ABSTRACT
Background
Ni-kshay Poshan Yojana (NPY), a direct benefit transfer scheme under the National Tuberculosis Elimination Program (NTEP) in India, provides a monthly benefit of INR500 for nutritional support of persons with TB (PwTB).
Objectives
To determine the proportion of PwTB receiving atleast one NPY instalment and pattern of utilisation; to ascertain factors associated with NPY non-receipt and association of NPY receipt with TB treatment outcome.
Methods
In our cross-sectional study, we used multi-stage sampling to select PwTB whose treatment outcome was declared between May 2022 and February 2023. A cluster-adjusted, generalized linear model was used to identify factors associated with the non-receipt of NPY and determine association between NPY receipt and TB treatment outcome.
Results
Among 3201 PwTB, 2888 (92.7%; 95% CI 89.8%, 94.8%) had received at least one NPY instalment, and 1903 (64.2%; 95% CI 58.9%, 69.2%) self-reported receipt of benefit. The median (IQR) time to receipt of first instalment was 105 (60,174) days. Non-receipt was significantly higher among PwTB from states with low TB score (aPR = 2.34; 95%CI 1.51, 3.62), who do not have bank account (aPR = 2.48; 95%CI 1.93, 3.19) and with unknown/missing diabetic status (aPR = 1.69; 95%CI 1.11, 2.55). Unfavorable treatment outcomes were associated with non-receipt of NPY (aPR 4.93; 95%CI 3.61,6.75) after adjusting for potential confounders.
Conclusion
Majority of the PwTB received atleast one NPY instalment, but they experience significant delays. Most of the recipients utilised NPY for nutrition. Longitudinal follow-up studies are required to study the impact of NPY on treatment outcomes.
KEYWORDS: Direct benefit transfer, nutrition, delay, pattern of utilization, treatment outcome
Paper context
Main findings: Five years since implementation, almost ninety percent of persons with tuberculosis in India had received at least one benefit under Ni-kshay Poshan Yojana, most of whom utilise it for nutrition.
Added knowledge: Persons with tuberculosis in India experience a median delay of over three months to receive the first instalment of the benefit.
Global health impact for policy and action: Ensuring timely credit of benefits is crucial to enable its utilisation by persons with tuberculosis for better nutrition and favourable treatment outcomes.
Background
Undernutrition is a significant risk factor for incidence of tuberculosis (TB) infection [1,2]. Over 25% of TB incidence in high TB burden countries is attributed to undernutrition [3–5], which is much higher than other risk factors like smoking (11%), diabetes (9%), and Human Immunodeficiency Virus (HIV) (5%) [6,7]. Undernutrition is also linked to TB disease severity and poor treatment outcomes [6,8] including increased mortality [9] by compromising immunity, influencing the pharmacodynamics, pharmacokinetics, tolerance, and adherence of the anti-tuberculosis treatment (ATT) [10].
Nutritional support is recommended as an integral part of TB management by WHO [11]. Nutrition supplementation interventions have effectively reduced TB incidence among household contacts [12], decreased mortality [12,13] and improved treatment outcomes [14]. Cash transfer schemes have been shown to improve treatment outcome in PwTB [15–18]. Non-receipt of direct benefit transfer (DBT) (during treatment) has been reported to be associated with death, loss to follow-up and treatment failure [15].
India suffers from high prevalence of undernutrition among PwTB [19] while also being one of the highest TB burden countries in the world. The Government of India has made a commitment to achieve the sustainable development goal end TB targets, by 2025. Under the ‘National strategic plan for TB elimination 2017–2025’, there are DBT initiatives that target all patients, specific vulnerable groups of patients like tribals, treatment providers in the private sector or treatment supporters like the Accredited Social Health Activist (ASHA) [20]. One of the DBT initiatives is the ‘Ni-kshay Poshan Yojana’ (NPY), which was launched in 1 April 2018 [21,22] to provide nutritional support to all PwTB. Under NPY, all notified PwTB receive INR 500 per month (~US$7) throughout the period of ATT [23,24]. The benefit is credited directly to the bank or post office accounts of the PwTB [20] through Public Financial Management System (PFMS).
The NPY is expected to enable PwTB to spend on their additional nutritional requirements and thus improve their nutritional status [25] and further increase the probability of favourable TB treatment outcomes. Additionally, it can also support the TB affected households in meeting the additional costs due to TB diagnosis and care and acts as an incentive for treatment adherence [15]. Previous evaluations of NPY conducted in smaller geographical regions of India had reported low coverage of NPY with longer delays [23,26–29] and documented early implementation challenges.
Entering the sixth year of its implementation, there has been no nationwide evaluation of NPY implementation and utilisation or assessment of its impact on TB treatment outcomes yet. Such evidence is required to provide vital insights to the national TB program to ensure optimal implementation of NPY. We determined the a) proportion of PwTB who had received at least one instalment, b) time to receive the first instalment, c) pattern of utilisation of the benefit, and d) impact of NPY receipt on treatment outcome.
Methods
Study design
Cross-sectional study using primary data from PwTB and secondary data from Ni-kshay, the case based real time data management system in National TB Elimination Program (NTEP).
Study setting
India is administratively divided into 28 states and eight Union Territories, which are further divided into administrative units called districts.
Under the NTEP, the district TB centres monitor the programme implementation through a network of sub-district level tuberculosis units (TUs) consisting of Peripheral Health Institutions (PHI) from both public and private sectors. All states and Union Territories of India have implemented NPY. On diagnosis, NTEP health workers collect the bank details of PwTB and the state/district level program managers validate it before forwarding them to the PFMS. The benefit will be credited upon validation of the bank or post office account details by the PFMS. The first two NPY instalments are credited together as INR 1000 (US$ 12.1) soon after diagnosis. Subsequently, advance monthly benefits of INR 500 (~US$7) are paid until their TB treatment outcome is declared.
We conducted this study in 30 districts across nine states in India namely, Bihar, Delhi, Rajasthan, Tamil Nadu, Telangana, Uttarakhand, Gujarat, Meghalaya, and Odisha under the NTEP programmatic setting.
Study population
We included PwTB aged ≥18 years, who were notified under the NTEP and whose TB treatment outcome had been declared between May 2022 and February 2023.
Sampling and sample size
We divided the states into three strata based on TB score (a composite score measuring NTEP performance and TB burden): high, medium, and low [30] (Supplementary table S1). From each stratum, we selected three states by simple random sampling and from the nine selected states, we selected thirty NTEP districts based on probability proportionate to size (TB notification) sampling. From each of the selected NTEP districts, we selected two TUs and from each TU we selected two/three PHIs using probability proportionate to size (TB notification) sampling.
Assuming that 50% of all notified PwTB would have received NPY benefit [23], we calculated a minimum required sample size of 960 persons (rounded up to 1000 per stratum) allowing a 5% alpha error, design effect of 2, absolute precision of 5% and 20% non-response. We obtained the list of all PwTB (N = 17608) in selected PHIs (N = 98) and randomly selected 25 to 30 PwTB per PHI.
Data collection
We collected data by in-person interviews from the selected PwTB or family members of deceased PwTB in their respective households using a structured electronic questionnaire on Open Data Kit (ODK) platform. We obtained PwTB demographic and clinical characteristics, and treatment outcome from current notification register (Ni-kshay), number of instalments and amount credited per instalment from NPY beneficiary register, and the dates of credit of each instalment from DBT Turn-around time (TAT) indicator register (Ni-kshay). We defined the TB treatment outcome as favourable if the documented outcome was either cured or completed.
Data analysis
The primary data were merged with the secondary data using the episode ID (Ni-kshay identifier). The proportion of PwTB who received at least one NPY instalment was estimated from the self-reported primary data and secondary data (Ni-kshay). We calculated cluster adjusted and weighted proportion of receiving at least one NPY instalment along with 95% Confidence Interval (CI) for each stratum using design weight and adjusting for non-response. We estimated the overall proportion of receipt of at least one NPY instalment based on stratum proportions. The time to receipt was calculated as the duration between the date of diagnosis and date of receipt of the first instalment. A cluster-adjusted, generalized linear model with the Poisson family and log link was used to identify factors associated with the non-receipt of NPY and to look for association between NPY receipt and unfavourable treatment outcome. To determine the association between receipt of NPY and treatment outcome, we defined receipt as PwTB who had received the first instalment before declaration of treatment outcome. Receiving the first instalment of NPY after declaration of treatment outcome was counted as non-receipt of NPY. Statistical analysis was done using Stata V.17.0 and R v.4.3.2.
Ethics and consent
The Institutional Human Ethics Committee (IHEC) of Indian Council of Medical Research – National Institute of Epidemiology (ICMR-NIE) (NIE/IHEC/202201–13) approved the study, and a non-disclosure agreement was signed between ICMR-NIE and Central TB Division for sharing the data based on the study requirements. We obtained administrative approvals from the state and district TB centres. We received informed written consent from all the study participants or family members (in case of deceased PwTB) after sharing the participant information sheet in the regional language.
Results
Sociodemographic and clinical characteristics
Of the 3201 PwTB, 1123 (35.1%) were from the low TB score stratum, 1975 (61.7%) were male, and 1381 (43.1%) were economically inactive. About 2581 (80.6%) had their own bank account. The median (IQR) monthly household income before TB was US$ 181.7 (116.3, 278.6). Medical insurance was accessible to 36.7% (n = 517) of the PwTB.
About 2698 (84.3%) PwTB were newly notified, and 2911 (90.9%) were notified from the public sector. There were 2421 (75.6%) persons with pulmonary TB and 3128 (97.7%) with drug-sensitive tuberculosis (DSTB). Thirty-two (1.0%) PwTB were HIV reactive and 307 (9.6%) were recorded as having diabetes mellitus. Overall, 248 (7.7%) PwTB had experienced unfavourable treatment outcomes (Table 1).
Table 1.
Stratum wise socio-demographic and clinical characteristics of PwTB in India, 2022 (N = 3201).
| Characteristics | Overall n (%) |
Low TB Score n (%) |
Medium TB Score n (%) |
High TB Score n (%) |
|---|---|---|---|---|
| Total | N = 3201 | N = 1123 (35.1%) | N = 1028 (32.1%) | N = 1050 (32.8%) |
| Age (in Years) | ||||
| ≥18 to ≤ 59 | 2607 (81.4) | 931 (82.9) | 809 (78.7) | 867 (82.6) |
| ≥60 | 594 (18.6) | 192 (17.1) | 219 (21.3) | 183 (17.4) |
| Gender | ||||
| Male | 1975 (61.7) | 661 (58.9) | 643 (62.5) | 671 (63.9) |
| Female | 1226 (38.3) | 462 (41.1) | 385 (37.5) | 379 (36.1) |
| Education | ||||
| Cannot read or write | 752 (23.5) | 297 (26.4) | 194 (18.9) | 261 (24.9) |
| Literate without formal schooling | 408 (12.8) | 161 (14.3) | 108 (10.5) | 139 (13.2) |
| Any formal schooling | 1604 (50.1) | 493 (43.9) | 551 (53.6) | 560 (53.3) |
| Any college education | 437 (13.6) | 172 (15.3) | 175 (17.0) | 90 (8.6) |
| Occupation† | ||||
| Self-employed | 424 (13.3) | 112 (10.0) | 138 (13.4) | 174 (16.6) |
| Employed | 1396 (43.6) | 452 (40.2) | 440 (42.8) | 504 (48.0) |
| Economically inactive | 1381 (43.1) | 559 (49.8) | 450 (43.8) | 372 (35.4) |
| Bank or Post office account | ||||
| Yes, self | 2581 (80.6) | 1029 (91.6) | 839 (81.6) | 713 (67.9) |
| Yes, relative’s/others’ | 409 (12.8) | 41 (3.7) | 143 (13.9) | 225 (21.4) |
| No | 138 (4.3) | 39 (3.5) | 21 (2.0) | 78 (7.4) |
| Do not know | 73 (2.3) | 14 (1.2) | 25 (2.4) | 34 (3.2) |
|
Monthly household income before TB Median (IQR) US $* |
181.7 (116.3, 278.6) | 181.7 (121.1, 278.6) | 181.7 (121.1, 302.8) | 157.4 (102.9, 247.1) |
| INR | 15000 (9600, 23000) | 15000 (10000, 23000) | 15000 (10000, 25000) | 13000 (8500, 20400) |
|
Monthly income of person before TB Median (IQR) US $** |
96.9 (60.6, 145.3) | 109.0 (72.7, 145.3) | 121.1 (72.7, 181.7) | 84.8 (60.6, 121.1) |
| INR | 8000 (5000, 12000) | 9000 (6000, 12000) | 10000 (6000, 15000) | 7000 (5000, 10000) |
| Notifying sector | ||||
| Public | 2911 (90.9) | 954 (84.9) | 947 (92.1) | 1010 (96.2) |
| Private | 290 (9.1) | 169 (15.1) | 81 (7.9) | 40 (3.8) |
| Type of patient | ||||
| New | 2698 (84.3) | 953 (84.9) | 896 (87.2) | 849 (80.9) |
| PMDT | 72 (2.3) | 24 (2.1) | 21 (2.0) | 27 (2.6) |
| Retreatment | 430 (13.4) | 145 (12.9) | 111(10.8) | 174 (16.6) |
| Unknown/missing | 1 (0.03) | 1 (0.1) | 0 (0.0) | 0 (0.0) |
| Site of disease | ||||
| Extrapulmonary | 763 (23.8) | 322 (28.7) | 227 (22.1) | 214 (20.4) |
| Pulmonary | 2421 (75.6) | 797 (71.0) | 797 (77.5) | 827 (78.8) |
| Unknown/missing | 17 (0.5) | 4 (0.3) | 4 (0.4) | 9 (0.8) |
| Drug type | ||||
| DSTB | 3128 (97.7) | 1098 (97.7) | 1007 (98.0) | 1023 (97.4) |
| DRTB | 72 (2.2) | 24 (2.2) | 21 (2.0) | 27 (2.6) |
| Unknown/Missing | 1 (0.1) | 1 (0.1) | 0 (0.0) | 0 (0.0) |
| HIV | ||||
| Reactive | 32 (1.0) | 4 (0.4) | 18 (1.7) | 10 (0.9) |
| Non-reactive | 3116 (97.3) | 1104 (98.3) | 1009 (98.2) | 1003 (95.5) |
| Unknown/missing | 53 (1.7) | 15 (1.3) | 1 (0.1) | 37 (3.5) |
| Diabetes | ||||
| Yes | 307 (9.6) | 78 (6.9) | 146 (14.2) | 83 (7.9) |
| No | 2782 (86.9) | 1003 (89.3) | 868 (84.4) | 911 (86.8) |
| Unknown/missing | 112 (3.5) | 42 (3.7) | 14 (1.4) | 56 (5.3) |
| Treatment outcome | ||||
| Favourable | 2953 (92.3) | 1064 (94.7) | 936 (91.1) | 953 (90.8) |
| Unfavourable | 248 (7.7) | 59 (5.3) | 92 (8.9) | 97 (9.2) |
†Self-employed (business/farm/shop); employed (regular employee government/regular employee private/temporary employee (government and private)/skilled worker/daily wage earner); economically inactive (unemployed/homemaker/retired/pensioner/student); *n = 3185, **n = 1996.
Abbreviations: PMDT, Programmatic Management of Drug Resistant Tuberculosis; DRTB, Drug-resistantuberculosis; DSTB, Drug-sensitive tuberculosis; HIV, Human Immunodeficiency Virus
Ni-kshay Poshan Yojana receipt
As per Ni-kshay, the first NPY instalment was credited to 2888 (92.7%; 95% CI 89.8%, 94.8%) PwTB of whom, 65.9% were aware of NPY receipt. Overall, when interviewed, 1903 (64.2%; 95% CI 58.9%, 69.2%) self-reported the receipt of at least one NPY instalment. The proportion of NPY receipt ranged from 90.8% (95% CI; 83.4%, 95.1%) in the low TB score stratum to 93.9% (95% CI; 88.5%, 96.9%) in the medium TB score stratum (Figure 1). The median (range) amount received by NPY recipients was INR 3000 (500,10500). Of the 2953 PwTB with favourable treatment outcomes, 2221 (75.2%) had received at least INR 3000 as benefit.
Figure 1.
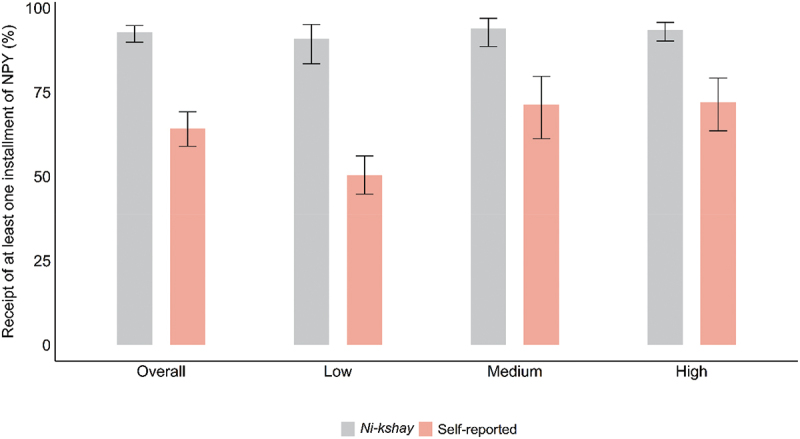
Stratum wise receipt of Ni-kshay Poshan Yojana among PwTB, India, 2022 (N = 3201).
Time to receipt of first Ni-kshay Poshan Yojana instalment
The median (IQR) time to receipt of first instalment was 105 (60,174) days. Overall, 1212 (42%) had received the first NPY instalment within two months of diagnosis, while 773 (24.1%) PwTB had received it after declaration of treatment outcome (Supplementary table S2).
Pattern of utilization of Ni-kshay Poshan Yojana
Of the 1903 PwTB who reported receipt of at least one NPY instalment, 1510 (79.4%) had completely spent the money, and 1400 (88.8%) (among partially and completely spent) had spent it on their nutritional requirements. About 86.6% (n = 1648) self-reported that the NPY incentive was insufficient to meet their nutritional requirements (Table 2).
Table 2.
Pattern of utilization of Ni-kshay Poshan Yojana instalments self-reported by the PwTB, India, 2022 (N = 1903).
| Characteristics | Overall n (%) | Low TB Score n (%) | Medium TB Score n (%) |
High TB Score n (%) |
|---|---|---|---|---|
| Total* | n = 1903 | n = 546 (28.7%) | n = 681 (35.8%) | n = 676 (35.5%) |
| Utilized NPY benefit | ||||
| Partially | 67 (3.5) | 7 (1.3) | 13 (1.9) | 47 (6.9) |
| Completely | 1510 (79.4) | 428 (78.4) | 569 (83.5) | 513 (75.9) |
| Saved for future | 180 (9.5) | 73 (13.4) | 46 (6.7) | 61 (9.0) |
| Do not know | 146 (7.7) | 38 (7.0) | 53 (7.8) | 55 (8.1) |
| Expenditure of NPY benefit# | ||||
| Nutritional requirements for oneself | 1400 (88.8) | 414 (95.2) | 507 (87.1) | 479 (85.5) |
| Nutritional requirements of the family | 259 (16.4) | 41 (9.4) | 126 (21.7) | 92 (16.4) |
| Family (excluding food and nutrition) | 61 (3.9) | 7 (1.6) | 24 (4.1) | 30 (5.4) |
| Repayment of loan/others | 22 (1.4) | 2 (0.5) | 13 (2.2) | 7 (1.3) |
| NPY incentive insufficient | 1648 (86.6) | 486 (89.0) | 586 (86.1) | 576 (85.2) |
*Received at least one NPY instalment, #Partially and completely spent the NPY instalments.
Factors associated with non-receipt of Ni-kshay Poshan Yojana instalment
PwTB from the low TB score stratum (aPR = 2.34; 95% CI 1.51, 3.62), PwTB who do not have their own bank accounts (aPR = 2.48; 95% CI 1.93, 3.19) and with unknown/missing diabetic status (aPR = 1.69; 95% CI 1.11, 2.55) were significantly (p < 0.05) associated with non-receipt of at least one NPY instalment (Table 3). There was no difference in the proportion of PwTB receiving NPY benefits across income quintiles.
Table 3.
Factors associated with non-receipt of at least one Ni-kshay Poshan Yojana instalment (based on Ni-kshay) among PwTB, India,2022 (N = 3201).
| Characteristics | N (%) | Non-recipients of NPY N = 313 (9.8%) |
Unadjusted PR* (95% CI) |
Adjusted PR (95% CI) |
|---|---|---|---|---|
| Stratum | ||||
| Low | 1123 (35.1) | 172 (15.3) | 1.71 (1.17, 2.50) | 2.34 (1.51, 3.62) |
| Medium | 1028 (32.1) | 47 (4.6) | 0.51 (0.30, 0.86) | 0.59 (0.34, 1.02) |
| High | 1050 (32.8) | 94 (8.9) | 1 | 1 |
| Age (in Years) | ||||
| ≥18 to ≤ 59 | 2607 (81.4) | 261 (10.0) | 1.14 (0.86, 1.52) | - |
| ≥60 | 594 (18.6) | 52 (8.7) | 1 | - |
| Gender | ||||
| Male | 1975 (61.7) | 199 (10.1) | 1.08 (0.86, 1.37) | - |
| Female | 1226 (38.3) | 114 (9.3) | 1 | - |
| Education | ||||
| Cannot read or write | 752 (23.5) | 81 (10.8) | 1.34 (0.87, 2.07) | 1.08 (0.70, 1.67) |
| Literate without formal schooling | 408 (12.8) | 38 (9.3) | 1.16 (0.74,1.82) | 0.98 (0.63, 1.52) |
| Any formal schooling | 1604 (50.1) | 159 (9.9) | 1.24 (0.85, 1.81) | 1.16 (0.79, 1.70) |
| Any college education | 437 (13.6) | 35 (8.0) | 1 | 1 |
| Occupation† | ||||
| Self employed | 424 (13.3) | 37 (8.7) | 0.90 (0.65, 1.25) | - |
| Employed | 1396 (43.6) | 135 (9.7) | 1 | - |
| Economically inactive | 1381 (43.1) | 141 (10.2) | 1.06 (0.85, 1.31) | - |
| Bank account | ||||
| Yes | 2581 (80.6) | 213 (8.2) | 1 | 1 |
| No | 620 (19.4) | 100 (16.1) | 1.95 (1.54, 2.48) | 2.48 (1.93, 3.19) |
| Monthly household Income before TB (quintiles)# | ||||
| 1st | 643 (20.1) | 46 (7.1) | 0.79 (0.53, 1.18) | - |
| 2nd | 703 (22.0) | 76 (10.8) | 1.19 (0.86, 1.64) | - |
| 3rd | 601 (18.8) | 66 (11.0) | 1.21 (0.86, 1.69) | - |
| 4th | 601 (18.8) | 62 (10.3) | 1.13 (0.85, 1.52) | - |
| 5th | 637 (19.9) | 58 (9.1) | 1 | - |
| Unknown/Missing | 16 (0.5) | 5 (31.2) | - | - |
| Notifying sector | ||||
| Public | 2911 (90.9) | 273 (9.4) | 1 | 1 |
| Private | 290 (9.1) | 40 (13.8) | 1.47 (0.94, 2.30) | 1.35 (0.79, 2.29) |
| Site of disease@ | ||||
| Extra pulmonary | 763 (23.8) | 60 (7.9) | 0.79 (0.60, 1.04) | 0.75 (0.56, 1.01) |
| Pulmonary | 2421 (75.6) | 240 (9.9) | 1 | 1 |
| Unknown/missing | 17 (0.5) | 13 (76.5) | - | - |
| Drug type | ||||
| DSTB | 3128 (97.7) | 305 (9.7) | - | - |
| DRTB | 72 (2.2) | 7 (9.7) | - | - |
| Unknown/missing | 1 (0.03) | 1 (100.0) | - | - |
| HIV | ||||
| Reactive | 32 (1.0) | 2 (6.2) | - | - |
| Non-reactive | 3116 (97.3) | 302 (9.7) | - | - |
| Unknown/missing | 53 (1.7) | 9 (17.0) | - | - |
| Diabetes | ||||
| Diabetic | 307 (9.6) | 26 (8.5) | 0.90 (0.61, 1.33) | 1.12 (0.80, 1.59) |
| Non-diabetic | 2782 (86.9) | 261 (9.4) | 1 | 1 |
| Unknown/missing | 112 (3.5) | 26 (23.2) | 2.47 (1.73, 3.54) | 1.69 (1.11, 2.55) |
†Self-employed (business/farm/shop); employed (regular employee government/regular employee private/temporary employee (government and private)/skilled worker/daily wage earner); economically inactive (Uunemployed/homemaker/retired/pensioner/student).
*For adjusted PR, p value of 0.2 is considered for statistical significance, 1 – reference category.
#N = 3185; @N = 3184.
Abbreviations: DSTB, Drug-sensitive Tuberculosis; DRTB, Drug-resistant Tuberculosis; HIV, Human Immunodeficiency Virus.
Ni-kshay Poshan Yojana receipt and TB treatment outcome
Sixty six (3.1%) PwTB who had received first instalment of NPY and 182 (16.8%) PwTB who had not received NPY experienced unfavourable treatment outcome. Non-receipt of NPY (aPR 4.93; 95% CI 3.61, 6.75) was significantly associated with suffering an unfavourable treatment outcome after adjusting potential confounders namely socio-demographic and clinical characteristics (Table 4).
Table 4.
Association of non-receipt of at least one Ni-kshay Poshan Yojana instalment with unfavourable treatment outcomes in PwTB, India, 2022 (N = 3201).
| Characteristics | N (%) | Unfavourable treatment outcome N = 248 (7.8%) |
Unadjusted PR (95% CI)* |
Adjusted PR (95% CI) |
|---|---|---|---|---|
| NPY receipt | ||||
| Received | 2109 (65.9) | 66 (3.1) | 1 | 1 |
| Not received | 1086 (33.9) | 182 (16.8) | 5.36 (3.94, 7.28) | 4.93 (3.61, 6.75) |
| Unknown/missing | 6 (0.2) | 0 (0) | - | - |
| Stratum | ||||
| Low | 1123 (35.1) | 59 (5.3) | 0.57 (0.38, 0.84) | 0.77 (0.49, 1.20) |
| Medium | 1028 (32.1) | 92 (9.0) | 0.97 (0.68, 1.39) | 1.45 (0.94, 2.23) |
| High | 1050 (32.8) | 97 (9.2) | 1 | 1 |
| Age (in Years) | ||||
| ≥18 to ≤ 59 | 2607 (81.4) | 172 (6.6) | 0.52 (0.40, 0.66) | 0.55 (0.42, 0.71) |
| ≥60 | 594 (18.6) | 76 (12.8) | 1 | 1 |
| Gender | ||||
| Male | 1975 (61.7) | 178 (9.0) | 1.58 (1.23, 2.02) | 1.38 (1.05, 1.80) |
| Female | 1226 (38.3) | 70 (5.7) | 1 | 1 |
| Education | ||||
| Cannot read or write | 752 (23.5) | 68 (9.0) | 1.72 (1.10, 2.68) | 1.28 (0.83, 1.96) |
| Literate without formal schooling | 408 (12.8) | 29 (7.1) | 1.35 (0.85, 2.16) | 1.25 (0.80, 1.94) |
| Any formal schooling | 1604 (50.1) | 128 (8.0) | 1.52 (1.03, 2.24) | 1.28 (0.87, 1.88) |
| Any college education | 437 (13.7) | 23 (5.3) | 1 | 1 |
| Occupation† | ||||
| Self-employed | 424 (13.3) | 40 (9.4) | 1.21 (0.85, 1.71) | - |
| Employed | 1396 (43.6) | 109 (7.8) | 1 | - |
| Economically inactive | 1381 (43.1) | 99 (7.2) | 0.92 (0.72, 1.17) | - |
| Monthly household Income before TB (quintiles)@ | ||||
| 1st quintile | 643 (20.1) | 53 (8.2) | 1.25 (0.81, 1.94) | 1.16 (0.74, 1.82) |
| 2nd quintile | 703 (22.0) | 57 (8.1) | 1.23 (0.82, 1.84) | 1.21 (0.83, 1.77) |
| 3rd quintile | 601 (18.8) | 42 (7.0) | 1.06 (0.75, 1.51) | 1.02 (0.72, 1.44) |
| 4th quintile | 601 (18.8) | 52 (8.7) | 1.31 (0.90, 1.92) | 1.42 (0.99, 2.05) |
| 5th quintile | 637 (19.9) | 42 (6.6) | 1 | 1 |
| Unknown/Missing | 16 (0.5) | 2 (12.5) | - | - |
| Notifying sector | ||||
| Public | 2911 (90.9) | 231 (7.9) | 1 | - |
| Private | 290 (9.1) | 17 (5.9) | 0.74 (0.39, 1.40) | - |
| Site of disease$ | ||||
| Extra pulmonary | 763 (23.8) | 32 (4.2) | 0.51 (0.31, 0.85) | 0.78 (0.49, 1.26) |
| Pulmonary | 2421 (75.6) | 199 (8.2) | 1 | 1 |
| Unknown/missing | 17 (0.5) | 17 (100) | - | - |
| Drug type^ | ||||
| DSTB | 3128 (97.7) | 231 (7.4) | 0.33 (0.22, 0.51) | 0.38 (0.24, 0.59) |
| DRTB | 72 (2.3) | 16 (22.2) | 1 | 1 |
| Unknown/missing | 1 (0.03) | 1 (100) | - | - |
| HIV | ||||
| Reactive | 32 (1.0) | 3 (9.4) | - | - |
| Non-reactive | 3116 (97.3) | 234 (7.5) | - | - |
| Unknown/missing | 53 (1.7) | 11 (20.8) | - | - |
| Diabetes | ||||
| Diabetic | 307 (9.6) | 33 (10.8) | 1.61 (1.12, 2.31) | 1.35 (0.93, 1.97) |
| Non-diabetic | 2782 (86.9) | 186 (6.7) | 1 | 1 |
| Unknown/missing | 112 (3.5) | 29 (25.9) | 3.87 (2.56, 5.86) | 2.58 (1.58, 4.22) |
†Self-employed (business/farm/shop); employed (regular employee government/regular employee private/temporary employee (government and private)/skilled worker/daily wage earner); economically inactive (unemployed/homemaker/retired/pensioner/student).
*For adjusted PR, p value of 0.2 is considered for statistical significance, 1 – reference category.
@N = 3185; $N = 3184; ^N = 3200.
Abbreviations: DSTB, Drug-sensitive tuberculosis; DRTB, Drug-resistant tuberculosis; HIV, Human Immunodeficiency Virus.
Discussion
In our cross-sectional study of 3201 PwTB in India, 92.7% had been credited at least one NPY instalment of whom 65.9% were aware of receipt of the benefit. The median delay in receipt of first benefit was around three months. One-fourth of the PwTB had received the benefit after declaration of treatment outcome. Most of the recipients had utilised the benefit wholly or partially for nutrition. The PwTB who did not receive NPY were more likely to experience unfavourable treatment outcomes.
The coverage of NPY was high compared to the earlier evaluations [15,18,23,26–28] possibly due to stronger political commitment to End TB, rectification of technical hiccups reported in early stages, better training of the implementing staff, and closer monitoring of NPY performance at district and state levels. The proportion of non-NPY receipt was highest among PwTB in low TB score stratum (15.3%) compared to the other strata. This may be reflective of the overall programmatic performance in the states in this stratum of which the TB score is an indicator. Previous studies conducted in low TB score states had also reported low coverage of 52.6% [31], and 10% [29] in Delhi. Other reasons for the difference in performance between the states could be due to state or district specific challenges such as being home to high proportion of migrants [31,32] and overburdening of staffs [28] or specific innovations that could have improved performance in some states.
Similar to our study, lack of bank account was reported as a major factor for the non-receipt of NPY in the previous studies [15,23,28,31]. This is because of lack of essential documents to open bank account [27], non-functional bank account [26,31], and migrant population [28]. Opening of bank account is still challenging for some PwTB especially among migrant population [28,31] and elderly despite initiatives like Pradhan Mantri Jan-Dhan Yojana (PMJDY) scheme [33], an initiative by the Government of India enabling people to open bank accounts with zero balance.
One-third of the PwTB were not aware of the receipt of the benefit. This could have been due to poor digital literacy [23], geographical access difficulties making it difficult to visit banks or ATMs, lack of counselling of the PwTB on benefits of better nutrition and provisions under NPY by the healthcare worker [34,35]. Unaware of receiving the benefit, the PwTB are also unable to utilize the benefit for nutrition.
A quarter of the PwTB had received their first instalment after their treatment outcome was declared. Similar long delays have been reported in Delhi with more than half of the PwTB receiving the first instalment during fourth and fifth month of treatment [31] and Gujarat where 34.4% PwTB received the first instalment after 6 months of treatment initiation [23]. Possible reasons for this delay could be due to the fact that bank accounts in certain rural or co-operative banks have difficulty in processing electronic transfers, re-initiating transfer after correcting bank details [28], merging of banks [26], complex formats of Ni-Kshay platform [36], technical issues due to updation and improvement of Ni-Kshay and PFMS portal [37], mismatch or rejection of bank details, unwillingness of PwTB to provide bank details [15,28], and more than one person using the same bank account [28], and the possible overload of NTEP staff [31,37]. Such delay precludes the timely utilization of the benefit by the PwTB for their nutrition.
Though received late, 88.8% of the PwTB reported fully utilising the NPY benefit for their nutrition. Similar to our results, earlier studies reported, 76% [34] and 64% [24] of the PwTB had utilised the benefits for their nutritional requirements. The possible reasons for the remaining 10.2% of PwTB not using the benefit for nutritional requirements could be the delay in receipt, lack of awareness about the purpose of the NPY benefit, and prioritising other household needs over their nutrition. There is a need for proper counselling of PwTB receiving treatment for tuberculosis about the importance of nutrition in their treatment. As reported in a previous study [38], the PwTB felt the monetary incentive is insufficient to meet their nutritional requirements. MoHFW recommends 40 Kcal/kg/day and 1.2 to 1.5 g/kg/day for an adult with BMI 21 kg/m2 [6]. Thus, an adult will require approximately 300 Kcal and 30 g protein in addition to his daily requirement of calories and proteins, which may cost a minimum of INR 750 to 1000 per month (US$ 9.1 to 12.1).
Earlier studies have also reported that PwTB who had not received the instalment were more likely to experience unfavourable treatment outcome such as loss of follow-up and death during treatment [15,39]. Timely receipt of instalment enables the PwTB to procure additional nutrition [24] in the form of protein-rich foods, supplements which improve tolerance to medication [40] and reduce loss to follow-up [15]. The better nutrition boosts immunity, also influences the pharmacodynamics and pharmacokinetics of the anti-TB drugs improving bacteriological clearance [41]. Boccia et al. discuss the numerous pathways through which a cash transfer intervention may impact TB incidence and treatment outcome [42]. Our cross-sectional design allows us to only point to this possible association, which has to be confirmed in a prospective study design or in trial settings in future studies.
Strengths and limitations
This is the first study conducted on a nationally representative sample to determine the coverage and utilization of NPY for nutrition. The variables on the generation of NPY benefits, status of credit, and dates of credit are auto-generated by the system leaving no room for errors due to manual entry or bias in analysis.
The anthropometric measures of PwTB are not recorded uniformly or in a standardized manner in Ni-kshay at the initiation of treatment. Hence, we could not assess the change in the nutritional status of PwTB through the course of anti-TB treatment. Objective verification of receipt of NPY benefit or its utilisation could not be done due to nonuniform availability of bank passbooks, or electronic messages of benefit credit or food bills among the PwTB interviewed.
Conclusion
Majority of the PwTB in India receive NPY, and most of them utilise it for nutrition. However, one-third continue to experience long delays to receive the first NPY instalment.
Recommendation
In order to reduce the delays in credit of instalment, we may increase the amount paid as first benefit and reduce the frequency of instalments to enable PwTB to utilise the benefit. The amount provided as benefit may be increased commensurate with the additional nutritional requirements recommended for PwTB. In areas where access to banking is still difficult and digital literacy is poor, we may consider alternate modes of credit of the NPY benefit or other modes of nutritional support through the program. Recording of height and weight of PwTB at diagnosis, at every follow-up visit and at treatment outcome assignment may be standardised to enable analysis determining effect of NPY benefit receipt on nutritional status and treatment outcome. To elicit the complex causal pathway between receipt of a cash benefit for nutritional support and TB treatment outcomes, future operational research may focus on novel designs and modelling exercises to address confounders and mediators.
Supplementary Material
Acknowledgments
We acknowledge Aishwarya B, Afeeq K, Afsana Khatoon, Prince Samuel J, Gokul Vikay B, Kavita Chandra, Kalaiarasi H, Kalyani D, Mercury R, Edraj J, Nandha Kumar S, Ansar Basha S, Sireesha G, Jeyashri C, Vignesh M, Muthumari D, Rajkumar E, Rajkumar T, Ashutosh Kumar Pandey, and Premnath G for collecting the quantitative data. The NPY Evaluation Group includes: B K Mishra, B K Vashisht, T K Soni, M Mawrie, Prasanta Kumar Hota, Vinod Garg, Asha Federick, A Rajesham, Pankaj Singh, Md Ashraf Rizvi, Purushottam Kumar, Anil Kataria, Sunaina Anand, Vishal Khanna, Khalid Umer Khayyam, Devendra Parmar, D N Barot, Zankhana Vasava, Easter Litha A Sangma, E Kalwing, Bayarilin Shanpru, Pravat Kumar Ojha, Biswabihari Mohanty, Niharendra Panda, Gunjan Khungara, Sudhir Sharma, Kuldeep Meena, K Jayasree, M Sankari, D Dheenadayal, M Srikanth, K Kalyan Chakravarthi, Vimal Gusain, Ramesh Kunwar, Rajesh Dhakhariyal and R K Singh.
Responsible Editor Jennifer Stewart Williams
Funding Statement
This study was funded by United States Agency for International Development and supported by Tuberculosis Implementation Framework Agreement (TIFA) implemented through John Snow Research & Training Institute Inc (JSI) under grant # 0011-0549-1023. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author contributors
JK and JWVT were involved in conceptualization. JK worked to design the study protocol and MVM, DS, JC and JWVT contributed in study design by critical revision. SP, STS, SLPG SR, SA, RS, VS, AC, SI and NPY evaluation group contributed to data collection. JK, JWVT, DS, SR, STS, and SP contributed to designing the study tool. JK, DS, JWVT, PS, and VJ contributed to data analysis. JK, DS, JWVT, and VJ prepared the tables and figures. JC, RR, SKM, and MVM reviewed the tables, figures, and results. RR, JK, DS, JWVT, VJ, SP, SLPG, and STS contributed to data interpretation. JK, SP, and SLPG prepared the first draft of the manuscript. All the investigators read, critically reviewed, and finalized the manuscript.
Data sharing policy
The datasets used and analysed in the present study are available from the corresponding author upon reasonable request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/16549716.2024.2363300.
References
- [1].Carwile ME, Hochberg NS, Sinha P.. Undernutrition is feeding the tuberculosis pandemic: a perspective. J Clin Tuberc Other Mycobact Dis. 2022;27:100311. doi: 10.1016/j.jctube.2022.100311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Central Tuberculosis Division . Ministry of health and family welfare; India TB report 2023. Leading the way. New Delhi: India; 2023. https://tbcindia.gov.in/WriteReadData/l892s/5646719104TB%20AR-2023_23-%2003-2023_LRP.pdf [Google Scholar]
- [3].Bhargava A, Bhargava M, Beneditti A, et al. Attributable is preventable: corrected and revised estimates of population attributable fraction of TB related to undernutrition in 30 high TB burden countries. J Clin Tuberc Other Mycobact Dis. 2022;27:100309. doi: 10.1016/j.jctube.2022.100309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sinha P, Davis J, Saag L, et al. Undernutrition and tuberculosis: public health implications. J Infect Dis. 2019;219:1356–10. doi: 10.1093/infdis/jiy675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lönnroth K, Castro KG, Chakaya JM, et al. Tuberculosis control and elimination 2010–50: cure, care, and social development. Lancet. 2010;375:1814–1829. doi: 10.1016/S0140-6736(10)60483-7 [DOI] [PubMed] [Google Scholar]
- [6].Central Tuberculosis Division, Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India . Guidance document - nutritional care & support for TB patients in India. New Delhi: India; 2017. Available from: https://tbcindia.gov.in/WriteReadData/Guidance%20Document%20-%20Nutritional%20Care%20%26%20Support%20for%20TB%20patients%20in%20India.pdf [Google Scholar]
- [7].Padmapriyadarsini C, Shobana M, Lakshmi M, et al. Undernutrition & tuberculosis in India: situation analysis & the way forward. Indian J Med Res. 2016;144:11–20. doi: 10.4103/0971-5916.193278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Sinha P, Lönnroth K, Bhargava A, et al. Food for thought: addressing undernutrition to end tuberculosis. Lancet Infect Dis. 2021;21:e318–e325. doi: 10.1016/S1473-3099(20)30792-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Park J, Yoon JH, Ki HK, et al. Association of duration of undernutrition with occurrence of tuberculosis. BMC Public Health. 2022;22:2392. doi: 10.1186/s12889-022-14876-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Sahile Z, Tezera R, Haile Mariam D, et al. Nutritional status and TB treatment outcomes in Addis Ababa, Ethiopia: an ambi-directional cohort study. PLOS ONE. 2021;16:e0247945. doi: 10.1371/journal.pone.0247945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].World Health Organization . Guideline: nutritional care and support for patients with tuberculosis. Geneva: World Health Organization; 2013. Available from: https://apps.who.int/iris/handle/10665/94836 [PubMed] [Google Scholar]
- [12].Bhargava A, Bhargava M, Velayutham B, et al. The RATIONS (Reducing activation of tuberculosis by improvement of nutritional sstatus) study: a cluster randomised trial of nutritional support (food rations) to reduce TB incidence in household contacts of patients with microbiologically confirmed pulmonary tuberculosis in communities with a high prevalence of undernutrition, Jharkhand, India. BMJ Open. 2021;11:e047210. doi: 10.1136/bmjopen-2020-047210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sinha P, Lakshminarayanan SL, Cintron C, et al. Nutritional supplementation would be cost-effective for reducing tuberculosis incidence and mortality in India: the ration optimization to impede tuberculosis (ROTI-TB) model. Clin Infect Dis. 2022;75:577–585. doi: 10.1093/cid/ciab1033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ukwaja KN. Social protection interventions could improve tuberculosis treatment outcomes. Lancet Glob Health. 2019;7:e167–e168. doi: 10.1016/S2214-109X(18)30523-0 [DOI] [PubMed] [Google Scholar]
- [15].Dave JD, Rupani MP. Does direct benefit transfer improve outcomes among people with tuberculosis? – a mixed-methods study on the need for a review of the cash transfer policy in India. Int J Health Policy Manag. 2022;1. doi: 10.34172/ijhpm.2022.5784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Richterman A, Steer-Massaro J, Jarolimova J, et al. Cash interventions to improve clinical outcomes for pulmonary tuberculosis: systematic review and meta-analysis. Bull World Health Organ. 2018;96:471–483. doi: 10.2471/BLT.18.208959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Alipanah N, Jarlsberg L, Miller C, et al. Adherence interventions and outcomes of tuberculosis treatment: a systematic review and meta-analysis of trials and observational studies. PLOS Med. 2018;15:e1002595. doi: 10.1371/journal.pmed.1002595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Rohit A, Kumar AMV, Thekkur P, et al. Does provision of cash incentive to HIV-infected tuberculosis patients improve the treatment success in programme settings? A cohort study from South India. J Family Med Prim Care. 2020;9:3955–3964. doi: 10.4103/jfmpc.jfmpc_474_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ministry of Health and Family Welfare, Government of India. National TB Prevalence Survey in India (2019-2021) . Summary report. New Delhi: India; 2022. Available from: https://tbcindia.gov.in/showfile.php?lid=3659 [Google Scholar]
- [20].Central Tuberculosis Division, Ministry of Health and Family Welfare, Government of India . Direct benefit transfer manual for national tuberculosis elimination programme. New Delhi: India; 2020. Available from: https://tbcindia.gov.in/WriteReadData/l892s/23294204DBTManualForNTEP.pdf [Google Scholar]
- [21].Ministry of Health and Family Welfare, Government of India . National health policy. New Delhi: India; 2017. [cited 2023 Aug 31]. Available from: https://main.mohfw.gov.in/sites/default/files/9147562941489753121.pdf [Google Scholar]
- [22].Central Tuberculosis Division . Ministry of health with family welfare, Government of India. New Delhi: India: National strategic plan for tuberculosis elimination 2017–2025; 2017. Available from: https://tbcindia.gov.in/WriteReadData/NSP%20Draft%2020.02.2017%201.pdf [Google Scholar]
- [23].Patel BH, Jeyashree K, Chinnakali P, et al. Cash transfer scheme for people with tuberculosis treated by the national TB programme in Western India: a mixed methods study. BMJ Open. 2019;9:e033158. doi: 10.1136/bmjopen-2019-033158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Sharma P, Raina A, Sharma K. Utilization of Nikshay poshan yojna in tuberculosis patients in two tuberculosis units of North India. Int J Contemp Pediatr. 2023;10:234–237. doi: 10.18203/2349-3291.ijcp20230090 [DOI] [Google Scholar]
- [25].Gupta D. Strategy and way forward for TB elimination. Indian J Tuberc. 2018;65:4–5. doi: 10.1016/j.ijtb.2017.12.013 [DOI] [PubMed] [Google Scholar]
- [26].Chadhar K, Madhappan N, Chandra A, et al. Coverage and utilization of nikshay poshan yojana among patients with tuberculosis: exploring patterns and influencing factors. Indian J Tuberc. 2023. [cited 2023 Nov 24]. doi: 10.1016/j.ijtb.2023.09.005 [DOI] [Google Scholar]
- [27].Verma P, Jadhav SL, Dhone A, et al. Coverage, delays and implementation challenges of ‘direct benefit transfer’ in the national tuberculosis elimination programme – a mixed methods study. Indian J Tuberc. 2023. [cited 2023 Oct 2]. doi: 10.1016/j.ijtb.2023.05.014 [DOI] [Google Scholar]
- [28].Nirgude AS, Kumar AMV, Collins T, et al. ‘I am on treatment since 5 months but I have not received any money’: coverage, delays and implementation challenges of ‘direct benefit transfer’ for tuberculosis patients – a mixed-methods study from South India. Glob Health Action. 2019;12:1633725. doi: 10.1080/16549716.2019.1633725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Singh SP, Khokhar A, Gupta NK. Enrolment under of nikshay poshan yojana among tuberculosis patients in a tertiary care hospital of Delhi. Indian J Tuberc. 2022;69:546–551. doi: 10.1016/j.ijtb.2021.08.032 [DOI] [PubMed] [Google Scholar]
- [30].Central Tuberculosis Division . Ministry of health and family welfare, Government of India. India TB Report 2020. New Delhi: India: National Tuberculosis Elimination Programme. Annual report; 2020. Available from: https://tbcindia.gov.in/WriteReadData/l892s/India%20TB%20Report%202020.pdf [Google Scholar]
- [31].Kumar R, Khayyam KU, Singla N, et al. Nikshay Poshan Yojana (NPY) for tuberculosis patients: early implementation challenges in Delhi, India. Indian J Tuberc. 2020;67:231–237. doi: 10.1016/j.ijtb.2020.02.006 [DOI] [PubMed] [Google Scholar]
- [32].Ministry of labour and employment. Migration of Labour in the Country . 2023. [cited 2023 Nov 6]. Available from: https://pib.gov.in/pib.gov.in/Pressreleaseshare.aspx?PRID=1941077
- [33].Ministry of Finance . Department of financial services, Government of India. Pradhan Mantri Jan-Dhan Yojana. 2016. [cited 2023 Oct 30]. https://pmjdy.gov.in/scheme [Google Scholar]
- [34].Begum J, Neelima Y, Ali SI, et al. Utilisation of nutritional support scheme among the patients of tuberculosis: a myth or a truth. J Family Med Prim Care. 2020;9:6109–6114. doi: 10.4103/jfmpc.jfmpc_1229_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Mohan M, Thangaraj JWV, Pandey S, et al. Need for operational simplicity and timely disbursal of benefits-a qualitative exploration of the implementation of a direct benefit transfer scheme for persons with tuberculosis in India. Infect Dis Poverty. 2024;13:36. doi: 10.1186/s40249-024-01206-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Hiwale M, Varadarajan V, Walambe R, et al. NikshayChain: a blockchain-based proposal for tuberculosis data management in India. Technologies. 2023;11:5. doi: 10.3390/technologies11010005 [DOI] [Google Scholar]
- [37].Nagpal M, Singh H, Chawla S, et al. Direct benefit transfer scheme for tuberculosis patients – performance challenges observed by the providers and patients. Indian J Community Health. 2022;34:72–77. doi: 10.47203/IJCH.2022.v34i01.014 [DOI] [Google Scholar]
- [38].Fuady A. Closing the evidence gap of cash transfer for tuberculosis-affected households comment on “Does direct benefit transfer improve outcomes among people with tuberculosis? - a mixed-methods study on the need for a review of the cash transfer policy in India”. Int J Health Policy Manag. 2022;12:7658. doi: 10.34172/ijhpm.2022.7658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Birlie A, Tesfaw G, Dejene T, et al. Time to death and associated factors among tuberculosis patients in Dangila Woreda, Northwest Ethiopia. PLOS ONE. 2015;10:e0144244. doi: 10.1371/journal.pone.0144244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Jahnavi G, Sudha CH. Randomised controlled trial of food supplements in patients with newly diagnosed tuberculosis and wasting. Singapore Med J. 2010;51:957–962. [PubMed] [Google Scholar]
- [41].Sinha P, Ponnuraja C, Gupte N, et al. Impact of undernutrition on tuberculosis treatment outcomes in India: a multicenter, prospective, cohort analysis. Clin Infect Dis. 2023;76:1483–1491. doi: 10.1093/cid/ciac915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Boccia D, Pedrazzoli D, Wingfield T, et al. Towards cash transfer interventions for tuberculosis prevention, care and control: key operational challenges and research priorities. BMC Infect Dis. 2016;16:307. doi: 10.1186/s12879-016-1529-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


