Abstract
Objective.
Describe COVID-19 mitigation measures in workplaces of employed, U.S. blood donors by industry and work arrangement.
Methods.
During May–December 2021, blood donors responded to a survey; we describe the distribution of reported workplace mitigation measures by industry and work arrangement organized using the hierarchy of controls.
Results.
Of 53,433 respondents representing 21 industries, ventilation upgrades were reported by 4%–38% of respondents (overall: 20%); telework access ranged from 14%–80% (53%). Requiring masks (overall: 84%; range: 40%–94%), physical distancing (77%; 51%–86%), paid leave for illness (70%; 38%–87%), and encouraging vaccination (61%; 33%–80%) were common. Independent workers reported fewer measures than those in traditional employment settings.
Conclusions.
Mitigation measures varied by industry and work arrangement. Some mitigation measures may be challenging or irrelevant to implement in certain industries, supporting the idea that mitigation is not a one-size-fits-all strategy.
Keywords: COVID-19, SARS-CoV-2, mitigation, industry, work, blood donors
Introduction:
The early stages of the 2019 novel coronavirus (COVID-19) pandemic posed significant challenges for industries worldwide.1 Mitigation measures were rapidly implemented in workplaces to prevent or reduce the transmission of SARS-CoV-2.2 Early in the pandemic, control measures included workplace closures, remote work (allowing employees to perform their duties from their homes) when possible, physical distancing, hygiene practices, and use of face masks and personal protective equipment (PPE) such as respirators.3 As the pandemic evolved, workplaces modified their mitigation strategies.4 Promotion of vaccines became a focus, as some employers mandated COVID-19 vaccinations while others took proactive measures to encourage and facilitate access to COVID-19 vaccines for their employees.5–7 Recognizing the importance of SARS-CoV-2 transmission via airborne particles and droplets, some industries also prioritized ventilation improvements8–10 to enhance indoor air quality and reduce the concentration of viral particles. This included increasing the supply of fresh air, improving filtration systems, and ensuring adequate ventilation in enclosed spaces.10–12
As the pandemic progressed, it became clear that not all strategies were equally effective in preventing workplace transmission.13,14 Widespread adoption of remote work arrangements15,16, allowance for sick leave17, implementation of physical distancing measures18, handwashing18, promotion of vaccines19, ventilation upgrades20, and use of appropriately fitted face masks or respirators18, were shown to be effective in mitigating the virus’s spread. Other mitigation strategies, such as implementation of physical barriers, COVID-19 trainings, and screening for COVID-19 symptoms at work, were shown to have mixed results on workplace transmission.18,21,22
The hierarchy of controls approach provides a framework for selecting and implementing mitigation measures.23 This approach prioritizes eliminating or substituting hazards at their source, followed by implementing engineering controls such as ventilation changes, administrative controls such as physical distancing, and finally, the use of personal protective equipment (PPE) as a last line of defense. Studies have found that participants with employers who implemented mitigation measures in all three control levels (engineering, administrative, and PPE) had lower odds of SARS-CoV-2 test positivity than those with fewer mitigation measures.24 The U.S. Centers for Disease Control and Prevention (CDC) and U.S. Occupational Safety and Health Administration (OSHA) released and updated general guidance for businesses and employers based on this framework.25,26
Although the framework provides guidance for designing mitigation strategies, implementation may vary across industries and work arrangements due to unique operational characteristics and workforce structures. Industry sectors where work might be done in open-air environments require different mitigation measures compared to industries with jobs predominantly located in indoor or potentially crowded settings.27 Similarly, work arrangements may affect the mitigation measures available to workers.28 For example, standard employment (salaried or hourly employee paid by a company) may mandate employees to follow mitigation measures that differ from those imposed by oneself when self-employed.29
Since workplaces are potential sites for SARS-CoV-2 transmission9, understanding the adoption of mitigation measures by industry is important for improving future workplace respiratory disease transmission, prevention, and control efforts. Available literature provides a limited perspective on which mitigation measures were implemented in U.S. workplaces during the COVID-19 pandemic. To date, there has not been an analysis to understand the adoption of mitigation measures by industry and work arrangement in the United States. Here, we used survey data from U.S. blood donors to describe the distribution of mitigation measures implemented by industry and work arrangement during March 2020–December 2021.
Methods:
A cohort of American Red Cross (ARC) blood donors participated in an electronic survey 2–6 weeks following their blood donation during May–December 2021; previous publications have described the survey in detail.30,31 The survey was sent to donors aged ≥18 years who were accessible by email and spoke English. The survey included questions on industry, mitigation measures used at work, and work arrangement.
Survey responses about industry were captured using free text. Responses were coded to 2012 North American Industry Classification System (NAICS) codes using the NIOSH Industry and Occupation Computerized Coding System and cross-walked to 2017 NAICS codes.32 We analyzed industry codes at the 2-digit sector group level.
Data on workplace mitigation measures came from responses to three questions (Supplemental Table 1). For questions on access to hand cleaning supplies and COVID-19 training, we combined ‘agree’ and ‘strongly agree’ responses. We also combined ‘Paid leave if you are sick with any illness including COVID-19’ and ‘Paid leave only if you are sick with COVID-19’ responses as having “Paid leave for illness.” Work arrangement was assessed directly with a question asking respondents about their work arrangement at their main job (Supplemental Table 1).
We used the hierarchy of controls to categorize mitigation measures.23 The hierarchy of controls consists of five levels, listed from most effective to least: elimination or removal of the hazard from the workplace, substitution (i.e., replacing the hazard with a less hazardous alternative), engineering controls (i.e., isolating workers from the hazard through use of machinery or barriers), administrative controls (i.e., implementing policies, procedures, and training to minimize exposure to the hazard), and PPE or source control (e.g., providing masks, respirators, gloves, or goggles to protect individuals from the hazard). In this analysis, engineering controls included changing or improving ventilation systems and installing plexiglass or other barriers or rearranging workstations to reduce exposure. Administrative controls included encouraging or providing vaccination, allowing teleworking, screening employees daily for symptoms or temperature, implementing physical distancing (6 feet or more) in the workplace, paid leave if sick with any illness, paid leave if needed to quarantine for possible COVID-19 exposure, access to hand cleaning supplies, and training about COVID-19. PPE or source control included requiring masks (including face masks or respirators) in the workplace and providing masks for employees and customers to wear.
In addition to describing all mitigation measures reported, we highlighted in figures mitigation measures that have been shown to reduce transmission of SARS-CoV-2 and varied in their implementation by industry. These measures included implemented ventilation upgrades, allowed telework, provided or encouraged vaccination, offered paid leave for illness, encouraged physical distancing, and required masks. Data on all mitigation measures are shown in supplemental tables.
Overall, 347,447 donors were eligible for the electronic survey, and 86,131 completed it (24.8% response rate) (hereafter referred to as respondents) (Figure 1). We excluded respondents with missing or less than 30 days of paid employment since March 2020 (24,483 respondents). We also excluded respondents with missing or uncodable industry and employment responses (n = 3,493), duplicate surveys (n = 284), discordant responses (survey answers on the intake form about COVID-19 did not match serological data) (n = 145), and responses where mitigation or work arrangement data was missing (n = 4,293). Following these exclusions, our analysis comprised a total of 53,433 responses (Figure 1).
Figure 1. Number of survey responses from American Red Cross blood donors collected and included in the analysis, July 2021–December 2021.
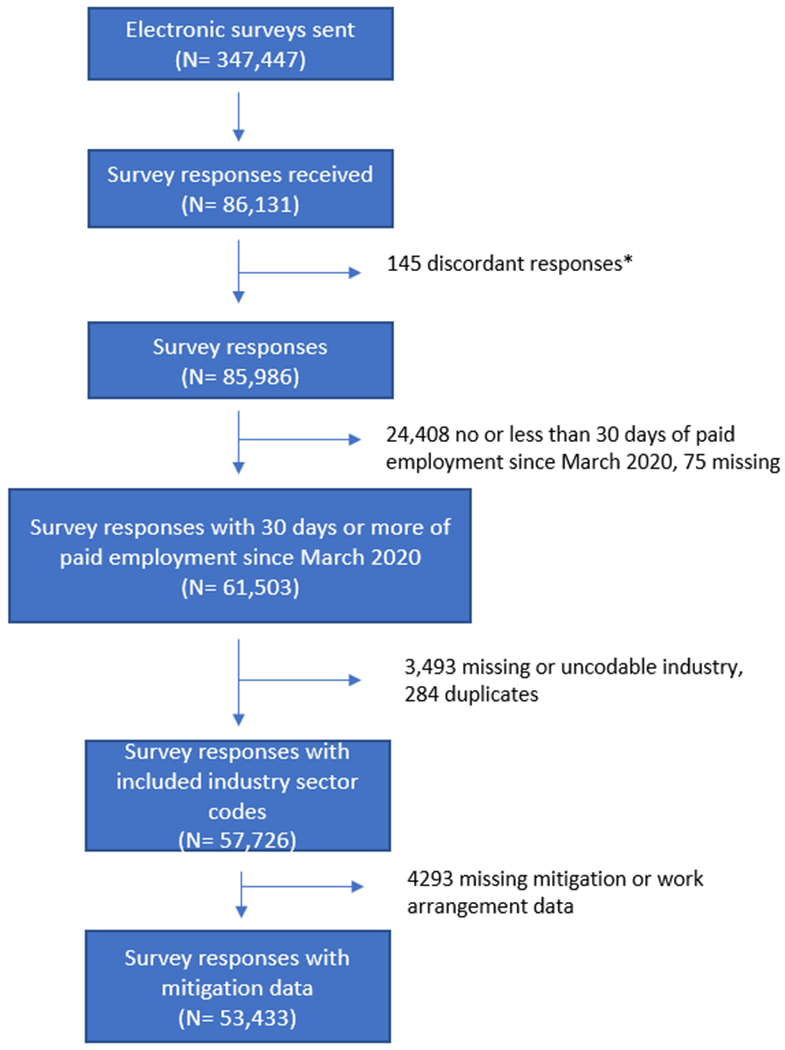
* Survey answers on the intake form about COVID-19 did not match serological data
We calculated the frequency of the aforementioned mitigation measures by industry and work arrangement. We also calculated the frequency of having one or more controls from each category (Engineering, Administrative, and PPE) to describe use of different levels of mitigation by industry and work arrangement. We conducted a sensitivity analysis excluding individuals who reported 100% telework because they may not be as familiar with other workplace mitigation measures. All analyses were conducted using R statistical software (version 4.0.3; R Foundation for Statistical Computing). Graphs were generated using Microsoft Excel (Office 16) or R statistical software.
Distribution of the survey underwent ARC institutional review board approval (IRB 2020-015). This activity was reviewed by CDC (CDC 0900f3eb81d52cce) and was conducted consistent with applicable federal law and CDC policy.*
Results:
Of 53,433 blood donor respondents included in this analysis, the largest industry groups represented were Healthcare & Social Assistance (n = 7,932), Education Services (n = 7,731), and Professional, Scientific, & Technical Services (n = 6,165) (Figure 2 and Supplemental Table 2).
Figure 2. Workplace mitigation measures in use at any time since March 2020 by industry group, U.S. Blood Donors, July 2021–December 2021.
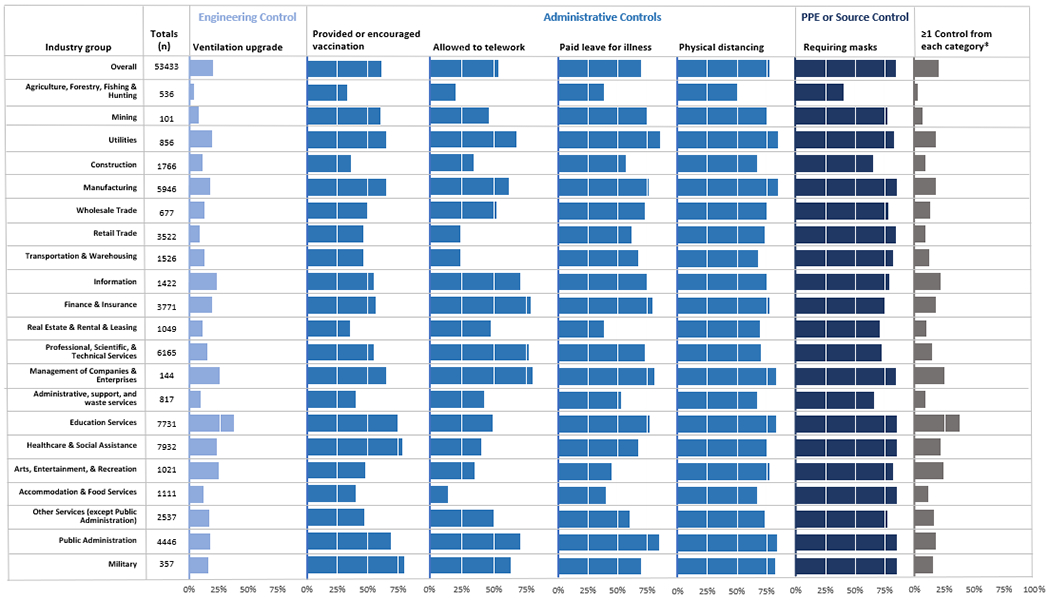
*≥1 control from each category means one or more engineering control and administrative control and Personal Protective Equipment (PPE) or source control were reported to have been implemented at the workplace.
The distribution of workplace mitigation measures in use at any time varied by industry group. Overall, almost all respondents reported access to hand cleaning supplies (n = 50,525; 95%) and COVID-19 training (n = 46,300; 87%) (Supplementary Table 2). Other frequently reported mitigation measures among all respondents were requiring masks (n = 44,664; 84%) and physical distancing (n = 40,964; 77%) (Figure 2).
Engineering Controls
A fifth of respondents reported ventilation upgrades at their workplace (n = 10,749; 20%; range across industries: 4%–38%) (Figure 2 and Supplemental Table 2). Education Services (n = 2,951; 38%) and Arts, Entertainment, & Recreation (n = 254; 25%) were industries with the highest proportion of respondents reporting ventilation upgrades. Ventilation upgrades were reported by fewer than 10% of workers in the Agriculture, Forestry Fishing & Hunting (n = 24; 4%), Mining (n = 8; 8%), and Retail Trade sectors (n = 332; 9%).
Administrative Controls
Approximately half of respondents reported they were allowed to telework (n = 28,209; 53%; range: 14%–80%) (Figure 2 and Supplemental Table 2). Management of Companies & Enterprises (n =115; 80%) and Finance & Insurance (n = 2924; 78%) had the highest proportion of workers reporting an ability to telework while Accommodation & Food Services (n = 153; 14%) and Agriculture, Forestry Fishing & Hunting (n = 106; 20%) had the lowest proportion of workers reporting an ability to telework.
Over half of respondents reported that their workplace provided or encouraged vaccination (n = 32,423; 61%; range: 33%–80%), had paid leave for illness (n = 37,493; 70%: range: 38%–85%), or promoted physical distancing (n = 40,964; 77%, range: 51%–86%) (Figure 2 and Supplemental Table 2). The top industry sectors that provided or encouraged vaccination was Military (n = 286, 80%) followed closely by Healthcare & Social Assistance (n = 6177; 78%). A high proportion of the Utilities and Public Administration sectors provided paid leave for illness (n = 742; 87% and n = 3,784; 85% respectively) and promoted physical distancing (n = 732; 86% and n = 3,716; 84% respectively). Only a third of workers in the Agriculture, Forestry, Fishing & Hunting (n = 177; 33%) or Real Estate & Rental & Leasing (n = 366; 35%) reported that their workplace provided or encouraged vaccination. Similarly, lower proportions of workers in the Agriculture, Forestry, Fishing & Hunting or Real Estate & Rental & Leasing sectors reported that their work provided paid leave for illness (n = 205; 38% and n = 402; 38% respectively).
PPE and source control
Overall, most industry sectors required masks at work (n = 44,664; 84%; range: 40%–94%) (Figure 2 and Supplemental Table 2). Requiring masking as a mitigation strategy was most frequently reported for Education Services (n = 7,286; 94%), Healthcare & Social Assistance (n = 7,362; 93%), and Military (n = 330; 92%) and least reported for Agriculture, Forestry, Fishing & Hunting (n = 213; 40%) and Administrative, Support, and Waste Services (n = 537; 66%).
Multiple levels of control
Workplaces in most industries did not implement controls from three different levels in the hierarchy of controls (Figure 2). Workplaces in Education Services had the highest proportion of one or more controls from each level reported (n = 2,860; 37%). Agriculture, Forestry, Fishing, & Hunting (n = 16; 3%), Mining (n = 7; 7%), Construction (n = 159; 9%), Retail Trade (n = 317; 9%), and Administrative, Support, & Waste Services (n= 73; 9%) relied more heavily on administrative controls or source control only.
Work arrangement
Reported workplace mitigation measures also varied by work arrangement (Figure 3 and Supplemental Table 2). Mitigation measures were reported more frequently by respondents in standard work arrangements; a high proportion of these workers reported that their workplace required masks (n = 40,619; 87%), encouraged physical distancing (n = 37,323; 80%), and provided paid leave for illness (n = 35,945; 77%). Independent contractor, consultant, or freelance workers reported lower percentages of each mitigation measure used at their workplace compared to respondents in standard work arrangements. The top work arrangement with one or more controls from each category was standard (n = 9,595; 21%) followed by paid by temp agency (n = 31; 15%). Industries with fewer reported mitigation measures tended to also be industries with more self-employed workers (Supplemental Table 3).
Figure 3. Workplace mitigation measures in use at any time since March 2020 by work arrangement, U.S. Blood Donors, July 2021–December 2021.
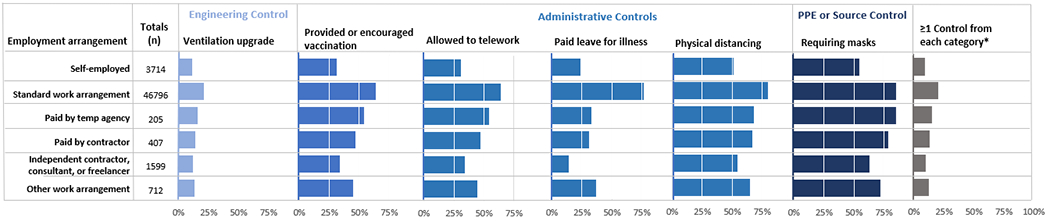
*≥1 control from each category means one or more engineering control and administrative control and Personal Protective Equipment (PPE) or source control were reported to have been implemented at the workplace.
No major differences in results by industry or by work arrangement were observed in sensitivity analysis excluding individuals who reported 100% telework (Supplemental Table 4).
Discussion
The distribution of workplace COVID-19 mitigation measures reported by employed U.S. respondents since March 2020 differed across industry groups and work arrangements. We found that Education Services and Healthcare & Social Assistance had a higher prevalence of adopting mitigation measures demonstrated to be effective. Additionally, these industries used a diverse range of strategies, incorporating multiple types of mitigation measures from various levels on the hierarchy of controls. The indoor nature of these two industries might have contributed to the number of mitigation measures employed, given greater feasibility of implementing engineering controls, such as ventilation changes. In addition, specific guidance tailored for healthcare and education settings offered by entities like CDC, OSHA, and state health departments may have played a role in the increased prevalence of mitigation measures in these two industries.
In contrast, industries such as Agriculture, Forestry, Fishing, & Hunting, Real Estate & Rental & Leasing, and Construction had fewer and less diverse mitigation measures overall. This may be attributed to several factors. First, there may be lower transmission risk in outdoor environments with higher levels of natural ventilation.33 Workers in these industries may work in non-traditional work settings such as outdoors or in semi-open spaces, or distant from others, which naturally reduced the concentration of potentially infectious air particles and minimized the risk of viral transmission compared to enclosed or crowded spaces.34 Second, barriers may exist in implementing certain mitigation measures (e.g., going to different worksites each day). The environments and dynamic nature of tasks in these industries often necessitates adaptability, which can make the implementation of mitigation strategies challenging.28 Third, the regulations within an industry, along with views of its management and workforce play a role in determining which mitigation measures are implemented.29 For instance, concerns or beliefs about vaccination among management or employees in a specific industry may lead to variations in adoption and enforcement of this mitigation strategy.6
The relationship between the extent of mitigation adoption by various industries and SARS-CoV-2 seroprevalence is complex. For example, Healthcare & Social Assistance, despite robust implementation of mitigation strategies, had high SARS-CoV-2 seroprevalence31, which may reflect the complex interplay of work-related and community-related factors in the transmission dynamics of SARS-CoV-2 among healthcare workers.35 Other industries like Accommodation & Food Services, which also had high seroprevalence31, did not exhibit a comprehensive adoption of mitigation measures. This pattern might be due to challenges some industries face in implementing effective mitigation strategies, influenced by factors such as operational characteristics, level of guidance and support from authorities, and the physical feasibility of deploying certain measures as discussed earlier.
Furthermore, the study highlighted differences in mitigation measures based on work arrangements. Respondents with standard work arrangements reported a higher number of workplace mitigation measures and that their workplaces were more likely to utilize multiple types of measures compared to self-employed individuals or contractors. This difference may be attributed to the presence of established protocols and regulations in standard work arrangements28, facilitating the implementation and enforcement of mitigation measures. Nevertheless, host employers are responsible for protecting the safety and health of all workers, including temporary and contract workers.36
Among mitigation measures included in this study, their effectiveness in preventing SARS-CoV-2 transmission has been demonstrated to differ in the published literature. Several measures, such as masking, physical distancing, and hand hygiene, have been widely recommended and implemented as crucial components of mitigating SARS-CoV-2 transmission.14,26,37 There is evidence supporting the effectiveness of these measures in reducing the spread of respiratory droplets containing the virus.14 Ventilation upgrades, including improved air filtration and increased outdoor airflow, have also been recognized as important measures in reducing indoor transmission38. These measures help dilute and remove airborne particles carrying the virus, thereby decreasing the risk of infection.
The global impact of the COVID-19 pandemic triggered a reassessment of sick leave policies. Recognizing the unprecedented challenges posed by the virus, governments worldwide responded by enacting legislation mandating paid sick leave. This shift in policy was not uniform, however, as implementation strategies varied across countries; with the United States being 1 of 11 countries without a national policy on paid sick leave for workers.39 Paid sick leave benefits allow workers to stay home or visit a healthcare provider when they are ill; comprehensive sick leave policies can mitigate the spread of infectious diseases.17 Our findings reveal variations in access to paid sick leave across industries in the United States, demonstrating room for improvement towards universal paid sick leave.
While the hierarchy of controls provides a framework for guiding the selection of mitigation measures in the workplace, the relevance and effectiveness of certain control measures, particularly in specific contexts or industries, requires consideration of the work environment, compliance, and community transmission rates. Our findings show a low prevalence of ventilation improvements in all industries as of December 2021. Although ventilation improvements may not be relevant in all environments (e.g., outdoor workplaces), these findings indicate an opportunity for improvement in many industries. In addition, our findings highlight industries within which workplaces implemented administrative, PPE, or source controls, and those that would benefit from further implementation in future responses. The combined impact of multiple strategies is believed to be more effective, forming overlapping barriers against transmission. However, the extent to which these measures complement each other and their cumulative efficacy across various settings will be informed by continued research. As we navigate future outbreaks, understanding the interplay of different mitigation strategies becomes paramount for creating robust defenses against occupational hazards. The findings from our study not only shed light on current industry practices but also emphasize the need for ongoing investigation to refine and optimize the application of the hierarchy of controls in diverse work environments.
It is important to recognize that the presence of a mitigation measure does not necessarily ensure its effective uptake, particularly with measures lower on the hierarchy of controls such as PPE. The effectiveness of these policies can be affected by factors including evolving public health guidance. Such variability can challenge the consistent application of mitigation strategies and could lead to varied outcomes across different regions and industries. Additionally, the structural setup of workplaces and the adequacy of employer support, such as making it feasible for employees to take paid leave or to access vaccination during work hours, are vital in determining the real-world effectiveness of these interventions.
Our findings should be interpreted in the context of multiple limitations. While blood donors who responded to the survey mirrored the proportions of workers in each industry group when compared to data from the Bureau of Labor Statistics40, individuals who choose to donate blood may not represent the general U.S. working population. Characteristics typical of blood donors, such as higher levels of education41 could influence their responses. Workplace mitigation measures were self-reported, and some people may not be aware of or have incorrect assumptions about the mitigation measures implemented at their workplace. For example, ventilation improvements in the workplace may not have been widely known by respondents and therefore, may be underestimated. In addition, survey wording might have been ambiguous, such as combining providing and encouraging vaccination in a single response option. This ambiguity prevented us from evaluating each component of a mitigation measure separately but represents the best information available at the time. A participant’s employment situation might have changed during the pandemic, or they may have worked more than one job; only information about their main employment was collected. Finally, no information about the timing or duration of mitigation measures or reasons for implementing or discontinuing measures was available. These limitations could have contributed to misclassification of mitigation measures or employment status in our analysis.
Supplementary Material
Policy Implications:
Tailored strategies to mitigate workplace risks of disease transmission are vital. Strategies should rely on effective methods for identifying workplace controls (e.g., hierarchy of controls) and account for industry-specific characteristics and workplace environments.
Public Health Implications.
Reported mitigation measures implemented at work within the first two years of the COVID-19 pandemic varied by industry group and work arrangement, underscoring the idea that mitigation is not a one-size-fits-all strategy. Tailored mitigation approaches that rely on proven methods for identifying workplace controls (e.g., hierarchy of controls) and account for industry-specific characteristics and workplace environments are imperative to combat future respiratory disease outbreaks.
Acknowledgements:
We acknowledge Hannah Free, Emilia Koumans, Stacey Marovich, Jeffrey Purdin, Pamela Schumacher, Jennifer Cornell, Elizabeth Smith, and Rebecca Purdin for their contributions to this project.
Funding:
The authors report that there was no funding source for the work that resulted in the article or the preparation of the article.
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Footnotes
Institution at which the work was performed: National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Cincinnati, Ohio
Institution and Ethics approval and informed consent: The American Red Cross institutional review board approved distribution of the survey (IRB 2020-015) and participants provided written informed consent. This activity was also reviewed by the Centers for Disease Control and Prevention (CDC 0900f3eb81d52cce) and was conducted consistent with applicable federal law and CDC policy.
Disclosure: the authors declare no conflicts of interest
45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq
References
- 1.West NEJ, Cheong WF, Boone E, Moat NE. Impact of the COVID-19 pandemic: a perspective from industry. Eur Heart J Suppl. 2020;22(Suppl Pt t):P56–p59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haigh KZ, Gandhi M. COVID-19 Mitigation With Appropriate Safety Measures in an Essential Workplace: Lessons for Opening Work Settings in the United States During COVID-19. Open Forum Infect Dis. 2021;8(4):ofab086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chughtai AA, Seale H, Macintyre CR. Effectiveness of Cloth Masks for Protection Against Severe Acute Respiratory Syndrome Coronavirus 2. Emerg Infect Dis. 2020;26(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guerin RJ, Barile JP, Groenewold MR, Free HL, Okun AH. COVID-19 Workplace Mitigation Strategies and Employee Leave Policies Implemented during the Height of the Pandemic, United States, Fall 2020 and 2021. Int J Environ Res Public Health. 2023;20(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothstein MA, Parmet WE, Reiss DR. Employer-Mandated Vaccination for COVID-19. Am J Public Health. 2021;111(6):1061–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruf AK, Völkl-Kernstock S, Eitenberger M, et al. Employer impact on COVID-19 vaccine uptake among nursing and social care employees in Austria. Front Public Health. 2022;10:1023914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riva MA, Paladino ME, Paleari A, Belingheri M. Workplace COVID-19 vaccination, challenges and opportunities. Occup Med (Lond). 2022;72(4):235–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riediker M, Briceno-Ayala L, Ichihara G, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med Wkly. 2022;152:w30133. [DOI] [PubMed] [Google Scholar]
- 9.Ingram C, Downey V, Roe M, et al. COVID-19 Prevention and Control Measures in Workplace Settings: A Rapid Review and Meta-Analysis. Int J Environ Res Public Health. 2021;18(15). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agarwal N, Meena CS, Raj BP, et al. Indoor air quality improvement in COVID-19 pandemic: Review. Sustain Cities Soc. 2021;70:102942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO Guidelines Approved by the Guidelines Review Committee. In: Atkinson J, Chartier Y, Pessoa-Silva CL, Jensen P, Li Y, Seto WH, eds. Natural Ventilation for Infection Control in Health-Care Settings. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 12.Morawska L, Tang JW, Bahnfleth W, et al. How can airborne transmission of COVID-19 indoors be minimised? Environ Int. 2020;142:105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yu XY, Xu C, Wang HW, et al. Effective mitigation strategy in early stage of COVID-19 pandemic in China. Infect Dis Poverty. 2020;9(1):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ayouni I, Maatoug J, Dhouib W, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mauras S, Cohen-Addad V, Duboc G, et al. Mitigating COVID-19 outbreaks in workplaces and schools by hybrid telecommuting. PLoS Comput Biol. 2021;17(8):e1009264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pizarro AB, Persad E, Durao S, et al. Workplace interventions to reduce the risk of SARS-CoV-2 infection outside of healthcare settings. Cochrane Database Syst Rev. 2022;5(5):Cd015112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pichler S, Wen K, Ziebarth NR. COVID-19 Emergency Sick Leave Has Helped Flatten The Curve In The United States. Health Aff (Millwood). 2020;39(12):2197–2204. [DOI] [PubMed] [Google Scholar]
- 18.Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. Bmj. 2021;375:e068302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mori K, Mori T, Nagata T, et al. COVID-19 vaccination coverage by company size and the effects of workplace vaccination program in Japan: a cohort study. Environ Health Prev Med. 2022;27:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghoroghi A, Rezgui Y, Wallace R. Impact of ventilation and avoidance measures on SARS-CoV-2 risk of infection in public indoor environments. Sci Total Environ. 2022;838(Pt 4):156518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bartels J, Estill CF, Chen IC, Neu D. Laboratory study of physical barrier efficiency for worker protection against SARS-CoV-2 while standing or sitting. Aerosol Sci Technol. 2022;56(3):295–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parker-Pope T Those Anti-Covid Plastic Barriers Probably Donʼt Help and May Make Things Worse. The New York Times 2021; https://www.nytimes.com/2021/08/19/well/live/coronavirus-restaurants-classrooms-salons.html. [Google Scholar]
- 23.CDC. Hierarchy of Controls - NIOSH Workplace Safety and Health Topic. Centers for Disease Control and Prevention. 2023.
- 24.Fierce L, Robey AJ, Hamilton C. High efficacy of layered controls for reducing exposure to airborne pathogens. Indoor Air. 2022;32(2):e12989. [DOI] [PubMed] [Google Scholar]
- 25.Interim guidance for businesses and employers to plan and respond to coronavirus disease 2019 (COVID-19), May 2020 : plan, prepare and pespond to coronavirus Disease 2019. 2020.
- 26.OSHA. Guidance on Preparing Workplaces for COVID-19. 2020; https://www.osha.gov/sites/default/files/publications/OSHA3990.pdf. Accessed June 27, 2023.
- 27.Cox-Ganser JM, Henneberger PK. Occupations by Proximity and Indoor/Outdoor Work: Relevance to COVID-19 in All Workers and Black/Hispanic Workers. Am J Prev Med. 2021;60(5):621–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O’Connor A, Peckham T, Seixas N. Considering Work Arrangement as an “Exposure” in Occupational Health Research and Practice. Front Public Health. 2020;8:363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Billock RM, Groenewold MR, Free H, Haring Sweeney M, Luckhaupt SE. Required and Voluntary Occupational Use of Hazard Controls for COVID-19 Prevention in Non-Health Care Workplaces - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2021;70(7):250–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah MM, Spencer BR, Feldstein LR, et al. Occupations Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Vaccination, US Blood Donors, May 2021–December 2021. Clinical Infectious Diseases. 2022. [DOI] [PubMed] [Google Scholar]
- 31.Shi DS, McDonald E, Shah M, et al. Prevalence of SARS-CoV-2 infection among US blood donors by industry, May-December 2021. Am J Ind Med. 2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collecting and Using Industry and Occupation Data. 2022; https://www.cdc.gov/niosh/topics/coding/code.html. Accessed January 31, 2023.
- 33.Bulfone TC, Malekinejad M, Rutherford GW, Razani N. Outdoor Transmission of SARS-CoV-2 and Other Respiratory Viruses: A Systematic Review. J Infect Dis. 2021;223(4):550–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Senatore V, Zarra T, Buonerba A, et al. Indoor versus outdoor transmission of SARS-COV-2: environmental factors in virus spread and underestimated sources of risk. EuroMediterr J Environ Integr. 2021;6(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chou R, Dana T, Buckley DI, Selph S, Fu R, Totten AM. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers: A Living Rapid Review. Ann Intern Med. 2020;173(2):120–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Administration OSaH. Protecting Temporary Workers. https://www.osha.gov/temporaryworkers. Accessed December 14, 2023.
- 37.Walensky RP, Del Rio C. From Mitigation to Containment of the COVID-19 Pandemic: Putting the SARS-CoV-2 Genie Back in the Bottle. Jama. 2020;323(19):1889–1890. [DOI] [PubMed] [Google Scholar]
- 38.Coyle JP, Derk RC, Lindsley WG, et al. Efficacy of Ventilation, HEPA Air Cleaners, Universal Masking, and Physical Distancing for Reducing Exposure to Simulated Exhaled Aerosols in a Meeting Room. Viruses. 2021;13(12). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heymann J, Sprague A, Earle A, McCormack M, Waisath W, Raub A. US Sick Leave In Global Context: US Eligibility Rules Widen Inequalities Despite Readily Available Solutions. Health Aff (Millwood). 2021;40(9):1501–1509. [DOI] [PubMed] [Google Scholar]
- 40.Employed persons by industry s, race, and occupation. U.S. Bureau of Labor Statistics. 2024; https://www.bls.gov/cps/cpsaat17.htm. Accessed February 1, 2024.
- 41.Patel EU, Bloch EM, Grabowski MK, et al. Sociodemographic and behavioral characteristics associated with blood donation in the United States: a population-based study. Transfusion. 2019;59(9):2899–2907. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


