Abstract
Primary Ciliary Dyskinesia (PCD) is a rare autosomal recessive disorder caused by impaired ciliary function. The incidence of PCD is 1 in 20,000 births. Kartagener's syndrome (KS), a subtype of PCD, is distinguished by the presence of situs inversus. KS occurs in about 1 in 32,000 to 40,000 births. Characterized by a triad of situs inversus totalis, sinusitis, and typically lower lobe bronchiectasis, Kartagener's syndrome presents with distinct radiological features, which are explored in this case study. We report on an adolescent male with Kartagener's syndrome, manifesting atypical bronchiectasis in the left upper lobe, leading to a bilateral lung transplant, and severe pectus excavatum requiring surgical correction. This case documents a male patient with concurrent Kartagener's syndrome and pectus excavatum, supporting a previously explored, albeit theoretical association between these conditions.
Keywords: Kartagener, Bronchiectasis, Excavatum, Situs Inversus
Introduction
Primary ciliary dyskinesia (PCD), an autosomal-recessive congenital disorder, is predominately characterized by impaired ciliary motility [1]. This is typically secondary to the absence or misalignment of dynein arms in the cilia, although microtubule and radial spoke anomalies have also been noted in the literature [2]. These structural defects manifest as reduced ciliary beat frequency, compromising respiratory secretion clearance and increasing infection susceptibility [3]. Given that ciliated epithelial are present throughout the nasal mucosa, paranasal sinuses and lower respiratory tract, patients have a predisposition for chronic sinusitis and bronchiectasis [4].
This case focuses on a patient with Kartagener's syndrome, a variant of Primary Ciliary Dyskinesia (PCD). This syndrome is characterized not just by typical respiratory symptoms of PCD but also by a notable anatomical anomaly: situs inversus, where organ placement is the reverse of the standard arrangement [5].
While situs inversus is uncommon in the general population, with an occurrence of about 1 in 10,000, it surprisingly manifests in half of those with PCD [6]. The explanation for this may lie in genetics; one hypothesis proposes a link between the genes governing ciliary development and those responsible for left-right body orientation [7]. Another theory posits that appropriate ciliary motion during embryonic development is crucial for correct visceral positioning. Structural ciliary defects, such as the lack of or misalignment of dynein arms, might result in disorganized and random visceral situs determination [8]. This could explain why situs inversus occurs in roughly 50% of PCD cases. Consequently, Kartagener's syndrome is defined by a triad of chronic sinusitis, bronchiectasis, and situs inversus [5].
Each element of the Kartagener's syndrome triad exhibits unique radiological features, which are detailed in this case report. Chronic sinusitis is radiologically discerned by mucosal thickening and obstruction of the osteomeatal complex [9]. Bronchiectasis, a result of persistent lower respiratory tract infections, presents as a consistent widening of the bronchial airways. Situs inversus totalis is identified through a radiological reversal of anatomical structures, including dextrocardia, a liver positioned on the left, spleen on the right, a displaced gastric bubble, and unusual lung lobation – 3 lobes in the left lung and 2 in the right [1]. Additionally, this report will discuss specific anatomical and pathological anomalies observed in our patient, such as pectus excavatum, identifiable by an increased Haller Index, and atypical upper lobar bronchiectasis.
The link between Kartagener's syndrome and pectus excavatum is a theoretical one, with 1 case series demonstrating a 9% incidence of pectus excavatum in a cohort of patients with Kartagener's syndrome, much greater than 0.3% prevalence in the general population [10]. While this link is unclear at this point, a diagnosis of Kartagener syndrome should be considered with patients with pectus excavatum and concomitant sinopulmonary disease.
Case presentation
This case report details the medical journey of an adolescent male diagnosed with Kartagener's syndrome at a young age. The patient was delivered via Lower Segment Caesarean Section at 42 weeks’ gestation due to meconium ileus and failure to progress in spontaneous labor. Postnatal complications included severe respiratory distress, requiring Neonatal Intensive Care Unit admission. A neonatal chest X-ray (CXR) revealed dextrocardia, a condition not previously detected via ultrasound. The patient was discharged at 3 weeks postpartum, necessitating home oxygen therapy.
The formal diagnosis of Kartageners was confirmed at 3 months of age by a nasal biopsy demonstrating immotile cilia. The patients’ early years were marked by recurrent upper respiratory tract infections, leading to a tonsillectomy, adenectomy, and 3 grommet insertions by age 3. They had their first episode of bronchiectasis at age 4, noted on a computed tomography (CT) chest scan. Recurrent presentations of sinusitis and bronchiectasis followed demanding extensive antibiotic regiments (including Amikacin, Bactrim, Clarithromycin, Moxifloxacin, Tobramycin, Cefepime, and Ceftazidime) to combat increasing resistance. Treatment often involved intravenous antibiotics via a Peripherally Inserted Central Catheter (PICC) line, supplemented by hospital-in-the-home (HITH) care.
The management for bronchiectasis in Kartagener syndrome involves a multi-faceted approach. Pulmonary rehabilitation, in addition to chest physiotherapy, has been shown to improve patient's exercise tolerance and health-related quality of life [11]. Antibiotics, both prophylactic and therapeutic, are used to treat persistent respiratory infections. This patient developed extensive resistance to antibiotics due to recurrent infections, which limited treatment. There has been limited evidence about the efficacy of mucolytic agents in bronchiectasis [12]. In severe cases of bronchiectasis refractory to conservative treatment options, lung transplantation can be considered. Due to this patient's young age and severe bronchiectasis, he was a good candidate for bilateral lung transplant and had a good outcome.
The patient first showed signs of pectus excavatum at 11 years, concurrent with the onset of mild finger clubbing. He developed severe pectus excavatum with a Haller index of 3.55. Severe pectus excavatum is associated with decreased cardiovascular function. Surgical correction is generally considered for Haller index of 3.25 or higher. Current literature describes 2 main methods for repair, the open Ravitch procedure via anterior chest wall incision, or the minimally invasive Nuss approach. Studies have shown both procedures to have good outcomes with minimal complications. In our case, this patient underwent a Ravitch procedure with positive postoperative outcomes.
Sinusitis can be managed by nasal irrigation, corticosteroids, or topical decongestants. In some instances, refractory cases can be managed surgically with functional endoscopic sinus surgery [13]. At age 14, this patent received endoscopic turbinate surgery for chronic sinusitis.
In this case study, we delve into the anatomical and pathological manifestations of this patient's disease process prior to surgical intervention.
Anatomical manifestations
Situs inversus
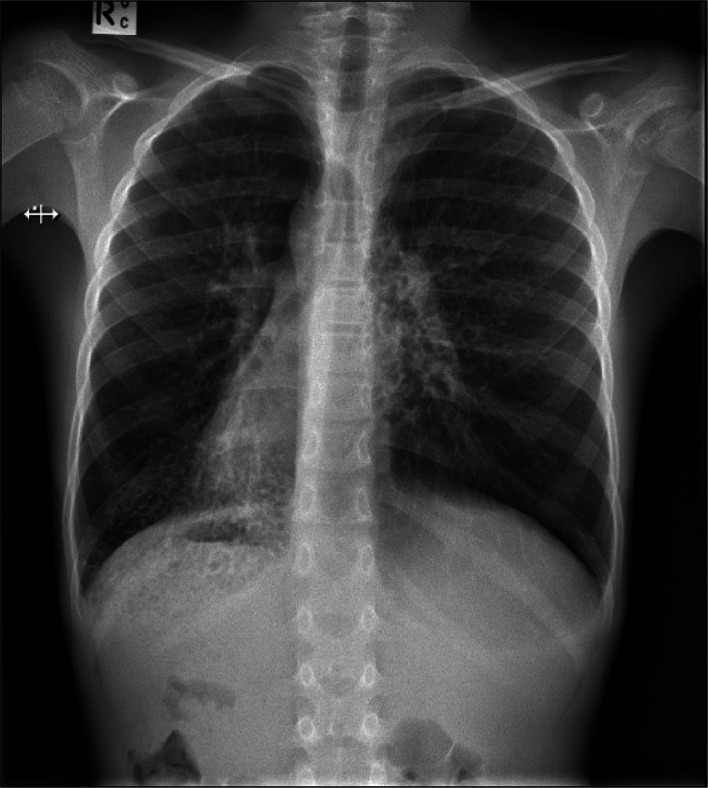
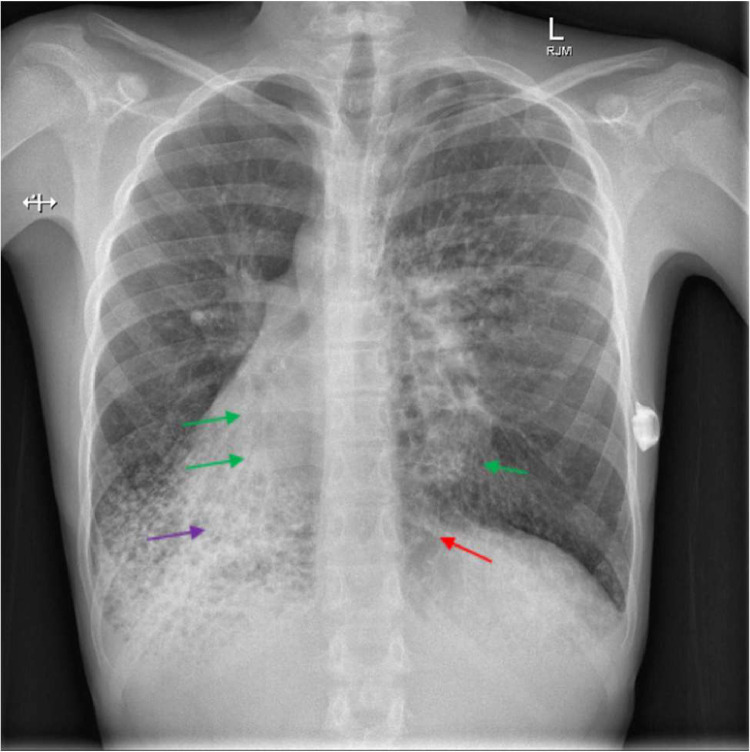
The initial radiographic assessment, utilizing a basic chest radiograph (CXR) (Fig. 1), prominently displays dextrocardia, evident from the heart's right-sided orientation and its base-apex axis directed towards the right [14]. Although in theory dextrocardia may be appreciated clinically (based on auscultation, palpation of the apex beat etc.) imaging is needed to confirm its presence. The positioning of the gastric bubble on the right side further indicates an unusual stomach placement, hinting at possible situs inversus.
Fig. 1.
Dextrocardia with right-sided orientation of heart (white arrow).
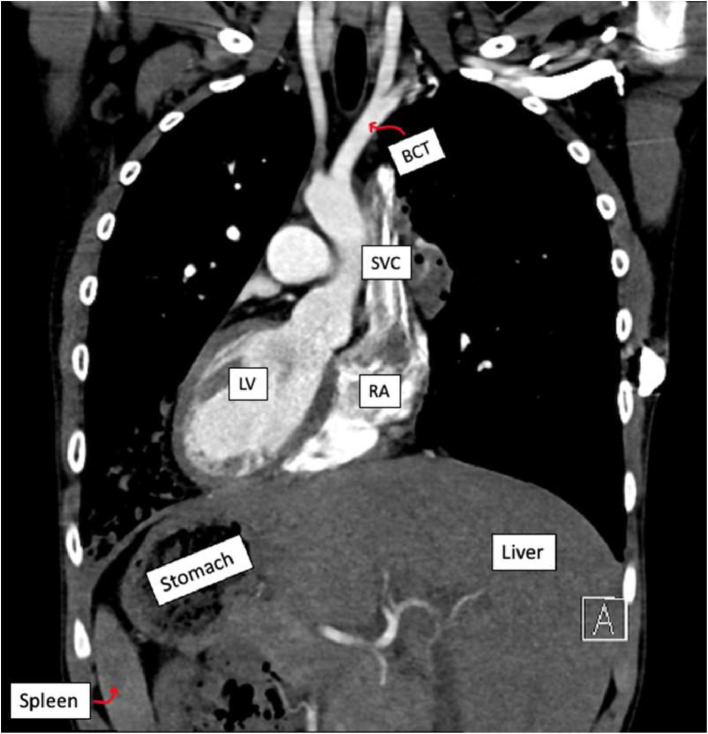
Subsequent examination via a coronal section CT (Fig. 2) confirms the right sided positioning of the stomach and demonstrates reversal of several other anatomical structures. In the abdomen, the spleen is situated on the right, while the liver is on the left. The superior vena cava (SVC) drains into the morphologically right atrium (RA) located on the left, and the aorta, originating from the morphologically left ventricle (LV) on the right, gives rise to the brachiocephalic trunk (BCT) as its first branch. The BCT bifurcates into the left (rather than right which is typical) common carotid and subclavian arteries. The right common carotid branch coming off distally from the aorta is also noted.
Fig. 2.
Coronal CT similarly demonstrating situs inversus (white arrow).
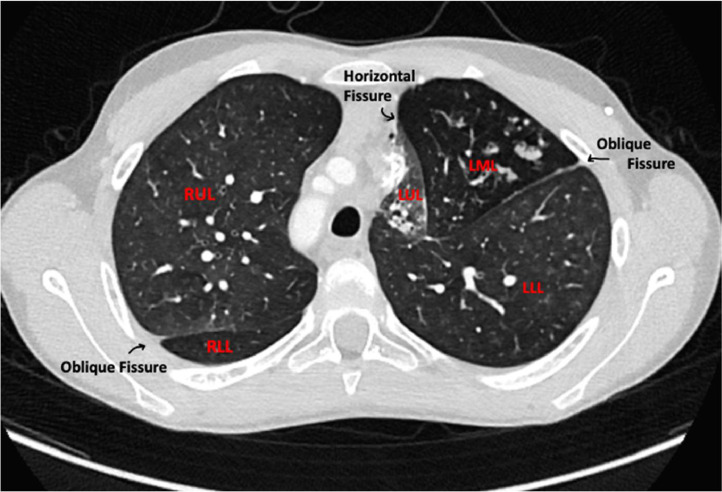
Analysis of the transverse slice (Fig. 3) reveals abnormal lung lobation. The patient has a bilobed right lung and a trilobed left lung. The right upper lobe (RUL) and right lower lobe (RLL) are demarcated by an oblique fissure, whereas the left upper lobe (LUL) and left middle lobe (LML) are separated by a horizontal fissure. Additionally, the LML and left lower lobe (LLL) are divided by another oblique fissure. This lobar arrangement is a mirror image of the standard lung structure. Ultimately, the reversal of all structures seen in the 2 CT scans substantiates the diagnosis of situs inversus totalis in this patient. This is distinct from heterotaxy, which can also be present in PCD, which is characterised by reversal of only some of the anatomical structures [15].
Fig. 3.
Axial CT chest demonstrating situs inversus in lungs with mirror image of normal lung structure.
Pectus excavatum
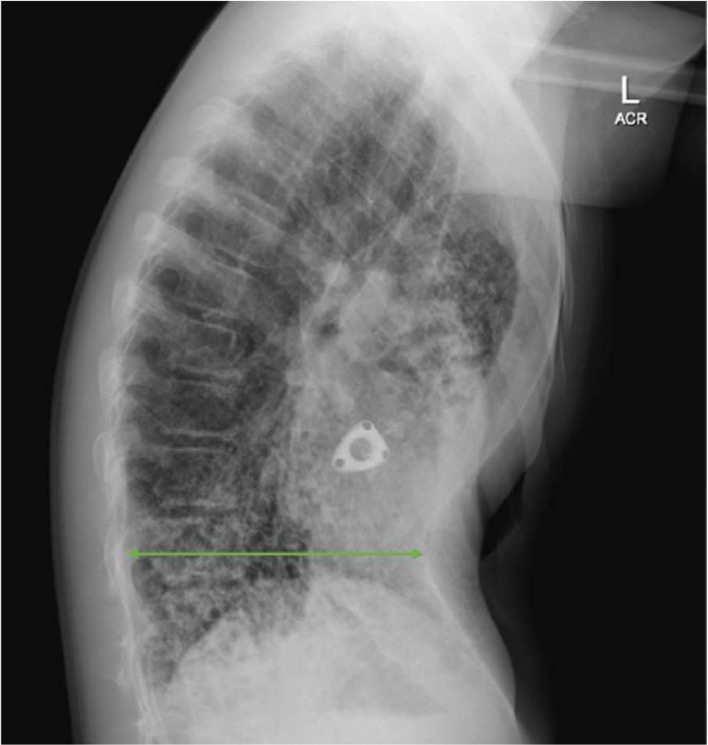
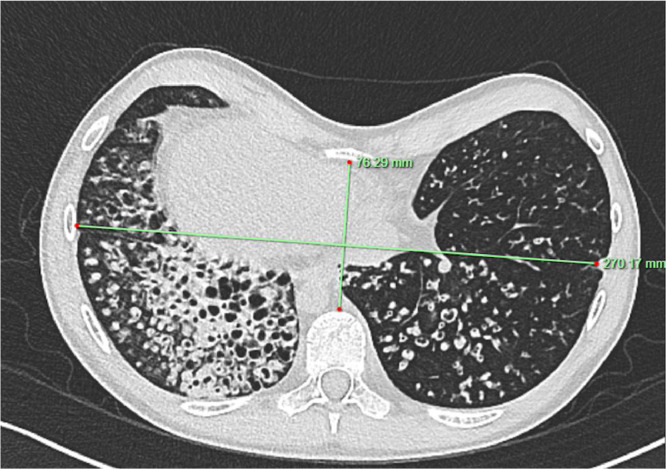
The patient's lateral chest X-ray (CXR) (Fig. 4) additionally reveals the presence of pectus excavatum, a congenital chest wall deformity. To assess the severity of this condition, we use the Haller Index, a quantitative measure derived by dividing the transverse (lateral) diameter of the rib cage by its anteroposterior (AP) diameter at the point of deepest concavity. These measurements can be seen on the patients CT below (Fig. 5). For this patient, this calculation results in a Haller Index of 3.55. A Haller Index exceeding 3.5 is generally indicative of severe pectus excavatum, and surgical intervention is typically considered for values of 3.25 or higher [16].
Fig. 4.
AP diameter of pectus deformity on sagittal view.
Fig. 5.
Calculation of Haller index with green lines demonstrating AP and lateral dimensions on axial view.
Pathological manifestations
Bronchiectasis
Impaired ciliary function in patients with Kartagener's syndrome leads to an increased susceptibility to lower respiratory tract infections. One of the primary complications arising from these chronic infections is bronchiectasis. Radiologically, bronchiectasis is defined by a persistent enlargement of the bronchial airways. Unlike normal bronchi, which taper as they extend towards the periphery of the lung, bronchi in bronchiectasis may result in a ‘tram-track’ appearance evident in scans aligned with the bronchi's course [17].
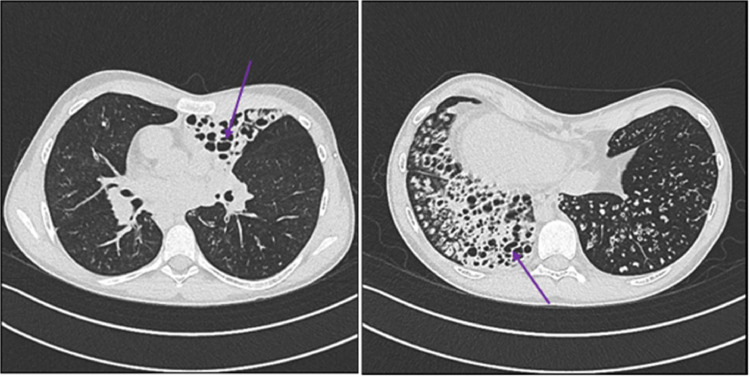
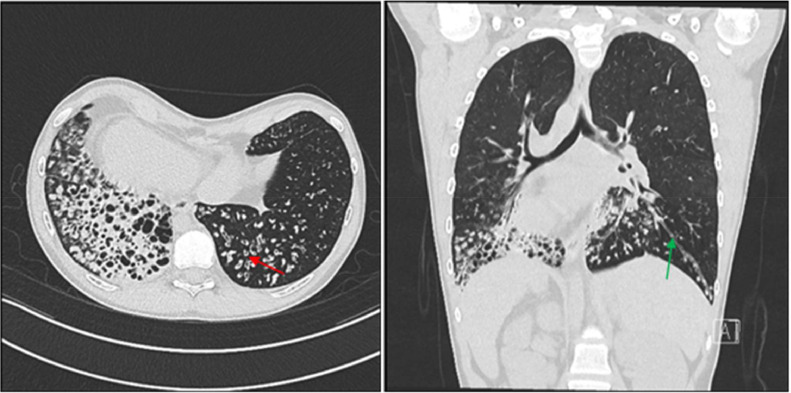
In cross-sectional imaging, the bronchi show significant dilation relative to the nearby pulmonary arteries, creating a 'signet ring' appearance [17]. In advanced stages, bronchiectasis can evolve into a saccular form (which may exhibit air-fluid levels within the bronchi), a condition referred to as cystic bronchiectasis. These radiological characteristics are exemplified in Fig. 6, Fig. 7, Fig. 8, where we have used color-coded arrows to highlight the specific features: green arrows indicate the 'tram-track' appearance, red arrows point to areas showing the 'signet ring' appearance, and purple arrows mark regions of cystic bronchiectasis. It is important to also observe the stark differences between the images in Figs. 1 and 6. A clear progression of the patient's bronchiectasis can be discerned, as Fig. 6 represents a more recent scan. This comparison underscores the advancing nature of bronchiectasis over time in this patient with Kartagener's syndrome.
Fig. 6.
Green marrow indicating tram track appearance. Red arrow indicating “signet-ring” appearance. Purple arrow showing areas of cystic bronchiectasis.
Fig. 7.
Areas of cystic bronchiectasis.
Fig. 8.
Red arrow demonstrates “Signet-ring” appearance and green arrow indicating tram track appearance of bronchiectasis.
In Fig. 7, it is particularly noteworthy that this patient exhibits distinct cystic bronchiectatic changes in the left upper lobe, an unusual manifestation. The upper lung lobes are generally less affected due to gravity-assisted mucociliary clearance, making them more resistant to infection and subsequent damage [10]. Therefore, in cases of Kartagener's syndrome, bronchiectasis predominantly affects the middle and lower lobes. In this case, the right middle and lower lobes and the base of the left lower lobe are also affected.
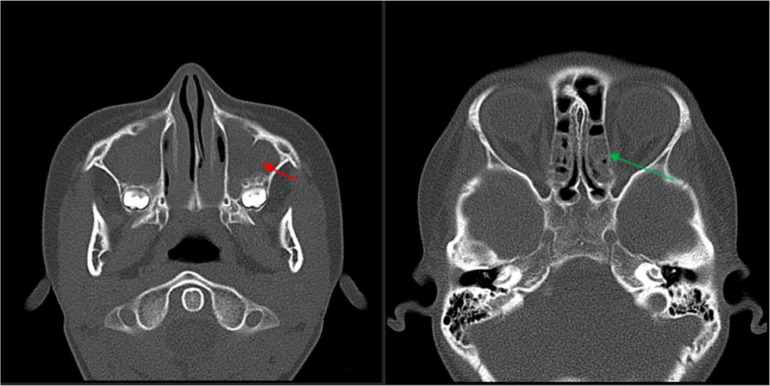
Chronic sinusitis
Impaired ciliary function also results in chronic sinusitis for patients with Kartageners which is identifiable on CT scans by mucosal thickening and blockage of the osteomeatal complex [9]. While additional findings such as thickened turbinates, opacified sinuses, and bony remodelling are observed, they are nonspecific and could indicate various conditions. The CT sinuses below (Fig. 9) demonstrate complete opacification of the maxillary sinuses (red arrow) and mucosal thickening of the posterior ethmoid (green arrow) sinuses.
Fig. 9.
Red arrow demonstrating opacification of the maxillary sinus. Green arrow demonstrating mucosal thickening of the posterior ethmoid sinus.
Discussion
The importance of medical imaging in the early diagnosis and management of Kartagener's syndrome is underscored in this case study, as it precisely identifies each element of the characteristic triad. The combination of radiological findings of the triad of situs inversus totalis, sinusitis, and bronchiectasis supports the diagnosis of Kartagener's syndrome in this patient. Situs inversus totalis was demonstrated by reversal of anatomical structures on both CXR and CT imaging. Sinusitis was seen in mucosal thickening and blockage of the osteomeatal complex on CT. Bronchiectasis was demonstrated by presence of ‘tram-track”, “signet-ring” appearance, and developing of cystic bronchiectasis in this patient.
Diagnostic criteria for Kartagener's syndrome encompass a history of repeated chest infections, bronchitis, and rhinitis since childhood, along with one or more of the following: situs inversus in the patient or a relative, non-motile spermatozoa, impaired transbronchial mucociliary clearance, or ciliary ultrastructural anomalies detectable through electron microscopy [18]. However, diagnosis is often delayed due to the prevalence of these symptoms in children. Nasal nitric oxide (NO) levels, while low in patients with PCD are not exclusively diagnostic, as similar reductions are seen in up to 40% of children, limiting their use to screening purposes [19].Invasive confirmatory tests like electron microscopy of nasal or tracheal biopsies are limited to specialized centers. Conversely, non-invasive imaging can readily reveal signs of situs inversus and other complications associated with Kartagener's syndrome, often sufficing for a diagnosis. This report aims to enhance the understanding and radiological detection of this rare disorder, emphasizing that early identification can significantly mitigate both short- and long-term morbidity by enabling prompt and effective management to preserve lung function. Furthermore, imaging plays a crucial role in prognosis, as evidenced by a study linking the severity of bronchiectasis inversely with FEV1 [10]. This is comparable to cystic fibrosis, where imaging is integral for tracking pulmonary exacerbations and guiding clinical studies, often revealing changes before they manifest in pulmonary function tests.
This case study presents some atypical findings not commonly associated with Kartagener's syndrome. Most notably, while bronchiectasis in Kartagener's syndrome predominantly affects the lower and middle lobes, our patient developed significant bronchiectasis in the left upper lobe (LUL). This is unusual, as one study indicated that the LUL is the least likely lobe to be affected in these patients, showing nearly half the prevalence found in the right upper lobe (RUL), which itself is relatively uncommon [18]. This anomaly could be attributed to anatomical differences; the bronchial opening of the LUL (corresponding to the RUL in a typical anatomy without situs inversus) is situated only 2 cm from the trachea/main carina, compared to the 5 cm distance of the RUL [20]. Consequently, the LUL is less prone to poor mucociliary clearance, reducing its susceptibility to infections and bronchiectasis. The presence of upper lobe bronchiectasis in a patient with Kartagener's syndrome is particularly significant since this pattern is more characteristic of cystic fibrosis [21]. Therefore, this case highlights the importance of not relying solely on this criterion to differentiate between the 2 conditions.
In this case, the patient displayed pectus excavatum, a congenital condition characterized by a recessed chest wall. Existing research suggests a potential link between Primary Ciliary Dyskinesia (PCD) and pectus excavatum, with a 9% occurrence rate in PCD patients [10], a figure markedly higher than the general incidence rate of approximately 0.25% [22]. These observations suggest that young patients who exhibit persistent respiratory symptoms and unusual physical features such as pectus excavatum might warrant a more thorough evaluation for Kartagener's syndrome. However, more extensive research is required to firmly establish this association.
Conclusion
In conclusion, this case study of an adolescent male with Kartagener's syndrome highlights the importance of recognizing atypical presentations in genetic disorders. The patient's unusual upper lobe bronchiectasis challenges conventional expectations and suggests a more complex interplay of symptoms in Kartagener's syndrome. This case underscores the vital role of medical imaging in diagnosing and managing such conditions, and points to the need for further research to better understand and treat the nuances of PCD and its variants
Patient consent
The author of this paper confirms that written and verbal, informed consent for publication has been obtained from the legal guardians of the patient.
Footnotes
Competing Interests: The authors have any conflicts of interest to disclose.
References
- 1.Peters R, de Jonge G. Kartagener's syndrome: situs inversus, chronic sinusitis and bronchiectasis. J Belg Soc Radiol. 2016;100(1):25. doi: 10.5334/jbr-btr.955. https://pubmed.ncbi.nlm.nih.gov/30038975/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson R, Boyton R. In: Encyclopedia of respiratory medicine. Laurent GJ, Shapiro SD, editors. Academic Press; United States: 2006. Bronchiectasis; pp. 259–268. [DOI] [Google Scholar]; ISBN 9780123708793. Available from https://www.sciencedirect.com/science/article/pii/B0123708796000478
- 3.Wilmott RW, Becker BA. In: Pediatric secrets. (Fifth Edition) Polin RA, Ditmar MF, editors. Mosby; United States: 2011. Chapter 17 - Pulmonology; pp. 648–678. [DOI] [Google Scholar]; ISBN 9780323065610. Available from https://www.sciencedirect.com/science/article/pii/B9780323065610000173
- 4.Garvey ML, Wilkes NC. In: Essence of anesthesia practice. (Third Edition) Fleisher LA, Roizen MF, editors. W.B. Saunders; United States: 2011. Kartagener’s Syndrome; p. 223. [DOI] [Google Scholar]; ISBN 9781437717204. Available from https://www.sciencedirect.com/science/article/pii/B9781437717204001965
- 5.Logan WD, Abbott OA, Hatcher CR. Kartagener's triad. Dis Chest. 1965;48(6):613–616. doi: 10.1378/chest.48.6.613. https://pubmed.ncbi.nlm.nih.gov/5295373/ Available from. [DOI] [PubMed] [Google Scholar]
- 6.Eitler K, Bibok A, Telkes G. Situs inversus totalis: a clinical review. Int J Gen Med. 2022;15:2437–2449. doi: 10.2147/IJGM.S295444. https://pubmed.ncbi.nlm.nih.gov/35264880/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schidlow DV, Steinfeld J. In: Pediatric pulmonology. Panitch H, Bell LM, editors. Mosby; United States: 2005. Chapter 8 - Primary Ciliary Dyskinesia (Immotile Cilia Syndrome—Kartagener Syndrome) pp. 131–139. [DOI] [Google Scholar]; ISBN 9780323019095. Available from https://www.sciencedirect.com/science/article/pii/B9780323019095500153
- 8.Afzelius BA. A human syndrome caused by immotile cilia. Science. 1976;193(4250):317–319. doi: 10.1126/science.1084576. https://pubmed.ncbi.nlm.nih.gov/1084576/ Available from. [DOI] [PubMed] [Google Scholar]
- 9.Tuladhar AS, Bhattarai A, Bimali S, Pokharel B, Pradhan S, Shrestha A, et al. Sinusitis among patients undergoing CT scan of paranasal sinuses in a tertiary care centre: a descriptive cross-sectional study. JNMA J Nepal Med Assoc. 2022;60(254):857–860. doi: 10.31729/jnma.7595. https://pubmed.ncbi.nlm.nih.gov/36705160/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kennedy MP, Noone PG, Leigh MW, Zariwala MA, Minnix SL, Knowles MR, et al. High-resolution CT of patients with primary ciliary dyskinesia. AJR Am J Roentgenol. 2007;188(5):1232–1238. doi: 10.2214/AJR.06.0965. https://pubmed.ncbi.nlm.nih.gov/17449765/ Available from. [DOI] [PubMed] [Google Scholar]
- 11.Mandal P, Sidhu MK, Kope L, Pollock W, Stevenson LM, Pentland JL, et al. A pilot study of pulmonary rehabilitation and chest physiotherapy versus chest physiotherapy alone in bronchiectasis. Respir Med. 2012;106(12):1647–1654. doi: 10.1016/j.rmed.2012.08.004. https://pubmed.ncbi.nlm.nih.gov/22947443/ Available from. [DOI] [PubMed] [Google Scholar]
- 12.Wilkinson M, Sugumar K, Milan SJ, Hart A, Crockett A, Crossingham I. Mucolytics for bronchiectasis. Cochrane Database Syst Rev. 2014;2014(5) doi: 10.1002/14651858.CD001289.pub2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6513404/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang X, Zou J, Liu S. Endoscopic sinus surgery for treatment of kartagener syndrome: a case report. Balkan Med J. 2013;30(2):244–247. doi: 10.5152/balkanmedj.2013.8152. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4115961/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evans WN, Acherman RJ, Collazos JC, Castillo WJ, Rollins RC, Kip KT, et al. Dextrocardia: practical clinical points and comments on terminology. Pediatr Cardiol. 2010;31(1):1–6. doi: 10.1007/s00246-009-9516-0. https://pubmed.ncbi.nlm.nih.gov/19727926/ Available from. [DOI] [PubMed] [Google Scholar]
- 15.Radiopaedia. Heterotaxy syndrome. Available from: https://radiopaedia.org/articles/heterotaxy-syndrome.
- 16.Radiopaedia. Haller index. Available from: https://radiopaedia.org/articles/haller-index.
- 17.Yudin A. Signet ring sign, tram-tracking sign (tram lines), string of pearls (string of cysts), and cluster of grapes (cluster of cysts). In: Metaphorical signs in computed tomography of chest and abdomen. 2023 pp. 59-60. doi: 10.1007/978-3-031-24494-0_30. Available from: https://www.researchgate.net/publication/370201337_Signet_Ring_Sign_Tram-Tracking_Sign_Tram_Lines_String_of_Pearls_String_of_Cysts_and_Cluster_of_Grapes_Cluster_of_Cysts.
- 18.Mishra M, Kumar N, Jaiswal A, Verma AK, Kant S. Kartagener's syndrome: a case series. Lung India. 2012;29(4):366–369. doi: 10.4103/0970-2113.102831. https://pubmed.ncbi.nlm.nih.gov/23243352/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collins SA, Walker WT, Lucas JS. Genetic testing in the diagnosis of primary ciliary dyskinesia: state-of-the-art and future perspectives. J Clin Med. 2014;3(2):491–503. doi: 10.3390/jcm3020491. https://pubmed.ncbi.nlm.nih.gov/26237387/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah SB, Chawla R, Hariharan U, Shukla S. An algorithm for difficult double lumen tube placement and troubleshooting a malpositioned double lumen tube harnessing A, B, Cs of lung isolation. Indian J Anaesth. 2022;66(Suppl 6):S328–S332. doi: 10.4103/ija.ija_318_22. https://pubmed.ncbi.nlm.nih.gov/36425911/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sahu S, Ranganatha R, Batura U, Choubey U, Ragasri Meghana D, Menon VR, et al. A case of unusual presentation of kartagener's syndrome in a 22-year-old female patient. Cureus. 2022;14(8):e28119. doi: 10.7759/cureus.28119. https://pubmed.ncbi.nlm.nih.gov/36134054/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Scalise PN, Demehri FR. The management of pectus excavatum in pediatric patients: a narrative review. Transl Pediatr. 2023;12(2):208–220. doi: 10.21037/tp-22-361. https://pubmed.ncbi.nlm.nih.gov/36891368/ Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]