Abstract
Background
In the intensive care unit (ICU), mechanical ventilation (MV) is a typical way of respiratory support. The severity of the illness raises the likelihood of death in patients who require MV. Several studies have been done in Ethiopia; however, the mortality rate differs among them. The objective of this systematic review and meta-analysis is to provide a pooled prevalence of mortality and associated factors among ICU-admitted patients receiving MV in Ethiopian hospitals.
Methods
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 criteria to conduct a comprehensive systematic review and meta-analysis in this study. We searched PubMed/Medline, SCOPUS, Embase, Hinari, and Web of Science and found 22 articles that met our inclusion criteria. We used a random-effects model. To identify heterogeneity within the included studies, meta-regression and subgroup analysis were used. We employed Egger’s regression test and funnel plots for assessing publication bias. STATA version 17.0 software was used for all statistical analyses.
Results
In this systematic review and meta-analysis, the pooled prevalence of mortality among 7507 ICU-admitted patients from 22 articles, who received MV was estimated to be 54.74% [95% CI = 47.93, 61.55]. In the subgroup analysis by region, the Southern Nations, Nationalities, and Peoples (SNNP) subgroup (64.28%, 95% CI = 51.19, 77.37) had the highest prevalence. Patients with COVID-19 have the highest mortality rate (75.80%, 95% CI = 51.10, 100.00). Sepsis (OR = 6.85, 95%CI = 3.24, 14.46), Glasgow Coma Scale (GCS) score<8 (OR = 6.58, 95%CI = 1.96, 22.11), admission with medical cases (OR = 4.12, 95%CI = 2.00, 8.48), Multi Organ Dysfunction Syndrome (MODS) (OR = 2.70, 95%CI = 4.11, 12.62), and vasopressor treatment (OR = 19.06, 95%CI = 9.34, 38.88) were all statistically associated with mortality.
Conclusion
Our review found that the pooled prevalence of mortality among mechanically ventilated ICU-admitted patients in Ethiopia was considerably high compared to similar studies in the United States (US), China, and other countries. Sepsis, GCS<8, medical cases, MODS, and use of vasopressors were statistically associated with mortality. Clinicians should exercise caution while mechanically ventilating ICU-admitted patients with these factors. However, it should be noted that the exact cause and effect relationship could not be established with this meta-analysis, as the available evidence is not sufficient. Thus, more studies using prospective methods will be required.
Introduction
In the intensive care unit (ICU), mechanical ventilation (MV) is a typical way of respiratory support. Mechanical ventilation is necessary for 20%-40% of admissions to the ICU in the United States, according to the Society of Critical Care Medicine [1]. According to the American Association for the Surgery of Trauma, more than half of ICU patients are ventilated within the first 24 hours of admission [2]. According to a study by A. Anzueto and A. Esteban, 39% to 49% of ICU patients undergo mechanical ventilation at any given moment [3]. The global burden of patients who require mechanical ventilation has increased due to the emerging severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral pandemic [4].
Between 3% and 20% of patients admitted to the hospital with coronavirus disease (COVID-19) require ICU treatment, and many of these patients require MV [5, 6]. Advances in critical care medicine, as well as the use of invasive mechanical ventilation in the ICU, have resulted in better short-term survival and mortality outcomes in critically ill patients [7, 8]. However, the degree of illness of patients admitted to the ICU increases the likelihood of death for patients requiring MV [9]. According to a large cohort study conducted in southern Brazil, the mortality rate of patients who required MV was approximately 51% [10]. Other studies in United States (US), China and an international study reported mortality rates of 29.75%, 35.36% and 28%, respectively [7, 9, 11].
In Ethiopia, the mortality rate of ICU patients receiving MV ranges from 28.6% in Tigray region’s Ayder Comprehensive Specialized Hospital to 88.5% in Addis Abeba’s St. Paul’s Millennium Medical College (SPMMC) [12, 13]. Different determinant factors have been reported in different studies done in Ethiopia. These include the presence of at least one comorbid illness, the length of stay on MV for more than three days, night time admission to the ICU, Glasgow coma scale (GCS) score ≤8 during admission, sepsis, use of vasopressor therapy, admission with medical cases, and multiple organ dysfunctions (MODS). The mortality rate also varies between different ICU settings, locations, and types of patients who were admitted to ICU and received MV [12, 14–18]. However, data on the nationally representative pooled mortality rate of ICU patients receiving MV in Ethiopia are scarce.
The objective of this systematic review and meta-analysis is to provide a pooled prevalence of mortality and associated factors among ICU-admitted patients receiving MV in Ethiopian hospitals. The findings of this research will serve as a baseline reference for local and national quality improvement activities aimed at improving the survival of ICU-admitted patients using MV. Furthermore, this review will identify the determinant factors associated with mortality in patients admitted to the ICU receiving MV and will provide information to clinicians and researchers to develop strategies to mitigate the effect of the identified determinant factors associated with mortality.
Methods
Study design and search strategy
The objective of this systematic review and meta-analysis was to determine the overall mortality rate among ICU patients in Ethiopia who received MV. For this systematic review and meta-analysis, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 checklist was used [19]. We ran a thorough search of many international databases, including PubMed/Medline, SCOPUS, Embase, Hinari, and Web of Science, to find published articles. In addition, we searched Google Scholar for unpublished studies and grey literature. All published and gray literature was retrieved, critically analyzed, and assessed for inclusion in this study until December 30, 2023.
To retrieve the articles, the following search phrases were used with "AND" and "OR" Boolean operators: (’mortality’ OR "death’ OR ’mortality rate’ OR ’rates, mortality’ OR ’death rate’ OR ’rate, death’ OR ’rates, death’) AND (’associated factors’ OR ’predictors’ OR ’determinants’) AND (’Patients who received mechanical ventilation’ OR ’Patients who received Ventilations, Mechanical’ OR ’Patients who received Mechanical Ventilations’ OR ’Patients who received Ventilation, Mechanical’) AND (’Intensive Care Units’ OR ’Intensive Care Unit’ OR ’Unit, Intensive Care’) AND (’Ethiopia’ OR ’Federal Democratic Republic of Ethiopia’). The search approach Co, Co, Pop (Condition, Context, and Population) was applied (S1 Table).
Inclusion and exclusion criteria
This review included observational studies (prospective and retrospective cohort, and cross-sectional) that reported the prevalence of mortality among pediatric and adult ICU-admitted patients who received MV in Ethiopia and were publishe or grey literature sources reported in English and published any time before December 30, 2023. Articles from which the prevalence of mortality could be estimated from the data reported in it were also included. However, articles that did not provide full text access, failed to report the prevalence of mortality in mechanically ventilated patients admitted to the ICU, and if the prevalence of mortality could not be estimated from the data within the article were excluded.
Outcomes
The primary outcome, represented as percentage and frequency in articles, was the prevalence of mortality among patients admitted to the ICU who received MV in Ethiopia. The secondary outcome was factors affecting the mortality of mechanically ventilated patients in Ethiopia, which were represented in the form of odds ratios and or in cross-tabulation as cell values of number of exposed with the outcome, number of exposed without the outcome, number of nonexposed with the outcome and number of nonexposed without the outcome. As a result, the secondary outcome was provided as odds ratios estimated by meta-analysis of odds ratios from individual studies that reported the determinant variable or the variable’s cell values from cross-tabulated data. The variables used in this meta-analysis to estimate the secondary outcome were those that were deemed statistically significant in the primary studies.
Data extraction and data quality assessment
The titles and abstracts of all the retrieved studies were independently evaluated by two reviewers (T.A. and M.A.M). Full-text review was open to papers that passed the title and abstract screening. Two authors (M.G and A.T.T) reviewed the full-text of eligible studies. The disagreement was resolved using the inclusion and exclusion criteria, and the final decision was made by the third reviewer (A.E).
Microsoft Excel 2019 was used to extract data that included the author’s name, publication year, study region, mortality prevalence, sample size, study design, and population category. Two independent reviewers (M.A.M and T.A) extracted and cross-checked the extracted data for any variations, and any inconsistencies were resolved by re-reading the full text.
The quality of the included studies was assessed using the Joanna Briggs Institute (JBI) quality assessment tool for prevalence studies [20]. The criteria to be met were as follows: 1) sample representativeness, 2) adequate sample size, 3) correct measurements, 4) acceptable statistical analysis procedures, and 5) response rates. Studies that met or above 50% of the assessment criteria were deemed low risk of bias.
Data analysis
To manage the selection process, Endnote version X8 reference management software was used. For data analysis, STATA version 17 was employed. Egger’s test and the funnel plot were used to look at potential publication bias [21, 22]. Article heterogeneity was evaluated with I2 statistics [23]. The random effects model of Der Simonian and Laird was used to assess the pooled prevalence of mortality and associated factors with 95% CI among ICU-admitted patients who underwent MV. To identify the source of heterogeneity, a meta-regression and subgroup analysis based on region, ICU type (adult versus pediatrics), COVID-19 status, study design and sample size was performed. The sensitivity test was performed to determine the impact of individual studies on the pooled estimate.
Results
Article selection
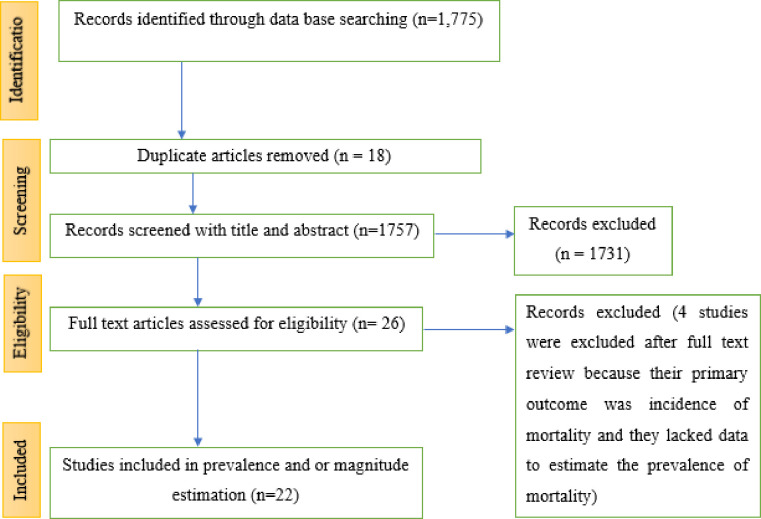
A total of 1,775 potentially qualifying studies were discovered using the PRISMA flow diagram. After eliminating duplicates and doing titles review, 26 studies were found. Four studies were excluded after full-text review because their primary outcome was incidence of mortality and they lacked data to estimate the prevalence of mortality. Finally, for the final systematic review and meta-analysis, 22 papers were included (Fig 1).
Fig 1. PRISMA flow-chart depicting the selection process of studies in Ethiopia, 2023.
Study characteristics
This review and meta-analysis included 22 studies with a total of 7507 participants that were conducted in Ethiopia and published in indexed journals or identified in grey literature. Seven of the studies were retrospective cohort, four were prospective cohort, and the remaining eleven were cross-sectional. The studies were done in Addis Ababa [12, 15–18, 24–28], Amhara [29–33], Oromia [34], Southern Nations, Nationalities and Peoples (SNNP) region [14, 35–37], and Tigray [13, 38]. The sample size ranged from 104 to 630 (Table 1).
Table 1. General characterisitcs of selected studies for the prevalence of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
| Authors name | Region | publication year | Source type | Study design | Type of ICU | Sample size | Prevalence (%) | JBI Quality |
|---|---|---|---|---|---|---|---|---|
| Alemayehu et al. [24] | Addis Ababa | 2022 | Journal | Cross-sectional | Adult | 202 | 41.7 | 9 |
| Debebe et al. [16] | Addis Ababa | 2022 | Journal | Retrospective cohort | Adult | 160 | 60.7 | 9 |
| Berhe, et al. [13] | Tigray | 2023 | Journal | Prospective cohort | Adult | 286 | 28.6 | 9 |
| Tilahun et al. [33] | Amhara | 2022 | Journal | Retrospective cohort | Adult | 376 | 33.78 | 9 |
| Zewudie et al. [32] | Amhara | 2023 | Journal | Retrospective cohort | Adult | 388 | 55.98 | 9 |
| Wotiye et al. [35] | SNNP | 2022 | Journal | Retrospective cohort | Adult | 310 | 80.82 | 7 |
| Bacha et al. [34] | Oromia | 2023 | Journal | Prospective cohort | Pediatrics | 206 | 34.5 | 7 |
| S. Seid et al. [31] | Amhara | 2022 | Journal | Cross-sectional | Adult | 402 | 37.6 | 9 |
| Tigist B. et al. [15] | Addis Ababa | 2021 | Journal | Cross-sectional | Pediatrics | 220 | 59.1 | 9 |
| Hunegnaw et al. [18] | Addis Ababa | 2022 | Journal | Cross-sectional | Adult | 247 | 57.1 | 9 |
| S.M. Abate et al. [14] | SNNP | 2021 | Journal | Retrospective cohort | Adult | 517 | 67.3 | 9 |
| Abate et al. [36] | SNNP | 2023 | Journal | Prospective cohort | Adult | 630 | 49 | 9 |
| Endeshaw et al. [25] | Addis Ababa | 2022 | Journal | Retrospective cohort | Adult | 410 | 77.45 | 9 |
| Seifu et al. [26] | Addis Ababa | 2022 | Journal | Cross-sectional | Pediatrics | 406 | 67.94 | 9 |
| Demass et al. [30] | Amhara | 2023 | Journal | Cross-sectional | Adult | 568 | 51.35 | 9 |
| Dendir et al. [37] | SNNP | 2023 | Journal | Cross-sectional | Pediatrics | 396 | 60.05 | 9 |
| Gemechu E. et al. [28] | Addis Ababa | 2022 | Journal | Cross-sectional | Pediatrics | 260 | 34.5 | 6 |
| Nega G et al. [27] | Addis Ababa | 2023 | Journal | Retrospective cohort | Adult | 496 | 63.3 | 9 |
| Korbu et al. [12] | Addis Ababa | 2023 | Journal | Cross-sectional | Adult | 104 | 88.5 | 6 |
| Tsegay et al. [17] | Addis Ababa | 2023 | Thesis | Cross-sectional | Adult | 210 | 54.8 | 9 |
| Haftu et al. [38] | Tigray | 2018 | Journal | Cross-sectional | Pediatrics | 400 | 37.5 | 9 |
| Teshager NW, et al. [29] | Amhara | 2020 | Journal | Prospective cohort | Pediatrics | 313 | 62.2 | 9 |
Prevalence of mortality among intensive care unit patients who received mechanical ventilation
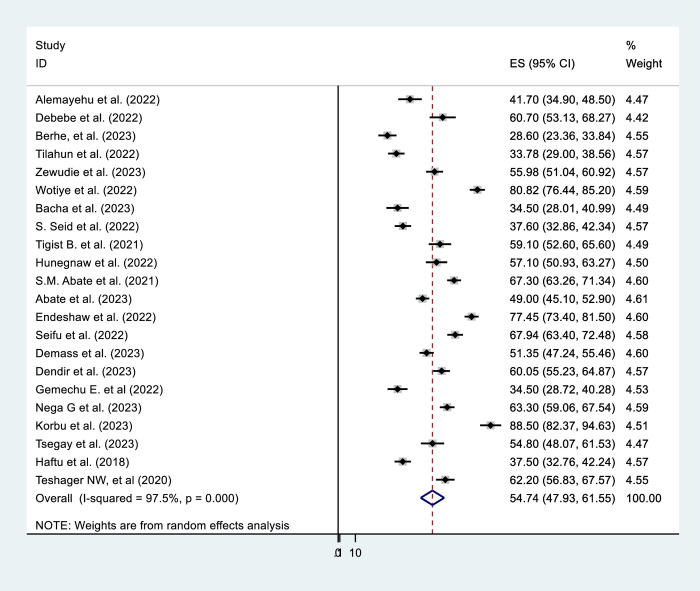
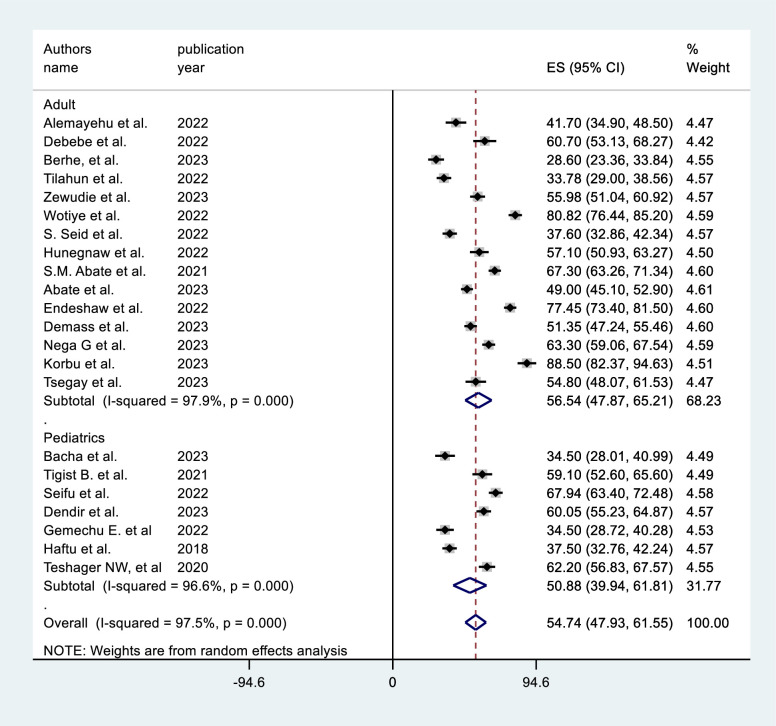
This systematic review and meta-analysis determined that the pooled prevalence of mortality among ICU-admitted patients on MV to be 54.74% [95% CI = 47.93, 61.55]. There was a high inter-study heterogeneity (I2 = 97.5%, P = 0.0001). (Fig 2). As a result, a subgroup analysis was done to identify the source of hetrogeneity by study location, sample size category, ICU type, study design and COVID-19 status (COVID-19 versus non-COVID-19 ICUs).
Fig 2. Prevalence of mortality among intensive care unit patients who received mechanical ventilation in Ethiopia, 2023.
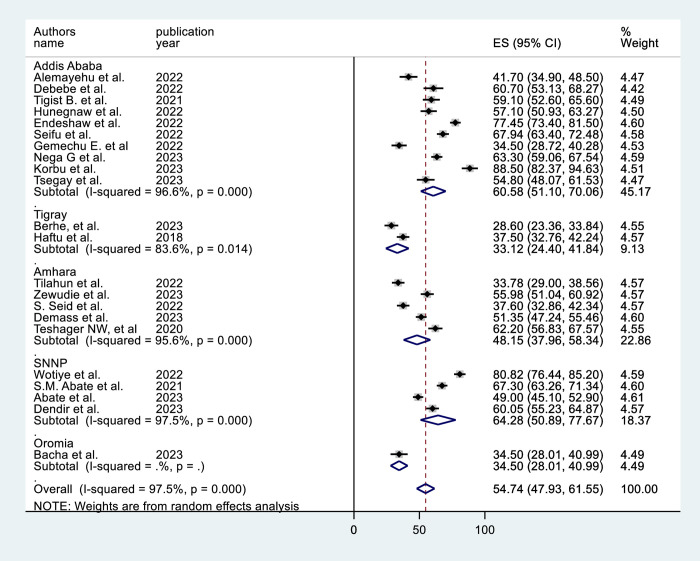
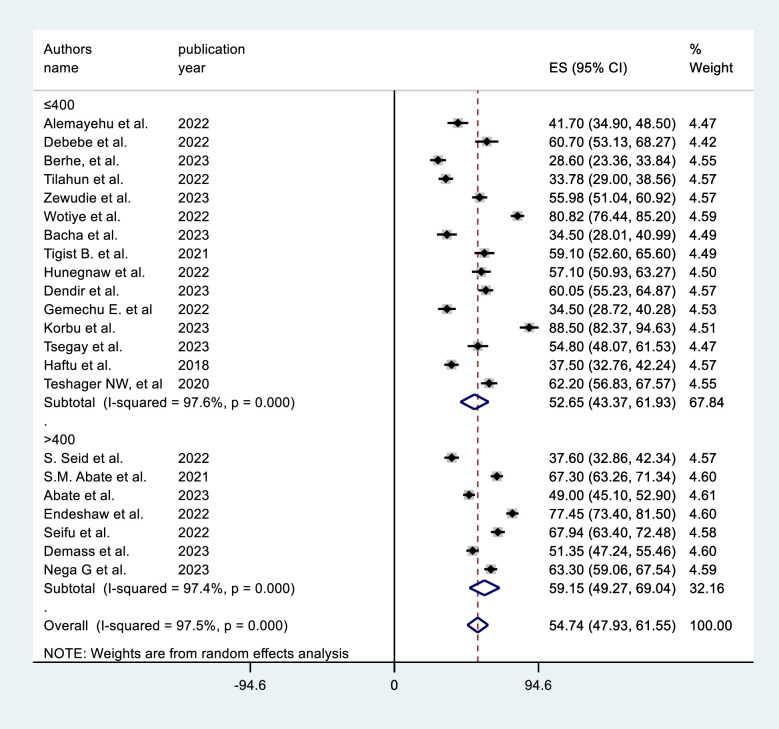
Subgroup analysis
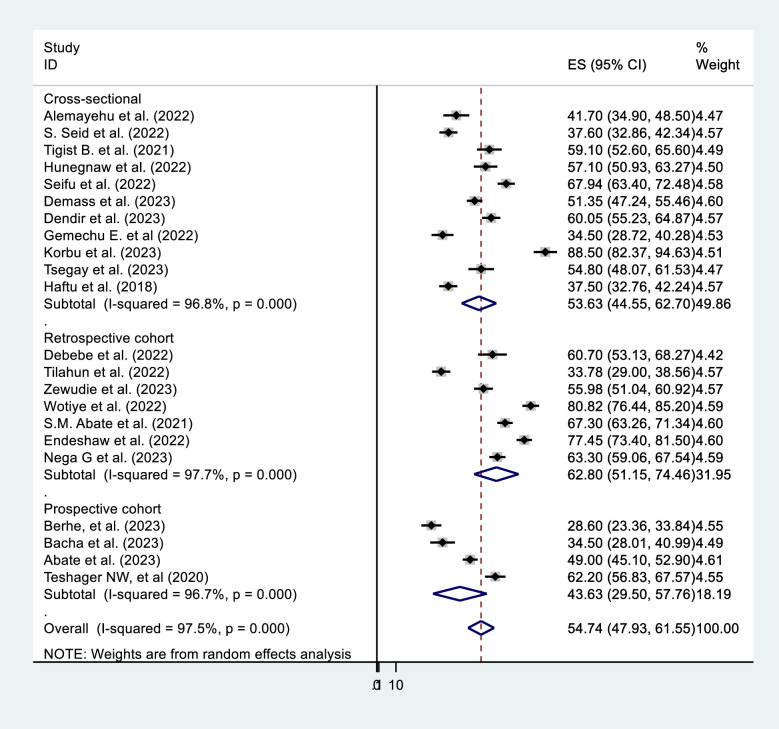
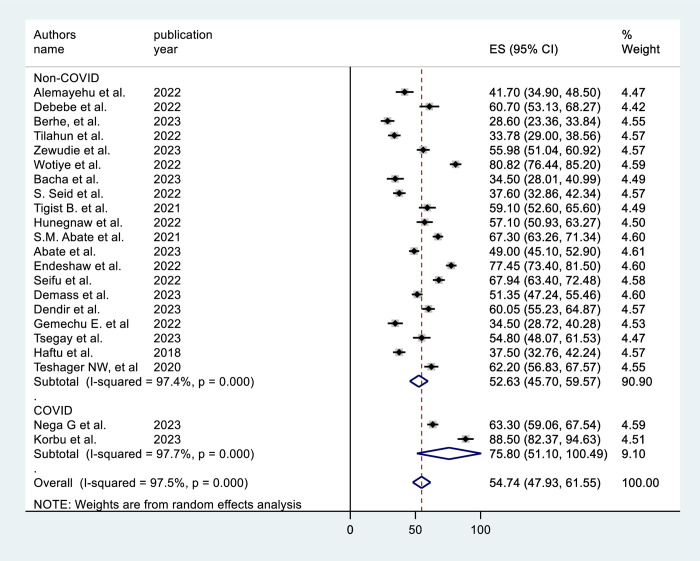
In the subgroup analysis by region, the SNNP subgroup (64.28%, 95% CI = 51.19, 77.37) had the highest prevalence (Fig 3). The subgroup analysis based on sample size shows that studies with sample size >400 results in a higher prevalence [59.15% (95% CI = 49.27, 69.04)] (Fig 4). Subgroup analysis by ICU type revealed that the studies conducted in adult ICUs yield the highest prevalence [56.4% (95% CI = 47.87, 65.21)] (Fig 5). In subgroup analysis by study design, retrospective cohort studies have the highest prevalence [62.8% (95% CI = 51.15, 74.46)], Whereas, prospective cohort studies show the lowest prevalence [43.63% (95% CI = 29.50, 57.76)] (Fig 6). The subgroup analysis of patients with COVID-19 versus non-COVID-19 patients revealed a significant difference in prevalence. COVID-19 patients have the highest mortality rate (75.80%, 95% CI = 51.10, 100.00) (Fig 7).
Fig 3. Subgroup analysis by region of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
Fig 4. Subgroup analysis by sample size of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
Fig 5. Subgroup analysis by type of ICU of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
Fig 6. Subgroup analysis by study design of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
Fig 7. Subgroup analysis by COVID-19 of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
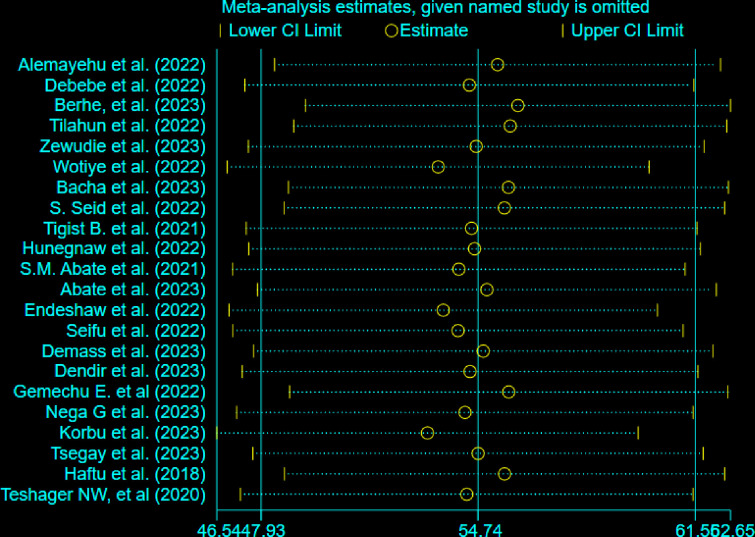
Sensitivity analysis
A sensitivity analysis was performed to see whether each study had an impact on the pooled prevalence estimates. The results of the sensitivity analysis indicated that, in a random-effects model, no study affected the total pooled prevalence (Fig 8).
Fig 8. Sensitivity analysis of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
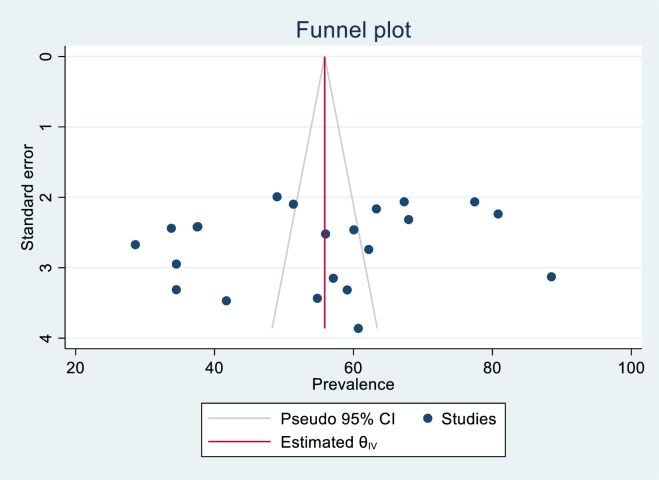
Publication bias
According to the results of Egger’s test with a p value of (p = 0.5331) and a symmetric funnel plot (Fig 9), there was no publication bias.
Fig 9. Funnel plot of mortality among mechanically ventilated ICU patients in Ethiopia, 2023.
Meta-regression
Meta-regression using publication year, JBI Quality and sample size as factors was used to find the cause of heterogeneity. However, the results demonstrated that these variables were not significant enough to be identified as causes of heterogeneity (Table 2).
Table 2. Meta-regression analysis of factors affecting between study heterogeneity.
| Hetroginity source | Coefficients | Standard error | p-valuse |
|---|---|---|---|
| Publication year | .9893661 | 3.08101 | 0.752 |
| Sample size | -.0053366 | .0274522 | 0.848 |
| JBI Quality | -2.507077 | 4.303919 | 0.567 |
Factors associated with mortality
This meta-analysis discovered various determinant factors for mortality in mechanically ventilated ICU-admitted patients in Ethiopia. GCS<8, sepsis, vasopressor use, medical cases, and the presence of MODS were significantly associated with death. Patients on MV who had sepsis were 6.85 (OR = 6.85, 95% CI = 3.24, 14.46) times more likely to die than those who did not have sepsis. Patients who were mechanically ventilated and had GCS<8 at the beginning of ventilation were 6.58 [OR = 6.58, 95%CI = 1.96, 22.11] times more likely to die than those who did not. Mechanically ventilated patients admitted with medical cases were 4.12 [OR = 4.12, 95%CI = 2.00, 8.48] times more likely to die than surgical cases admitted. Patients with MODS and on mechanical ventilation were 2.70 [OR = 2.70, 95%CI = 4.11, 12.62] times more likely to die than those without MODS. Mechanically ventilated patients who received vasopressor medication were 19.06 times more likely to die [OR = 19.06, 95% CI = 9.34, 38.88] than those who did not (Table 3).
Table 3. Factors affecting mortality of mechanically ventilated ICU patients in Ethiopia, 2023.
| Predictors | Number of studies | OR (95% CI) | I2 (p value) |
|---|---|---|---|
| Sepsis | 2 [12, 24] | 6.85 (3.24, 14.46) | 0.0% (0.349) |
| GCS<8 | 4 [16, 17, 24, 36] | 6.58 (1.96, 22.11) | 93.4% (0.000) |
| ICU admission with medical cases | 4 [15–17, 36] | 4.12 (2.00, 8.48) | 85.1% (0.000) |
| MODS | 3 [15, 17, 24] | 2.70 (4.11, 12.62) | 46.6% (0.154) |
| Vassopressor treatment | 2 [12, 24] | 19.06 (9.34, 38.88) | 0.0% (0.0975) |
Discussion
Maintaining appropriate oxygenation and ventilation while lowering the risk of complications and enabling the patient’s lungs to recover or regain function is the major objective of MV. Although MV is not typically thought of as a treatment for acute respiratory failure per se, ventilator management needs to be closely monitored, as improper ventilation could aggravate morbidity and mortality by injuring the lungs or respiratory muscles [39, 40]. The general prevalence of mortality among ICU-admitted patients using MV in Ethiopia was estimated in this systematic review and meta-analysis.
The pooled prevalence of mortality among mechanically ventilated ICU-admitted patients in Ethiopia was determined to be 54.74%, according to our review. Our findings are comparable to those of a Brazilian study (51%) [10]. Our result, however, is higher than those of other similar studies conducted in the US (29.75%) [11], China (35.36%) [9], and an international study(28%) [7]. The disparities could be related to differences in research settings, which could be described in terms of ICU advancements. The ICUs in developed nations such as the United States and China are more modern in terms of equipment and medical personnel than in Ethiopia [41].
In the subgroup analysis, there is a substantial difference in mortality prevalence between the COVID-19 and non-COVID-19 groups. Mortality was observed to be higher in mechanically ventilated COVID-19 patients than in non-COVID-19 patients (75.80% versus 52.64%). A comparable result was observed in another study, with mechanically ventilated COVID-19 patients dying at a rate of 97% [42]. This could be attributed to the acute respiratory distress syndrome and sepsis caused by COVID-19 infection [43, 44].
Compared to the other regions included in the review, the SNNP region had the highest (64.28%) prevalence of mortality. This could be owing to a regional shortage of specialist personnel and other ICU resources. According to a review of critical care services in Ethiopia released in 2022, not all ICUs in the region had critical care physicians, and the region had insufficient ventilation capacity [45].
According to this meta-analysis, mechanically ventilated individuals with sepsis were 6.85 times more likely to die than those without sepsis. A study by the Japan Sepsis Alliance study group and the American Association for Respiratory Care support this [46, 47]. This could be because MV can induce lung injury, which can aggravate the condition in patients with sepsis. Furthermore, sepsis can result in respiratory failure, which increases the risk of death [48, 49].
Patients on MV with GCS<8 at the start of ventilation were 6.58 times more likely to die than those with GCS>8. Another study found that intubation at admission was linked to increased mortality, ICU days, and overall length of stay in patients with GCS of 6–8 [50]. Tanaka, A. et al., 2022 found that patients with GCS scores < 8 had significantly higher hospital mortality [51]. Unconsciousness during admission could be a sign of a more serious condition, leading to a higher mortality rate. However, it is crucial to highlight that the association between unconsciousness and mortality is not always clear and can rely on a variety of factors such as the underlying cause of unconsciousness, the duration of unconsciousness, and the patient’s overall health status [52, 53].
The mortality rate for mechanically ventilated patients admitted with medical cases was 4.12 times higher than that of individuals admitted with surgical cases. Other similar studies by Oscar Peñuelas et al. (2021) and the Respiratory Therapy Zone webpage’s (2024) report support this [53, 54]. This could be explained by the greater likelihood of chronic respiratory disorders, such as chronic obstructive pulmonary disease (COPD), in those with medical diagnoses [55]. Another explanation is that individuals with medical conditions are often older and have more comorbidities, increasing the risk of complications and death. Patients with surgical diagnoses, on the other hand, are often younger and healthier, which can contribute to better outcomes [56].
Patients who were mechanically ventilated and had MODS were 2.70 times more likely to die than their counterparts. A comparable report has been found in two different studies: Xiao, K. et al., 2014 and Xiao, K. et al., 2020 [57, 58]. This might be due to the fact that MODS can set off a chain of events that might cause more damage to the body and increase the risk of complications and mortality [58].
Patients on MV who received vasopressor medication were 19.06 times more likely to die than those who did not. Another study conducted in Korea found that the use of vasopressors was strongly related to in-hospital mortality in mechanically ventilated patients [59]. This could be explained by the possibility of ICU-acquired weakness linked to the use of vasoactive drugs [60]. In most cases, ICU-acquired weakness is associated with considerable morbidity and mortality [61, 62].
Strength and limitation
To ensure that the findings were thorough and representative, this systematic review and meta-analysis attempted to encompass all available information, including published and gray literature, as well as cross-sectional and cohort study designs from Ethiopia. However, the included research covers only five of Ethiopia’s more than nine regions. As a result, considering the limitations inherent in the original studies would be advantageous to a more accurate interpretation of the results.
Conclusion
The pooled prevalence of mortality among mechanically ventilated ICU patients in Ethiopia was determined to be 54.74%, according to our review. This conclusion is significantly high compared to similar research in the US, China, and other countries. Sepsis, GCS<8 during admission to the ICU, medical cases, MODS, and the use of vasopressors were statistically associated with mortality. Clinicians should exercise caution while mechanically ventilating ICU-admitted patients with sepsis, who are unconscious with GCS<8, who have a medical case diagnosis, and who receive vasopressor medications. However, it is important to note that this meta-analysis could not demonstrate an accurate cause-and-effect association because the included studies only observe and record events without manipulating variables, and the available evidence is insufficient. Thus, more studies using prospective methods will be required to determine the factors that contribute to mortality in ICU-admitted patients on mechanical ventilation.
Supporting information
(DOCX)
(DOCX)
(XLSX)
Acknowledgments
Our grattitude goes to all individual at Debre Markos University, College of Health Sciences and School of Medicine, who assisted us in this review.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Fan E, Del Sorbo L, Goligher EC, Hodgson CL, Munshi L, Walkey AJ, et al. An official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. American journal of respiratory and critical care medicine. 2017;195(9):1253–63. doi: 10.1164/rccm.201703-0548ST [DOI] [PubMed] [Google Scholar]
- 2.Kirton O. Mechanical Ventilation in the Intensive Care Unit. The American Association for the Surgery Trauma, Chicago, IL, accessed May. 2011;18:2021.
- 3.Anzueto A, Esteban A. Utilization of Mechanical Ventilation in Critical Care. Yearbook of Intensive Care and Emergency Medicine 2000: Springer; 2000. p. 265–82. [Google Scholar]
- 4.Duca A, Memaj I, Zanardi F, Preti C, Alesi A, Della Bella L, et al. Severity of respiratory failure and outcome of patients needing a ventilatory support in the Emergency Department during Italian novel coronavirus SARS-CoV2 outbreak: Preliminary data on the role of Helmet CPAP and Non-Invasive Positive Pressure Ventilation. EClinicalMedicine. 2020;24. doi: 10.1016/j.eclinm.2020.100419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McWilliams D, Weblin J, Hodson J, Veenith T, Whitehouse T, Snelson C. Rehabilitation levels in patients with COVID-19 admitted to intensive care requiring invasive ventilation. An observational study. Annals of the American Thoracic Society. 2021;18(1):122–9. doi: 10.1513/AnnalsATS.202005-560OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singer AJ, Morley EJ, Meyers K, Fernandes R, Rowe AL, Viccellio P, et al. Cohort of four thousand four hundred four persons under investigation for COVID-19 in a New York hospital and predictors of ICU care and ventilation. Annals of emergency medicine. 2020;76(4):394–404. doi: 10.1016/j.annemergmed.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esteban A, Frutos-Vivar F, Muriel A, Ferguson ND, Peñuelas O, Abraira V, et al. Evolution of mortality over time in patients receiving mechanical ventilation. American journal of respiratory and critical care medicine. 2013;188(2):220–30. doi: 10.1164/rccm.201212-2169OC [DOI] [PubMed] [Google Scholar]
- 8.Donahoe MP. Current venues of care and related costs for the chronically critically ill. Respiratory care. 2012;57(6):867–88. doi: 10.4187/respcare.01656 [DOI] [PubMed] [Google Scholar]
- 9.Liang J, Li Z, Dong H, Xu C. Prognostic factors associated with mortality in mechanically ventilated patients in the intensive care unit: A single-center, retrospective cohort study of 905 patients. Medicine. 2019;98(42). doi: 10.1097/MD.0000000000017592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fialkow L, Farenzena M, Wawrzeniak IC, Brauner JS, Vieira SRR, Vigo A, et al. Mechanical ventilation in patients in the intensive care unit of a general university hospital in southern Brazil: an epidemiological study. Clinics. 2016;71:144–51. doi: 10.6061/clinics/2016(03)05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zilberberg MD, Nathanson BH, Ways J, Shorr AF. Characteristics, hospital course, and outcomes of patients requiring prolonged acute versus short-term mechanical ventilation in the United States, 2014–2018. Critical care medicine. 2020;48(11):1587–94. doi: 10.1097/CCM.0000000000004525 [DOI] [PubMed] [Google Scholar]
- 12.Deksisa A, korbu S, Solomon M, Aklog E, Zewdie A, et al. Treatment Outcomes of Mechanically Ventilated Patients with COVID-19 and Associated Factors among Hospitalized Patients at ICU of SPHMMC, Addis Ababa, Ethiopia. SciBase Crit Care Emerg Med. 2023; 1(1): 1001 [Google Scholar]
- 13.Berhe E, Gebrehiwet TG, Teka H, Gebrehiwot KG, Abraha HE, Tequare MH. Clinical characteristics and determinants of invasive mechanical ventilation outcome in adult intensive care unit in Northern Ethiopia: A resource-limited setting. Journal of the Pan African Thoracic Society. 2023;4(1):11–21. [Google Scholar]
- 14.Abate SM, Assen S, Yinges M, Basu B. Survival and predictors of mortality among patients admitted to the intensive care units in southern Ethiopia: A multi-center cohort study. Annals of Medicine and Surgery. 2021;65:102318. doi: 10.1016/j.amsu.2021.102318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bacha T, Tsegaye N, Tuli W. Characteristics and outcomes of mechanically ventilated pediatric patients in a tertiary referral hospital, Addis Ababa, Ethiopia: cross sectional study. Ethiopian journal of health sciences. 2021;31(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Debebe F, Goffi A, Haile T, Alferid F, Estifanos H, Adhikari NK. Predictors of ICU Mortality among Mechanically Ventilated Patients: An Inception Cohort Study from a Tertiary Care Center in Addis Ababa, Ethiopia. Critical Care Research and Practice. 2022;2022. doi: 10.1155/2022/7797328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsegay K, Teklu T, Debebe F, Beza L. Outcomes of Patients on Mechanical Ventilation among Adult Intensive Care Units of Tikur Anbesa Specialized Hospital, Addis Ababa, Ethiopia. 2023.
- 18.Hunegnaw W, Bayisa T. Outcome of mechanical ventilator use and associated factors at Saint Paul’s Hospital Millennium Medical College Medical Intensive Care Unit. MJH; 2022.
- 19.Tugwell P, Tovey D. PRISMA 2020. Journal of Clinical Epidemiology. 2021;134:A5–A6. doi: 10.1016/j.jclinepi.2021.04.008 [DOI] [PubMed] [Google Scholar]
- 20.Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). JBI evidence implementation. 2019;17(1):36–43. [DOI] [PubMed] [Google Scholar]
- 21.Sterne JA, Becker BJ, Egger M. The funnel plot. Publication bias in meta‐analysis: Prevention, assessment and adjustments. 2005:73–98. [Google Scholar]
- 22.Harbord RM, Harris RJ, Sterne JA. Updated tests for small-study effects in meta-analyses. The Stata Journal. 2009;9(2):197–210. [Google Scholar]
- 23.Thorlund K, Imberger G, Johnston BC, Walsh M, Awad T, Thabane L, et al. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PloS one. 2012;7(7):e39471. doi: 10.1371/journal.pone.0039471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alemayehu M, Azazh A, Hussien H, Baru A. Characteristics and outcomes of mechanically ventilated patients at adult ICU of selected public hospitals in Addis Ababa, Ethiopia. Open Access Emergency Medicine. 2022:395–404. doi: 10.2147/OAEM.S369752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Endeshaw AS, Fekede MS, Gesso AS, Aligaz EM, Aweke S. Survival status and predictors of mortality among patients admitted to surgical intensive care units of Addis Ababa governmental hospitals, Ethiopia: A multicenter retrospective cohort study. Frontiers in medicine. 2023;9:1085932. doi: 10.3389/fmed.2022.1085932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seifu A, Eshetu O, Tafesse D, Hailu S. Admission pattern, treatment outcomes, and associated factors for children admitted to pediatric intensive care unit of Tikur Anbessa specialized hospital, 2021: a retrospective cross-sectional study. BMC anesthesiology. 2022;22(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nega G, Sibhat M, Mekonnen A, Techane T. Survival status and predictors of mortality among mechanically ventilated COVID-19 patients in Addis Ababa COVID-19 Care Centers, Ethiopia: A survival analysis. F1000Research. 2023;11:1329. [Google Scholar]
- 28.Edae G, Tekleab AM, Getachew M, Bacha T. Admission pattern and treatment outcome in pediatric intensive care unit, Tertiary Hospital, Addis Ababa, Ethiopia. Ethiopian journal of health sciences. 2022;32(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Teshager NW, Amare AT, Tamirat KS. Incidence and predictors of mortality among children admitted to the pediatric intensive care unit at the University of Gondar comprehensive specialised hospital, northwest Ethiopia: a prospective observational cohort study. BMJ open. 2020;10(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Demass TB, Guadie AG, Mengistu TB, Belay ZA, Melese AA, Berneh AA, et al. The magnitude of mortality and its predictors among adult patients admitted to the Intensive care unit in Amhara Regional State, Northwest Ethiopia. Scientific reports. 2023;13(1):12010. doi: 10.1038/s41598-023-39190-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seid S, Adane H, Mekete G. Patterns of presentation, prevalence and associated factors of mortality in ICU among adult patients during the pandemic of COVID 19: a retrospective cross-sectional study. Annals of Medicine and Surgery. 2022;77:103618. doi: 10.1016/j.amsu.2022.103618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zewudie MM, Melesse DY, Filatie TD, Zeleke ME. Variables associated to intensive care unit (ICU)-mortality among patients admitted to surgical intensive care unit in Ethiopia: a retrospective observational study. BMC anesthesiology. 2023;23(1):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tilahun L, Molla A, Ayele FY, Nega A, Dagnaw K. Time to recovery and its predictors among critically ill patients on mechanical ventilation from intensive care unit in Ethiopia: a retrospective follow up study. BMC emergency medicine. 2022;22(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bacha AJ, Gadisa DA, Gudeta MD, Beressa TB, Negera GZ. Survival Status and Predictors of Mortality Among Patients Admitted to Pediatric Intensive Care Unit at Selected Tertiary Care Hospitals in Ethiopia: A Prospective Observational Study. Clinical Medicine Insights: Pediatrics. 2023;17:11795565231169498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wotiye AB, Shimber ET, Ayele BA. Factors Associated with ICU Mortality at Hawassa University Comprehensive Specialized Hospital (HUCSH). Ethiopian journal of health sciences. 2022;32(3). doi: 10.4314/ejhs.v32i3.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Abate SM, Basu B, Jemal B, Ahmed S, Mantefardo B, Taye T. Pattern of disease and determinants of mortality among ICU patients on mechanical ventilator in Sub-Saharan Africa: a multilevel analysis. Critical Care. 2023;27(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dendir G, Awoke N, Alemu A, Sintayhu A, Eanga S, Teshome M, et al. Factors associated with the outcome of a pediatric patients admitted to intensive care unit in resource-limited setup: cross-sectional study. Pediatric Health, Medicine and Therapeutics. 2023:71–9. doi: 10.2147/PHMT.S389404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haftu H, Hailu T, Medhaniye A, G/tsadik T Assessment of pattern and treatment outcome of patients admitted to pediatric intensive care unit, Ayder Referral Hospital, Tigray, Ethiopia, 2015. BMC research notes. 2018;11:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goligher EC, Ferguson ND, Brochard LJ. Clinical challenges in mechanical ventilation. The Lancet. 2016;387(10030):1856–66. doi: 10.1016/S0140-6736(16)30176-3 [DOI] [PubMed] [Google Scholar]
- 40.Pham T, Brochard LJ, Slutsky AS, editors. Mechanical ventilation: state of the art. Mayo Clinic proceedings; 2017: Elsevier. [DOI] [PubMed] [Google Scholar]
- 41.Dünser MW, Baelani I, Ganbold L. A review and analysis of intensive care medicine in the least developed countries. Critical care medicine. 2006;34(4):1234–42. doi: 10.1097/01.CCM.0000208360.70835.87 [DOI] [PubMed] [Google Scholar]
- 42.Tsikala Vafea M, Zhang R, Kalligeros M, Mylona EK, Shehadeh F, Mylonakis E. Mortality in mechanically ventilated patients with COVID-19: a systematic review. Expert Review of Medical Devices. 2021;18(5):457–71. doi: 10.1080/17434440.2021.1915764 [DOI] [PubMed] [Google Scholar]
- 43.Nicholson CJ, Wooster L, Sigurslid HH, Li RH, Jiang W, Tian W, et al. Estimating risk of mechanical ventilation and in-hospital mortality among adult COVID-19 patients admitted to Mass General Brigham: The VICE and DICE scores. EClinicalMedicine. 2021;33. doi: 10.1016/j.eclinm.2021.100765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dimbath E, Maddipati V, Stahl J, Sewell K, Domire Z, George S, et al. Implications of microscale lung damage for COVID-19 pulmonary ventilation dynamics: A narrative review. Life Sciences. 2021;274:119341. doi: 10.1016/j.lfs.2021.119341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kifle F, Boru Y, Tamiru HD, Sultan M, Walelign Y, Demelash A, et al. Intensive care in sub-Saharan Africa: a national review of the service status in Ethiopia. Anesthesia and analgesia. 2022;134(5):930. doi: 10.1213/ANE.0000000000005799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Oami T, Imaeda T, Nakada Ta, Abe T, Takahashi N, Yamao Y, et al. Mortality analysis among sepsis patients in and out of intensive care units using the Japanese nationwide medical claims database: a study by the Japan Sepsis Alliance study group. Journal of Intensive Care. 2023;11(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Freundlich RE, Li G, Leis A, Engoren M. Factors Associated With Initiation of Mechanical Ventilation in Patients With Sepsis: Retrospective Observational Study. American Journal of Critical Care. 2023;32(5):358–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang T, Shen Y, Park JG, Schulte PJ, Hanson AC, Herasevich V, et al. Outcome after intubation for septic shock with respiratory distress and hemodynamic compromise: an observational study. BMC anesthesiology. 2021;21(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Besen BAMP Tomazini BM, Azevedo LCP. Mechanical ventilation in septic shock. Current Opinion in Anesthesiology. 2021;34(2):107–12. [DOI] [PubMed] [Google Scholar]
- 50.Hatchimonji JS, Dumas RP, Kaufman EJ, Scantling D, Stoecker JB, Holena DN. Questioning dogma: does a GCS of 8 require intubation? European Journal of Trauma and Emergency Surgery. 2021;47:2073–9. doi: 10.1007/s00068-020-01383-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tanaka A, Uchiyama A, Kitamura T, Sakaguchi R, Komukai S, Matsuyama T, et al. Association between early tracheostomy and patient outcomes in critically ill patients on mechanical ventilation: a multicenter cohort study. Journal of intensive care. 2022;10(1):19. doi: 10.1186/s40560-022-00610-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang X, Zhu Y, Zhen S, Wang L. Mechanical power of ventilation is associated with mortality in neurocritical patients: a cohort study. Journal of Clinical Monitoring and Computing. 2022;36(6):1621–8. doi: 10.1007/s10877-022-00805-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peñuelas O, del Campo-Albendea L, de Aledo ALG, Añón JM, Rodríguez-Solís C, Mancebo J, et al. Long-term survival of mechanically ventilated patients with severe COVID-19: an observational cohort study. Annals of intensive care. 2021;11(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Respiratory Therapy Zone. 97+ Mechanical Ventilation Facts and Statistics (2024) 2024 Available from: https://www.respiratorytherapyzone.com/mechanical-ventilation-statistics/.
- 55.Walter K. Mechanical ventilation. Jama. 2021;326(14):1452–. doi: 10.1001/jama.2021.13084 [DOI] [PubMed] [Google Scholar]
- 56.Azizi BA, Munoz-Acuna R, Suleiman A, Ahrens E, Redaelli S, Tartler TM, et al. Mechanical power and 30-day mortality in mechanically ventilated, critically ill patients with and without Coronavirus Disease-2019: a hospital registry study. Journal of Intensive Care. 2023;11(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xiao K, Su L, Han B, Guo C, Feng L, Jiang Z, et al. Prognosis and weaning of elderly multiple organ dysfunction syndrome patients with invasive mechanical ventilation. Chinese Medical Journal. 2014;127(1):11–7. [PubMed] [Google Scholar]
- 58.Xiao K, Liu B, Guan W, Yan P, Song L, Wang Y, et al. Prognostic analysis of elderly patients with multiple organ dysfunction syndrome undergoing invasive mechanical ventilation. Journal of healthcare engineering. 2020;2020. doi: 10.1155/2020/6432048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Park S, Kim W-Y, Baek MS. Risk factors for mortality among mechanically ventilated patients requiring pleural drainage. International journal of general medicine. 2022:1637–46. doi: 10.2147/IJGM.S349249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wolfe KS, Patel BK, MacKenzie EL, Giovanni SP, Pohlman AS, Churpek MM, et al. Impact of vasoactive medications on ICU-acquired weakness in mechanically ventilated patients. Chest. 2018;154(4):781–7. doi: 10.1016/j.chest.2018.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bloch S, Polkey MI, Griffiths M, Kemp P. Molecular mechanisms of intensive care unit-acquired weakness. European Respiratory Journal. 2012;39(4):1000–11. doi: 10.1183/09031936.00090011 [DOI] [PubMed] [Google Scholar]
- 62.Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive care medicine. 2020;46(4):637–53. doi: 10.1007/s00134-020-05944-4 [DOI] [PMC free article] [PubMed] [Google Scholar]