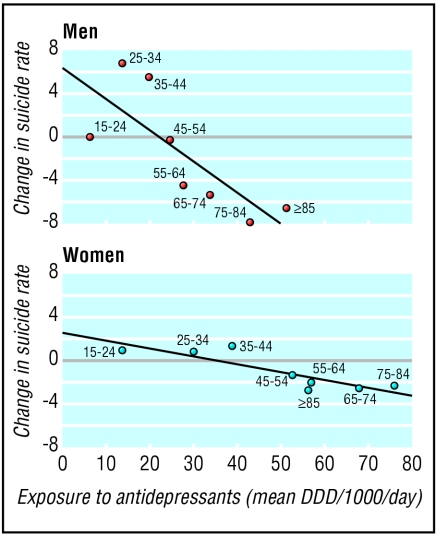
Editor—Hall et al's data on suicide rates and antidepressant prescribing contradict their own conclusions.1 The conventional and intuitive way of analysing trends in rates of antidepressant use by age group would be to look at ratios of rates of use in 1998-2001 and 1990-1.
Figure 1.
Data on bmj.com show that rates increased 7.5 times for men aged 25-34 and 2.1 times for men aged 75-84. Spearman correlations using these ratios for all age groups and the difference in suicide rates as defined by Hall et al showed a strong positive correlation. Increases in suicide rates were associated with higher rates of increase in the use of antidepressants. For men, Spearman's correlation coefficient was rs = 0.86, P = 0.007; for women, rs = 0.76, P = 0.03.
Hall et al seem to have analysed absolute differences in rates of prescribing. The use of daily dependent dose is also problematic and not clearly explained. Daily dependent doses represent units of therapeutic doses as defined by the World Health Organization. is probably accounted for partly by a change from prescribing lower doses of tricyclic anti-depressants to prescribing selective serotonin reuptake inhibitors at standard doses.
Evidence that lower doses of tricyclics are less efficacious than standard doses is not strong.2 In addition, daily dependent doses relate to the general adult population. They will therefore underestimate prescribing rates of tricyclic antidepressants in elderly people in whom therapeutic and tolerable doses are accepted to be lower.
That the massive increase in antidepressant prescribing has had any objective and positive impact on the health of populations remains difficult to prove. Other commentators have implied that there is no impact on suicide trends and pointed out that rates of self harm are rising, not falling.3 Long term incapacity due to depression in the United Kingdom continued to rise throughout the 1990s.4
Competing interests: None declared.
References
- 1.Hall DW, Mant A, Mitchell PB, Rendle VA, Hickie IB, McManus P. Association between antidepressant prescribing and suicide in Australia, 1991-2000: trend analysis. BMJ 2003;326: 1008-12. (10 May.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Furukawa TA, McGuire H, Barbui C. Meta-analysis of effects and side effects of low dosage tricyclic antidepressants in depression: systematic review. BMJ 2002; 325: 991-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Praag HM. Why has the antidepressant era not shown a significant drop in suicide rates? Crisis 2002;23: 77-82. [DOI] [PubMed] [Google Scholar]
- 4.Moncrieff J, Pommerleau J. Trends in sickness benefits in Great Britain and the contribution of mental disorders. J Public Health Med 2000;22: 59-67. [DOI] [PubMed] [Google Scholar]