Abstract
High blood pressure (BP) is the leading cause of cardiovascular disease in Uganda accounting for more than 50% of cardiovascular related deaths each year. In Uganda, more than 25% of adults have high BP with lack of awareness being the main barrier to achieving satisfactory control rates. May measurement month (MMM) is a global initiative aimed at raising awareness of high BP and to act as a temporary solution to the lack of BP screening programmes. A cross-sectional survey of voluntary screenees aged 18 years and above was carried out between May and September 2021. Screening was carried out in two outpatient departments of two referral hospitals within the capital city, Kampala. BP measurements, the definition of hypertension and statistical analysis followed the standard MMM protocol. A total of 1671 people were screened and included in analysis. After multiple imputation, 1018 (60.9%) had hypertension. Of all 1018 participants with hypertension, 765 (75.1%) were aware and 750 (69.3%) were on antihypertensive medicine. Of the participants on antihypertensive medicine, 248 (35.2%) had controlled BP (<140/90 mmHg). Previous history of stroke and taking alcohol 1–6 times per week were significantly associated with higher diastolic BP. The MMM21 Uganda campaign highlights the importance of measuring BP as it generates real-time data on untreated and inadequately treated hypertension. This should motivate government and policy makers to promote routine local screening for BP.
Keywords: Hypertension, Blood pressure, Screening, Treatment, Control
Introduction
Hypertension is a major worldwide problem. The global prevalence of hypertension has increased over the past few decades especially in the low- and middle-income countries.1 In Uganda, the prevalence of hypertension was estimated to be between 24% and 28.5% in urban communities.2 In 2014, 24.3% (3.9 million) of the adult population in Uganda had hypertension. Of the 3.9 million hypertensive patients, only 16.8% were aware of the diagnosis, 6.9% were on treatment, and only 2.3% were well controlled. A large private hospital in Uganda documented a prevalence of hypertension of 41.6% among screened patients, 39.4% of patients with hypertension received medication at least once.2 Overall, 18.3% of patients achieved control.3 Strategies are therefore needed to increase the prevention, detection, awareness, treatment, and control of hypertension in sub–Saharan Africa in general and in Uganda in particular. The WHO has set the following recommendations: to address population prevalence and control of hypertension through reducing modifiable risk factors, improving and expanding identification and treatment of people with hypertension, treatment intensification for patients whose BP is not controlled, ensuring access to medicines, tracking BP control rates in clinical settings, and measuring population prevalence.
May Measurement Month (MMM) was launched in 2017 by the International Society of hypertension (ISH) as a global initiative aimed at raising awareness and facilitating opportunistic screening for hypertension worldwide. Here, we provide the relevant results of the MMM21 campaign for Uganda.
Methods
The study was coordinated by the cardiology team at Kiruddu National Referral Hospital in Uganda. Two sites from the capital city of Kampala participated in Uganda: St Francis Hospital, Nsambya and Kiruddu Hospital. The screening sites conducted training using the training materials supplied by MMM. OMRON M2 Intelli IT blood pressure monitors and T-shirts were also supplied by MMM.
We conducted a cross-sectional survey between May and September 2021 among volunteers aged 18 years and above using convenience sampling. The campaign was advertised through various media and screening stations were set up in outpatient departments of the participating hospitals. This occurred most of the days of the month. Blood pressure was measured after at least 5 min of rest. Hypertension was defined as a systolic BP ≥ 140 mmHg or a diastolic BP of ≥90 mmHg (based on the mean of the second and third of three consecutive BP readings) or in those on treatment for BP. In the small number (21) of participants who did not have all three readings, multiple imputation was performed to impute the mean of the second and third BP readings, based on the global data and as described previously.4 Research ethics approval was sought from Clarke International University REC No. CLARKE-2023-609. The BP measurement, definition of hypertension, and statistical analysis followed the standard MMM protocol.
Results
We screened a total of 1671 individuals. The mean age was 48.3 (SD 15.9) years, and 1050 (62.8%) were female. The main ethnicity of those screened was Black (98.7%), 167 (10.0%) had diabetes, 49 (2.9%) had a history of myocardial infarction, and 58 (3.5%) had a history of stroke. 2.8% of participants were current smokers and 80.1% drank alcohol rarely or never. 6.7% of women screened were pregnant. 174 (10.4%) participants were taking aspirin, and 140 (8.4%) were taking statins. A total of 79 (4.7%) participants reported having previously tested positive for COVID-19 and 383 (22.9%) had received one or more COVID-19 vaccinations. When asked if COVID-19 affected their BP treatment, 98.1% answered ‘No’.
After multiple imputation, of all 1671 participants, 1018 (60.9%) had hypertension, of whom 765 (75.1%) were aware and 750 (69.3%) were on antihypertensive medication. Of the participants on antihypertensive medication, 248 (35.2%) had controlled BP (Table 1).
Table 1.
Total participants and proportions with hypertension, awareness, on medication, and with controlled blood pressure
| Total participants | Number (%) with hypertension | Number (%) of hypertensives aware | Number (%) of hypertensives on medication | Number (%) of those on medication with controlled BP | Number (%) of all hypertensives with controlled BP |
|---|---|---|---|---|---|
| 1671 | 1018 (60.9%) | 765 (75.1%) | 705 (69.3%) | 248 (35.2%) | 248 (24.4%) |
After adjustment for age and sex, treated hypertensive participants had significantly lower systolic BP than those who were untreated (9.0 mmHg lower; P = 0.009). Adjusting for age, sex, and antihypertensive treatment, previous history of stroke and taking alcohol 1–6 times per week were significantly associated with higher diastolic BP (3.9 and 5.7 mmHg, P = 0.033 and P = 0.016, respectively).
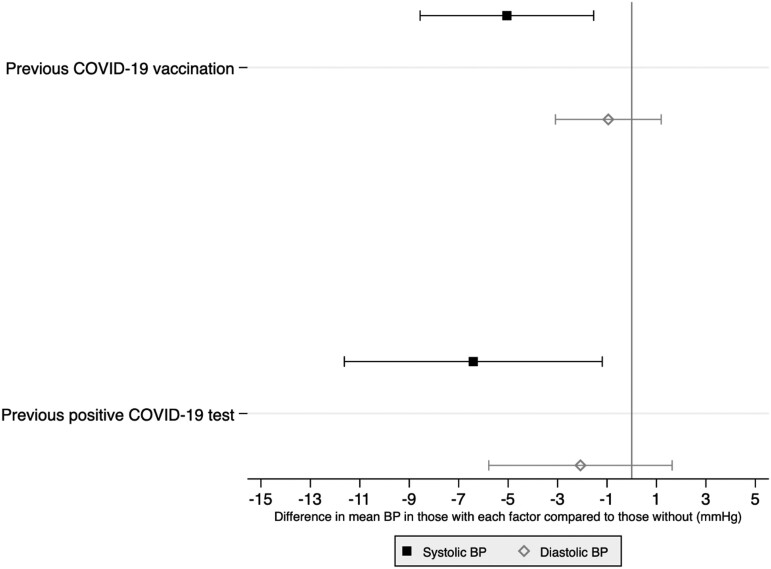
In contrast, a significantly lower systolic BP was observed in participants with history of positive COVID-19 test or received at least one dose of COVID-19 vaccine (Figure 1). No association was found between BP levels and diabetes, history of myocardial infarction, pregnancy and smoking.
Figure 1.
Difference in mean blood pressure according to history of COVID-19 infection and vaccination from linear mixed model adjusted for age, sex and, antihypertensive medication.
Discussion
In this hypertension screening activity, 60.9% of participants were found to be hypertensive. This prevalence is much higher than the global data,5 other African countries6,7 and previous Uganda population based surveys.1 Potential explanations may include convenience sampling in a hospital setting, with potential bias towards unhealthier and possibly more stressed individuals compared to the general community. Despite the hospital setting, 24.9% of those with hypertension were not aware of their BP status and only 35.2% of those taking antihypertensive medication were having good BP control. This low awareness and low level of controlled hypertension, compared to the global data (61.9%)5 and Sub-African data (49%), calls for enhanced efforts in hypertension awareness and control in the community. The linear regression showed participants taking antihypertensive medication had significantly lower BP than those untreated. This result is in contrast to global5 and other African data5,6 possibly due to the small sample size and hospital-based setting. Our MMM data suggest an absence of any significant increase in BP due to COVID-19, although some studies have suggested a trend of both post COVID-19 hypertension8,9 and increased BP following vaccination.10,11 The relationship between COVID-19 infection or vaccination and risk of cardiovascular disease remains uncertain and requires further investigation. Our study could have been limited by selection bias due to the hospital setting and the convenience sampling used. Nevertheless, despite the limitations and challenges, the Ugandan MMM21 campaign highlights the potential and importance of opportunistic screening for hypertension and generates much needed data on the scale of untreated and inadequately treated hypertension as a public health issue. There is urgent need to sensitize communities to the burden and effects of hypertension and to enhance screening and control of hypertension, to reduce the global burden of disease associated with raised BP.
Acknowledgements
We are grateful to the MMM21 Ugandan volunteers, Ugandan cardiologists/doctors and staff from the participating hospitals, the participants, leadership of Kiruddu National Referral Hospital, and other partners who supported this project in Uganda. Kiruddu National Referral Hospital provided funds for regulatory approvals fees and stipend for the data entry assistant.
Contributor Information
Zhang Wanzhu, Uganda Heart Institute, Mulago Hospital, Kampala, Uganda.
Pauline Byakika-Kibwika, Department of Medicine, Makerere University College of Health Sciences, Plot No. 1, Upper Mulago Hill Road, P.O. Box 7072, Kampala, Uganda.
Prossie Ingabire, Department of Medicine, St. Francis Hospital, Nsambya, Kampala, Uganda; Department of Medicine, China-Uganda Friendship Hospital Naguru, Kampala, Uganda.
Stella Nabirye, Department of Medicine, Kiruddu National Referral Hospital, Salaama Road, P.O. Box 6588, Kampala, Uganda.
Thomas Beaney, Imperial Clinical Trials Unit, Imperial College London, Stadium House, 68 Wood Lane, London W12 7RH, UK; Department of Primary Care and Public Health, Imperial College London, St Dunstan’s Road, London W6 8RP, UK.
Carolina Janssen-Telders, Imperial Clinical Trials Unit, Imperial College London, Stadium House, 68 Wood Lane, London W12 7RH, UK; Department of Cardiology, Amsterdam UMC location Vrije Universiteit Amsterdam, De Boelenlaan 1117, Amsterdam, The Netherlands.
Neil R Poulter, Imperial Clinical Trials Unit, Imperial College London, Stadium House, 68 Wood Lane, London W12 7RH, UK.
Charles Kiiza Mondo, Department of Medicine, Makerere University College of Health Sciences, Plot No. 1, Upper Mulago Hill Road, P.O. Box 7072, Kampala, Uganda; Department of Medicine, Kiruddu National Referral Hospital, Salaama Road, P.O. Box 6588, Kampala, Uganda.
Funding
MMM provided a modest reimbursement fee for the volunteers and in kind provision of blood pressure machines.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
- 1. Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol 2021;18:785–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guwatudde D, Mutungi G, Wesonga R, Kajjura R, Kasule H, Muwonge J et al. The epidemiology of hypertension in Uganda: findings from the national non-communicable diseases RiskFactor survey. PLoS One 2015;10:e0138991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Majumdar U, Clarke N, MoranAE R, Doupe P, Gadikota-Klumpers DD, Gidio A et al. Hypertension screening, prevalence, treatment, and control at a large private hospital in Kampala, Uganda: a retrospective analysis. PLOS Glob Public Health 2022;2:e0000386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beaney T, Wang W, Schlaich MP, Schutte AE, Stergiou GS, Alcocer L et al. Global blood pressure screening during the COVID-19 pandemic: results from the May Measurement Month 2021 campaign. J Hyperten 2023;41:1446–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Beaney T, Schutte AE, Tomaszewski M, Ariti C, Burrell LM, Castillo RR et al. May measurement month 2017: an analysis of blood pressure screening results worldwide. Lancet Global Health 2018;6:e736–e743. [DOI] [PubMed] [Google Scholar]
- 6. Ellenga-Mbolla B, Makani-Bassakouahou J, Landa CK, Monabeka MG, Ossou-Nguiet PM, Ngamami SM et al. May Measurement Month 2019: an analysis of blood pressure screening results from Republic of the Congo. Eur Heart J Suppl 2021;23:B49–b51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ogola EN, Barasa F, Barasa AL, Gitura BM, Njunguna B, Beaney T et al. May measurement month 2017: the results of blood pressure screening of 14 845 individuals in Kenya-Sub-Saharan Africa. Eur Heart J Suppl 2019;21:D71–Dd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Delalić Đ, Jug J, Prkačin I. Arterial hypertension following COVID-19: a retrospective study of patients in a central European tertiary care center. Acta Clin Croat 2022;61:23–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Akpek M. Does COVID-19 cause hypertension? Angiology 2022;73:682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Simonini M, Scarale MG, Tunesi F, Manunta P, Lanzani C. COVID-19 vaccines effect on blood pressure. Eur J Intern Med 2022;105:109–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sanidas E, Papadopoulos D, Anastasiou T, Velliou M, Michalaki E, Fotsali A et al. Short-term blood pressure alterations after COVID-19 vaccination. J Hypertens 2022;40:e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.