their uses
| Device | Use (% of cases) | Types of lesion |
|---|---|---|
| Balloon catheter | 100% | Multiple types |
| Stent | 70-90% | Most types |
| Drug eluting stent | 0-50% | High risk of restenosis (possibly all) |
| Cutting balloon | 1-5% | In-stent restenosis, ostial lesions |
| Rotablator | 1-3% | Calcified, ostial, undilatable lesions |
| Brachytherapy | 1-3% | In-stent restenosis |
| Atherectomy | <1% | Bulky, eccentric, ostial lesions |
| Stent graft | <1% | Aneurysm, arteriovenous malformation, perforation |
| Thrombectomy | <1% | Visible thrombus |
| Laser | <1% | Occlusions, in-stent restenosis |
| Distal protection | <1% | Degenerate vein graft |
New device technology
Pre-eminent among new devices is the drug eluting (coated) stent, which acts as a drug delivery device to reduce restenosis. The first of these was the sirolimus coated Cypher stent. Sirolimus is one of several agents that have powerful antimitotic effects and inhibit new tissue growth inside the artery and stent. In a randomised controlled trial (RAVEL) this stent gave a six month restenosis rate of 0% compared with 27% for an uncoated stent of the same design. A later randomised study (SIRIUS) of more complex stenoses (which are more prone to recur) still produced a low rate of restenosis within stented segments (9% v 36% with uncoated stents), even in patients with diabetes (18% v 51% respectively). Other randomised studies such as ASPECT and TAXUS II have also shown that coated stents (with the cytotoxic agent paclitaxel) have significantly lower six month restenosis rates than identical uncoated stents (14% v 39% and 6% v 20% respectively). By reducing the incidence of restenosis (and therefore recurrent symptoms), drug eluting stents will probably alter the balance of treating coronary artery disease in favour of percutaneous intervention rather than coronary artery bypass surgery. However, coated stents will not make any difference to the potential for percutaneous coronary intervention to achieve acute success in any given lesion; nor do they seem to have any impact on acute and subacute safety.
Table 2.
Performance of percutaneous coronary intervention
| General statistics | |
|---|---|
| • Success rate of procedure | >95% |
| • Symptoms improved after procedure | 90% |
| • Complications* | 2% |
| • Restenosis | 15% (range 5-50%) |
| • Duration of procedure | 15 minutes-3 hours |
| • Access point: | |
| Femoral artery | 95% |
| Radial or brachial artery | 5% |
| • Time in hospital after procedure: | |
| Overnight | 60% |
| Day case | 20% |
| Longer | 20% |
| • Intravenous contrast load | 100-800 ml |
| • X ray dose to patient | 75 Gy/cm2† |
| Special conditions | |
| • Success of direct procedure for acute myocardial infarction | >95% |
| • Success for chronic (>3 month) occluded vessel | 50-75% |
| • Mortality for procedure in severe cardiogenic shock | 50% |
| • Restenosis: | |
| Vessels <2.5 mm in diameter, >40 mm length | 60% |
| Vessels >3.5 mm diameter, <10 mm length | 5% |
| • Lesion recurrence later than 6 months after procedure | <5% |
| • Re-restenosis: | |
| After repeat balloon dilatation | 30-50% |
| After brachytherapy | <15% |
Death, myocardial infarction, coronary artery bypass surgery, cerebrovascular accident
Equivalent to 1-2 computed tomography scans
Although coated stents may, paradoxically, be too effective at altering the cellular response and thus delay the desirable process of re-endothelialisation, there is no evidence that this is a clinical problem. However, this problem has been observed with brachytherapy (catheter delivered radiotherapy over a short distance to kill dividing cells), a procedure that is generally reserved for cases of in-stent restenosis. This may lead to late thrombosis as platelets readily adhere to the “raw” surface that results from an impaired healing response. This risk is minimised by prolonged treatment with antiplatelet drugs and avoiding implanting any fresh stents at the time of brachytherapy.
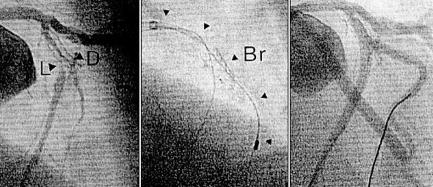
Figure 1.
Triple vessel disease is no longer a surgical preserve, and particularly good results are expected with drug eluting stents. In this case, lesions in the left anterior descending (LAD), circumflex (Cx), and right coronary arteries (RCA) (top row) are treated easily and rapidly by stent (S) implantation (bottom row)
Other energy sources may also prove useful. Sonotherapy (ultrasound) may have potential, less as a treatment in its own right than as a facilitator for gene delivery, and is “benign” in its effect on healthy tissue. Photodynamic therapy (the interaction of photosensitising drug, light, and tissue oxygen) is also being investigated but is still in early development. Laser energy, when delivered via a fine intracoronary wire, is used in a few centres to recanalise blocked arteries.
New work practices
Twenty years ago, a typical angioplasty treated one proximally located lesion in a single vessel in a patient with good left ventricular function. Now, it commonly treats two or three vessel disease, perhaps with multiple lesions (some of which may be complex), in patients with impaired left ventricular function, advanced age, and comorbidity. Patients may have undergone coronary artery bypass surgery and be unsuitable for further heart surgery. Isolated left main stem and ostial right coronary artery lesions, though requiring more experience and variations on traditional techniques, are also no longer a surgical preserve.
Figure 2.


Unprotected left main stem stenoses (LMS, top) may, with careful selection, be treated by stent implantation (S, bottom). Best results (similar to coronary artery bypass surgery) are achieved in stable patients with good left ventricular function and no other disease. Close follow up to detect restenosis is important. (LAD=left anterior descending artery, Cx=circumflex coronary artery)
Role of percutaneous coronary intervention
The role of percutaneous intervention has extended to the point where up to 70% of patients treated have acute coronary syndromes. Trial data now support the use of a combination of a glycoprotein IIb/IIIa inhibitor and early percutaneous intervention to give high risk patients the best long term results. The same applies to acute myocardial infarction, where percutaneous procedures achieve a much higher rate of arterial patency than thrombolytic treatment. Even cardiogenic shock, the most lethal of conditions, may be treated by an aggressive combination of intra-aortic balloon pumping and percutaneous intervention.
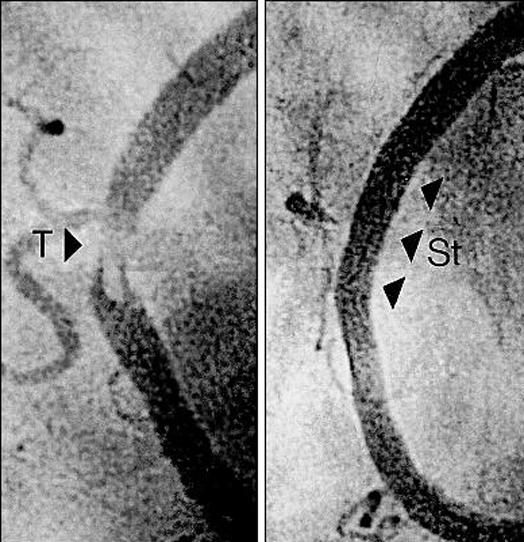
Figure 4.
Angiograms showing severe, diffuse, in-stent restenosis in the left anterior descending artery and its diagonal branch (L and D, left). This was treated with balloon dilatation and brachytherapy with β irradiation (Novoste) from a catheter (Br, centre), with an excellent final result (right)
The potential for percutaneous procedures to treat a wide range of lesions successfully with low rates of restenosis raises the question of the relative roles of percutaneous intervention and bypass surgery in everyday practice. It takes time to accumulate sufficient trial data to make long term generalisations possible.
Figure 5.
Angiogram of an aortocoronary vein graft with an aneurysm and stenoses (A and S, top). Treatment by implantation of a membrane-covered stent excluded the aneurysm and restored a tubular lumen (bottom)
Early trials comparing balloon angioplasty with bypass surgery rarely included stents and few patients with three vessel disease (as such disease carried higher risk and percutaneous intervention was not as widely practised as now). The long term results favoured bypass surgery, but theses trials are now outdated. In the second generation of studies, stents were used in percutaneous intervention, improving the results. As in the early studies, surgery and intervention had similarly low complications and mortality. The intervention patients still had more need for repeat procedures because of restenosis than the bypass surgery patients, but the differences were less.
Table 3.
Names of trials
| • ASPECT—Asian paclitaxel-eluting stent clinical trial |
| • RAVEL—Randomized study with the sirolimus eluting velocity balloon expandable stent in the treatment of patients with de novo native coronary artery lesions |
| • SIRIUS—Sirolimus-coated velocity stent in treatment of patients with de novo coronary artery lesions trial |
| • TAXUS II—Study of the safety and superior performance of the TAXUS drug-eluting stent versus the uncoated stent on de novo lesions |
The major drawback of all these studies was an exclusion rate approaching 95%, making the general clinical application of the findings questionable. This was because it was unusual at that time to find patients with multivessel disease who were technically suitable for both methods and thus eligible for inclusion in the trials. Now that drug eluting stents are available, more trials are under way: the balance will now probably tip in favour of percutaneous coronary intervention. Meanwhile, the decision of which treatment is better for a patient at a given time is based on several factors, including the feasibility of percutaneous intervention (which is generally considered as the first option), completeness of revascularisation, comorbidity, age, and the patient's own preferences.
Figure 7.

Bifurcation lesions, such as of the left anterior descending artery and its diagonal branch (L and D, left), are technically challenging to treat but can be well dilated by balloon dilatation and selective stenting (S, right)
Implications for health services
These issues are likely to pose major problems for health services. Modern percutaneous techniques can be used both to shorten patients' stay in hospital and to make their treatment minimally hazardous and more comfortable. They can also be used in the first and the last (after coronary artery bypass surgery) stages of a patient's “ischaemic career.”
On the other hand, for the role of percutaneous coronary intervention in acute infarction to be realised, universal emergency access to this service will be needed. However, most health systems cannot afford this—the main limiting factor being the number of interventionists and supporting staff required to allow a 24 hour rota compatible with legal working hours and the survival of routine elective work.
The future for percutaneous coronary intervention
Will percutaneous coronary intervention exist in 20 years time, or, at least, be recognisable as a logical development of today's procedures? Will balloons and stents still be in use? It is likely that percutaneous procedures will expand further, although some form of biodegradable stent is a possibility. A more “biological” stent might also be able to act as an effective drug or gene reservoir, which may extend local drug delivery into new areas of coronary artery disease. We may find ourselves detecting inflamed (“hot”) plaques with thermography catheters and treating these before they rupture. We may even be able to modify the natural course of coronary artery disease by releasing agents “remotely” (possibly using an external ultrasound trigger) or by injecting an agent that activates the molecular cargo in a stent.
Figure 8.
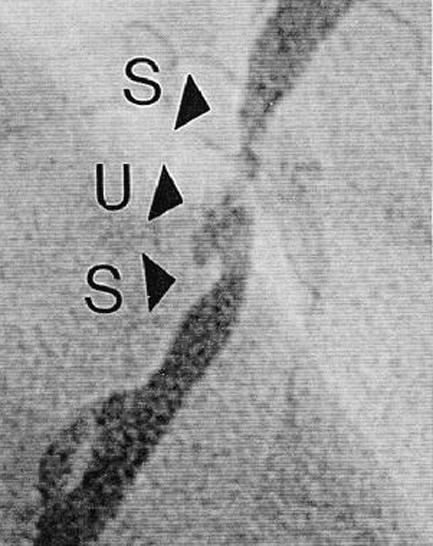

An acute coronary syndrome was found to be due to stenoses and an ulcerated plaque in the right coronary artery (S and U, left). This was treated with a glycoprotein IIb/IIIa inhibitor followed by stent implantation (right). This is an increasingly common presentation of coronary artery disease to catheterisation laboratories
A persistent challenge still limiting the use of percutaneous coronary intervention is that of chronic total occlusions, which can be too tough to allow passage of an angioplasty guidewire. An intriguing technique is percutaneous in situ coronary artery bypass. With skill and ingenuity, a few enthusiasts have anastomosed the stump of a blocked coronary artery to the adjacent cardiac vein under intracoronary ultrasound guidance, thereby using the vein as an endogenous conduit (with reversed flow). This technique may assist only a minority of patients. More practical, we believe, is the concept of drilling through occlusions with some form of external guidance, perhaps magnetic fields.
Figure 10.
Right coronary artery containing large, lobulated thrombus (T, left) on a substantial stenosis. After treatment with glycoprotein IIb/IIIa inhibitor, the lesion was stented successfully (St, right)
“Direct” myocardial revascularisation (punching an array of holes into ischaemic myocardium) has had a mixed press over the past decade. Some attribute its effect to new vessel formation, others cite a placebo effect. Although the channels do not stay open, they seem to stimulate new microvessels to grow. Injection of growth factors (vascular endothelial growth factor and fibroblast growth factor) to induce new blood vessel growth also has this effect, and percutaneous injection of these agents into scarred or ischaemic myocardium is achievable. However, we need a more thorough understanding of biological control mechanisms before we can be confident of the benefits of this technology.
Table 4.
General roles of percutaneous coronary intervention (PCI) and coronary artery bypass surgery (CABG)
|
PCI
|
|||
|---|---|---|---|
| Condition | 1993 | 2003 | CABG |
| Acute presentation | |||
| Acute coronary syndrome | ++ | +++ | ++ |
| Cardiogenic shock | +/- | + | +/- |
| Acute full thickness myocardial infarction | + | +++ | - |
| Bailout after failed thrombolysis | + | ++ | - |
| Chronic presentation | |||
| Impaired left ventricle with left main stem stenosis and blocked right coronary artery | -- | - | +++ |
| Impaired left ventricle and 3 vessel disease | + | ++ | +++ |
| Impaired left ventricle and 3 vessel disease with ≥ 1 occlusion | - | + | +++ |
| Diabetes and 3 vessel disease | + | ++ | +++ |
| Good left ventricle and 3 vessel disease | + | ++ | +++ |
| 2 occluded vessels | - | - | ++ |
| Good left ventricle and 2 vessel disease | + | +++ | ++ |
| Repeat revascularisation after PCI | ++ | +++ | ++ |
| Good left ventricle and 1 vessel disease | +++ | +++ | + |
| 2-3 vessel diffuse or distal disease | + | ++ | + |
| Repeat revascularisation after CABG | + | ++ | + |
| Palliative partial revascularisation | + | ++ | - |
| Revascularisation of frail patient or with severe comorbidity | + | ++ | - |
highly effective role
useful role
limited role
treatment not preferred
treatment usually strongly advised against
Challenges to mechanical revascularisation
Deaths from coronary artery disease are being steadily reduced in the Western world. However, with increasing longevity, it is unlikely that we will see a reduction in the prevalence of its chronic symptoms. More effective primary and secondary prevention; antismoking and healthy lifestyle campaigns; and the widespread use of antiplatelet drugs, β blockers, statins, and renin-angiotensin system inhibitors may help prevent, or at least delay, the presentation of symptomatic coronary artery disease. In patients undergoing revascularisation, they are essential components of the treatment “package.” More effective anti-atherogenic treatments will no doubt emerge in the near future to complement and challenge the dramatic progress being made in percutaneous coronary intervention.
The ABC of interventional cardiology is edited by Ever D Grech and will be published as a book in autumn 2003.
The coronary artery imaging was provided by John Bowles, clinical specialist radiographer, and Nancy Alford, clinical photographer, Sheffield Teaching Hospitals NHS Trust, Sheffield.
Competing interests: None declared.
Further reading
- •.Morice M-C, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med 2002;346: 1773-80 [DOI] [PubMed] [Google Scholar]
- •. Park SJ, Shim WH, Ho DS, Raizner AE, Park SW, Hong MK, et al. A paclitaxel-eluting stent for the prevention of coronary restenosis. N Engl J Med 2003;348: 1537-45 [DOI] [PubMed] [Google Scholar]
- •. Raco DL, Yusuf S. Overview of randomised trials of percutaneous coronary intervention: comparison with medical and surgical therapy for chronic coronary artery disease. In: Grech ED, Ramsdale DR, eds. Practical interventional cardiology. 2nd ed. London: Martin Dunitz, 2002: 263-77
- •. Teirstein PS, Kuntz RE. New frontiers in interventional cardiology: intravascular radiation to prevent restenosis. Circulation 2001;104: 2620-6 [DOI] [PubMed] [Google Scholar]
- •. Tsuji T, Tamai H, Igaki K, Kyo E, Kosuga K, Hata T, et al. Biodegradable stents as a platform to drug loading. Int J Cardiovasc Intervent 2003;5: 13-6 [DOI] [PubMed] [Google Scholar]
- •. Hariawala MD, Sellke FW. Angiogenesis and the heart: therapeutic implications. J R Soc Med 1997;90: 307-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- •. Serruys PW, Unger F, Sousa JE, Jatene A, Bonnier HJ, Schonberger JP, et al, for the Arterial Revascularization Therapies Study Group. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med 2001;344: 1117-24 [DOI] [PubMed] [Google Scholar]
- •. SoS Investigators. Coronary artery bypass surgery versus percutaneous coronary intervention with stent implantation in patients with multivessel coronary artery disease (the stent or surgery trial): a randomised controlled trial. Lancet 2002;360: 965-70 [DOI] [PubMed] [Google Scholar]