Abstract
Introduction
The knowledge regarding eating behavior and disorders in women with polycystic ovary syndrome (PCOS) and severe obesity is limited. This study aimed to assess eating behavior and lifestyle factors in women with severe obesity (BMI ≥35 kg/m2), with and without PCOS, and the effect of weight loss on these behaviors.
Material and Methods
A prospective clinical trial with participants screened for PCOS using National Institutes of Health criteria. Participants completed the Food Frequency Questionnaire, International Physical Activity Questionnaire, Three‐Factor Eating Questionnaire, and Questionnaire of Eating and Weight Patterns‐revised, and were evaluated regarding binge eating disorder using DSM‐5 criteria before and after a 12‐month weight loss intervention. Clinicaltrials.gov: NCT01319162.
Results
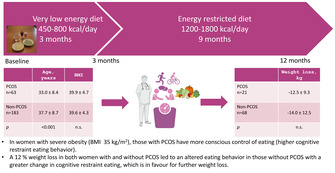
246 women were included (PCOS n = 63, age 33.0 ± 8.4, BMI 39.9 ± 4.7; non‐PCOS n = 183, age 37.7 ± 8.7, BMI 39.6 ± 4.3). Women with PCOS showed elevated baseline scores in cognitive restraint eating (50.0 [33.3–63.2]) compared to women without PCOS (38.9 [27.8–55.6]; p = 0.012). No differences were observed between groups in emotional and uncontrolled eating. In both groups, cognitive restraint eating was negatively correlated with energy intake (PCOS: r = −0.315, p < 0.05; non‐PCOS: r = −0.214, p < 0.001), while uncontrolled eating displayed a positive correlation with energy intake (PCOS: r = 0.263, p = 0.05; non‐PCOS: r = 0.402, p < 0.001). A positive correlation was found between emotional eating and energy intake only in women without PCOS (r = 0.400, p < 0.001). Baseline self‐reported energy intake and physical activity did not differ between groups. At 12‐month follow‐up, women with PCOS reported reduced fat intake. Women without PCOS reported reduced energy intake, carbohydrates and sugar, increased protein, reduced scores for emotional and uncontrolled eating, and heightened scores for cognitive restraint eating. Comparing changes from baseline to follow‐up, differences were found between groups in cognitive restraint, intake of fat, carbohydrates, and sugar. The mean weight loss was 12–14 kg, with no between‐group difference (p = 0.616).
Conclusions
Women with severe obesity and PCOS showed elevated cognitive restraint eating behaviors compared to women without PCOS. Although significant weight loss was seen in both groups, alterations in eating behavior more favorable for weight loss were only seen in women without PCOS.
Keywords: dietary intake, eating behavior, obesity, polycystic ovary syndrome, weight loss
In women with severe obesity (BMI ≥35 kg/m2), those with PCOS have more conscious control of eating (higher cognitive restraint eating behavior). A 12% weight loss in both women with and without PCOS led to an altered eating behavior in those without PCOS with a greater change in cognitive restraint eating, which is in favor of further weight loss.
Abbreviations
- BMI
body mass index
- PCOS
polycystic ovary syndrome
- VLED
very low energy diet
Key message.
In severe obesity, women with PCOS have more conscious control over their eating than those without PCOS. Weight loss interventions led to substantial and comparable weight loss in both groups; however, altered eating behaviors were specifically noted among women without PCOS.
1. INTRODUCTION
Polycystic ovary syndrome (PCOS) is a common endocrine disorder, with a prevalence of approximately 10% in women of fertile age. 1 The condition is characterized by hyperandrogenism and insulin resistance, leading to a spectrum of symptoms including reproductive disturbances such as oligo‐anovulation and infertility, 2 hirsutism, metabolic disturbances, including hyperinsulinemia, type 2 diabetes, obesity, hyperlipidemia, and hypertension, 3 , 4 as well as psychiatric disorders such as anxiety and depression. 5
The prevalence of obesity (BMI ≥30 kg/m2) in Sweden is 16%, with a predominance of severe obesity among women compared to men. 6 A strong association exists between PCOS and obesity, with a 50%–70% prevalence of obesity in American women with PCOS 7 and a 34% prevalence of obesity in a Nordic population of women with PCOS. 8 The reasons for the association between PCOS and obesity remain unclear, but it has been shown that women with PCOS have a higher rate of weight gain than women without PCOS, especially in early adulthood. 9 However, previous studies have identified comparable resting metabolic rate, energy intake, and physical activity in women with and without PCOS of fertile age across normal‐ and overweight categories. 10 , 11 Nevertheless, a higher prevalence of disordered eating and binge eating disorders (BEDs) has been observed in women with PCOS. 12
Lifestyle treatment, including dietary modifications, physical activity, and behavioral adjustments, is regarded as the first‐line therapeutic approach for weight management, aimed at both weight loss and maintenance of a healthy body weight in women with PCOS. 13 In women with PCOS, such interventions are considered beneficial in alleviating symptoms associated with PCOS and preventing metabolic complications associated with PCOS over time. 14 Despite this, there are few studies examining dietary intake, physical activity, and eating behavior in women with severe obesity (BMI ≥35 kg/m2) and PCOS during obesity treatment.
This study aimed to investigate self‐reported eating behavior, energy intake, and physical activity before and after a 12‐month weight loss intervention in a cohort of women with severe obesity, with and without PCOS, and to compare the results within and between the two groups.
2. MATERIAL AND METHODS
2.1. Design setting and participants
This is a prospective clinical trial carried out between 2011 and 2017, at the Regional Obesity Center at Sahlgrenska University Hospital, Gothenburg, Sweden, to which the participants had been referred for weight loss treatment. Women aged 18–50 years were invited to the present study. Before initiation of a weight loss intervention, all individuals that consented to participate underwent screening for PCOS using the National Institutes of Health (NIH) criteria, requiring both oligo‐/anovulation and the presence of clinical and/or biochemical hyperandrogenism, with the exclusion of other endocrine disorders. The diagnostic procedure for PCOS has been described in detail earlier. 15 Subsequently, before the start of treatment and at 12 months, patients underwent anthropometric assessments and laboratory sampling and responded to self‐administered questionnaires regarding eating behavior, dietary intake, and physical activity. The same questionnaires were completed by the participants at both baseline and follow‐up. At baseline, based on PCOS status, participants were categorically assigned to two groups: PCOS and non‐PCOS.
2.2. Anthropometry and biochemistry
Body height, weight, and waist circumference were measured according to standard protocol at baseline and at 12 months. BMI was calculated by kg/m2. 16
2.3. Eating behavior
The 21‐item Three‐Factor Eating Questionnaire (TFEQ‐R21) 17 is a questionnaire assessing eating behavior divided into three subscales that cover different eating behavior domains: emotional eating (EE), cognitive restraint eating (CR), and uncontrolled eating (UE). EE subscale assess eating as a response to emotions, cognitive restraint eating subscale assess consciously choosing to restrict food intake to lose or maintain weight and uncontrolled eating subscale assess loss of control regarding eating. Raw scores were transformed into scaled scores of 1–100, where higher scores for each subscale indicate greater emotional eating, greater cognitive restraint eating, and greater emotional eating characteristics.
2.4. Binge eating disorder
The identification of BED was done according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5) criteria, 18 based on questions from the Questionnaire of Eating and Weight Patterns‐revised (QEWP‐r), which has been translated and validated in the translated version. 19
2.5. Dietary intake
Dietary intake was assessed with a validated semi‐quantitative Food Frequency Questionnaire (FFQ) and covered habitual dietary intake over the last 3 months when completing the FFQ. 20 Energy and nutrient calculations were done with the food database from the Swedish Food Agency. 21
2.6. Physical activity
To assess physical activity, the short version of the International Physical Activity Questionnaire (IPAQ) 22 was used. IPAQ is a validated questionnaire with nine items, measuring recalled physical activity during the last 7 days with information on the time spent walking, activities of vigorous or moderate intensity, and sedentary activity/sitting. Answers were given in hours and minutes.
2.7. Intervention
All participants started the 12‐month weight loss intervention with a 12‐week period of a very low‐energy diet (VLED), which has been described in detail before. 15 The VLED regimen consisted of a liquid diet with a calorie intake of 450–800 kcal per day. 23 Subsequently, solid foods were gradually introduced within the context of an energy‐reduced diet, with caloric content adjusted to achieve a reduction of 30% from the estimated energy requirements for weight maintenance. The reintroduction of solid foods followed a step‐based pattern, starting with one meal at a time, starting with breakfast, and continuing with VLED at the other meals during the day. After 6 weeks, the next meal was reintroduced, and after another 6 weeks, the third meal was reintroduced. By that time, the participants had no meals left with VLED. Dietary advice within the framework of an energy‐reduced diet included more foods with low energy density, eg vegetables, fruits, and foods with high satiation effects, eg whole‐grain cereals. Counseling regarding physical activity was given during the whole treatment period and was individualized in relation to the preferences of the participants. Appointments were scheduled once a month for all participants with either a study nurse or a dietician. These appointments included weight assessments and support for both dietary modifications and increased physical activity.
2.8. Statistical analyses
Statistical analyses were performed using SPSS 27.0 software. Normally distributed data was presented as mean ± SD, and skewed data was presented as median and IQ range. Between‐group comparisons of women with and without PCOS were conducted using a Student's t‐test for normally distributed variables or Mann–Whitney U‐test for skewed variables, adjusting for age with an analysis of covariance (ANCOVA). The chi‐squared test was used when comparing the proportions of BEDs.
Changes from baseline to 12 months within groups were assessed using a paired t‐test and Wilcoxon signed‐rank test, and independent samples t‐test for comparing changes between the groups. Correlations were determined using the Spearman correlation test. The results were considered statistically significant at p < 0.05.
3. RESULTS
At baseline, a total of 246 women characterized by severe obesity volunteered to participate in the study (PCOS n = 63, non‐PCOS n = 183). The characteristics of the included participants are shown in Table 1. Women with PCOS were younger (PCOS 33.0 ± 8.4 years, non‐PCOS 37.7 ± 8.7 years; p < 0.001) compared to women without PCOS. No differences in BMI were observed between the two groups (PCOS 39.9 ± 4.7 kg/m2, non‐PCOS 39.6 ± 4.3 kg/m2; p = 0.787; Table 1).
TABLE 1.
Baseline characteristics in women with severe obesity with and without PCOS.
| PCOS (n = 63) | Non‐PCOS (n = 183) | p‐value crude | p‐value adjusted for age | |
|---|---|---|---|---|
| Age (years) | 33.0 ± 8.3 | 37.9 ± 8.21 | <0.001 | |
| Weight (kg) | 111.0 ± 16.8 | 110.7 ± 14.6 | 0.893 | 0.872 |
| BMI (kg/m2) | 39.9 ± 4.7 | 39.7 ± 4.3 | 0.715 | 0.763 |
| Waist circumference (cm) | 115.5 ± 12.8 | 114.9 ± 10.2 | 0.697 | 0.358 |
| Physical activity | ||||
| Sedentary behavior (min/day) | 360 (120–600) | 300 (120–555) | 0.195 | 0.213 |
| Medium/vigorous activity (min/week) | 136 (90–184) | 124 (83–165) | 0.194 | 0.354 |
| Walking (min/week) | 771 (0–1268) | 758 (0–1163) | 0.730 | 0.679 |
| Dietary intake | ||||
| Energy (kcal/day) | 2692 ± 1181 | 2648 ± 1081 | 0.787 | 0.423 |
| Protein, E% | 16.3 ± 2.6 | 16.2 ± 3.0 | 0.796 | 0.771 |
| Fat, E% | 39.0 ± 5.3 | 38.8 ± 5.6 | 0.733 | 0.878 |
| Carbohydrates, E% | 43.4 ± 5.6 | 43.7 ± 6.3 | 0.757 | 0.770 |
| Sugar, E% | 19.8 ± 5.9 | 19.9 ± 5.9 | 0.900 | 0.806 |
| Alcohol, E% | 1.0 ± 1.3 | 1.1 ± 1.8 | 0.673 | 0.944 |
| Fiber (g) | 23.6 ± 12.9 | 22.5 ± 10.4 | 0.499 | 0.142 |
| Iron (mg) | 14.7 ± 6.2 | 14.8 ± 5.7 | 0.895 | 0.663 |
| Vitamin C (mg) | 142.2 ± 77.4 | 130.0 ± 82.0 | 0.313 | 0.230 |
| Vitamin D (μg) | 8.4 ± 3.9 | 7.6 ± 3.6 | 0.163 | 0.050 |
Note: Values are presented as mean ± SD, except for physical activity, which is presented as median and IQ range. Comparisons between groups were made with an independent sample t‐test and Mann–Whitney U‐test, with adjustment for age with ANCOVA; p < 0.05 was considered statistically significant. Bold shows statistically significant p‐values.
Abbreviations: BMI, body mass index; E%, energy percent; IQ range, interquartile range; PCOS, polycystic ovary syndrome; SD, standard deviation.
At 12 months, a total of 72 women (PCOS, n = 21; non‐PCOS, n = 68) had completed the follow‐up assessments. Compared to baseline, women with PCOS lost 12.5 ± 9.3 kg, p < 0.001, and women without PCOS lost 14.0 kg ± 12.5, p < 0.001, with no difference between groups (p = 0.616). The percentage of weight loss was 11.5 ± 8.4% for women with PCOS and 12.3 ± 10.5% for those without PCOS.
3.1. Eating behavior
At baseline, women with PCOS had higher scores of cognitive restraint eating compared to women without PCOS (p = 0.012; Figure 1). However, no significant differences were found between the groups in emotional eating or uncontrolled eating (Table 1). The prevalence of BED did not differ between the PCOS and non‐PCOS groups (PCOS: 11.5%; non‐PCOS: 17.5%, p = 0.27).
FIGURE 1.
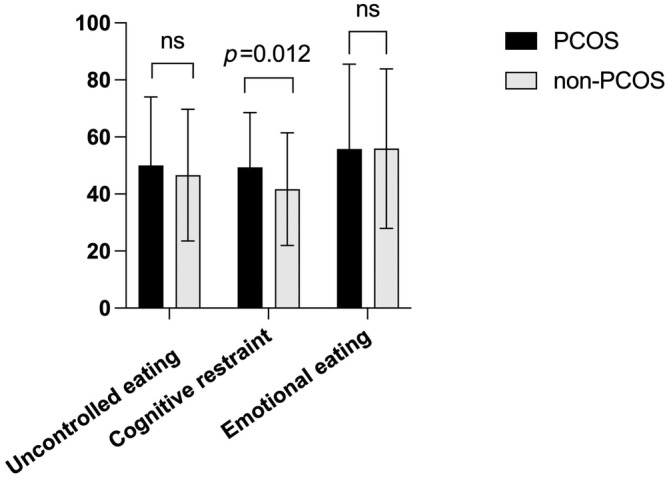
Eating behavior domains at baseline in women with severe obesity with and without PCOS. ns, non‐significant; PCOS, polycystic ovary syndrome.
Among women with PCOS who completed the 12‐month follow‐up, no significant difference was observed in self‐reported eating behavior compared to baseline. Conversely, women without PCOS reported reductions in uncontrolled eating and emotional eating and increased cognitive restraint eating compared to baseline (Table 2). At the 12‐month follow‐up, none of the 21 women with PCOS received a diagnosis of BED, while four out of the 68 women without PCOS were diagnosed with BED.
TABLE 2.
Eating behavior, dietary intake, and physical activity in women with severe obesity with and without PCOS at baseline and after a 12‐month weight loss intervention.
| PCOS (n=21) | Non‐PCOS (n=68) | p‐value b | |||||
|---|---|---|---|---|---|---|---|
| 0 mån | 12 mån | p‐value a | 0 mån | 12 mån | p‐value a | ||
| n = 16 | n = 56 | ||||||
| Weight (kg) | 106.1 ± 13.1 | 93.6 ± 13.2 | <0.001 | 110.9 ± 15.3 | 96.9 ± 16.2 | <0.001 | 0.796 |
| BMI (kg/m2) | 38.4 ± 2.3 | 33.8 ± 3.8 | <0.001 | 39.4 ± 4.3 | 34.5 ± 5.4 | <0.001 | 0.827 |
| Waist circumference (cm) | 113.2 ± 10.7 | 102.1 ± 11.2 | <0.001 | 114.4 ± 11.0 | 102.8 ± 12.3 | <0.001 | 0.941 |
| Eating behavior | |||||||
| Uncontrolled eating | 40.7 (29.6–63.0) | 55.56 (33.1–77.8) | 0.656 | 44.4 (25.9–63.0) | 38.9 (18.5–52.8) | 0.033 | 0.084 |
| Cognitive restraint | 50.0 (41.7–66.7) | 61.1 (50.0–61.7) | 0.231 | 38.9 (33.3–50.0) | 66.7 (50.0–83.3) | <0.001 | 0.004 |
| Emotional eating | 61.1 (44.4–83.3) | 55.6 (33.3–77.8) | 0.474 | 61.1 (38.9–83.3) | 50.0 (26.4–66.7) | 0.002 | 0.532 |
| Dietary intake | n = 14 | n = 48 | |||||
| Energy (kcal/day) | 2372 ± 850 | 1938 ± 740 | 0.120 | 2719 ± 971 | 2094 ± 653 | <0.001 | 0.704 |
| Protein (E%) | 16.9 ± 2.9 | 17.8 ± 1.5 | 0.372 | 15.7 ± 2.8 | 18.1 ± 4.1 | <0.001 | 0.519 |
| Fat (E%) | 41.9 ± 6.8 | 37.9 ± 3.3 | 0.041 | 39.3 ± 4.8 | 40.2 ± 7.2 | 0.373 | 0.024 |
| Carbohydrates (E%) | 40.4 ± 7.2 | 43.0 ± 4.0 | 0.101 | 43.4 ± 6.1 | 40.3 ± 8.3 | 0.012 | 0.017 |
| Sugar (E%) | 17.0 ± 5.4 | 18.7 ± 3.7 | 0.250 | 20.1 ± 6.0 | 17.4 ± 7.0 | 0.006 | 0.017 |
| Alcohol (E%) | 0.7 ± 1.0 | 1.0 ± 2.0 | 0.541 | 1.4 ± 2.1 | 1.1 ± 1.7 | 0.070 | 0.070 |
| Fiber (g) | 19.7 ± 8.7 | 19.8 ± 7.8 | 0.969 | 23.3 ± 10.9 | 23.6 ± 11.0 | 0.419 | 0.766 |
| Iron (mg) | 12.9 ± 4.3 | 11.6 ± 3.6 | 0.284 | 14.8 ± 4.6 | 13.3 ± 3.8 | 0.010 | 0.766 |
| Vit C (mg) | 93.2 ± 36.5 | 109.1 ± 54.7 | 0.195 | 146.3 ± 111.6 | 138.7 ± 78.5 | 0.301 | 0.301 |
| Vit D (μg) | 7.1 ± 2.7 | 6.3 ± 2.3 | 0.174 | 7.5 ± 3.4 | 6.9 ± 3.4 | 0.162 | 0.162 |
| Physical activity | n = 16 | n = 56 | |||||
| Sedentary behavior (min/day) | 480 (210–615) | 300 (225–435) | 0.343 | 360 (120–600) | 360 (120–480) | 0.043 | 0.851 |
| Medium/vigorous activity (min/week) | 101 (71–135) | 183 (0–530) | 0.041 | 135 (78–181) | 180 (0–300) | 0.129 | 0.234 |
| Walking (min/week) | 899 (65–1399) | 178 (60–298) | 0.121 | 863 (315–1261) | 165 (64–420) | <0.001 | 0.914 |
Note: Values are presented as mean and ± SD for anthropometrics and energy intake, and median and IQ range for eating behavior and physical activity. Bold shows statistically significant p‐values.
Abbreviations: CR, cognitive restraint; E%, energy percent; EE, emotional eating; IQ range, interquartile range; PCOS, polycystic ovary syndrome; SD, standard deviation; UE, uncontrolled eating.
p‐value within group, paired samples t‐test for anthropometrics and energy intake, and Wilcoxon signed‐rank test for eating behavior and physical activity.
p‐value of change between groups at 12 months was analyzed with Mann–Whitney U‐test.
3.2. Dietary intake and physical activity
At baseline, there was no difference in self‐reported energy intake, macronutrients or micronutrients, or physical activity levels between women with and without PCOS (Table 1).
Among women with PCOS who remained at 12‐month follow‐up, a reduced intake of energy percent (E%) fat was found compared to baseline (Table 2). Women without PCOS reported a reduction in energy intake, E% carbohydrates, and sugars, increased E% protein, and reduced iron intake compared to baseline (Table 2). No statistically significant changes in micronutrients were found within groups at 12‐month follow‐up or in change between groups (Table 2).
Furthermore, at 12‐month follow‐up, women with PCOS reported increased time spent on medium‐to‐vigorous activity, while women without PCOS reported reduced time spent walking (Table 2).
3.3. 12‐month follow‐up
From baseline to follow‐up, a difference in cognitive restraint eating was found with a higher increase in that score in the non‐PCOS group compared with the PCOS‐group (p = 0.004), for fat intake, where women with PCOS decreased fat intake more (p = 0.024), and in carbohydrate intake and sugar intake, where women without PCOS decreased their intake more, with both nutrients (p = 0.017) compared to women with PCOS.
3.4. Weight change categories
All participants, independent of PCOS status, were divided into two weight change categories: <5% or weight gain, and ≥10% (Table 3). Within the ≥10% weight loss group, weight loss was −24.5 ± 9.8%, and in the <5% weight loss or weight gain group, weight loss was −0.3 ± 4.0% (Table 3). Women in the ≥10% weight loss group reported higher cognitive restraint eating (p = 0.002), lower emotional eating (p = 0.047), and more time spent in sedentary activity (p = 0.037) compared to those in the <5% weight loss group. No differences were found between the two weight change categories for emotional eating (Table 3).
TABLE 3.
Energy intake, eating behavior, and physical activity for all women at 12 months in relation to two weight change categories.
| >10% (n = 29) | <5% or gain (n = 16) | p‐value | |
|---|---|---|---|
| Weight loss (%) | −24.5 ± 9.8 | −0.3 ± 4.0 | <0.001 |
| Energy intake (kcal/day) | 1985 ± 615 | 2253 ± 761 | 0.205 |
| Moderate/vigorous activity (min/week) | 180 (0–570) | 165 (0–345) | 0.155 |
| Walking (min/week) | 200 (60–420) | 190 (71–592) | 0.618 |
| Sedentary behavior (min/day) | 360 (165–480) | 150 (41–570) | 0.037 |
| Uncontrolled eating | 33.3 (14.8–59.3) | 48.2 (27.8–63.9) | 0.231 |
| Cognitive restraint | 72.2 (61.1–83.3) | 55.6 (44.4–66.7) | 0.002 |
| Emotional eating | 38.9 (13.9–61.1) | 61.1 (33.3–83.3) | 0.047 |
Note: Values are presented as mean ± SD, except for physical activity and eating behavior, which is presented as median and IQ range. Comparisons between groups were made with independent samples t‐test for weight loss and energy intake, and Mann–Whitney U‐test physical activity and eating behavior. p < 0.05 was considered statistically significant. Bold shows statistically significant p‐values.
Abbreviations: E%, energy percent; IQ range, interquartile range; PCOS, polycystic ovary syndrome; SD, standard deviation.
3.5. Correlations
At baseline, within both groups, a negative correlation was found between cognitive restraint and energy intake (r = −0.315, p < 0.05 [PCOS group], r = −0.214, p < 0.001 [non‐PCOS group]), whereas uncontrolled eating demonstrated a positive correlation with energy intake (r = 0.263, p < 0.05 [PCOS group], r = 0.402, p < 0.001 [non‐PCOS group]; Table 4). A positive correlation was found between emotional eating and energy intake only in women without PCOS (r = 0.400, p < 0.001; Table 4). Furthermore, there was a negative correlation between reported E% fat at baseline and weight change in the PCOS‐group (r = −0.470, p < 0.05). In women without PCOS, a negative correlation was found between baseline sedentary behavior/sitting time and weight change (r = −0.268, p < 0.05) and a negative correlation between baseline uncontrolled eating and weight change (r = −0.298, p < 0.05; Table 4).
TABLE 4.
Correlations between physical activity, dietary intake, and eating behavior at baseline with a 12‐months weight change in women with severe obesity with and without PCOS.
| PCOS (n= 63) | Moderate/vigorous activity | Walking | Sedentary activity | Energy intake | Protein | Fat | Carbohydrates | UE | CR | EE |
|---|---|---|---|---|---|---|---|---|---|---|
| Weight change (n= 16) | 0.221 | −0.039 | −0.405 | −0.014 | 0.201 | −0.470 * | 0.369 | −0.191 | −0.151 | −0.054 |
| Moderate/vigorous activity | −0.150 | −0.219 | 0.557 ** | −0.314 * | −0.181 | 0.348 ** | −0.036 | 0.080 | −0.290 * | |
| Walking | 0.119 | −0.100 | 0.368 ** | −0.001 | −0.206 | 0.412 ** | 0.082 | 0.755 ** | ||
| Sedentary activity | 0.055 | 0.116 | 0.153 | −0.230 | 0.295 * | −0.122 | 0.301 * | |||
| Energy intake | −0.307* | 0.242 | −0.036 | 0.263 * | −0.315* | −0.072 | ||||
| Protein | −0.078 | −0.424 ** | 0.024 | −0.089 | 0.209 | |||||
| Fat | −0.843 ** | 0.196 | 0.119 | 0.018 | ||||||
| Carbohydrates | −0.183 | −0.107 | −0.137 | |||||||
| UE | −0.077 | 0.614 ** | ||||||||
| CR | −0.033 |
| Non‐ PCOS (n= 183) | Moderate/vigorous activity | Walking | Sedentary | Energy intake | Protein | Fat | Carbohydrates | UE | CR | EE |
|---|---|---|---|---|---|---|---|---|---|---|
| Weight change (n= 56) | −0.038 | −0.156 | −0.268 * | −0.138 | 0.089 | −0.009 | −0.075 | −0.298 * | 0.205 | −0.161 |
| Moderate/vigorous activity | 0.127 | −0.161 * | 0.455 ** | −0.144 | −0.168 * | 0.236 ** | 0.092 | 0.010 | 0.051 | |
| Walking | 0.033 | 0.198 ** | 0.219 ** | 0.136 | −0.172* | 0.446 ** | −0.009 | 0.659 ** | ||
| Sedentary activity | −0.010 | 0.054 | 0.135 | −0.152 | 0.162 * | −0.070 | 0.052 | |||
| Energy intake | −0.355 ** | 0.222 ** | 0.022 | 0.402 ** | −0.214 ** | 0.400 ** | ||||
| Protein | 0.044 | −0.497 ** | −0.185 * | 0.180 * | −0.177 * | |||||
| Fat | −0.845 ** | 0.267 ** | −0.018 | 0.185 * | ||||||
| Carbohydrates | −0.132 | −0.087 | −0.015 | |||||||
| UE | −0.131 | 0.621 ** | ||||||||
| CR | −0.081 |
Note: Values are presented as the correlation coefficient r. Correlation analyses were made with the Spearman correlation test, and p < 0.05 was considered statistically significant. Bold shows statistically significant p‐values.
Abbreviations: CR, cognitive restraint; E%, energy percent; EE, emotional eating; PCOS, polycystic ovary syndrome; UE, uncontrolled eating.
p < 0.05;
p < 0.001.
4. DISCUSSION
This study found higher levels of cognitive restraint eating behavior in women with severe obesity and PCOS. This behavior was associated with lower energy intake, whereas uncontrolled eating was associated with higher energy intake in both women with and without PCOS. After a weight loss intervention with clinically significant and similar weight loss in both groups, altered eating behaviors were noted only in women without PCOS. Those who lost ≥10% in weight, independent of PCOS status, after the 12‐month intervention reported higher cognitive restraint eating behavior and less emotional eating.
In this study, women with PCOS demonstrated elevated cognitive restraint eating behavior at baseline in comparison to their counterparts without PCOS, while scores for emotional and uncontrolled eating were similar between the two groups. Cognitive restraint eating behavior entails a heightened preoccupation with the type and quantity of food consumed to influence bodyweight and shape, representing an eating behavior that promotes weight loss or weight maintenance. 24 Notably, earlier research on eating behavior in women with PCOS has found inconsistent results. Larsson et al. 10 found no differences in eating behavior between women with and without PCOS, while Basar et al. 25 showed elevated cognitive restraint eating in women with PCOS. It is relevant to note that both of these studies included women with a mean BMI ranging from overweight to obesity but not severe obesity. 10 , 25 Thus, the result of the present study is supported by the study of Basar et al., 25 which shows that cognitive restraint eating behavior is more prevalent in women with severe obesity and PCOS compared to women with severe obesity without PCOS. One plausible explanation for the elevated cognitive restraint eating in women with severe obesity and PCOS could be attributed to the perception of being overweight and the multiple weight loss attempts that have been shown in women with PCOS 26 that may contribute to an increased awareness of weight‐related concerns.
The prevalence of BED in the general population ranges from 1%–2% to 14%–19% in populations with severe obesity, 27 which is in line with our results. In the present study, no difference in BED could be found between PCOS and the non‐PCOS groups. This stands in contrast to previous studies, indicating a higher prevalence of any eating disorder, including BED, in women with PCOS. 12 However, studies specifically addressing BEDs in women with PCOS are limited.
A substantial variation in self‐reported energy intake was noted, as reflected by large standard deviations in both groups, with no statistically significant differences between groups. Previous studies in women with PCOS have reported similar levels of energy intake when compared with women without PCOS. 10 It is important to note that self‐reported data on energy intake introduce the potential for reporting bias. However, when utilizing the mean estimated energy requirements for weight stability, according to the Mifflin St. Jeor equation, 28 the reported energy intake at baseline in both groups was comparable with the energy requirements for the participants' weight at the time, which implies a reasonably accurate reporting of the energy intake at baseline.
The adherence during the strict VLED period was high due to the average weight loss during that period (data not shown). In another study on patients with psoriatic arthritis, we collected data on participants' experiences of the VLED period and their return from VLED to regular foods. 29 The participants found the strict VLED period easy to implement, while the return to regular foods was more difficult. 29 Although this is another patient group, it could be assumed that difficulties regarding dietary change for weight loss are similar regardless of diagnosis.
Baseline physical activity in both study groups falls below the recommended levels outlined for adults by the World Health Organization (WHO), 30 which are also the recommendations for women with PCOS. 13 This observation is comparable with prior findings indicating reduced physical activity in individuals with obesity 31 and supports the inverse relationship documented between body mass index (BMI) and physical activity. 32
During the strict VLED period, energy intake is markedly reduced to facilitate significant and rapid weight loss, with the aim of encouraging further behavioral changes for weight loss. 23 Due to this intervention, including VLED, both groups reduced significantly in weight from baseline to follow‐up. The important finding was that women with PCOS responded to the weight loss intervention similarly to women without PCOS, with comparable average weight loss in both groups. Based on clinical experience, women with PCOS may say that due to having PCOS, they have more difficulties losing weight than women without PCOS. However, the present study shows that they respond to a weight loss treatment as well as women without PCOS, and this information may be used in discussions with women with PCOS and obesity. A reduction in self‐reported energy intake was seen only in women without PCOS. This was associated with an increased intake of protein and a decreased intake of carbohydrates and sugar at the 12‐month follow‐up. In women with PCOS, self‐reported energy intake did not decrease significantly; however, a reduction in E% fat was found. Although a reduction in E% sugar was found in women without PCOS, both groups reported a very high sugar intake both before and after weight loss intervention, with an almost double intake compared to recommendations from international guidelines. 33 Comparing changes between groups, women with PCOS reduced fat intake more than women without PCOS, whereas women without PCOS reduce their intake of carbohydrates and sugar more than women with PCOS. Previous studies showed no difference in weight loss after a low‐fat diet compared to a low‐carbohydrate diet, 34 and indeed, the two groups in the present study did not differ in weight loss.
Wang et al. 35 observed reduced energy intake and significant but modest weight loss in women with severe obesity, both in those with and without PCOS, following a 6‐month lifestyle intervention. This study was a post‐hoc analysis of a treatment group in a randomized controlled study in women scheduled for infertility treatment, with a dropout rate of 25% in the PCOS group and 20% in the non‐PCOS group, respectively. 35 Caution is warranted in interpreting the findings, as the motivation for weight loss may be influenced by the context of infertility treatment. However, the findings of the latter study support our results that women with obesity and PCOS can reduce their weight as well as women without PCOS. Although our study had a longer follow‐up, we also had a higher dropout rate compared to the study of Wang et al. 35
Alterations in eating behavior after intervention, characterized by reductions in uncontrolled eating, emotional eating, and increased cognitive restraint eating, and behaviors in favor of weight loss, were exclusively observed in women without PCOS. Women without PCOS also increased their cognitive restraint more compared to those with PCOS. These results are comparable with a previous study in women with overweight or obesity without PCOS, who underwent a 12‐week dietary intervention, resulting in modest weight loss with improvements in all three domains of eating behavior. 36 Conversely, in a 12‐month RCT in women with PCOS trying to achieve pregnancy, the lifestyle intervention resulted in 5% weight loss and the participants reported increased restraint eating post‐intervention. 37 However, these studies used different eating behavior questionnaires than the present study and did not compare women with and without PCOS.
The reason why women with PCOS, in the present study, showed no change in cognitive restraint eating while women without PCOS did could be explained by the limited number of participants at follow‐up, resulting in a potential lack of statistical power.
In women with obesity and PCOS, a weight loss greater than 5% has demonstrated improvement in symptoms of PCOS 38 ; however, most studies are small, and to date, international evidence‐based guidelines for PCOS do not recommend a specific percentage of weight loss for women with PCOS to improve hormonal and metabolic variables. 13 In the present study, categorizing participants based on weight loss, individuals achieving 10% weight loss exhibited higher cognitive restraint compared to those with <5% weight loss or weight gain. Due to the limited number of participants at follow‐up, categorization by PCOS diagnosis was not feasible. These results may imply that substantial weight loss can foster behavioral changes in favor of further weight loss, especially in women with severe obesity. This is supported by previous findings that indicate that individuals achieving rapid weight loss, which is often the case with treatment including VLED, are more likely to maintain long‐term weight loss. 39
In both groups, cognitive restraint eating exhibited a negative correlation with energy intake at baseline. Uncontrolled eating correlated positively with energy intake in women without PCOS, whereas this correlation was not evident in women with PCOS. These results indicate that cognitive restraint eating can favor weight loss, whereas uncontrolled eating can be a barrier to weight loss.
In women without PCOS, sedentary behavior/sitting time and uncontrolled eating were negatively correlated with weight loss; thus, the higher the baseline sedentary behavior/sitting time and uncontrolled eating, the greater the weight loss at 12 months. This seems contradictory but could be explained by the fact that more unfavorable behaviors for weight loss at baseline give room for larger behavioral changes during the intervention.
The strengths of this study include a relatively large baseline cohort with no statistically significant differences between the PCOS and non‐PCOS groups regarding anthropometric measures. Other strengths were the usage of validated questionnaires and the structured weight loss intervention with regular check‐up visits, as well as the long follow‐up time of 12 months. Limitations include the selected group of women with severe obesity, and therefore the generalizability to other age‐ and BMI groups is limited. Additionally, self‐reported dietary intake is another limitation, where participants may tend to both under‐report and mis‐report dietary intake. However, average energy intake seems reasonable in relation to energy needs for the average baseline weight in both women with and without PCOS.
The substantial dropout impedes the power of the study, potentially explaining the absence of statistically significant changes. High drop‐out rates are common in weight loss interventions, and this study falls within the upper interval, possibly caused by the follow‐up time of the study. Those dropping out of weight loss studies tend to be those who lose less weight during the intervention or those who are younger than 50 years, 40 as women were in this study. In women with PCOS specifically, drop‐out from a weight loss intervention is associated with more depressive symptoms, while higher appointment attendance is associated with a greater adherence rate and a greater weight loss. 41
Notably, no difference in age, anthropometry, or metabolic parameters was observed between dropouts and completers in the present study. 15
5. CONCLUSION
In this prospective study of women with severe obesity, those with PCOS reported higher conscious control regarding eating than women without PCOS, a behavior correlated with lower self‐reported energy intake irrespective of PCOS status. A 1‐year weight loss program resulted in clinically significant weight loss in both groups but did not elicit discernible effects on eating behavior in women with PCOS. In contrast, the intervention induced alterations in eating behavior among women without PCOS that may be favorable for further weight loss or the maintenance of achieved weight loss. To evaluate long‐term effects of weight loss intervention on eating behavior, longer follow‐up studies regarding eating behavior after weight loss intervention is warranted in women with severe obesity and PCOS.
AUTHOR CONTRIBUTIONS
Josefin Kataoka, Elisabet Stener‐Victorin, J.S., and I.L. contributed to conception and planning of the study, drafting, and revising of the manuscript. Josefin Kataoka and Ingrid Larsson contributed to analyzing and interpreting data. All authors approved the final version of the manuscript.
FUNDING INFORMATION
The work was supported by the Vetenskapsrådet (project no. 2018‐02872 and 2022‐005520); Novo Nordisk Foundation (NNF19OC0056647 and NNF22OC0072904 ESV); Diabetes Foundation (DIA2021‐633); Strategic Research Programme (SRP) in Diabetes at Karolinska Institutet; the Regional Agreement on Medical Training and Clinical Research between the Stockholm County Council and the Karolinska Institutet ALFMedN 20 190 079 (all ESV); and Göteborgs läkaresällskap Research grant for PhD student (GLS 961123) (JK).
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interests to disclose.
ETHICS STATEMENT
The study was conducted following the Declaration of Helsinki and was approved by the regional ethical review board of the University of Gothenburg, Sweden, DNR‐106‐11. Date of approval was 2011‐03‐31. All participants gave oral and written informed consent before entering the study. The study was registered at Clinicaltrial.gov: NCT01319162, March 18, 2011.
Kataoka J, Stener‐Victorin E, Schmidt J, Larsson I. A prospective 12‐month structured weight loss intervention in women with severe obesity and polycystic ovary syndrome: Impact of weight loss on eating behaviors. Acta Obstet Gynecol Scand. 2024;103:1615‐1624. doi: 10.1111/aogs.14867
REFERENCES
- 1. March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25:544‐551. [DOI] [PubMed] [Google Scholar]
- 2. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. 2010;8:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Legro RS, Kunselman AR, Dodson WC, Dunaif A. Prevalence and predictors of risk for type 2 diabetes mellitus and impaired glucose tolerance in polycystic ovary syndrome: a prospective, controlled study in 254 affected women. J Clin Endocrinol Metab. 1999;84:165‐169. [DOI] [PubMed] [Google Scholar]
- 4. Ollila ME, Kaikkonen K, Järvelin MR, et al. Self‐reported polycystic ovary syndrome is associated with hypertension: a northern Finland birth cohort 1966 study. J Clin Endocrinol Metab. 2019;104:1221‐1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cooney LG, Dokras A. Depression and anxiety in polycystic ovary syndrome: etiology and treatment. Curr Psychiatry Rep. 2017;19:83. [DOI] [PubMed] [Google Scholar]
- 6. The public health agency of Sweden The national public health survey: public health in Sweden. 2022.
- 7. Lim SS, Norman RJ, Davies MJ, Moran LJ. The effect of obesity on polycystic ovary syndrome: a systematic review and meta‐analysis. Obes Rev. 2013;14:95‐109. [DOI] [PubMed] [Google Scholar]
- 8. Ollila MM, Piltonen T, Puukka K, et al. Weight gain and dyslipidemia in early adulthood associate with olycystic ovary syndrome: prospective cohort study. J Clin Endocrinol Metab. 2016;101:739‐747. [DOI] [PubMed] [Google Scholar]
- 9. Teede HJ, Joham AE, Paul E, et al. Longitudinal weight gain in women identified with polycystic ovary syndrome: results of an observational study in young women. Obesity. 2013;21:1526‐1532. [DOI] [PubMed] [Google Scholar]
- 10. Larsson I, Hulthén L, Landén M, Pålsson E, Janson P, Stener‐Victorin E. Dietary intake, resting energy expenditure, and eating behavior in women with and without polycystic ovary syndrome. Clin Nutr. 2016;35:213‐218. [DOI] [PubMed] [Google Scholar]
- 11. Lin AW, Kazemi M, Jarrett BY, et al. Dietary and physical activity behaviors in women with polycystic ovary syndrome per the new international evidence‐based guideline. Nutrients. 2019;11:2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tay CT, Teede HJ, Hill B, Loxton D, Joham AE. Increased prevalence of eating disorders, low self‐esteem, and psychological distress in women with polycystic ovary syndrome: a community‐based cohort study. Fertil Steril. 2019;112:353‐361. [DOI] [PubMed] [Google Scholar]
- 13. Teede HJ, Tay CT, Laven J, et al. Recommendations from the 2023 international evidence‐based guideline for the assessment and management of polycystic ovary syndrome. Hum Reprod. 2023;38:1655‐1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Moran LJ, Hutchison SK, Norman RJ, Teede HJ. Lifestyle changes in women with polycystic ovary syndrome. Cochrane Database Syst Rev. 2011;(7):CD007506. [DOI] [PubMed] [Google Scholar]
- 15. Kataoka J, Larsson I, Björkman S, Eliasson B, Schmidt J, Stener‐Victorin E. Prevalence of polycystic ovary syndrome in women with severe obesity—effects of a structured weight loss programme. Clin Endocrinol. 2019;91:750‐758. [DOI] [PubMed] [Google Scholar]
- 16. WHO Expert Committee on physical Status: the use and interpretation of anthropometry (1993: Geneva, Switzerland) & World Health Organization . Physical status: the use of and interpretation of anthropometry, report of a WHO Expert Committee. World Health Organization; 1995. [PubMed] [Google Scholar]
- 17. Karlsson J, Persson LO, Sjöström L, Sullivan M. Psychometric properties and factor structure of the three‐factor eating questionnaire (TFEQ) in obese men and women. Results from the Swedish obese subjects (SOS) study. Int J Obes Relat Metab Disord. 2000;24:1715‐1725. [DOI] [PubMed] [Google Scholar]
- 18. Diagnostic and Statistical Manual of Mental Disorders (5th ed., DSM‐5). 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 19. Borges MB, Morgan CM, Claudino AM, da Silveira DX. Validation of the portuguese version of the questionnaire on eating and weight patterns‐revised (QEWP‐R) for the screening of binge eating disorder. Braz J Psychiatry. 2005;27:319‐322. [DOI] [PubMed] [Google Scholar]
- 20. Lindroos AK, Lissner L, Sjöström L. Validity and reproducibility of a self‐administered dietary questionnaire in obese and non‐obese subjects. Eur J Clin Nutr. 1993;47:461‐481. [PubMed] [Google Scholar]
- 21. The Swedish Food Composition Database . The Swedish food agency. 2015.
- 22. Craig CL, Marshall AL, Sjöström M, et al. International Physical Activity Questionnaire: 12‐country reliability and validity. Med Sci Sports Exerc. 2003;35:1381‐1395. [DOI] [PubMed] [Google Scholar]
- 23. Mustajoki P, Pekkarinen T. Very low energy diets in the treatment of obesity. Obes Rev. 2001;2:61‐72. [DOI] [PubMed] [Google Scholar]
- 24. Urbanek JK, Metzgar CJ, Hsiao PY, Piehowski KE, Nickols‐Richardson SM. Increase in cognitive eating restraint predicts weight loss and change in other anthropometric measurements in overweight/obese premenopausal women. Appetite. 2015;87:244‐250. [DOI] [PubMed] [Google Scholar]
- 25. Başar Gökcen B, Akdevelioğlu Y, Canan S, Bozkurt N. Increased risk of eating disorders in women with polycystic ovary syndrome: a case‐control study. Gynecol Endocrinol. 2020;36:764‐767. [DOI] [PubMed] [Google Scholar]
- 26. Pesonen E, Nurkkala M, Niemelä M, et al. Polycystic ovary syndrome is associated with weight‐loss attempts and perception of overweight independent of BMI: a population‐based cohort study. Obesity. 2023;31:1108‐1120. [DOI] [PubMed] [Google Scholar]
- 27. Björkman S, Wallengren O, Laurenius A, Eliasson B, Larsson I. Nocturnal eating but not binge eating disorder is related to less 12 months' weight loss in men and women with severe obesity: a retrospective cohort study. Clin Obes. 2020;10:e12408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mifflin MD, St Jeor ST, Hill LA, Scott BJ, Daugherty SA, Koh YO. A new predictive equation for resting energy expenditure in healthy individuals. Am J Clin Nutr. 1990;51:241‐247. [DOI] [PubMed] [Google Scholar]
- 29. Klingberg E, Bilberg A, Björkman S, et al. Weight loss improves disease activity in patients with psoriatic arthritis and obesity: an interventional study. Arthritis Res Ther. 2019;21:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bull FC, Al‐Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54:1451‐1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sander C, Ueck P, Mergl R, Gordon G, Hegerl U, Himmerich H. Physical activity in depressed and non‐depressed patients with obesity. Eat Weight Disord. 2018;23:195‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Besson H, Ekelund U, Luan J, et al. A cross‐sectional analysis of physical activity and obesity indicators in European participants of the EPIC‐PANACEA study I. Int J Obes. 2009;33:497‐506. [DOI] [PubMed] [Google Scholar]
- 33. Blomhoff R, Andersen R, Arnesen EK, et al. Nordic nutrition recommendations 2023: integrating environmental aspects. 2023. doi: 10.6027/nord2023-003 [DOI]
- 34. Gardner CD, Trepanowski JF, Del Gobbo LC, et al. Effect of low‐fat vs low‐carbohydrate diet on 12‐month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA. 2018;319:667‐679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wang Z, Groen H, Cantineau AEP, et al. Effectiveness of a 6‐month lifestyle intervention on diet, physical activity, quality of life, and markers of cardiometabolic health in women with PCOS and obesity and non‐PCOS obese controls: one size fits all? Nutrients. 2021;13:3425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Beaulieu K, Casanova N, Oustric P, et al. Matched weight loss through intermittent or continuous energy restriction does not lead to compensatory increases in appetite and eating behavior in a randomized controlled trial in women with overweight and obesity. J Nutr. 2020;150:623‐633. [DOI] [PubMed] [Google Scholar]
- 37. Jiskoot G, de Loos AD, Timman R, Beerthuizen A, Laven J, Busschbach J. Changes in eating behavior through lifestyle treatment in women with polycystic ovary syndrome (PCOS): a randomized controlled trial. J Eat Disord. 2022;10:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kiddy DS, Hamilton‐Fairley D, Bush A, et al. Improvement in endocrine and ovarian function during dietary treatment of obese women with polycystic ovary syndrome. Clin Endocrinol. 1992;36:105‐111. [DOI] [PubMed] [Google Scholar]
- 39. Rolland C, Johnston KL, Lula S, Macdonald I, Broom J. Long‐term weight loss maintenance and management following a VLCD: a 3‐year outcome. Int J Clin Pract. 2014;68:379‐387. [DOI] [PubMed] [Google Scholar]
- 40. Batterham M, Tapsell LC, Charlton KE. Predicting dropout in dietary weight loss trials using demographic and early weight change characteristics: implications for trial design. Obes Res Clin Pract. 2016;10:189‐196. [DOI] [PubMed] [Google Scholar]
- 41. Moran LJ, Noakes M, Clifton P, et al. Predictors of lifestyle intervention attrition or weight loss success in women with polycystic ovary syndrome who are overweight or obese. Nutrients. 2019;11(3):492. [DOI] [PMC free article] [PubMed] [Google Scholar]


