Abstract
The meniscal position within the knee is critical to maintain normal knee function. The joint capsule might dynamically coordinate the medial meniscus (MM) by transmitting a semimembranosus action. However, their interrelationships in vivo are unclear. We aimed to determine relationships among the MM, joint capsule, and semimembranosus during passive tibial external-internal and isometric tibial internal rotation at the medial and posteromedial knees of 10 healthy individuals in vivo using ultrasound. We analyzed images of the MM and joint capsule locations at the medial and posteromedial knee and the velocity waveform similarity of each structure during rotational tasks. Both isometric internal rotation with semimembranosus action and passive tibial external rotation displaced the MM inward at the medial knee. The MM and joint capsule during these MM displacements coordinately moved with more than moderate cross-correlation coefficients (passive external and isometric internal rotations, ≥ 0.54 and ≥ 0.90, respectively). The movements of the MM and joint capsule to the semimembranosus during isometric internal rotation also coordinated with moderate cross-correlation coefficients (≥ 0.62). Therefore, the joint capsule might dynamically coordinate the MM by transmitting semimembranosus action. Whether increased tibial internal rotation or semimembranosus shortening causes MM extrusion awaits further investigation.
Keywords: Joint capsule, Medial meniscus, Semimembranosus, Tibial rotation, Ultrasonography
Subject terms: Musculoskeletal system, Ultrasonography, Rehabilitation
Introduction
The meniscus in the proper position can transmit the load from the knee while dispersing the mechanical stress between the femur and tibia. Therefore, the position of the meniscus within the knee is critical for maintaining normal knee function1. Notably, medial meniscal (MM) extrusion, the displacement of the MM beyond the outermost margin of the tibial plateau, has recently been considered a structural cause of early knee osteoarthritis2–5. Understanding the stabilization mechanism that maintains the MM in a proper position may contribute to establishing prevention methods for the initiation and progression of early knee osteoarthritis.
The MM has been supported by the static stabilizer provided by the ligament (e.g., the medial collateral ligament) and dynamic stabilizer provided by the muscles (e.g., the semimembranosus and muscles comprising the pes anserinus, such as the semitendinosus, gracilis, and sartorius)6–11. The semimembranosus has been well focused especially as the dynamic stabilizer due to its connection to the joint capsule6–8. In contrast, a recent anatomical study clarified that the conventional posteromedial knee ligaments, including the medial collateral ligament, were not distinct cord-like structures but part of the joint capsule that formed the semimembranosus tendinous sheath12. Therefore, the proposed anatomical hypothesis was that the knee ligaments and muscles may not independently coordinate the MM location; instead, the joint capsule may dynamically coordinate the MM by transmitting the muscular force of the semimembranosus through the tendinous sheaths12. However, these interrelationships among the movements of the MM, joint capsule, and semimembranosus have not yet been fully elucidated in vivo.
To investigate these interrelationships among the MM, joint capsule, and semimembranosus, tibial rotation is an appropriate exercise task because the MM at the medial knee moves inward during external rotation13,14, conventional knee ligaments, such as the medial collateral ligament, are tensed during external rotation15–18, and the semimembranosus acts on internal rotation19,20. However, it remains unclear in vivo whether the semimembranosus action during the rotational task, such as the isometric internal rotation, displace the MM, and it has not been quantified whether the MM and joint capsule coordinately move during the tibial rotation. Ultrasound can visualize all the structures, including the location of the MM21,22, and based on the recorded images, the time-series velocity of the visualized structures during an exercise task can be quantified by the particle image velocimetry (PIV) method23,24. Comparison of the time-series velocity of the visualized structures can evaluate whether the visualized structures move together or not24. Therefore, by simultaneously visualizing the MM, joint capsule, and semimembranosus during tibial rotation tasks, their movement interrelationships can be quantitatively analyzed in vivo using ultrasound.
This study aimed to investigate the in vivo interrelationships of velocity between the MM, joint capsule, and semimembranosus during passive tibial external-internal rotation and isometric tibial internal rotation using ultrasound. We hypothesized that isometric internal rotation with the semimembranosus action displaced the MM inward at the medial knee, and based on the time-series change of the velocity, all structures (MM, joint capsule, and semimembranosus) were coordinated with more than moderate cross-correlation coefficients during these tibial rotation tasks.
Materials and methods
Participants
Thirteen healthy volunteers (nine men and four women; mean age, 22.8 ± 5.8 years; height, 164.8 ± 8.1 cm; weight, 61.1 ± 11.2 kg) at the Morinomiya University of Medical Sciences were investigated. The study design was approved by the ethics committee of the Morinomiya University of Medical Sciences (#2022–095), and all procedures were performed in accordance with the Declaration of Helsinki (last modified in 2013) and Japanese guidelines entitled “Ethical Guidelines for Medical and Health Research Involving Human Subjects.” All the participants provided written informed consent.
Participants with no history of lower-extremity orthopedic conditions or surgery were included. One participant was unable to perform the following exercise task described below owing to the compensatory movements, and two were unable to obtain clear ultrasound images; therefore, the remaining 10 participants (seven men and three women; mean age, 23.4 ± 6.6 years; height, 165.0 ± 7.3 cm; weight, 62.8 ± 11.7 kg) were analyzed based on the ultrasound imaging assessment.
Ultrasound assessment
Ultrasound assessment of the knee was performed using two ultrasound scanners (Aplio 300 [Canon Medical Systems, Tokyo, Japan] with a 12-MHz linear transducer and SNiBLE [Konica Minolta, Tokyo, Japan] with an 18-MHz linear transducer). Two ultrasound images, a long-axis B-mode image of the medial knee (Fig. 1a) and one of the semimembranosus of the posteromedial knee (Fig. 1b), were recorded in synchronization using Obs Studio (Open Broadcaster Software, ver. 27.2.4). Thus, the movement of the MM, joint capsule, and semimembranosus was simultaneously visualized during the ultrasound assessment.
Figure 1.
Ultrasound assessments of the medial and posteromedial knees. (a) Long axis image of the medial knee. The location of the ultrasound transducer is indicated by the red doted box in the lower-left panel, which is a schematic illustration of the medial aspects of the right knee. The arrow indicates the perpendicular distance of the outermost margin of the medial meniscus (MM) from the line connecting the medial borders of the femur and tibia. (b) Long axis image of the semimembranosus (SM) at the posteromedial knee. The location of the ultrasound transducer is indicated by the red doted box in the lower-left panel. The arrow indicates the perpendicular distance of the outer margin of the joint capsule (Cap) from the line connecting the posteromedial borders of the femur and tibia on the line passing through the midpoint of the joint space. (c) and (d) Show assessments of the ultrasound images using flow particle image velocimetry, corresponding to (a) and (b), respectively. White boxed regions indicate the region of interest for the measurement. The colored bar represents the approximate velocity corresponding to the different colors of the arrow heads. dCap, distal joint capsule; pCap, proximal joint capsule; Sub, subcutaneous tissue; Dist, distal; Med, medial; post/med, posteromedial.
The assessment was performed in the supine position with the knee in 20° flexion and ankle in 0° plantar dorsiflexion during the following two exercise tasks: 1. passive movement of the tibial external-internal rotation (range, 15° external rotation—20° internal rotation; angular velocity, 10°/s); 2. Isometric tibial internal rotation (intensity, maximum strength without compensatory movements in other joints; duration, 4 s; rest, 4 s). The posture during both exercise tasks was fixed using an isokinetic dynamometer (Biodex System 4; Biodex Medical System Inc., Shirley, NY, USA). Using surface electromyography (Wave Plus Wireless EMG; Cometa System Inc., Milan, Italy), the absence of semimembranosus contraction was confirmed during passive movement of the tibial external-internal rotation and the presence of semimembranosus contraction during isometric tibial internal rotation. Ultrasound images during these exercise tasks for the five trials were recorded as movie images.
Imaging analysis
Based on the recorded images, the MM location at the medial knee and the joint capsule location at the posteromedial knee were analyzed using ImageJ software version 1.53 (National Institutes of Health, Bethesda, MD, USA). The location of the MM in the medial knee was defined as the perpendicular distance of the outermost margin of the MM from the line connecting the medial borders of the femur and the tibia (Fig. 1a)22. The location of the joint capsule at the posteromedial knee, which can be regarded as the MM location at the site, was defined as the perpendicular distance of the outer margin of the joint capsule from the line connecting the posteromedial borders of the femur and tibia to the line passing through the midpoint of the joint space (Fig. 1b). For the passive movement of the tibial external-internal rotation, the locations of the MM in the medial knee and joint capsule at the posteromedial knee were compared between the internal and external rotation positions, and for the isometric tibial internal rotation, measurements were compared between rest and during contraction. The average measurement of five trials was recorded for statistical analysis.
Furthermore, to analyze the interrelationships among the MM, joint capsule, and semimembranosus during the two exercise tasks, the recorded movies were analyzed by the PIV method using the application software Flow PIV (Library, Inc., Tokyo, Japan), in accordance with a previously verified method24. Flow PIV, which applies the pattern tracking algorithms using the gray level difference as a similarity index of correlation area and the successive abandonment method25, can isolate the relative pixel motion between successive frames of an ultrasound movie to visualize the flow direction and velocity and quantify them in the region of interest. For tracking each structure and recording its velocity, the regions of interest (24fps, 3-frame intervals) were set within the MM, proximal and distal joint capsule, subcutaneous (50 × 30 pixels for each, 0.17 mm/pixel) at the medial knee image (Fig. 1c) and semimembranosus (30 × 20 pixels for each, 0.11 mm/pixel) at the posteromedial knee images (Fig. 1d). All regions of interest were positioned to exclude other tissues during the movie recording. In particular, the proximal joint capsule was placed in such a position that part of the regions of interest was covered just above the medial epicondyle, the distal joint capsule was placed at its proximal end not exceeding the superior border of the tibia, and the semimembranosus was placed as distally as possible. The framewise mean of each flow velocity and its time series were recorded for the passive movement of the tibial external-internal rotation (Fig. 2a) and isometric tibial internal rotation (Fig. 2b). Based on the acquired velocity waveforms, waveform similarity was statistically analyzed as an interrelationship between each structure. In addition, to validate the analysis, their maximum velocity was also recorded, and we analyzed whether the subcutaneous tissue velocity was slower than that of the other structures in both tasks, and whether the semimembranosus velocity was faster than that of the other structures in the isometric tibial internal rotation. The measurement medians of the five trials were statistically analyzed.
Figure 2.
Representative waveforms of the velocity of the pericapsular structures. (a) Velocity waveform of each structure during the passive movement of the tibial external-internal rotation. The black waveform indicates the medial meniscus (MM) velocity. The blue one indicates the proximal joint capsule (pCap) velocity. The blue dotted one indicates the distal joint capsule (dCap) velocity. The black dotted line indicates the approximate timing of rotation direction switching. (b) Velocity waveform of each structure during the isometric tibial internal rotation. The green waveform indicates the semimembranosus (SM) velocity.
Statistical analyses
All statistical analyses were performed using the SPSS software (version 27.0; IBM Corp., Armonk, NY, USA). Using the paired t-test, both the MM location at the medial knee and joint capsule location at the posteromedial knee were statistically compared between the internal and external rotation positions in passive movement and between rest and contraction in isometric tibial internal rotation. Mean differences and 95% confidence intervals (CI) were calculated. The significance level of the comparisons was set at 0.05. In addition, intraclass correlation coefficients (ICCs) were calculated to determine the intra-rater reliability using measurement values from the five trials obtained during the analysis process23. The qualitative cut-offs for intraclass correlation coefficients values are reported as follows: poor, < 0.40; fair, 0.40–0.59; good, 0.60–0.74; and excellent, 0.75–1.026. All ICCs were ≥ 0.72 (range, 0.72–0.99), indicating good or excellent agreement (Table S1).
To analyze the waveform similarity of each structural velocity, we calculated the cross-correlation coefficient for the relationship between each structure during passive movement (MM-proximal joint capsule, MM-distal joint capsule, and MM-semimembranosus) and isometric tibial internal rotation (MM-proximal joint capsule, MM-distal joint capsule, MM-semimembranosus, semimembranosus-proximal joint capsule, and semimembranosus-distal joint capsule). Regarding the analysis of the maximum velocity, Tukey's honest significant difference (HSD) test was applied, and the significance level of the comparisons was set at 0.05. According to Tukey's HSD test, the maximum velocity of the subcutaneous tissue was significantly lower than that of the other structures in both tasks, and the maximum velocity of the semimembranosus was higher than that of the other structures in the isometric tibial internal rotation (Table S2), indicating the validity of the velocity measurement.
Results
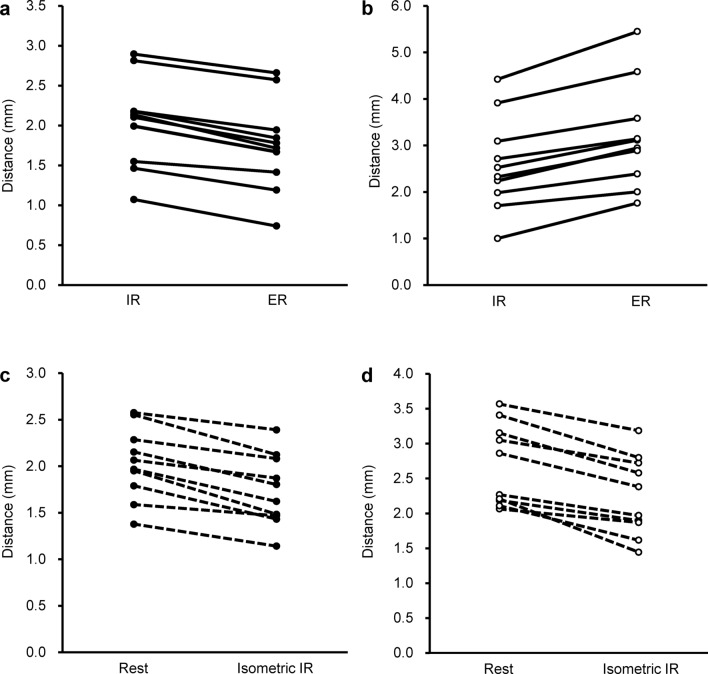
During passive tibial rotation from the internal to the external side, the distance of the outermost margin of the MM from the tibia at the medial knee was significantly smaller during external rotation (mean [standard deviation, SD], 1.8 [0.6] mm) than that during internal rotation (mean [SD], 2.0 [0.6] mm) (Fig. 3a, p < 0.001; mean difference, − 0.29; 95% CI − 0.34 to − 0.23). At the posteromedial knee, the distance of the outermost margin of the joint capsule from the tibia was significantly greater during external rotation (mean [SD], 3.2 [1.1] mm) than those during internal rotation (mean [SD], 2.6 [1.0] mm) (Fig. 3b, p < 0.001; mean difference, 0.59; 95% CI 0.44–0.74). During the isometric tibial internal rotation, the distance of the outermost margin of the MM from the tibia at the medial knee was significantly smaller during contraction (mean [SD], 1.7 [0.4] mm) than that at rest (mean [SD], 2.0 [0.4] mm) (Fig. 3c, p < 0.001; mean difference, − 0.29; 95% CI − 0.37 to − 0.21). At the posteromedial knee, the distance of the outermost margin of the joint capsule from the tibia was significantly smaller during contraction (mean [SD], 2.2 [0.6] mm) than that at rest (mean [SD], 2.7 [0.6] mm) (Fig. 3d, p < 0.001; mean difference, − 0.44; 95% CI − 0.57 to − 0.32).
Figure 3.
Changes of the distance of the medial meniscus and joint capsule from the tibia and femur according to the exercise tasks. (a) Comparison of the medial meniscus location during passive movement in tibial internal and external rotations (IR and ER, respectively) at the medial knee. (b) Comparison of the joint capsule location during passive movement in IR and ER at the posteromedial knee. (c) Comparison of the medial meniscus location in rest and isometric IR at the medial knee. (d) Comparison of the joint capsule location in rest and isometric IR at the posteromedial knee. The locations of the measurement distance of (a) and (c) are demonstrated by the arrow in Fig. 1(a); moreover, those of (b) and (d), are demonstrated by the arrow in Fig. 1(b). A paired t-test showed a p-value < 0.001 for all comparisons.
Regarding the waveform similarity of each structural velocity during passive tibial rotation, the cross-correlation coefficients between the MM and proximal/distal joint capsule were ≥ 0.54, although those between the MM and semimembranosus were < 0.3 or not correlated (passive IR-ER in Table 1). During isometric tibial internal rotation, the cross-correlation coefficients between the MM and proximal/distal joint capsules were ≥ 0.90, those between the MM and semimembranosus, and those between the semimembranosus and proximal/distal joint capsules were ≥ 0.62 (isometric IR in Table 1).
Table 1.
Cross-correlation coefficient among the pericapsular structures.
| Tasks | Structures | Cross-correlation coefficient | |
|---|---|---|---|
| Median | IQR | ||
| Passive IR-ER | MM-pCap | 0.54 | 0.42–0.67 |
| MM-dCap | 0.63 | 0.55–0.64 | |
| MM-SM | 0.23 | − 0.12–0.30 | |
| Isometric IR | MM-pCap | 0.92 | 0.90–0.96 |
| MM-dCap | 0.90 | 0.79–0.95 | |
| MM-SM | 0.64 | − 0.33–0.86 | |
| SM-pCap | 0.69 | 0.44–0.84 | |
| SM-dCap | 0.62 | − 0.41–0.70 | |
dCap distal joint capsule, ER external rotation, IQR interquartile range, IR internal rotation, MM medial meniscus, pCap proximal joint capsule, SM semimembranosus.
Discussion
The present study revealed that both passive external rotation (mean difference [internal rotation − external rotation], − 0.29 mm) and isometric internal rotation (mean difference [rest − contraction], − 0.29 mm) significantly decreased the distance of the MM from the tibia at the medial knee (both p values, < 0.001). In contrast, passive external rotation significantly increased the distance of the posteromedial joint capsule from the tibia (mean difference [internal rotation − external rotation], 0.59 mm), whereas isometric internal rotation decreased it (mean difference [rest − contraction], − 0.44 mm) (both p values, < 0.001). During passive tibial rotation, the MM and proximal/distal joint capsules moved in coordination with cross-correlation coefficients ≥ 0.54. During isometric tibial internal rotation, the MM and proximal/distal joint capsule were coordinated with cross-correlation coefficients ≥ 0.90, and the movements of the MM and proximal/distal joint capsule to the semimembranosus were also coordinated with cross-correlation coefficients ≥ 0.62.
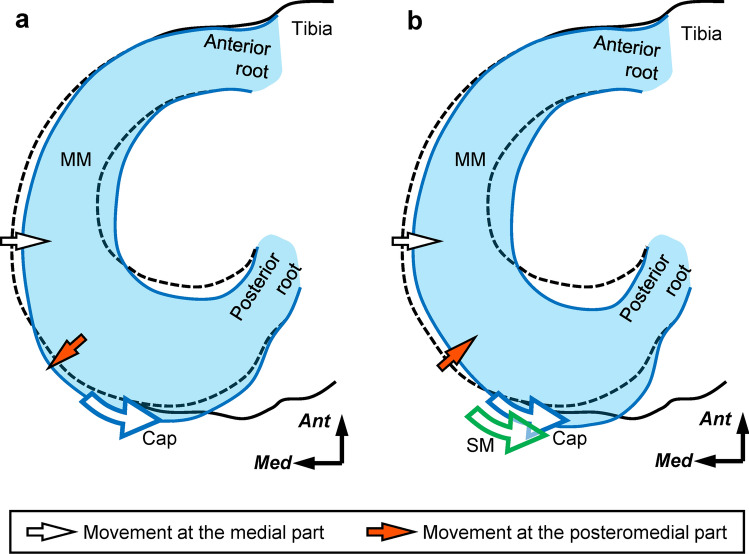
During tibial external rotation, the MM moves in the direction of internal rotation relative to the tibia, that is, in the posterolateral direction13,14. A recent study using magnetic resonance imaging quantified the MM movement in vivo27. The present study revealed that tibial external rotation decreased the distance of the MM from the tibia at the medial knee and increased the distance of the posteromedial joint capsule from the tibia. The inward meniscus movement at the medial knee results in decreasing the distance of the MM from the tibia (Fig. 4a, white arrow). The outward joint capsule movement at the posteromedial knee results in increasing the distance of the posteromedial joint capsule from the tibia. If the joint capsule movement at the posteromedial knee can be regarded as that of the MM (Fig. 4a, red arrow), our demonstration of inward meniscus movement at the medial knee and outward joint capsule movement at the posteromedial knee during passive tibial external rotation are similar to MM movement in the direction of internal rotation relative to the tibia reported in previous studies13,14,27 (Fig. 4a).
Figure 4.
Schematic diagram of the medial meniscus movements by the passive external and isometric internal rotations. Superior aspect of the tibia. Passive tibial external rotation (a) and isometric tibial internal rotation (b) can displace the medial meniscus (MM) inward at the medial knee (indicated by the white arrows) owing to the internal rotation movement of the MM relative to the tibia. These MM movements were considered to be caused by joint capsule (Cap) tension (indicated by the blue curved arrow). The displacement direction difference of the posteromedial joint capsule between (a) and (b) (indicated by red arrows) may result from the semimembranosus (SM) action (indicated by the green curved arrow) transmitted through the cap during isometric tibial internal rotation. Ant, anterior; Med, medial.
On the other hand, the present study also demonstrated that isometric internal rotation decreased the distance of the MM from the tibia at the medial knee and the distance of the posteromedial joint capsule from the tibia. The inward meniscus movement at the medial knee and the joint capsule movement at the posteromedial knee result in the decrease of their distances from the tibia at both locations (Fig. 4b, white and red arrows). Thus, the isometric internal rotation with semimembranosus action can displace not only the posteromedial joint capsule inward, but also the MM at the medial knee. Based on the MM movement pattern during tibial external rotation13,14,27, the inward meniscus movement at the medial knee during isometric internal rotation may be due to movement in the direction of internal rotation relative to the tibia (Fig. 4b).
Regarding the waveform similarity of each structural velocity, Kawanishi et al.24 suggested that a high correlation coefficient (approximately 0.7) among structural velocities represents simultaneous movement, and a low correlation coefficient (approximately 0.4) represents independent movement, in other musculoskeletal regions. Because, during passive tibial rotation, the MM and proximal/distal joint capsules moved in coordination with cross-correlation coefficients ≥ 0.54, the presence of these interrelationships was quantitatively verified in vivo by the moderate cross-correlation coefficients between the velocity of the MM and joint capsule. Conventional knee ligaments, which represent the joint capsule itself12, are tensed during external rotation15–18; therefore, the interrelationships between the MM and proximal/distal joint capsules during passive external rotation may be interpreted as due to MM movement caused by tension in the joint capsule (Fig. 4a, blue curved arrow).
Additionally, because, during isometric tibial internal rotation, the movements of the MM and proximal/distal joint capsule to the semimembranosus were coordinated with cross-correlation coefficients ≥ 0.62, the presence of the interrelationship among the MM, joint capsule, and semimembranosus was verified by the moderate cross-correlation coefficients among their velocities. Therefore, these in vivo quantitative findings support the anatomical hypothesis that the joint capsule dynamically coordinates the MM by transmitting semimembranosus action through tendinous sheaths (Fig. 4b, green and blue curved arrows)12. The displacement direction difference of the posteromedial joint capsule during passive external rotation and isometric internal rotation may have resulted from the semimembranosus action, because the difference in the tension applied between the passive tibial external and isometric tibial internal rotations may be attributed to the contraction of the semimembranosus.
In terms of clinical relevance, our findings indicate that, in healthy individuals, a sufficient tension change in the joint capsule by passive tibial external rotation and/or semimembranosus action can displace the MM inward at the medial knee. Recently, based on a retrospective study, Yoshizuka et al.28 hypothesized that stretching the semimembranosus and passive knee range of motion exercises may reduce the extent of MM extrusion in patients with knee osteoarthritis. Our findings support this conclusion. To maintain and/or improve the proper MM position within the knee, it may be critical to have sufficient knee range of motion (e.g., tibial external rotation) and semimembranosus flexibility to transmit sufficient tension to the joint capsule. Future studies should determine whether MM extrusion is caused by increased tibial internal rotation or semimembranosus shortening.
Our study had several limitations. First, we could not verify whether our findings are applicable to the elderly or individuals with knee osteoarthritis and whether they are applicable in weight-bearing conditions, and our theory provides speculative clinical implications. Second, the sample size was relatively small. However, a post-hoc power analysis using G*Power software version 3.1.9.6 based on the MM location at the medial knee and joint capsule location at the posteromedial knee showed that the power was > 0.99. Therefore, a larger sample size may not have been necessary. Future studies on individuals with knee osteoarthritis and other conditions is needed, using the data from the present study as preliminary findings. Third, the tension itself, which would be generated in the joint capsule and semimembranosus, was not visualized by the shear wave elastography or other relevant tests. Fourth, we did not perform a three-dimensional analysis; thus, the entire MM movement could not be visualized. Finally, the extent of the semimembranosus action was not fully unified; however, we believe that it had no considerable impact on verifying the presence of interrelationships.
In conclusion, isometric tibial internal rotation with semimembranosus action can displace the MM inward at the medial knee, possibly because of meniscal internal rotation relative to the tibia as well as passive tibial external rotation. During meniscus movement, the MM and joint capsule coordinately moved with more than moderate cross-correlation coefficients, and during isometric tibial internal rotation, both the MM and joint capsule moved in coordination with moderate cross-correlation coefficients relative to the semimembranosus. Accordingly, the joint capsule may dynamically coordinate the MM by transmitting semimembranosus action.
Supplementary Information
Acknowledgements
The authors thank Keisuke Hirakawa, MSc, for his assistance with data collection. This study was supported by the Morinomiya University President’s Research Encouragement Award (Grant Number 2023MPA1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors also thank Editage (www.editage.com) for English language editing.
Author contributions
All the authors contributed to the conception and design of this study. S.K. and S.K. collected the data, and M.T. and S. K. analyzed the data. M.T. wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. All the authors have read and approved the final version of the manuscript.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-024-68088-1.
References
- 1.Englund, M., Roemer, F. W., Hayashi, D., Crema, M. D. & Guermazi, A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat. Rev. Rheumatol.8, 412–419 (2012). 10.1038/nrrheum.2012.69 [DOI] [PubMed] [Google Scholar]
- 2.Adams, J. G., McAlindon, T., Dimasi, M., Carey, J. & Eustace, S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin. Radiol.54, 502–506 (1999). 10.1016/S0009-9260(99)90846-2 [DOI] [PubMed] [Google Scholar]
- 3.Badlani, J. T., Borrero, C., Golla, S., Harner, C. D. & Irrgang, J. J. The effects of meniscus injury on the development of knee osteoarthritis: Data from the osteoarthritis initiative. Am. J. Sports Med.41, 1238–1244 (2013). 10.1177/0363546513490276 [DOI] [PubMed] [Google Scholar]
- 4.Gale, D. R. et al. Meniscal subluxation: Association with osteoarthritis and joint space narrowing. Osteoarthr. Cartil.7, 526–532 (1999). 10.1053/joca.1999.0256 [DOI] [PubMed] [Google Scholar]
- 5.Swamy, N., Wadhwa, V., Bajaj, G., Chhabra, A. & Pandey, T. Medial meniscal extrusion: Detection, evaluation and clinical implications. Eur. J. Radiol.102, 115–124 (2018). 10.1016/j.ejrad.2018.03.007 [DOI] [PubMed] [Google Scholar]
- 6.Cavaignac, E. et al. What is the relationship between the distal semimembranosus tendon and the medial meniscus? A gross and microscopic analysis from the SANTI study group. Am. J. Sports Med.49, 459–466 (2021). 10.1177/0363546520980076 [DOI] [PubMed] [Google Scholar]
- 7.Dephillipo, N. N. et al. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: Defining meniscal ramp lesions. Am. J. Sports Med.47, 372–378 (2019). 10.1177/0363546518814258 [DOI] [PubMed] [Google Scholar]
- 8.Laprade, R. F. et al. The anatomy of the medial part of the knee. J. Bone Joint Surg. Am.89, 2000–2010 (2007). 10.2106/00004623-200709000-00016 [DOI] [PubMed] [Google Scholar]
- 9.Mameri, E. S. et al. Review of meniscus anatomy and biomechanics. Curr. Rev. Musculoskelet. Med.15, 323–335 (2022). 10.1007/s12178-022-09768-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Śmigielski, R., Becker, R., Zdanowicz, U. & Ciszek, B. Medial meniscus anatomy-from basic science to treatment. Knee Surg. Sports Traumatol. Arthrosc.23, 8–14 (2015). 10.1007/s00167-014-3476-5 [DOI] [PubMed] [Google Scholar]
- 11.Warren, L. F. & Marshall, J. L. The supporting structures and layers on the medial side of the knee: An anatomical analysis. J. Bone Joint Surg. Am.61, 56–62 (1979). 10.2106/00004623-197961010-00011 [DOI] [PubMed] [Google Scholar]
- 12.Tsutsumi, M., Nimura, A., Tharnmanularp, S., Kudo, S. & Akita, K. Posteromedial capsular anatomy of the tibia for consideration of the medial meniscal support structure using a multidimensional analysis. Sci. Rep.13, 12030 (2023). 10.1038/s41598-023-38994-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Braus, H. & Elze, C. Bewegungsapparat in Anatomie des Menschen ein Lehrbuch für Studierende und Ärzte 3rd edn. (Springer-Verlag, Berlin, 1954). [Google Scholar]
- 14.Kapandji, I. A. The Physiology of the Joints 7th edn. (Handspring Publishing Ltd., East Lothian, UK, 2019). [Google Scholar]
- 15.Griffith, C. J. et al. Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. Am. J. Sports Med.37, 1762–1770 (2009). 10.1177/0363546509333852 [DOI] [PubMed] [Google Scholar]
- 16.Laprade, R. F. & Wijdicks, C. A. The management of injuries to the medial side of the knee. J. Orthop. Sports Phys. Ther.42, 221–233 (2012). 10.2519/jospt.2012.3624 [DOI] [PubMed] [Google Scholar]
- 17.Robinson, J. R., Bull, A. M., Thomas, R. R. & Amis, A. A. The role of the medial collateral ligament and posteromedial capsule in controlling knee laxity. Am. J. Sports Med.34, 1815–1823 (2006). 10.1177/0363546506289433 [DOI] [PubMed] [Google Scholar]
- 18.Wijdicks, C. A. et al. Medial knee injury: Part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am. J. Sports Med.37, 1771–1776 (2009). 10.1177/0363546509335191 [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto, T. et al. Semimembranosus release reduces tibial internal rotation and flexion angle in cruciate-retaining total knee arthroplasty. J. Arthroplasty30, 1537–1541 (2015). 10.1016/j.arth.2015.03.039 [DOI] [PubMed] [Google Scholar]
- 20.Spinner, R. J., Krych, A. J. & Bernard, C. D. Knee and leg. In Gray’s Anatomy: The Anatomical Basis of Clinical Practice 42nd edn (ed. Standring, S.) 1395–1429 (Elsevier Health Sciences, New York, 2021). [Google Scholar]
- 21.Farivar, D. et al. Medial meniscal extrusion of greater than 3 millimeters on ultrasound suggests combined medial meniscotibial ligament and posterior medial meniscal root tears: A cadaveric analysis. Arthroscopy39, 1815-1826.e1 (2023). 10.1016/j.arthro.2023.01.104 [DOI] [PubMed] [Google Scholar]
- 22.Özdemir, M. & Turan, A. Correlation between medial meniscal extrusion determined by dynamic ultrasound and magnetic resonance imaging findings of medial-type knee osteoarthritis in patients with knee pain. J. Ultrasound Med.38, 2709–2719 (2019). 10.1002/jum.14976 [DOI] [PubMed] [Google Scholar]
- 23.Anegawa, K. et al. Tibial nerve dynamics during ankle dorsiflexion: The relationship between stiffness and excursion of the tibial nerve. J. Biomech.155, 111646 (2023). 10.1016/j.jbiomech.2023.111646 [DOI] [PubMed] [Google Scholar]
- 24.Kawanishi, K., Kudo, S. & Yokoi, K. Relationship between gliding and lateral femoral pain in patients with trochanteric fracture. Arch. Phys. Med. Rehabil.101, 457–463 (2020). 10.1016/j.apmr.2019.09.011 [DOI] [PubMed] [Google Scholar]
- 25.Kaga, A., Inoue, Y. & Yamaguchi, K. Pattern tracking algorithms using successive abandonment. J. Flow Vis. Image Process.1, 283–296 (1993). 10.1615/JFlowVisImageProc.v1.i4.30 [DOI] [Google Scholar]
- 26.Cicchetti, D. V. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess.6, 284–290 (1994). 10.1037/1040-3590.6.4.284 [DOI] [Google Scholar]
- 27.Fuchs, A. et al. In-vivo assessment of meniscal movement in the knee joint during internal and external rotation under load. J. Exp. Orthop.9, 102 (2022). 10.1186/s40634-022-00540-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoshizuka, H., Taniguchi, T., Fukuta, K., Mitsutake, T. & Honda, S. Decrease in medial meniscal extrusion after physical therapy to improve knee pain and range of motion in patients with knee osteoarthritis: A retrospective study. PLOS ONE17, e0277628 (2022). 10.1371/journal.pone.0277628 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.