Abstract
Background:
Toilet seat dermatitis (TSD) is a localized form of dermatitis that commonly occurs in the buttocks and upper posterior aspect of the thigh in school-going children. Previously, it was mostly seen due to allergic contact dermatitis to wood, but recently, many other allergens in toilet seats along with the possibility of irritant contact dermatitis (ICD) to detergents were reported.
Materials and Methods:
Six cases diagnosed clinically as atopic dermatitis per Hanifin and Rajka criteria presented with posterior thigh dermatitis. Patch testing using the Indian Standard Series, toilet seat scrapings, and detergents was conducted.
Results:
Patch testing showed negative results at 48, 96, and 168 hours, including lesional site testing. Symptomatic management, including topical steroids and later tacrolimus, was administered, coupled with counselling on toilet seat cover use, with a follow-up after four weeks. Lesions showed resolution and reduced itching.
Limitation:
This study’s limitation lies in its small sample size from a single geographic area.
Conclusion:
Lesion resolution through topical treatment and toilet seat avoidance, support a diagnosis of contact dermatitis; however, the role of atopy remains crucial, suggesting a complex interplay. Larger studies are needed for a comprehensive understanding of this dermatological condition.
Keywords: Atopic dermatitis, patch test, toilet seat dermatitis
Introduction
Toilet seat dermatitis (TSD) is a localized form of contact dermatitis occurring typically over the buttocks and upper posterior aspect of the thigh. Prior to the era of plastic toilet seats and sanitary covers, this condition was commoner and frequently attributed to allergic contact dermatitis (ACD) to wooden toilet seats and their associated varnishes, lacquers, and paints.[1,2] Nowadays, both ACD, due to polypropylene and, polyurethane foam, and irritant contact dermatitis (ICD) to detergents (containing quaternary ammonium compounds, phenol, and formaldehyde) have been reported to cause TSD.[3]
In this series, we intend to report six cases of TSD that we came across at our tertiary hospital in India, all of whom were negative for patch testing.
Materials and Methods
Six cases of atopic dermatitis that were clinically diagnosed as per Hanifin and Rajka criteria presented with posterior thigh dermatitis. The age of the patients ranged from 5 years to 10 years (four females and two males). The lesions in all the cases were typically limited to the buttocks and the posterior upper thigh area. The morphology of the lesions ranged from well- to ill-defined erythematous scaly plaques to papulonodular lesions present symmetrically over bilateral buttocks and posterior thighs [Figures 1–4]. The duration of the lesions in each patient was variable, ranging from 4 months to 1.5 years. The plaques were pruritic in all the patients and they had a remitting and relapsing course. Most of the patients in our series were previously clinically diagnosed with tinea corporis and were given topical and systemic antifungals, without improvement.
Figure 1.

(a) Well-defined, erythematous plaques with surface scaling present bilaterally symmetrical over the buttocks. (b) Subsidence of the erythematous plaques four weeks after therapy. Post-inflammatory hypopigmentation seen over bilateral buttocks
Figure 4.

Sharply demarcated dry scaly plaques present over outer margin of buttocks extending to posterior aspect of bilateral thighs
Figure 2.
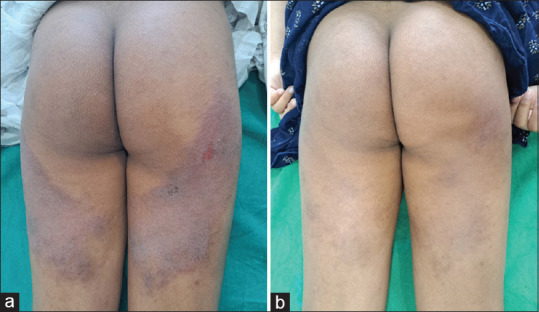
(a) Well defined erythematous scaly plaques present symmetrically over the outer margin of the buttocks extending to posterior thigh (b) Subsidence of the lesions with mild post inflammatory hyperpigmentation after 4 weeks of therapy
Figure 3.

Well- to ill-defined erythematous scaly plaques present over the outer margin of buttocks extending up to posterior aspect of thighs
Upon presentation, a detailed history and examination were done. History of atopy was elicited in all. No history of any topical application apart from antifungal was present in any of the cases. Skin scrapings were taken from the lesion and a KOH mount for fungal elements was performed which turned out to be negative in all the patients [Table 1].
Table 1.
Case series of six patients with TSD
| Age/Sex | Presentation | Duration | Relevant atopic history | Patch test | Treatment given | Follow-up (after four weeks) |
|---|---|---|---|---|---|---|
| 5 years/F | Well-defined erythematous scaly plaques over buttocks and bilateral posterior thighs | 6 months | Hyperlinear palms, family history of atopy | Negative | Short course of potent topical corticosteroids + bland emollient followed by only emollient | No new lesions or flare up and complete subsidence of existing lesions |
| 8 years/F | Well-defined erythematous scaly plaques over buttocks | 1 year | Pityriasis alba Known case of atopic dermatitis | Negative | Short course of potent topical corticosteroids + bland emollient followed by topical tacrolimus + emollient | Patient had complete subsidence by 2 weeks. New lesions appeared after 2 weeks of stoppage of topical corticosteroids |
| 9 years/M | Erythematous itchy papulo- nodular lesions over buttocks and posterior thighs | 4 months | Hyperlinear palms, Dennie Morgan folds, history of allergic rhinitis | Negative | Oral corticosteroids + anti histamines + bland emollient followed by topical tacrolimus + emollient | No new lesions or flare up and the existing lesion subsided by post-inflammatory hyperpigmentation |
| 10 years/M | Ill-defined itchy scaly plaques over outer margin of buttocks and bilateral posterior thighs | 1.5 years | Generalized xerosis, hyperlinear palms, history of allergic rhinitis, family history of atopy | Negative | Bland emollient + tacrolimus ointment + anti-histamines | No new lesions or flare up and there was complete subsidence of existing lesions |
| 7 years/F | Well-defined erythematous scaly plaques over buttocks | 5 months | History of asthma and allergic rhinitis, hyper linearity of palms, prurigo like lesions over bilateral legs | Negative | Short course of potent topical corticosteroids + bland emollient followed by topical tacrolimus + emollient | There was no complete subsidence even at the end of 4 weeks |
| 5 years/F | Well-defined erythematous plaque over the buttocks and posterior thighs with loosely adherent surface scaling | 9 months | Palmer hyper linearity, pityriasis alba and wide spread xerosis of skin | Negative | Short course of potent topical corticosteroids + bland emollient followed by topical tacrolimus + emollient | No new lesions or flare up and the existing lesions showed only superficial scaling |
Seeing the localized pattern of the lesion in the above cases, we enquired about the lavatory habits; all of the patients were using Western toilets. Hence, on the basis of the history and physical findings, a working diagnosis of toilet-seat contact dermatitis was made. Textile dermatitis as a differential was considered but ruled out as the anterior aspect was not involved in any case. Patch testing with the Indian Standard Series, scrapings of the toilet seat, and regularly used detergents (placed in a finn chamber using a micropipette at a concentration of 0.125% and 0.25% with 30 micro ml/cm2 amount)[4] was done in all the cases to know the exact causative agent.
Results
The patch testing in all cases was negative on day 2 (48 hours), day 4 (96 hours), and day 7 [Figure 5]. The lesional site was also patch tested but was negative. The patients were managed symptomatically with a short course of topical steroids which were later replaced by tacrolimus and an emollient. All patients and the parents were counseled about the source of the rash and advised to use toilet seat covers. The patients were then followed up after four weeks during which the lesions had resolved and itching was to the minimum.
Figure 5.
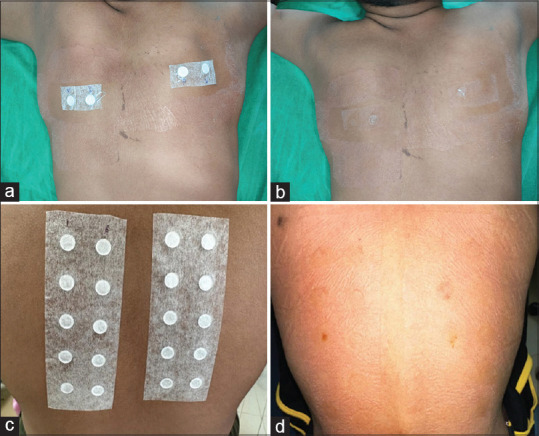
(a) Patch test performed with scrapings of toilet seat (right) and detergents at concentration of 0.125% and 0.25% (left). (b) Patch test negativity seen after 48 hours to both the agents. (c) Patch test performed with Indian standard series in the same patient. (d) Patch test negativity after 48 hours noted
Discussion
TSD has been described as a site-specific ACD to toilet seats. Wood had previously been the most common cause of toilet seat contact dermatitis,[5] but incidence declined after the replacement of wooden seats with plastic alternatives. Recently, other allergens reported in the literature include polypropylene and polyurethane foam in a worn leather seat.[6] This condition is highly misdiagnosed with tinea corporis. Increased washing of the area with soap aggravates dermatitis. TSD responds well to emollients, topical steroids, and regular use of toilet seat covers, and it is often not necessary to subject the patient to patch testing or other evaluations before starting treatment. It is important to counsel the patient and the guardian that regular use of toilet seat covers is the key to success in treatment.
Posterior thigh dermatitis, a term synonymously used for TSD, usually presents as well- to ill-defined, round, pink-red eczematous lesions over the lateral and lower posterior thighs. Hunt et al. described it as an ACD to daily use objects such as exposed metal surfaces on chair seats which was supported through patch test positivity to nickel (++) and cobalt (+). They managed the patient by proper counseling, avoidance of metal exposures with the use of chair pads or chairs without uncovered metal, and mid-potency topical corticosteroid application as needed.[7,8] The terms “atopic thigh” and “school chair sign” have been reported for this manifestation.[9]
A literature search revealed patch test positivity in cases of suspected TSD to be infrequently positive.[3] In fact, it is now believed that ICD to detergents used to clean the toilets may be another causative factor. In a recent study of TSD in the pediatric age group, they found thiomersal as the most common allergen positive for patch testing followed by cetrimide, neomycin, cobalt, PPD (para-phenylenediamine), potassium dichromate, and epoxy resin.[10] Among these allergens, thiomersal, being the commonest, is not present in the Indian Standard Series which might be the reason for patch test negativity.
Another common denominator in most reports of patients developing TSD was a personal or family history of atopy.[11] It is a well-known fact that atopic patients are predisposed to developing both ACD and ICD. In a retrospective study done by Hogeling et al., 100 children and adolescents were studied to determine the frequency of patch test positivity in the pediatric population. The most positive test was seen with nickel sulfate followed by cobalt. They observed that 41% of the children had a history of atopic dermatitis.[12]
Limitation
Further studies should be conducted with a larger sample size involving patients from various geographical areas.
Conclusion
In our case series of six atopic children presenting with TSD, the patch test (toilet seat scrapings and detergents) was negative in all the patients. This creates a debatable doubt of whether this is just a minor manifestation of atopic dermatitis rather than contact dermatitis. However, the relevance of this finding is questionable considering that it is quite possible to miss the exact allergen in suspected ACD cases. Also, ICD to detergents causing TSD is another possibility. Although clearing of the lesions with topical treatment, strict avoidance of contact with the toilet seats, and use of toilet liners still favor contact dermatitis, the background of atopy should be considered as an important contributory factor in all patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.MacKee GM. X-Rays and Radium in the Treatment of Diseases of the Skin. 2nd ed. Philadelphia, PA: Lea and Febiger; 1927. [Google Scholar]
- 2.Heilig S, Adams DR, Zaenglein AL. Persistent allergic contact dermatitis to plastic toilet seats. Pediatr Dermatol. 2011;28:587–59. doi: 10.1111/j.1525-1470.2010.01211.x. [DOI] [PubMed] [Google Scholar]
- 3.Litvinov IV, Sugathan P, Cohen BA. Recognizing and treating toilet-seat contact dermatitis in children. Pediatrics. 2010;125:e419–22. doi: 10.1542/peds.2009-2430. [DOI] [PubMed] [Google Scholar]
- 4.Johansen JD, Aalto-Korte K, Agner T, Andersen KE, Bircher A, Bruze M, et al. European society of contact dermatitis guideline for diagnostic patch testing –recommendations on best practice. Contact Dermatitis. 2015;73:195–221. doi: 10.1111/cod.12432. [DOI] [PubMed] [Google Scholar]
- 5.Holme SA, Stone NM, Mills CM. Toilet seat contact dermatitis. Pediatr Dermatol. 2005;22:344–5. doi: 10.1111/j.1525-1470.2005.22413.x. [DOI] [PubMed] [Google Scholar]
- 6.Turan H, Saricaoglu H, Turan A, Tunali S. Polyurethane toilet seat contact dermatitis. Pediatr Dermatol. 2011;28:731–2. doi: 10.1111/j.1525-1470.2011.01482.x. [DOI] [PubMed] [Google Scholar]
- 7.Hunt RD, Feldstein SI, Krakowski AC. Itching to learn: School chair allergic contact dermatitis on the posterior thighs. J Clin Aesthet Dermatol. 2014;7:48–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Pride HB, Tollefson M, Silverman R. What's new in pediatric dermatology?Part I. Diagnosis and pathogenesis. J Am Acad Dermatol. 2013;68:885.e1–12. doi: 10.1016/j.jaad.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Fredriksson T, Faergemann J. The atopic thigh: A “starting-school'symptom? Acta Derm Venereol. 1981;61:452–3. [PubMed] [Google Scholar]
- 10.Mohamed NKV, Rashmi Mary Philip. Study of toilet seat dermatitis in pediatric age groups. Indian J Appl Res. 2019;9 [Google Scholar]
- 11.Dorfman CO, Barros MA, Zaenglein AL. Contact dermatitis to training toilet seat (potty seat dermatitis) Pediatr Dermatol. 2018;35:251–2. doi: 10.1111/pde.13534. [DOI] [PubMed] [Google Scholar]
- 12.Hogeling M, Pratt M. Allergic contact dermatitis in children: The Ottawa hospital patch-testing clinic experience, 1996 to 2006. Dermatitis. 2008;19:86–9. [PubMed] [Google Scholar]


