Abstract
Antiretroviral therapy (ART) has extended the lifespan of people living with HIV/AIDS (PLHIV), exposing them to a higher risk of cardiovascular diseases (CVD). Hypertension (HTN), the primary contributor to CVD burden, is increasingly concerning for PLHIV. This study aimed to assess the prevalence and associated factors of hypertension in PLHIV on ART at the National Teaching Hospital Hubert Koutoukou Maga (HKM) of Benin using a prospective cross-sectional study conducted between October and December 2021. Patients who had a systolic blood pressure ≥ 140 mmHg or/and diastolic blood pressure ≥ 90 mmHg or/and current use of antihypertensive medication from medical records were considered to have HTN. A total of 352 patients, including 260 women with a sex ratio of 0.3 were included. The mean age was 42.9 ± 11.9 years. Most patients were educated and did not use tobacco. 42.0% were current alcohol drinkers. The duration of ART treatment ranged from 0 to 22 years, with a median duration of 5.0 years. 14.2% were hypertensives with 3.1% newly diagnosed and 11.1% known with hypertension. Age above 40 years, living with a partner, alcohol consumption and body mass index greater than 25 were significantly associated with HTN. HTN in PLHIV is associated with numerous factors. Reducing the burden of the disease in target people in Benin requires a wide range of actions that need to be implemented.
Keywords: Prevalence, Hypertension, People living with HIV, Benin
Subject terms: Cardiology, Medical research, Risk factors
Introduction
Currently, one of the predominant global health challenges lies in the escalating burden of HIV/AIDS, with a cumulative toll of 40.1 million lives worldwide. In 2021 alone, HIV-related causes led to 650,000 deaths globally, while 1.5 million individuals contracted the disease globally. Statistics provided by the World Health Organization (WHO) reveal that by the conclusion of 2021, approximately 38.4 million individuals were living with HIV, with the WHO African region harboring two-thirds of this population, estimated at 25.6 million1. In Benin, despite a declining trend in HIV incidence from 2.2 in 1995 to 0.2 in 2021, approximately 1.2% of adults were HIV positive, translating to an estimated 69,000 People Living with HIV (PLHIV) in the country as per ONUSIDA2,3. In the past decade, notable advancements have been made in the management of HIV/AIDS due to the proliferation of various antiretroviral therapies (ART). In 2014, the Joint United Nations Program on HIV/AIDS (UNAIDS) introduced the 90–90-90 targets, aimed at achieving 90% awareness of HIV status among all individuals, ensuring that 90% of diagnosed HIV cases receive continuous ART, and attaining viral suppression in 90% of those receiving ART4. These initiatives have led to a decline in HIV/AIDS-related mortality rates. For instance, in Benin, the proportion of PLHIV receiving ART surged from 41 to 84% between 2014 and 2021, as reported by The National Health Program against HIV/AIDS. Conversely, the annual count of HIV/AIDS-related deaths has decreased from 2400 to 1600 during the same period3,5.
Additionally, cardiovascular diseases (CVD) represent a prominent global health concern and stand as the foremost cause of mortality worldwide6,7. Hypertension (HTN), described as an elevated and persistent level of blood pressure, is the main risk factor for CVD and contributes significantly to mortality due to its numerous complications6,8. Despite the heavy burden of infectious diseases on the African continent, there are also trends of higher prevalence of HTN and CVD9. In Benin, findings from the 2015 STEPS survey unveiled a concerning statistic: one in every four adults suffered from HTN. This health issue permeates every segment of the population, and PLHIV are no exception. The coexistence of HIV/AIDS and HTN is intricately linked with the increasing life expectancy of PLHIV, who are consequently exposed to a myriad of risk factors including both traditional risk factors and virologic and treatment-related factors. These factors encompass chronic inflammation, immune reconstitution, and lipodystrophy10–12. Numerous studies have underscored the notably high prevalence of HTN among PLHIV13,14. Despite this, in Benin, there remains a paucity of research that delves into the factors associated with HTN among PLHIV15. Therefore, the primary objective of this study is to evaluate the prevalence of HTN and identify factors that may influence its occurrence among PLHIV receiving care at the National Teaching Hospital Hubert Koutoukou Maga (HKM).
Materials and method
The present study comprised an institutional-based cross-sectional investigation carried out at the Benin’s National Teaching Hospital HKM during the period spanning October to December 2021. As the largest medical facility in Benin, the National Teaching Hospital HKM plays a pivotal role in healthcare provision within the country. Notably, PLHIV receive ongoing care and monitoring at the hospital’s outpatient clinic, which serves as a critical hub for managing their medical needs. Overseeing a significant caseload, the outpatient clinic routinely attends to approximately 1000 patients, underscoring its substantial impact on HIV healthcare delivery in the region.
Study population
PLHIV who were on follow-up in the hospital’s outpatient clinic, receiving ART and were available during the data collection period.
Inclusion and exclusion criteria
We included patients whose age was ≥ 18 years old. Pregnant women living with HIV and individuals living with HIV (PLHIV) who were unable to provide accurate responses due to cognitive impairment were excluded.
Sample size and sampling techniques
All PLHIV on follow-up in the outpatient clinic during the data collection period were included.
Study variables
The dependent variable was HTN and independent variables were sociodemographic characteristics (age, sex, education, marital status), lifestyle related factors (alcohol drinking, smoking, physical activity), body measurement factors (height, body mass index) and HIV related factors (ART duration, HIV type, class of ART).
Operational definition
Hypertension was defined according to the European Society of Hypertension (ESH) guidelines as a systolic blood pressure ≥ 140 mmHg and/or a diastolic blood pressure ≥ 90 mmHg16,or/and the current use of antihypertensive medication as documented in medical records. Living with a partner, alcohol consumption, and smoking status were all based on patient declarations. Body mass index (BMI) was used to classify physical status as follows: underweight for BMI ≤ 18.5 kg/m2, normal for BMI between 18.5 and 24.9 kg/m2, overweight for BMI between 25.0 and 29.9 kg/m2, and obesity for BMI > 30 kg/m2. ART duration was defined as the time since the first prescription of antiretroviral therapy (ART) based on patient records. The classes of ART included Nucleoside Reverse Transcriptase Inhibitors (NRTI), Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTI), Protease Inhibitors (PI), and Integrase Strand Transfer Inhibitors (INSTI).
Data collection
Data were systematically collected between October and December 2021. The latest French version of the WHO STEPS questionnaire, tailored to the context of Benin, served as the primary instrument for data collection. This questionnaire provided comprehensive insights into various dimensions including socio-demographic profiles, behavioral patterns, clinical risk factors, and the medical history of non-communicable diseases (NCDs). These data were sourced from multiple channels, including patient self-reports, medical records, and physical measurements. Upon arrival at the clinic, patients were thoroughly briefed on the study objectives and procedural steps, following which their informed consent was solicited prior to any data acquisition activities. The data collection process was executed by rigorously trained medical personnel, who adhered to standardized protocols. Blood pressure (BP) measurements were conducted on participants in a rested, seated position for a minimum of five (5) minutes using electronic blood pressure monitors (OMRON Model: HEM-CACO-734). Subsequent to a series of three (3) measurements taken at three-minute intervals, the average of the last two readings was computed to determine the participant’s blood pressure status and facilitate result analysis. Additionally, weight measurements were obtained using mechanical scales, with participants standing symmetrically on the scale until stabilization of the reading. Data collection procedures were conducted in a controlled manner, with interviewers facing respondents to ensure accuracy and reliability of measurements.
Data quality control and collection procedure
The data collection process involved administering a questionnaire to the patient through face-to-face interviews, followed by taking physical measurements. Data were collected using Open Data Kit software (ODK) on smartphones and real-time monitoring of the data were carried out to ensure completeness and validity of the collected data. The collected data was then consolidated, edited and checked for internal consistency.
Statistical analysis
Data analysis was conducted utilizing R version 4.0.1 software, with statistical tests executed at a significance level of α = 5%. Descriptive statistics were computed for the variables under investigation. Quantitative descriptive variables were expressed as mean ± standard deviation for normally distributed data, and as median and interquartile range for non-normally distributed data, while qualitative variables were presented as frequencies and percentages. For univariable analysis, comparisons of proportions between two groups were made employing the uncorrected Pearson Chi-square test and the Fisher exact test (utilized when theoretical numbers were less than 5). Subsequently, multivariable stepwise descending logistic regression was performed. Adjusted odds ratios with corresponding 95% confidence intervals were calculated to quantify the strength of associations. All variables exhibiting an association less than or equal to 0.2 were included in the model, with stepwise downward regression executed thereafter. The Hosmer–Lemeshow test was conducted to assess the goodness of fit of the model to the data.
Ethics approval and consent to participate
Doctoral school of Health sciences of University of Abomey-Calavi approved the research protocol. Permission to conduct the study was obtained from the National Teaching Hospital HKM of Benin. Written informed consent was obtained from all the subjects before the study. The study was also conducted following the Helsinki Declaration of research involving human subjects (https://www.who.int/bulletin/79(4)373.pdf).
Results
Sociodemographic, lifestyle and clinical characteristics of respondents
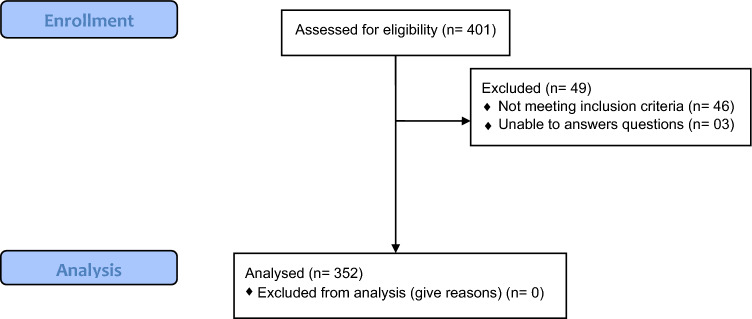
We have enrolled 352 subjects in our study, with a notable predominance of females, comprising 260 individuals, yielding a sex ratio (M/F) of 0.3 (Fig. 1). Among these participants, 21.3% reported no formal education. The mean age of the cohort was determined to be 42.9 ± 11.9 years, with the age range spanning from 18 to 76 years. These findings indicate a diverse sample population with a significant representation of females and a wide age range. The proportion of participants reporting no formal education underscores potential disparities in educational attainment within the study population. Moreover, the calculated mean age provides insight into the demographic characteristics of the cohort, highlighting the middle-aged profile of the study participants (Table 1).
Figure 1.
Consort diagram of included patients in our study, National Teaching Hospital of Benin, 2021.
Table 1.
General characteristics of PLHIV on ART in National Teaching Hospital of Benin, 2021.
| n | % | |
|---|---|---|
| Sex | ||
| Male | 92 | 26.1 |
| Female | 260 | 73.9 |
| Level of school education | ||
| None | 75 | 21.3 |
| Primary school | 101 | 28.7 |
| Secondary | 143 | 40.6 |
| University | 33 | 9.4 |
| Living with a partner | ||
| No | 157 | 54.6 |
| Yes | 195 | 55.4 |
| Tobacco intake | ||
| Never smoked | 339 | 96.3 |
| Former smoker | 8 | 2.3 |
| Current smoker | 5 | 1.4 |
| Alcohol intake | ||
| Never drank | 170 | 48.3 |
| Former drinker | 34 | 9.7 |
| Current drinker | 148 | 42.0 |
| Regular physical activity | ||
| No | 98 | 27.8 |
| Yes | 254 | 72.8 |
| ART treatment | ||
| NRTI | 352 | 100.0 |
| NNRTI | 158 | 44.9 |
| PI | 6 | 1.7 |
| INSTI | 184 | 52.3 |
| Treatment length | ||
| Less than 5 years | 187 | 53.1 |
| Between 5 and 10 years | 86 | 24.4 |
| Between 10 and 15 years | 45 | 12.9 |
| More than 15 years | 34 | 9.7 |
Additionally, the findings of our study reveal a notable prevalence of health-conscious behaviors among the participants. Specifically, a substantial proportion, comprising 96.0% of the patient cohort, reported never having used tobacco, while approximately half (48.3%) disclosed a history of abstaining from alcohol consumption. Moreover, a mere 0.3% acknowledged indulging in excessive salt intake, while a modest 2.3% claimed regular consumption of fruits and vegetables. Additionally, an encouraging trend was observed regarding physical activity, with nearly three-quarters of the subjects reporting adherence to regular exercise routines.
Furthermore, all individuals enrolled in our study were confirmed to be HIV positive and were receiving non-nucleoside reverse transcriptase inhibitor (NNRTI)-class antiretroviral therapy (ART). The results indicated that 10.5% of participants met the criteria for clinical failure, while 6.0% were classified as experiencing immunological failure. Furthermore, approximately 43.5% of the study cohort exhibited a normal body mass index (BMI), whereas only 3.1% were classified as overweight. These findings suggest a concerning proportion of participants with abnormal Body Mass Index.
Prevalence of hypertension
Table 2 describe the distribution of hypertension prevalence among HIV patients on ART in our study sample. Among these patients, 14.2% had hypertension. The frequency of those who were known to be hypertensive was 11.1% and 3.1% were screened during the study. Amongst those who had a history of HTN, 93.7% had a normal blood pressure on the day of measurement.
Table 2.
Distribution of HTN in PLHIV in National Teaching Hospital of Benin, 2021.
| n | % | |
|---|---|---|
| Overall hypertension | ||
| No | 302 | 85.8 |
| Yes | 50 | 14.2 |
| Known hypertension | ||
| No | 313 | 88.9 |
| Yes | 39 | 11.1 |
| Newly diagnosed hypertension | ||
| No | 341 | 96.9 |
| Yes | 11 | 3.1 |
Factors associated with hypertension among PLHIV on ART
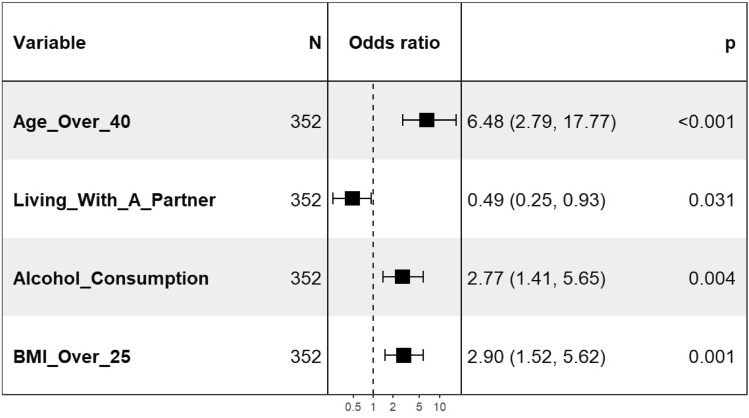
The univariable analysis identified age as the sole sociodemographic factor significantly associated with hypertension, with older individuals exhibiting a higher risk. Notably, alcohol consumption (p = 0.0082), and the duration of ART (p = 0.0088) also showed significant associations with hypertension, while no significant association was observed between the type of treatment and hypertension. Moreover, higher BMI was significantly associated with hypertension (p = 0.0001). Subsequent multivariable analysis, conducted through stepwise descending logistic regression, revealed that age (p < 0.0001), marital status (p = 0.0313), alcohol consumption (p = 0.0037), and body mass index (p = 0.0012) were the variables demonstrating association with hypertension (Table 3). Regarding the direction of association, individuals aged over 40 (aOR: 6.5; 95% CI: 2.8–17.8), those who consumed alcohol (aOR: 2.8; CI: 1.4–5.6), and those with a BMI over 25 (aOR: 2.9; CI = 2.9; 1.5—5.6) exhibited an increased risk of hypertension. Conversely, individuals living with a partner (aOR: 0.5; CI: 0.2–0.9) demonstrated a reduced risk of developing hypertension (Fig. 2).
Table 3.
Analysis of factors associated with HTN in PLHIV in National Teaching Hospital of Benin, 2021.
| Variables | HTN | Odds ratio (OR) | ||||
|---|---|---|---|---|---|---|
| Yes | No | Unadjusted OR (95% CI) |
p-value | Adjusted OR (95% CI) | p-value | |
| Age | < 0.001 | < 0.001 | ||||
| Less than 40 years | 6 | 135 | Reference | Reference | ||
| 40 years and over | 44 | 167 | 5.9 (2.5–14.3) | 6.5 (2.8–17.8) | ||
| Sex | 0.844 | |||||
| Male | 12 | 80 | Reference | |||
| Female | 38 | 222 | 1.1 (0.6–2.3) | |||
| Level of education | 0.848 | |||||
| None | 10 | 65 | Reference | |||
| Primary school | 22 | 79 | 1.8 (0.8–4.1) | 0.215 | ||
| Secondary | 15 | 128 | 0.8 (0.3–1.8) | 0.688 | ||
| University | 3 | 30 | 0.7 (0.2–2.5) | 0.750 | ||
| Living with partner | 0.110 | 0.031 | ||||
| No | 28 | 129 | Reference | Reference | ||
| Yes | 22 | 173 | 0.5 (0.3–1.1) | 0.5 (0.3–0.9) | ||
| Tobacco intake | 0.702 | |||||
| No | 49 | 290 | Reference | |||
| Yes | 1 | 12 | 0.5 (0.1–3.5) | |||
| Alcohol drinking | 0.008 | 0.004 | ||||
| No | 15 | 155 | Reference | Reference | ||
| Yes | 35 | 147 | 2.5 (1.3–4.7) | 2.8 (1.4–5.6) | ||
| Physical activity | 1.000 | |||||
| No | 14 | 84 | Reference | |||
| Yes | 36 | 218 | 1.0 (0.5–1.9) | |||
| ART treatment | ||||||
| NNRTI | 0.551 | |||||
| No | 30 | 164 | Reference | |||
| Yes | 20 | 138 | 1.3 (0.7–2.3) | |||
| INSTI | 0.182 | |||||
| No | 19 | 149 | Reference | |||
| Yes | 31 | 153 | 1.5 (0.9–2.9) | |||
| Treatment duration | 0.009 | |||||
| Less than 5 years | 23 | 164 | Reference | |||
| 5 to 9 years | 7 | 79 | 0.6 (0.3–1.5) | 0.417 | ||
| 10 to 14 years | 13 | 32 | 2.9 (1.3–6.3) | 0.011 | ||
| Over 15 years | 7 | 27 | 1.8 (0.7–4.7) | 0.273 | ||
| BMI | < 0.001 | 0.001 | ||||
| BMI < 25 | 20 | 207 | Reference | Reference | ||
| BMI ≥ 25 | 30 | 95 | 3.2 (1.8–6.0) | 2.9 (1.5–5.6) | ||
Figure 2.
Factors associated with HTN in PLHIV in National Teaching Hospital of Benin, 2021.
Discussion
The objective of this investigation was to ascertain the determinants linked to hypertension among PLHIV receiving ART at the National Teaching Hospital HKM of Benin. The observed prevalence of hypertension in this cohort stood at 14.2%, comprising 11.1% with a documented history of hypertension and 3.1% newly diagnosed cases. The average age of participants was 42.9 ± 11.9 years, with a majority being females (73.9%). A significant proportion reported never smoking, while approximately half disclosed no prior alcohol consumption. Key factors associated with hypertension included advancing age, marital status, alcohol intake, and body mass index (BMI). These findings reveal the multifactorial nature of hypertension in PLHIV on ART and emphasize the importance of targeted interventions addressing modifiable risk factors such as lifestyle habits and obesity.
The prevalence of hypertension in our study population appears comparatively low, ranging from 24.7% in Rwanda to 43.9% in Denmark, as reported in previous studies13,15,17–21. This lower prevalence could be attributed to the relatively younger age of our cohort compared to those in other studies, as age is a well-established risk factor for hypertension, with individuals over 40 years exhibiting a higher risk. This finding aligns with similar observations in the literature15,19,21.
Moreover, our study revealed a notable female predominance, with women comprising 73.9% of the population, a trend also observed in studies from Nigeria, South Africa, and Kenya19,22–24. This prevalence among women in Africa may stem from increased HIV screening during maternity care. While our study did not find a significant gender disparity in hypertension prevalence, some literature suggests a higher prevalence among men living with HIV compared to women, possibly attributed to hormonal differences25,26.
About half of our study participants lived with a partner and there is an association between living with a partner and Hypertension. Same proportions have been noted in other studies15,24,27. People living with a partner had fewer risk of HTN. An explanation to this report can be the fact that day to day support from a partner can play a role in reducing the stress that can have an effect on the onset of HTN. Almost half of the patients declared that they did not consume alcohol. Alcohol consumption was another factor associated with hypertension. A similar association has been found in several studies19,28. These different data confirm the often-described role of alcohol consumption as a risk factor for hypertension21. Even though our study doesn’t suggest an association between smoking and HTN, data from the literature suggest that smoking is a risk factor of HIV21. Actually, the very little proportion of our study participants who reported tobacco intake is not sufficient for good analysis.
In our study the majority of the patients maintained a normal BMI, with only a small percentage classified as overweight or obese. This low prevalence of overweight or obese aligns with findings reported in the literature. For instance, research conducted by Ogunmola in Nigeria and Van Heerden in Denmark supports these observations, suggesting a similar trend in BMI distribution within different populations22,23. Conversely, research conducted in Cameroon and South Africa, has identified a higher prevalence of overweight and obesity among PLHIV. In our population, overweight or obese participants had an increased risk of developing high blood pressure. Similar observations have been found in Africa, particularly in Nigeria and Cameroon, but also in the United States. The persistent association between obesity and high blood pressure is thought to be linked to the effects of visceral fat on the heart and blood vessels. Several other studies on the population of PLHIV on ART made similar findings15,19,26,29.
The findings of this study carry significant implications. A regular blood pressure monitoring, psychological support and increase attention to the risk factors of the disease are crucial in reducing the incidence of HTN in PLHIV. Effective management of PLHIV require a multidisciplinary approach and underscores the need to develop a new health workforce capable of providing integrated HIV and NCD care. Furthermore, the implementation of innovative and effective models for integrated NCD and HIV care, including task-sharing strategies and telemedicine, can address the shortage of qualified human resources, thereby improving life expectancy of PLHIV and preventing HTN related complications in this peculiar population.
Our study, however, has several limitations. Due to a lack of funding, we were unable to investigate biologic factors associated with HTN. Moreover, the cross-sectional study performed doesn’t allow for understanding of the chronological relationship between HTN and its associated factors. Nevertheless, the data were collected using an adapted version of the WHO STEPS questionnaire, making our findings comparable to those of other studies on NCD risk factors. In addition, the multivariable analysis enable the identification of factors associated with hypertension by adjusting for potential confounding variables.
Conclusion and recommendations
HTN in PLHIV is influenced by various factors, including age, alcohol consumption, cohabitation status, and body mass index (BMI). The presence of both conditions necessitates the integration of non-communicable disease (NCD) care into HIV/AIDS management. Regular blood pressure monitoring and proactive measures to prevent NCDs among PLHIV are crucial steps in reducing mortality rates and enhancing life expectancy within this specific population.
Data availabilty
The data supporting the finding will be attached to the editorial office with a reasonable request at any time.
Acknowledgements
The authors acknowledge all data collectors and respondents. They also extend their thanks to the National Teaching Hospital HKM administrators for permitting to conduct this research.
Author contributions
Conceptualization was led by B.M.A., C.O.A., and C.Y.H. Field data collection was conducted by C.O.A., S.A.S., and J.A. Database design and management were overseen by E.Y. Data curation responsibilities were shared among B.M.A., C.O.A., and E.Y. Formal analysis was performed by B.M.A., C.O.A., and O.A.J.A. Methodology development involved contributions from B.M.A., C.O.A., and C.Y.H. Supervision was provided by B.M.A., D.S.H., C.Y.H., S.A., and J.N. Visualization tasks were handled by C.O.A. The original draft of the writing was prepared by C.O.A. and B.M.A. Writing review and editing involved B.M.A., C.O.A., O.A.J.A., C.Y.H., E.Y., S.A., J.N., C.O.A., S.A.S., and D.S.H. It is not applicable because the manuscript cannot contain a person’s data in any form (including an individual’s detailed images or Videos).
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: C. O. Assogba and B. M. Ale.
References
- 1.WHO. Consolidated guidelines on HIV, viral hepatitis and STI prevention, diagnosis, treatment and care for key populations. 144 p. [PubMed]
- 2.Banque mondiale. Incidence du VIH (% de la population de 15 à 49 ans) - Benin | Data [Internet]. [cité 10 janv 2023]. Disponible sur: https://donnees.banquemondiale.org/indicator/SH.HIV.INCD.ZS?locations=BJ
- 3.UNAIDS. Benin Country factsheets [Internet]. [cité 10 janv 2023]. Disponible sur: https://www.unaids.org/fr/regionscountries/countries/benin
- 4.Avila, D. et al. Immunodeficiency at the start of combination antiretroviral therapy in low-, middle- and high-income countries. J. Acquir. Immune Defic. Syndr.65(1), e8-16 (2014). 10.1097/QAI.0b013e3182a39979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.CNLS-TP. Rapport sur le suivi mondial de la lutte contre le sida 2020 [Internet]. Cotonou; 2020 mars [cité 5 févr 2023]. Disponible sur: https://www.unaids.org/sites/default/files/country/documents/BEN_2020_countryreport.pdf
- 6.Lozano, R. et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the global burden of disease study 2010. Lancet.380(9859), 2095–2128 (2012). 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol.16(4), 223–237 (2020). 10.1038/s41581-019-0244-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oparil, S. et al. Hypertension. Nat. Rev. Dis. Primers.4, 18014 (2018). 10.1038/nrdp.2018.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bosu, W. K., Reilly, S. T., Aheto, J. M. K. & Zucchelli, E. Hypertension in older adults in Africa: A systematic review and meta-analysis. PLoS One.14(4), e0214934 (2019). 10.1371/journal.pone.0214934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brites, C. et al. Short communication: Getting older with HIV: Increasing frequency of comorbidities and polypharmacy in Brazilian HIV patients. AIDS Res. Hum. Retrovir.35(11–12), 1103–1105 (2019). 10.1089/aid.2019.0069 [DOI] [PubMed] [Google Scholar]
- 11.Wandeler, G., Johnson, L. F. & Egger, M. Trends in life expectancy of HIV-positive adults on antiretroviral therapy across the globe: Comparisons with general population. Curr. Opin. HIV AIDS.11(5), 492 (2016). 10.1097/COH.0000000000000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maffongelli, G. et al. Impact of HIV-1 tropism on the emergence of non-AIDS events in HIV-infected patients receiving fully suppressive antiretroviral therapy. AIDS.30(5), 731–741 (2016). 10.1097/QAD.0000000000000977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu, Y., Chen, X. & Wang, K. Global prevalence of hypertension among people living with HIV: A systematic review and meta-analysis. J. Am. Soc. Hypertens.11(8), 530–540 (2017). 10.1016/j.jash.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 14.Peck, R. N. et al. Hypertension, kidney disease, HIV and antiretroviral therapy among Tanzanian adults: A cross-sectional study. BMC Med.12(1), 125 (2014). 10.1186/s12916-014-0125-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Angèle, A. K. et al. Factors associated with high blood pressure in people living with HIV at the national teaching hospital hubert Koutoukou Maga and Cotonou teaching hospital of the armed forces. Open J. Internal Med.11(4), 283–297 (2021). 10.4236/ojim.2021.114025 [DOI] [Google Scholar]
- 16.Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the European society of cardiology (ESC) and the European society of hypertension (ESH). Eur. Heart J.39(33), 3021–3104 (2018). 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 17.Gazzaruso, C. et al. Hypertension among HIV patients: Prevalence and relationships to insulin resistance and metabolic syndrome. J. Hypertens. juill21(7), 1377–1382 (2003). 10.1097/00004872-200307000-00028 [DOI] [PubMed] [Google Scholar]
- 18.Gelpi, M. et al. Higher risk of abdominal obesity, elevated low-density lipoprotein cholesterol, and hypertriglyceridemia, but not of hypertension, in people living with human immunodeficiency virus (HIV): Results from the copenhagen comorbidity in HIV infection study. Clin. Infect. Dis.67(4), 579–586 (2018). 10.1093/cid/ciy146 [DOI] [PubMed] [Google Scholar]
- 19.Dzudie, A. et al. Hypertension among people living with HIV/AIDS in Cameroon: A cross-sectional analysis from Central Africa international epidemiology databases to evaluate AIDS. PLoS One.16(7), e0253742 (2021). 10.1371/journal.pone.0253742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Serrão, R. et al. Non-AIDS-related comorbidities in people living with HIV-1 aged 50 years and older: The AGING POSITIVE study. Int. J. Infect. Dis.79, 94–100 (2019). 10.1016/j.ijid.2018.10.011 [DOI] [PubMed] [Google Scholar]
- 21.Uwanyirigira, D. et al. Prevalence and factors associated with hypertension among HIV positive patients on antiretroviral therapy: A hospital-based cross-sectional study in Rwanda. Vasc. Health Risk Manag.19, 857–870 (2023). 10.2147/VHRM.S442108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ogunmola, O. J., Oladosu, O. Y. & Olamoyegun, A. M. Association of hypertension and obesity with HIV and antiretroviral therapy in a rural tertiary health center in Nigeria: A cross-sectional cohort study. Vasc. Health Risk Manag.10, 129 (2014). 10.2147/VHRM.S58449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Heerden, A., Barnabas, R. V., Norris, S. A., Micklesfield, L. K., van Rooyen, H. & Celum, C. High prevalence of HIV and non‐communicable disease (NCD) risk factors in rural KwaZulu‐Natal, South Africa. J. Int. AIDS Soc. 20(2), (2020). [DOI] [PMC free article] [PubMed]
- 24.Achwoka, D. et al. Noncommunicable disease burden among HIV patients in care: A national retrospective longitudinal analysis of HIV-treatment outcomes in Kenya, 2003–2013. BMC Public Health19, 1–10 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mulugeta, H. et al. Incidence and predictors of hypertension among HIV patients receiving ART at public health facilities, Northwest Ethiopia: A one-year multicenter prospective follow-up study. HIV.13, 889–901 (2021). 10.2147/HIV.S329838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thiébaut, R. et al. Predictors of hypertension and changes of blood pressure in HIV-infected patients. Antivir. Ther.10(7), 811–823 (2005). 10.1177/135965350501000706 [DOI] [PubMed] [Google Scholar]
- 27.Kagaruki, G. B. et al. Magnitude and risk factors of non-communicable diseases among people living with HIV in Tanzania: A cross sectional study from Mbeya and Dar es Salaam regions. BMC Public Health14, 1–9 (2014). 10.1186/1471-2458-14-904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zewudie, B. T. et al. The magnitude of undiagnosed hypertension and associated factors among HIV-positive patients attending antiretroviral therapy clinics of Butajira General Hospital, Gurage zone, Southern Ethiopia. SAGE Open Med.10, 20503121221094456 (2022). 10.1177/20503121221094454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fan, H. et al. Incidence of hypertension among persons living with HIV in China: A multicenter cohort study. BMC Public Health.20(1), 834 (2020). 10.1186/s12889-020-08586-9 [DOI] [PMC free article] [PubMed] [Google Scholar]