Abstract
Background
Inequalities in immigrants' oral health are often masked in population-level data. Therefore, this paper was planned to assess the prevalence data on oral health diseases, namely dental caries, and periodontitis, among immigrants worldwide.
Methods
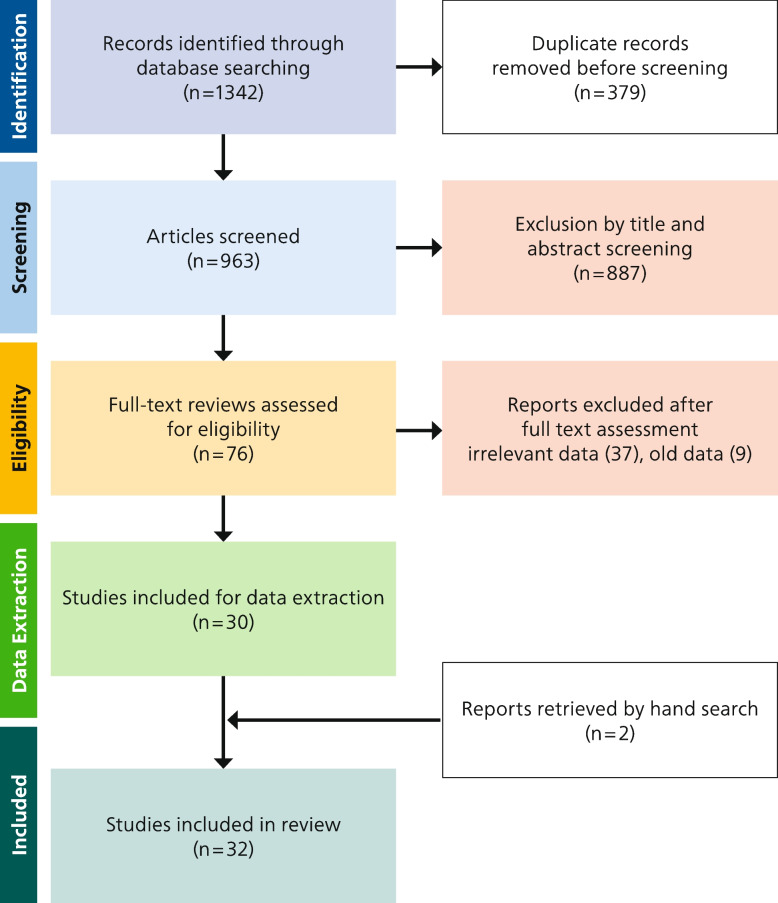
Following a systematic search in Scopus, Embase, and PubMed for studies published between 2011 and 2023, 1342 records were identified. Following title and abstract screening, 76 studies remained for full-text eligibility-screening based on predefined inclusion criteria. Thirty-two studies were included in the review.
Results
Dental caries figures were higher in immigrant populations compared to the local population, regardless of host countries, age, gender, or nationality. In children, the overall mean and standard deviation (SD) for decayed, missing, and filled teeth in the primary dentition (d3mft) was 3.63(2.47), and for D3MFT (permanent dentition), it was 1.7(1.2).
Upon comparing overall mean caries counts in children and adults with their control groups in the included studies, untreated dental caries (D3T and d3t) constituted the dominant share of caries experience (D3MFT and d3mft) in immigrant children. For the local population, the highest proportion of caries experience was attributed to filled teeth (FT and ft).
Dentin caries prevalence among immigrants ranged from 22% to 88.7% in the primary dentition and 5.6% to 90.9% in the permanent dentition. Gingivitis ranged from 5.1% to 100%. Oral health varied greatly between studies. Regarding oral health accessibility, 52% to 88% of immigrant children had never been to a dentist, suggesting a very limited level of accessibility to dental health services.
Conclusion
It is imperative to develop interventions and policies that have been customized to address the oral health disparities experienced by immigrant populations. Additionally, host countries should actively implement measures aimed at enhancing the accessibility of oral health care services for these individuals. The utilization of available data is crucial in establishing a hierarchy of objectives aimed at enhancing the oral health of immigrant populations.
Trial registration
The Scoping review protocol was registered at OSF Registries with registration number (https://doi.org/10.17605/OSF.IO/MYXS4).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-024-19354-4.
Keywords: Global burden of oral disease, Emigrants and Immigrants, Oral health, Dental caries, Periodontal diseases, Gingivitis, DMFT, Dmft, Caries lesion
Introduction
In recent years, international migration has dramatically increased, becoming a significant worldwide phenomenon. According to the World Migration Report, there were 281 million international migrants in 2020 globally, an increase of 60 million from 2010. This number includes individuals of all ages who have crossed international borders to reside in countries other than their birthplace [1].
The health and oral health of immigrants may be adversely affected by a number of challenges, such as linguistic and cultural barriers, socioeconomic changes, limited access to healthcare facilities, lack of medical and dental insurance, and loss of social networks [2, 3]. These challenges can often result in poor oral health outcomes among immigrant populations. In this context, the prevalence of oral health problems is expected to be high among immigrants [4]. However, data on the extent of oral health issues and research to inform policymakers about the oral health needs of immigrants are still very limited [5]. There is an urgent need to study oral health in this population due to the growing number of immigrants.
Oral health is an important component of overall health and well-being; however, it is often overlooked in public health discussions. Oral diseases (i.e., dental caries and periodontitis) contribute significantly to the global burden of chronic disease [6, 7]. These oral health conditions can cause significant pain, discomfort, tooth loss, malnutrition, and impair a person's ability to eat, communicate, and smile confidently [8, 9]. These conditions can have adverse impacts on a person's overall health and quality of life [10]. Furthermore, untreated dental caries and periodontal disease can be involved in more serious health complications, such as cardiovascular disease, respiratory infections, and even diabetes [11, 12].
With the increasing globalization and migration of people, it is important to understand the prevalence and risk factors of dental caries and periodontal problems among immigrant populations worldwide. Research has also shown that the prevalence of these oral health diseases in immigrant populations varies depending on their country of origin, level of acculturation, and length of stay in the host country [13, 14].
In summary, oral health diseases are among the most neglected aspects of health, regardless of location, culture, education, or economic standing, and particularly in low- and middle-income countries. Thus, gaining a holistic overview of the prevalence of oral health problems among immigrants might assist policymakers in defining treatment needs and treatment strategies as well as the best ways to adapt them to the health systems of the host countries. Furthermore, oral health disparities between immigrants and non-immigrants can exacerbate existing health inequities and contribute to broader health disparities.
In a previous paper, dental caries and periodontal issues in refugees were described and discussed [15]. In the present review, the focus was put on immigrant populations and compare their data with those of local population of the host country. An immigrant is someone who voluntarily relocates to a different country, whereas a refugee is an individual who is compelled to leave the country of origin.
To the best of authors’ knowledge, this is the first review that addresses dental caries and periodontal problems in the immigrant populations on a global quantitative scale. The main goals were to synthesize the evidence of the prevalence of dental caries among immigrants using the Decayed Missing and Filled index (D3MFT/d3mft) and to evaluate the prevalence of periodontal disease. Further, the dental care services provided to immigrants and their needs and deficiencies were appraised.
Materials and methods
The Scoping review protocol was registered at OSF Registries with registration number (10.17605/OSF.IO/MYXS4). The review was completed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement [16].
Research question and search strategy
What is the prevalence of dental caries and periodontal diseases among immigrants worldwide, and is this higher than those of the general population of the host country?
The research question for this scoping review was outlined based on sample, phenomenon of interest, design, evaluation, and research type (SPIDER) [17] tool. Three electronic databases, Scopus, Embase, and PubMed were searched using the following search strategy. Search strings were created using the keywords and synonyms in conjunction with the Boolean operators "AND" and "OR". In addition to electronic database searches, a comprehensive hand search was conducted to ensure that relevant literature was included in the review. An example of a search string used for PubMed is included here, and the others can be found in Appendix (page 2).
S (Sample): (("Emigrants AND Immigrants"[MeSH Terms] OR "Undocumented Immigrants"[MeSH Terms] OR ("Refugees"[MeSH Terms] OR "Refugee Camps"[MeSH Terms]) OR "Ethnicity"[MeSH Terms] OR "Ethnic and Racial Minorities"[MeSH Terms] OR "asylum seeker*"[Title/Abstract] OR "displaced person*"[Title/Abstract] OR "refugee*"[Title/Abstract]).
P (Phenomenon) of I (Interest): All the articles that related to either dental caries or periodontal problems.
D (Design): not restricted.
E (Evaluation): (("Dental Caries"[MeSH Terms] OR "Root Caries"[MeSH Terms] OR "Dental Caries Susceptibility"[MeSH Terms] OR "Periodontal Pocket"[MeSH Terms] OR "Periodontal Index"[MeSH Terms] OR "Gingivitis"[MeSH Terms] OR "DMF Index"[MeSH Terms] OR "dmf index*"[Title/Abstract] OR "dental decay*"[Title/Abstract] OR "carious lesion*"[Title/Abstract] OR "Carious white spot*"[Title/Abstract] OR "periodontal pocket*"[Title/Abstract] OR "dmft s*"[Title/Abstract] OR "gingival index*"[Title/Abstract] OR "dmft*"[Title/Abstract] OR "dmft index*"[Title/Abstract] OR "bleeding on probing*"[Title/Abstract] OR "probing pocket depth*"[Title/Abstract] OR "clinical attachment loss*"[Title/Abstract]).
R (Research type): not restricted.
Eligibility criteria
This scoping review included all quantitative and qualitative studies on dental caries or periodontal problems of immigrant populations of any age published from 2011 to August 2023. This timeframe was selected specifically to ensure the review is current and relevant. The review was conducted as part of a Ph.D. project addressing oral health disparities in marginalized communities. Therefore, the search population included terms like refugees and ethnic minorities, while the present review focused only on the immigrant population.
Studies with insufficient oral health data about dental caries or periodontal disease, as well as those involving refugees, asylum seekers, ethnic minorities, or indigenous populations, were excluded. Non-peer-reviewed papers and unpublished research (e.g., theses, abstracts, and preprints) were excluded. Only papers published in English, Italian, German, and French were considered.
Study selection
The selection was conducted using structured procedures. After removing duplicates, the titles and abstracts of search results were examined by two independent reviewers (SABR, AM) to determine their relevance and whether they matched the planned inclusion criteria. Any uncertainties regarding the inclusion of a study were discussed with a third reviewer (GC).
Risk of bias
After excluding ineligible papers, two independent reviewers (SABR, AM) critically rated all eligible full texts using critical appraisal instruments for prevalence studies in the Joanna Briggs Institute (JBI) System for the Unified Management of the Assessment and Review of Information (SUMARI) software (Joanna Briggs Institute, Adelaide, Australia) (appendix page 3). There were nine questions to which the answers were "yes," "no," and "unclear." Uncertainties were resolved through discussion or the assistance of a third reviewer (GC).
Data extraction and data synthesis
One author (SABR) extracted the data using an ad hoc designed excel file for data collection, which was then checked by a second author (GC).
The following information was provided on the data extraction form:
Study characteristics: first author's last name, year of publication, journal, country of study, study design, sampling procedures, calculation of sample size, and methods of data collection
Participant characteristics and outcome measure: number of participants, sex, age, prevalence of dental caries and periodontal problems, oral health accessibility, and some other findings from the original papers.
Parameters measured in the review
In line with the WHO methodology [18], the decayed (d3/D3), missing (m/M), and filled (f/F) teeth (d3mft/D3MFT) index score (e.g. DMF, DMFT, dmft, DMFS, deft, dft) was applied to evaluate oral health status [19]. Where this index is reported in this review, it refers to caries measured at the dentinal caries threshold (D3MF/d3mf) and excludes enamel caries, unless otherwise specified [20]. As we aimed to report on caries prevalence comprehensively, we included studies that utilized both WHO and ICDAS criteria. The D3/d3 level, representing caries lesions in dentine (open and closed), was chosen as a common metric. We acknowledged the differences in diagnostic thresholds between the WHO criteria, which typically focus on cavitated lesions, and the ICDAS criteria, which offer a more detailed assessment of caries progression, including non-cavitated stages. By reporting on both indices, we aimed to present a more complete picture of caries prevalence as reported in the included studies.
The mean and standard deviation (SD) of the prevalence of dental caries and range were calculated where relevant. Studies with prevalence (% d3mft/D3MFT > 0) or caries count (mean d3mft/D3MFT) data on either primary or permanent dentition or periodontal problems (e.g., gingivitis, periodontitis) were taken into consideration.
Periodontal health in children and adults was evaluated using criteria such as gingivitis (Gingival Index and Community Periodontal Index), clinical attachment loss, periodontal pocket depth, bleeding on probing, and radiographic bone loss if reported by the included studies.
Results
Study selection
The initial search with the keywords resulted in 928 papers in Scopus, 116 results in Embase, and 298 results in PubMed (Fig. 1). The authors (SABR and AM) screened the studies by title after the removal of duplicates (n = 379). After the title and abstract screening, 76 studies were left for full-text screening. Data extraction was then performed on 30 articles that met the inclusion criteria. In addition, two papers [21, 22] were retrieved by hand search, so overall 32 studies were included. The studies excluded after the full-text review are listed in appendix (page 4). The list of the included studies sorted by country of study is reported in Table 1.
Fig. 1.
PRISMA flow diagram of study selection
Table 1.
List of all included papers in the review ordered alphabetically by country where the study was conducted
| Year of study | Study type | Country of study | Country of origin of study participants |
Participants (n) |
Age Range (years) |
|
|---|---|---|---|---|---|---|
| Christian B et al., [23] | 2012 | exploratory trial | Australia | Iraq, Pakistan, and Lebanon | 625 | 1–4 |
| Gibbs et al., [24] | 2012 | Cross-sectional | Australia | Iraq, Pakistan, and Lebanon | 630 | 1–4 |
| Hoover et al., [25] | 2012 | Pilot Study | Canada | The Indian subcontinent, other parts of Asia, and the rest of the world | 133 | 3–15 |
| Amin et al., [26] | 2013 | Cross-sectional | Canada | Africa | 125 | 1.7–6 |
| Elyasi et al., [27] | 2015 | Cross-sectional | Canada | South Asia, East Asia, Africa,and East Europe | 274 | 1–12 |
| Dahlan et al., [28] | 2017 | Cross-sectional | Canada | South Asia, South East and East Asia, Arabs, Africans, East Europeans, and Hispanics | 336 | 2–12 |
| Azrak et al., [29] | 2017 | Cross-sectional | Canada | Africa, Eastern Mediterranean, and South East Asia | 211 | 1–5.9 |
| Liu et al., [30] | 2012 | Cross-sectional: | China | NR | 1323 | 7–12 |
| Zhang et al., [31] | 2013 | Cross-sectional | China | NR | 10,150 | 5–15 |
| Mattila et al., [32] | 2012 | pilot study | Finland | Iraq, Afghanistan, Iran, Russia, Thailand, Somalia, Turkey, Hungary, Slovakia, China, Vietnam, South Sudan, Syria, Sweden and Morocco | 38 | 18–53 |
| Aarabi et al., [33] | 2012 | Cross-sectional | Germany | Austria, Croatia, Italy, Turkey, Iran, Tunisia, Vietnam, Israel, Poland, Russia and Jamaica | 112 | 60+ |
| Pavlopoulou et al., [21] | 2010 | Cross-sectional: | Greece | Albania,Meldova,Egypt,Afghanistan, Bangladesh, India, Iran, Kenya, Lebanon, Pakistan, Ukraine,China | 300 | 1–14 |
| Diamanti et al., [34] | 2013 | Cross-sectional | Greece | Mostly Albania,Eastern European countries (such as Georgia, Romania, Bulgaria and Russia) | 4409 | 5–15 |
| Sivakumar et al., [35] | 2016 | Cross-sectional | India | Tibet | 865 | 11–13 |
| Ferrazzano et al., [36] | 2014 | Retrospective Study | Italy | NR | 553 | 12–14 |
| Campus et al., [37] | 2017 | Cross-sectional | Italy | NR | 6,825 | 3–4 |
| Hashizume et al., [38] | 2011 | Cross-sectional | Japan | Brazil | 378 | 6–14 |
| Lee et al., [39] | 2016 | Cross-sectional | South Korea | North Korea, Vietnam, China, Japan, Philippine, Thailand, Cambodia, Mongolia, and Uzbekistan | 6,931 | 19–80 |
| García-Pola et al., [40] | 2010 | prospective case–control | Spain | South America, Africa, Europe and Asia | 90 | 6–41 |
| Gómez-Costa et al., [41] | 2011 | Cross-sectional | Spain | NR | 115,123 | 15– 64 |
| Soria et al., [22] | 2014 | Cross-sectional | Spain | Morocco, Ecuador, Eastern Europe | 333 | 6–17 |
| Rodriguez-Alvarez et al., [42] | 2016 | Cross-sectional | Spain | NR | 1388 | 4–9 |
| Duran et al., [43] | 2018 | Cross-sectional | Spain | Asia, South America,Africa,Central America, North America, Euroupe | 1400 | 3–14 |
| Olerud et al., [44] | 2014 | Cross-sectional | Sweden | Iran and the Horn of Africa,Balkans,Central Asia | 42 | 60+ |
| Thorbert-Mros et al., [45] | 2021 | Cross-sectional | Sweden | Somalia | 179 | 10–17 |
| Baggio et al., [46] | 2011 | Cross-sectional | Switzerland | NR | 856 | 3–6 |
| Y.C.Lin et al., [47] | 2011 | Cross-sectional | Taiwan | Vietnam and Indonesia | 590 | 4–6 |
| Ying-Chun Lin et al., [48] | 2015 | Cross-sectional: | Taiwan | NR | 32,611 | 3–5 |
| Traisuwan et al., [49] | 2016 | Cross-sectional | Thailand | Myanmar,Republic of Lao,Cambodia, | 418 | 20+ |
| Meva Altas et al.¸ [50] | 2022 | descriptive and retrospective study | Turkey | Syria | 549 | 6–12 |
| Wilson et al., [51] | 2013 | Cross-sectional | USA | Mexico | 4520 | 20–65+ |
| Kabani et al., [52] | 2011 | Cross-sectional: | USA | Central and South America | 9143 | 1–17 |
NR Not reported
Quality assessment
No papers were excluded solely based on methodological quality assessment. Despite aiming for high methodological quality studies, we recognized that excluding moderate quality studies could potentially miss valuable insights. Studies with a quality assessment score of 5,or 6 were included, even if they weren't of the highest quality. Incorporating a broader range of evidence allowed us to gain a more comprehensive understanding of oral health disparities. Studies of moderate quality contribute valuable data and perspectives, and their inclusion helps mitigate publication bias.
Only two studies [34, 51] out of a total of 32 studies, had all the questions of the critical appraisal answered with a “yes”, gaining a score of 9 out of 9. The least favorable scores were given to questions regarding the frame and adequacy of the sample size. The lowest score was five [32, 44, 45] and four studies [25, 29, 38, 43] scored six because there was no description of the sampling frame, participant selection procedures, and sample size calculation. Only thirteen studies reported procedures for calculating sample size or if the sample size was acceptable for the target group. Nineteen studies provided a detailed description of the study's setting and participants. Four studies [35, 38, 44, 45] failed to indicate the confidence interval (CI) for the mean value. The detailed quality assessment can be found in Appendix (page 3).
Characteristics of included studies
Seventeen studies had a control group [21, 22, 31–37, 39, 40, 42, 45, 47–50]. The control groups were the local population of the host country, except for three papers [21, 25, 32] which had a refugee population as a control group.
Among the included papers, three papers [25, 29, 47] assessed the treatment need of immigrants. Ten papers [2, 23, 26–29, 33, 38, 49, 50] reported the utilization of oral health services. Four papers [27, 30, 38, 48] investigated the dietary factors and two papers measured the household acculturation rate [28, 52]. Two papers studied the oral health status of pregnant immigrant women [40, 49] and two papers [33, 44] only included elderly population. None of the included studies had access to the oral health status of the sample group prior to their immigration.
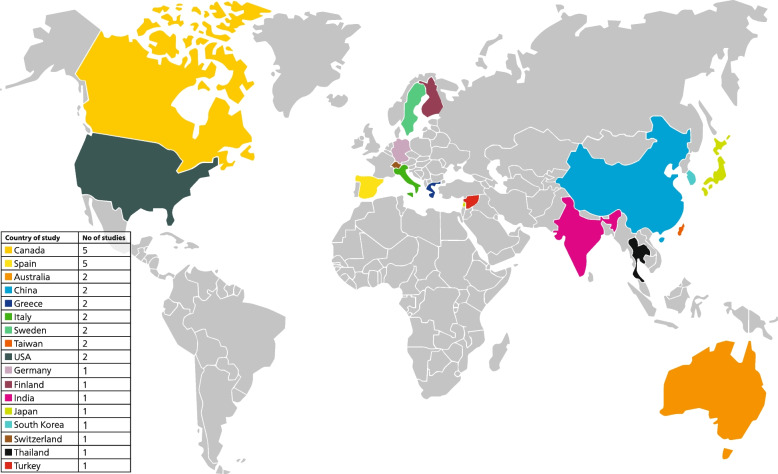
The study participants were children in twenty-four studies, in two studies both children and adults [40, 41] and in six studies only adults [32, 33, 39, 44, 49, 51] were involved. Immigrants originated from a wide range of countries, with a majority coming from South Asia, Africa, Eastern Europe and Central and South America as listed in Table 1. The frequency and distribution of the geographical location of countries of study are shown in Fig. 2, where it is clearly observable the highest number of studies on immigrants have been conducted in Canada and Spain.
Fig. 2.
World map showing the host countries, where the studies on the oral health of immigrants have been conducted. The key on the left shows the number of studies per country, with the countries sorted by number of studies (from the highest to the lowest). Countries in which no studies could be found are marked in grey
Dental caries in immigrants
Regarding dentin caries in children, two papers [47, 48] reported higher d3mft counts compared to other studies included in the review (mean d3mft > 5), both studies were conducted in Taiwan. The overall d3mft count (primary dentition) of studies identified was 3.63 (2.47) and for D3MFT (permanent teeth), it was 1.7 (1.2). Four papers [28, 35, 36, 42] also showed an expanded version of the decayed missing filled teeth (D3MFT) index with individual components, as seen in Table 2.
Table 2.
Caries distribution in immigrants and control groups in included studiesa
| Sample size | D3MFT | D3t | Mt | Ft | D3mft | d3t | mt | ft | D3MFT/d3mft | D3t/d3t | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Immigrant group | ||||||||||||||||
| Adults | ||||||||||||||||
| Traisuwan et al., [49] | 208 | 5.8 (4.4) | 5.5 (3.6) | 1.5 (1) | 3.2 (2.5) | NR | NR | NR | NR | NR | NR | |||||
| García-Pola et al., [37] | 45 | 8.33 (6.66) | NR | NR | NR | NR | NR | NR | NR | NR | NR | |||||
| Aarabi et al., [33] | 61 | 24.8 (3.9) | 5.3 (4.6) | 14.4 (8.8) | 5 (4.6) | NR | NR | NR | NR | NR | NR | |||||
| Children | ||||||||||||||||
| Hashizume et al., [38] | 378 | 1.28 (2.22) | NR | NR | NR | NR | NR | NR | NR | NR | NR | |||||
| Ferrazzano et al., [36] | 183 | 3.92 (2.92) | 2.49 (1.98) | 0.88 (1.24) | 0.56 (1.1) | NR | NR | NR | NR | NR | NR | |||||
| Y.C. Lin et al., [47] | 150 | NR | NR | NR | NR | 6.05 | 4.5 | 0.39 | 1.16 | NR | NR | |||||
| Liu et al., [30] | 1323 | 2.74 (3.02) | 0.01 | 0 | NR | 3.17 (3.12) | 2.71 | 0.01 | 0.01 | NR | NR | |||||
| Sivakumar et al., [35] | 431 | 1.14 (1.04) | 1.13 (1.07) | 0.04 (0.25) | 0 | 0.18 ( 0.5) | 0.12 (0.4) | 0.04 (0.26) | 0.02 (0.15) | NR | NR | |||||
| Ying-Chun Lin et al., [48] | 1046 | NR | NR | NR | NR | 8.47 | 5.38 | 0.3 | 2.79 | NR | NR | |||||
| Zhang et al., [31] | 3412 | 1.05 (0.34) | NR | NR | NR | 3.18 (0.57) | NR | NR | NR | NR | NR | |||||
| Dahlan et al., [28] | 336 | NR | NR | NR | NR | NR | NR | NR | NR | 3.7 | NR | |||||
| Diamanti et al., [34] | 707 | 2.5 (0.14) | 1.75 (0.07) | 00 (0.1) | 0.75 (0.21) | 3 (3.8) | 2.7 (3.9) | 0.0 (0.4) | 0.3 (1.1) | NR | NR | |||||
| Rodriguez-Alvarez et al., [42] | 413 | 0.1 (0.42) | 0.1 (0.4) | NR | NR | 1.7 (2.6) | 1.5 (2.5) | NR | NR | NR | NR | |||||
| Soria et al., [22] | 177 | NR | NR | NR | NR | NR | NR | NR | NR | 7.8 | NR | |||||
| Azrak et al., [29] | 211 | NR | NR | NR | NR | 2.2 (3.8) | 1.7 (3) | 0.2 (0.8) | 0.3 (1.6) | NR | NR | |||||
| Hoover et al., [25, 53] | 44 | NR | NR | 0.64 (1.12) | 0.48 (1.52) | NR | NR | NR | NR | 3.52 (3.78) | 2.41 (3.44) | |||||
| Meva Altas et al.¸ [50] | 549 | 0.94 (0.18) | NR | NR | NR | 4.8 (1.6) | NR | NR | NR | NR | NR | |||||
| Elyasi et al., [27] | 274 | NR | NR | NR | NR | NR | NR | NR | NR | 3.28 (3.76) | NR | |||||
| García-Pola et al., [37] | 45 | NR | NR | NR | NR | NR | 3.5 (3.4) | NR | NR | NR | NR | |||||
| Overall | 9679 | 1.7 (1·2) | 1.36 (1.01) | 0.52 (0.43) | 0.59 (0.13) | 3.63 (2.47) | 2.76 (1.69) | 0.18 (0.16) | 0.76 (1.07) | 4.57 (2.15) | 2.41 | |||||
| Control group | ||||||||||||||||
| Adults | ||||||||||||||||
| Traisuwan et al., [49] | 210 | 4.8 (4) | 3.8 (2.9) | 2 (1.5) | 3.1 (2.5) | NR | NR | NR | NR | NR | NR | |||||
| García-Pola et al., [37] | 45 | 8.07 (6.05) | NR | NR | NR | NR | NR | NR | NR | NR | NR | |||||
| Aarabi et al., [33] | 51 | 23.4 (4.6) | 2.1 (2.8) | 12.6 (9.5) | 8.6 (6.2) | NR | NR | NR | NR | NR | NR | |||||
| Children | ||||||||||||||||
| Y.C.Lin et al., [47] | 440 | NR | NR | NR | NR | 3.88 | 1.57 | 0.17 | 2.13 | NR | NR | |||||
| Ferrazzano et al., [36] | 370 | 3.29 (3.21) | 1.16 (1.35) | 0.71 (1.43) | 1.38 (1.98) | NR | NR | NR | NR | NR | NR | |||||
| Sivakumar et al., [35] | 434 | 0.45 (0.8) | 0.32 (0.69) | 0.02 (0.16) | 0.1 (0.36) | 0.58 (0.98) | 0.3 (0.72) | 0.23 (0.65) | 0.04 (0.21) | NR | NR | |||||
| Ying-Chun Lin et al., [48] | 31,565 | NR | NR | NR | NR | 8.10 | 4.37 | 0.23 | 3.5 | NR | NR | |||||
| Zhang et al., [31] | 6738 | 1 (0.31) | NR | NR | NR | 2.61 (0.66) | NR | NR | NR | NR | NR | |||||
| Rodriguez-Alvarez et al., [42] | 839 | 0.0 (0.28) | 0.0 (0.2) | NR | NR | 0.7 (1.5) | 0.6 (1.4) | NR | NR | NR | NR | |||||
| Soria et al., [22] | 136 | NR | NR | NR | NR | NR | NR | NR | NR | 6.6 | 7.3 (4.4) | |||||
| Hoover et al., [25] | 89 | NR | NR | 1.25 (2.2) | 1.55 (2.36) | NR | NR | NR | NR | 5.8 (4.2) | 3 (3.4) | |||||
| García-Pola et al., [37] | 45 | NR | NR | NR | NR | NR | 0.24 (0.6) | NR | NR | NR | NR | |||||
| Overall | 40,656 | 1.58 (1.5) | 0.74 (0.59) | 0.66 (0.61) | 1.01 (0.79) | 2.68 (3) | 1.71 (1.85) | 0.21 (0.03) | 1.89 (1.74) | 6.2 (0.56) | 5.15 (3.04) | |||||
D3MFT – caries experience in the permanent dentition, d3mft – caries experience in the primary dentition, D3T – decayed teeth in the permanent dentition, MT – missing teeth in the permanent dentition, FT – filled teeth in the permanent dentition, d3t – decayed teeth in the primary dentition, mt – missing teeth in the primary dentition, ft – filled teeth in the primary dentition, NR Not reported, SD Standard deviation
aData presented as mean (SD) unless otherwise specified
Upon comparing the overall caries means of the included studies, untreated dental Caries (D3T and d3t) constituted the dominant share of the caries experience (D3MFT and d3mft) in immigrant children. While, within their respective control groups, the highest proportion of caries experience was attributed to Filled Teeth (FT and ft).
Among the papers that had the local population as control group, the immigrant children had a higher mean D3MFT/d3mft (SD) compared to local children. This difference was significant except for two papers [31, 42], which only showed a significant difference for primary dentition and not the permanent dentition.
There were only three studies [33, 40, 49] reported caries using D3MFT in adults, suggesting that there is a lack of caries data in immigrant adults. The mean D3MFT count among immigrant adults was higher than that of the local population. This difference was significant except for two studies [33, 40]. It is important to emphasize that we only reported the statistics generated by the included studies. As regards caries experience, due to the limited number of studies and heterogeneity of study participants in the adult population, the overall mean for caries experience was not calculated.
Caries prevalence and further detail of included papers
The main focus of all included studies was oral health (OH) except for two [21, 25], which also involved general health (GH). Only three studies [21, 42] reported a caries prevalence of below 20% for immigrant children. Caries prevalence in the primary dentition ranged from 22% to 88.7%, and in the permanent dentition from 5.6% to 90.9%. Overall, the caries prevalence, regardless of dentition stage, ranged from 17% to 97.3% among the immigrant population (Table 3).
Table 3.
Further detail of included papers and caries prevalence
| Focus GH or OH | Dentist involved | Instruments mentioned | Reliability tested† | Caries detection method |
Caries prevalence (%) |
Caries prevalence in control group (%) |
|
|---|---|---|---|---|---|---|---|
| Primary Dentition | |||||||
| Christian B et al., [23] | OH | NR | NR | NR | ICDAS II | 22 | NR |
| Gibbs et al., [24] | OH | Yes | Yes | Yes | ICDAS/ WHO | 34 | NR |
| Baggio et al., [46] | OH | Yes | Yes | Yes | WHO | 38.6 | 12.1 |
| Rodriguez-Alvarez et al., [42] | OH | One dentist | Yes | No | WHO | 42.6 | 24.1 |
| Azrak et al., [29] | OH | Yes | Yes | NR | WHO | 45.5 | NR |
| Amin et al., [26] | OH | Yes | Yes | Yes | WHO | 56 | NR |
| Duran et al., [43] | OH | Yes | Yes | Yes | NR | 62.3 | 42.6 |
| Diamanti et al., [34] | OH | Yes | Yes | Yes | ICDAS II | 64.2 | NR |
| Liu et al., [30] | OH | Yes | Yes | Yes | WHO | 65.7 | NR |
| García-Pola et al., [37] | OH | Yes | Yes | NR | WHO | 66.6 | 15.5 |
| Ying-Chun Lin et al., [48] | OH | Yes | Yes | NR | WHO | 68.1 | 56.7 |
| Zhang et al., [31] | OH | Yes | Yes | Yes | WHO | 71.4 | 64.5 |
| Campus et al., [37] | OH | Yes | Yes | Yes | ICDAS | 72.6 | 41.6 |
| Y.C. Lin et al., [47] | OH | NR | Yes | Yes | WHO | 88.7 | NR |
| Permanent Dentition | |||||||
| Rodriguez-Alvarez et al., [42] | OH | One dentist | Yes | No | WHO | 5.6 | 2.4 |
| Duran et al., [43] | OH | Yes | Yes | Yes | NR | 16.4 | 12.2 |
| Liu et al., [30] | OH | Yes | Yes | Yes | WHO | 28.1 | NR |
| Wilson et al., [51] | OH | Yes | NR | NR | NS | 38 | 34.4 |
| Hashizume et al., [38] | OH | Yes | Yes | NR | WHO | 38.1 | NR |
| Zhang et al., [31] | OH | Yes | Yes | Yes | WHO | 42.5 | 39.6 |
| Lee et al., [39] | OH | Yes | Yes | NR | WHO | 54.8 | 24.9 |
| Mattila et al., [32] | OH | Yes | NR | NR | NR | 65 | 57 |
| Diamanti et al., [34] | OH | Yes | Yes | Yes | WHO | 67.1, | NR |
| Sivakumar et al., [35] | OH | NR | Yes | Yes | WHO | 71 | 53.9 |
| Olerud et al., [44] | OH | One dentist | Yes | NR | NR | 75 | NR |
| Ferrazzano et al., [36] | OH | Yes | Yes | Yes | WHO | 77.5 | 55.9 |
| García-Pola et al., [37] | OH | Yes | Yes | NR | WHO | 88.9 | 80 |
| Traisuwan et al., [49] | OH | Yes | NR | Yes | WHO | 90.9 | 85.2 |
| Aarabi et al., [33] | OH | Yes | Yes | Yes | WHO | NR | NR |
| Unspecified dentition | |||||||
| Pavlopoulou et al., [21] | GH | NR | NR | NR | NR | 17.4 | 24.7 |
| Kabani et al., [52] | OH | NR | NR | NR | WHO | 24.9 | NR |
| Elyasi et al., [27] | OH | Yes | Yes | NR | WHO | 52 | NR |
| Soria et al., [22] | OH | Yes | NR | NR | NR | 92.3 | NR |
| Meva Altas et al.¸ [50] | OH | One dentist | Yes | NR | NR | 97.3 | NR |
| Dahlan et al., [28] | OH | Yes | Yes | NR | WHO | NR | NR |
| Gómez-Costa et al., [41] | OH | Yes | NR | NR | WHO | NR | NR |
| Thorbert-Mros et al., [45] | OH | Yes | Yes | NR | WHO | NR | NR |
| Hoover et al., [25] | GH | Yes | Yes | NR | NR | NR | NR |
GH General health, OH Oral health, NR Not reported, WHO World health organization, ICDAS International Caries Detection and Assessment System
†Reliability tested: If the studies gave information about inter or intra reliability of dental examination, it is showed as Yes or NR. The studies that did not report the caries prevalence, reported caries in other forms DMFT/S
When comparing the caries prevalence to the local population, the immigrants always had a higher prevalence. Only one study [21] reported a lower caries prevalence than in the control group however, in this instance the control group was a refugee population. Visual comparison of caries prevalence between immigrant groups and their corresponding control groups via bar charts can be found in the appendix (page 5).
Other indices to report caries: DMFS and ICDAS
Five papers [24, 26, 29, 34, 37] reported caries prevalence in other forms using D3MF at the surface level (D3MFS) or International Caries Detection and Assessment System (ICDAS). Two papers [26, 29] reported caries using D3MFS (Table 4). Two papers [24, 34] used the dmfs index derived from the full range of ICDAS scores [53], as a result, their count of caries experience included both enamel and dentine caries since both are recorded by the ICDAS index [54]. Analysis of tooth surfaces found that early caries lesions were especially frequent in age groups 12 and 15, with respective mean values of 1.9(2.1) and 2.4(3.0) [34].
Table 4.
Caries distribution in immigrants in studies using DMFS and ICDAS as caries indicesa
| Sample size | Age in years | dmfs | Decayed surfaces | Missing surfaces | Filled surfaces | |
| Amin et al., [26] | 125 | 1.7–6 | 7.2 (11.6) | 4.2 (7.4) | NR | NR |
| Azrak et al., [29] | 211 | 1–5.9 | 4.8 (11) | 3 (6.7) | 0.7 (3.5) | 1.1 (6.2) |
| ICDAS Study | Sample size | Age in years | DMFS/dmfs ICDAS 1–6 | DFMS/dmfs ICDAS1-3 | DMFS/dmfs ICDAS 4–6 | |
| Diamanti et al., [34] | 707 | 5 | 4.1 (9.1) | 1.1 (1.6) | 5 (7.9) | |
| 12 | 3.6 (4.4) | 1.9 (2.1) | 3.6 (4.4) | |||
| 15 | 3.7 (4.8) | 2.4 (3) | 3.7 (4.8) | |||
| Gibbs et al., [24] | 630 | 1–4 | 1.9 (4.62) | NA | 0.91 (3.47) | |
NR Not reported, DMFS Decayed, missing, and filled surfaces, ICDAS International Caries Detection and Assessment System
aCaries value is reported as mean (SD) unless otherwise specified
Periodontal Health in immigrants
Nine papers [25, 32, 33, 41, 44, 45, 49–51] examined the periodontal health. Four of them [25, 32, 45, 50] focused on children and five [33, 41, 44, 49, 51] on adults. Two paper [33, 44] only included an elderly population and one paper included only pregnant migrant women [49].
Regarding periodontal health in children, the prevalence of gingivitis ranged from 5.1% to 100%, indicating a high variation. In particular, the prevalence of gingivitis was reported as very high in three studies [25, 32, 45], with one paper reporting that almost all children had chronic gingivitis [45] and two papers reporting a prevalence of two thirds [25, 32]. Although gingival inflammation was apparently high from the aforementioned studies, one paper [50] reported a prevalence of gingivitis of 5.1%. Another paper showed a higher prevalence of gingivitis in immigrant children compared to the local population with a margin of 25% [45].
Regarding periodontal health in adults, the prevalence of periodontitis was present in half of the population observed [51], similar was observed in another study [44] which reported two-thirds of participants had periodontitis and a quarter of them were diagnosed with severe periodontitis (gingival pockets of 6 mm or deeper). Based on the Papillary Bleeding Index, a study [33] conducted on elderly immigrants showed a greater prevalence of papillary bleeding compared to their peers (46.3% vs 30.5%).
The one paper that included only pregnant Immigrant women, reported almost all participants had gingivitis, the periodontitis was three times more prevalent in immigrant pregnant women compared to local pregnant women (74.5% vs 22.4%). Moreover, 11% were diagnosed with severe periodontitis compared to only 0.5% in the host population, which showed a huge difference in periodontal health between pregnant migrant women and local pregnant ones [49].
Oral health accessibility
Access to oral health care is an important determinant of oral health status [55]. Unfamiliarity with the dental care delivery system, lack of proper insurance (where relevant) and high costs of dental treatment might make obtaining proper oral care difficult [26].
Eight papers [23, 26–29, 33, 49, 50] explored the history of dental visits in immigrants, all papers addressed children except for two [33, 49]. Four papers [27, 28, 33, 49] reported, whether the participants have had a dental visit in the last year while others asked about history of dental visit in their lifetime.
When asking immigrants’ children about the history of their last dentist visit, the percentage of children who never visited a dentist in their life, ranged from 52 to 88% (appendix page 6). For adults, there was a significant difference in dental visits between migrants and local women, with 61.1% of migrants never having visited the dentist or visiting less frequently than once a year [49]. Regarding last year dental visit, 88.2% of non-migrant Germans had at least one dental examination, compared to 68.9% of immigrants.
Discussion
Based on the included studies, it was evident that immigrants were more likely to suffer from oral health problems than the local population in their host country. The perceived treatment needs varied between studies, still dental caries and periodontal disease were most commonly regarded as urgent problems among immigrants.
A variety of factors have been identified as influencing dental caries prevalence among immigrant children, including family socioeconomic status, household acculturation, oral health accessibility, child's age, gingival inflammation, fluoride exposure,country of origin, and generational status [22, 25, 46, 52]. These factors collectively contribute to caries development, highlighting the complex interaction between diverse influences on dental health outcomes within different demographic contexts.
Acculturation and oral health have a dynamic relationship [3]. Oral health might be affected by acculturation, which has been defined as "lifestyle and behavioral changes as a result of moving from one culture to another, usually as a result of immigration” [56]. According to one study [52], household acculturation was a significant predictor of dental caries in children, whereas another study [28] found no association between parental acculturation and children’s dmft/DMFT level.
Lower age was directly correlated to higher caries prevalence [34, 50]. In another study, the same was observed but just for the primary dentition [31]. The disparity in caries between immigrant children and their peers in older age groups was less, which it has been suggested indicates that the dental health of migrants children was better in older children [31, 34, 50]. The decrease in caries disparity among older immigrant children might be due to improved socioeconomic status of parents [34], increased access to oral health services, local peers’ influences at schools [31], and ultimately development of better oral health habits, such as proper oral hygiene practices(frequent and adequate brushing and flossing) and healthier nutritional choices. It might be hypothesized that the older children are more mature and generally more familiarized with the new language and therefore adopt easier to dental health habits of their host country, while younger children usually continue to follow their parents' traditional practices. According to a study conducted in Spain, the second generation of immigrant children had lower caries prevalence than first-generation and they were almost similar to Spanish-born children after adjustment for confounders (social class, marital status, and maternal education) [22]. However, there are many confounding variables at play, as well as methodological limitations, which limits confidence in any conclusions about age-related disparities drawn from cross-sectional studies.
All studies, except one [41], reported that the prevalence of periodontitis in immigrants was higher compared to the local population. According to one study [41], there was a similar proportion of gum bleeding among immigrants (16 to 23%) and Spanish nationals (17 to 21%). immigrant women, as well as immigrants between the ages of 25–64, were less likely to experience gum bleeding than their local peers.
The socio-demographic characteristics of immigrant children significantly impacted their use of dental care. These factors included parental education [28], income level [28], dental coverage [23, 26–28], child's age [26], mother's age [26, 28], the duration of parental residence in the host country [26], household structure [28] (whether living with both parents or with a single parent), frequency of parent's dental visits [23] (characterized by infrequent attendance), primary reasons for dentist visits (primarily for treatment rather than preventive care) [23], parental perception of the child's dental care needs [23], and parental assimilation scores [28]. Among the various factors considered by the studies, requiring insurance coverage was identified as the most common and significant factor affecting children's dental visits [23, 26–28]. One paper [23] specifically explores reasons related to the immigrant child’s non-utilization of dental services and their parents/guardians reported cost, long waiting periods for treatment, language barriers and “no need for child to visit” were the main barriers for accessing to oral health services for their children.
Oral health disparities are not limited to immigrant groups and are widespread in numerous nations, reflecting the present global tendency to emphasize specialized treatments rather than ensuring equal access to care [57, 58]. It is evident that a number of global factors might be contributing to the weaker oral health of immigrants compared to native people in host countries. Firstly, there are disparities in oral health across the world that are impacted by socioeconomic, cultural, and environmental variables. Second, these difficulties could also be exacerbated by obstacles such as language barriers, inadequate insurance, and unfamiliarity with the healthcare systems in the host countries. Oral health disparities across immigrant populations can be made exacerbated by differences in income, education, and healthcare facilities between the countries of origin and the host countries. To address these global factors contributing to oral health inequalities, multi-level interventions aimed at providing equitable access to dental healthcare services are needed [57, 59].
Our search strategy was unable to find any studies conducted in South America or Africa. This might be attributed to a lack of scientific research on immigrant dental caries or periodontal problems after 2011 in these regions or to the fact that these studies have not yet been published in indexed journals. In our review, the majority of studies employed cross-sectional designs and had a pure descriptive scope, indicating that this issue is still in its exploratory phase.
This scoping review has some limitations, including the possibility that some information could have been overlooked, as the studies retrieved in the systematic database search showed considerable differences in the characterization and reported data of the immigrant population. Additionally, we observed significant differences in sampling procedures, power calculations, and geographic location among the included studies; some studies [25, 29, 38, 43] did not specify sample size calculation, and immigrant populations were generally smaller than the control groups. There are also existing intra-immigrant disparities, which might be due to variations in socioeconomic status, healthcare access, cultural practices, and health literacy which was not discussed in detail in our review.
Due to a lack of comparability and high heterogeneity among the studies, we did not conduct a meta-analysis. Since we included studies published exclusively after 2011, our findings are less generalizable due to the limited number of publications on this topic, especially from developing and underdeveloped countries. Moreover, including only articles published in English, Italian, German, and French might have introduced a language bias, excluding studies published in other languages. In addition, human errors and bias may have contributed to the loss of information or bias of the results.
In spite of these limitations, to our knowledge, the present review was the first to summarize oral health diseases of immigrants in a quantitative manner on a global scale. The study provides additional information on special needs and associations that can be used to improve oral health in immigrants.
The findings of our study have significant implications for professionals in oral health as well as public health efforts. Inequalities in immigrants' oral health care are often masked by population-level data since immigrants constitute a small proportion of populations in host countries. Our findings successfully addressed the reality of immigrant oral health in their respective countries.
Conclusion
There is a higher prevalence of dental caries among immigrants than among the local population in each host country, regardless of age, gender, or country. Untreated dental caries (D3T, d3t) were more prevalent in this population. The existing data can be used to set priorities for improving immigrants' oral health worldwide. Immigrants worldwide face major oral health challenges, including dental caries, periodontal diseases and limited access to oral health services.
Efforts must be made to reduce oral health disparities among immigrants. Host countries must implement strategies to significantly increase access to dental care for immigrants such as Providing oral health insurance to immigrant children, developing community healthcare centers, expanding financial assistance, and integrating dental services into primary healthcare.. Further studies are needed to contribute to real-world knowledge about immigrants' oral health, as they can assist host-country policymakers in improving immigrants' oral health and developing more cost-effective preventative measures.
Supplementary Information
Acknowledgements
The authors would like to thank Bernadette Rawyler and Ines Badertscher from the graphic Department of School of Dental Medicine, University of Bern, Switzerland for the help to create the figures.
Abbreviations
- OSF
Open science framework
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SPIDER
Sample phenomenon of interest, design, evaluation, and research type
- JBI SUMARI
Joanna Briggs Institute System for the Unified Management of the Assessment and Review of Information
- WHO
World health organization
- D3MFT
Caries experience in the permanent dentition
- d3mft
Caries experience in the primary dentition
- D3T
Decayed teeth in the permanent dentition
- MT
Missing teeth in the permanent dentition
- FT
Filled teeth in the permanent dentition
- d3t
Decayed teeth in the primary dentition
- mt
Missing teeth in the primary dentition
- ft
Filled teeth in the primary dentition
- NR
Not reported
- SD
Standard deviation
- GH
General health
- OH
Oral health
- ICDAS
International Caries Detection and Assessment System
- DMFS
Decayed, missing, and filled surfaces
Authors’ contributions
S.A.B.R, G.C, and M.E.O contributed to design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; G.VA.D, A.M, and P.C provided critical insights and revised the manuscript at various stages. All authors gave their final approval and agreed to be accountable for all aspects of the work.
Funding
The research presented in the manuscript received funding from Swiss Government Excellence Scholarship Grants: #2021.0876.
Availability of data and materials
Any data that support the findings of this study are available from the corresponding author, upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Seyed Ahmad Banihashem Rad and Marcella Esteves-Oliveira are joint first authors.
References
- 1.McAuliffe M, Khadria B. International Organization for Migration (2021). World Migration Report. 2022
- 2.Liu Y. Differentiation of self-rated oral health between American non-citizens and citizens. Int Dent J. 2016;66(6):350–5. 10.1111/idj.12248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu B, Mao W, Qi X, Pei Y. Immigration and oral health in older adults: an integrative approach. J Dent Res. 2021;100(7):686–92. 10.1177/0022034521990649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Armfield JM, Spencer AJ, Slade GD. Changing inequalities in the distribution of caries associated with improving child oral health in Australia. J Public Health Dent. 2009;69(2):125–34. 10.1111/j.1752-7325.2008.00110.x [DOI] [PubMed] [Google Scholar]
- 5.Riggs E, Gibbs L, Kilpatrick N, Gussy M, van Gemert C, Ali S, et al. Breaking down the barriers: a qualitative study to understand child oral health in refugee and migrant communities in Australia. Ethn Health. 2015;20(3):241–57. 10.1080/13557858.2014.907391 [DOI] [PubMed] [Google Scholar]
- 6.Collaborators GOD, Bernabe E, Marcenes W, Hernandez C, Bailey J, Abreu L, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–73. 10.1177/0022034520908533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wen P, Chen M, Zhong Y, Dong Q, Wong H. Global burden and inequality of dental caries, 1990 to 2019. J Dent Res. 2022;101(4):392–9. 10.1177/00220345211056247 [DOI] [PubMed] [Google Scholar]
- 8.Kisely S. No mental health without oral health. Can J Psychiatry. 2016;61(5):277–82. 10.1177/0706743716632523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor oral health as a determinant of malnutrition and sarcopenia. Nutrients. 2019;11(12):2898. 10.3390/nu11122898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fiorillo L. Oral health: the first step to well-being. MDPI; 2019. p. 676. [DOI] [PMC free article] [PubMed]
- 11.Carramolino-Cuéllar E, Tomás I, Jiménez-Soriano Y. Relationship between the oral cavity and cardiovascular diseases and metabolic syndrome. Med Oral Patol Oral Cir Bucal. 2014;19(3): e289. 10.4317/medoral.19563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cronin A. Periodontal disease is a risk marker for coronary heart disease? Evidence-Based Dentistry. 2009;10(1):22. [DOI] [PubMed]
- 13.Ramos-Gomez F, Kinsler JJ. Addressing social determinants of oral health, structural racism and discrimination and intersectionality among immigrant and non-English speaking Hispanics in the United States. J Public Health Dent. 2022;82:133–9. 10.1111/jphd.12524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riley JL, Gilbert GH, Heft MW. Socioeconomic and demographic disparities in symptoms of orofacial pain. J Public Health Dent. 2003;63(3):166–73. 10.1111/j.1752-7325.2003.tb03495.x [DOI] [PubMed] [Google Scholar]
- 15.Banihashem Rad SA, Esteves Oliveira M, Maklennan A, Castiglia P, Campus G. Higher prevalence of dental caries and periodontal problems among refugees: A scoping review. J Glob Health. 2023;13:04111. 10.7189/jogh.13.04111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88: 105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 17.Cooke A, Smith D, Booth A. Beyond PICO: the SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012;22(10):1435–43. 10.1177/1049732312452938 [DOI] [PubMed] [Google Scholar]
- 18.Organization WH. Oral health surveys: basic methods: World Health Organization; 2013.
- 19.Klein H, Palmer CE, Knutson JW. Studies on dental caries: I. Dental status and dental needs of elementary school children. Public Health Reports (1896–1970). 1938:751–65.
- 20.Pitts N, Fyffe H. The effect of varying diagnostic thresholds upon clinical caries data for a low prevalence group. J Dent Res. 1988;67(3):592–6. 10.1177/00220345880670031401 [DOI] [PubMed] [Google Scholar]
- 21.Pavlopoulou ID, Tanaka M, Dikalioti S, Samoli E, Nisianakis P, Boleti OD, et al. Clinical and laboratory evaluation of new immigrant and refugee children arriving in Greece. BMC Pediatr. 2017;17(1):1–10. 10.1186/s12887-017-0888-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Valcarcel Soria R, Bernabé E, Somacarrera Perez ML. Acculturation and dental caries among children in Spain. J Immigr Minor Health. 2019;21:699–705. 10.1007/s10903-018-0848-9 [DOI] [PubMed] [Google Scholar]
- 23.Christian B, Young D, Gibbs L, de Silva A, Gold L, Riggs E, et al. Exploring child dental service use among migrant families in metropolitan Melbourne. Aust Dental J. 2015;60(2):200–4. 10.1111/adj.12321 [DOI] [PubMed] [Google Scholar]
- 24.Gibbs L, de Silva AM, Christian B, Gold L, Gussy M, Moore L, et al. Child oral health in migrant families: a cross-sectional study of caries in 1–4 year old children from migrant backgrounds residing in Melbourne. Aust Commun Dental Health. 2016;33(2):100–6. [PubMed] [Google Scholar]
- 25.Hoover J, Vatanparast H, Uswak G. Risk determinants of dental caries and oral hygiene status in 3–15 year-old recent immigrant and refugee children in Saskatchewan, Canada: a pilot study. J Immigr Minor Health. 2017;19:1315–21. 10.1007/s10903-016-0452-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amin MS, Perez A, Nyachhyon P. Parental awareness and dental attendance of children among African immigrants. J Immigr Minor Health. 2015;17:132–8. 10.1007/s10903-013-9912-7 [DOI] [PubMed] [Google Scholar]
- 27.Elyasi M, Abtahi M, Kornerup I, Amin M. Impact of Parents’ Sense of Coherence on Children’s Oral Health-Related Behaviors and Dental Caries Experience among Newcomers. J Health Care Poor Underserved. 2021;32(1):423–34. 10.1353/hpu.2021.0032 [DOI] [PubMed] [Google Scholar]
- 28.Dahlan R, Bohlouli B, Salami B, Saltaji H, Amin M. Parental acculturation and oral health of children among immigrants. J Public Health Dent. 2022;82(4):426–36. 10.1111/jphd.12481 [DOI] [PubMed] [Google Scholar]
- 29.El Azrak M, Huang A, Hai-Santiago K, Bertone MF, DeMaré D, Schroth RJ. The oral health of preschool children of refugee and immigrant families in Manitoba. J Can Dent Assoc. 2017;83(h9):1488–2159. [PubMed] [Google Scholar]
- 30.Liu C-j, Zhou W, Feng X-s. Dental caries status of students from migrant primary schools in Shanghai Pudong New Area. BMC Oral Health. 2016;16:1–8. [DOI] [PMC free article] [PubMed]
- 31.Zhang H, Zeng X, Jiang Y, Xu W, Wang X, Li C, et al. The disparity in caries and sealants between migrant and native children in Shanghai: A cross-sectional study. Int J Dental Hygiene. 2020;18(1):84–91. 10.1111/idh.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mattila A, Ghaderi P, Tervonen L, Niskanen L, Pesonen P, Anttonen V, et al. Self-reported oral health and use of dental services among asylum seekers and immigrants in Finland—a pilot study. Eur J Public Health. 2016;26(6):1006–10. 10.1093/eurpub/ckw116 [DOI] [PubMed] [Google Scholar]
- 33.Aarabi G, Reissmann DR, Seedorf U, Becher H, Heydecke G, Kofahl C. Oral health and access to dental care–a comparison of elderly migrants and non-migrants in Germany. Ethn Health. 2018;23(7):703–17. 10.1080/13557858.2017.1294658 [DOI] [PubMed] [Google Scholar]
- 34.Diamanti I, Berdouses ED, Kavvadia K, Arapostathis KN, Polychronopoulou A, Oulis CJ. Dental caries prevalence and experience (ICDAS II criteria) of 5-, 12-and 15-year-old children and adolescents with an immigrant background in Greece, compared with the host population: a cross-sectional study. Int J Environ Res Public Health. 2021;19(1):14. 10.3390/ijerph19010014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sivakumar V, Jain J, Haridas R, Paliayal S, Rodrigues S, Jose M. Oral health status of Tibetan and local school children: a comparative study. J Clin Diagnos Res. 2016;10(11):ZC29. [DOI] [PMC free article] [PubMed]
- 36.Ferrazzano G, Cantile T, Sangianantoni G, Ingenito A, Rengo S, Alcidi B, et al. Oral health status and Unmet Restorative Treatment Needs (UTN) in disadvantaged migrant and not migrant children in Italy. Eur J Paediatr Dent. 2019;20(1):10–4. [DOI] [PubMed] [Google Scholar]
- 37.Campus G, Cocco F, Strohmenger L, Wolf TG, Balian A, Arghittu A, et al. Inequalities in caries among pre-school Italian children with different background. BMC Pediatr. 2022;22(1):1–10. 10.1186/s12887-022-03470-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hashizume LN, Shinada K, Kawaguchi Y. Factors associated with prevalence of dental caries in Brazilian schoolchildren residing in Japan. J Oral Sci. 2011;53(3):307–12. 10.2334/josnusd.53.307 [DOI] [PubMed] [Google Scholar]
- 39.Lee H, Seo S, Kang R, Kim Y, Hyun H-K. Increasing access to oral healthcare for marriage-immigrant women in South Korea: programme design to policy recommendation. Int Dent J. 2019;69(5):354–60. 10.1111/idj.12479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.García-Pola M, González-Díaz A, García-Martín JM. Effect of a preventive oral health program starting during pregnancy: a case-control study comparing immigrant and native women and their children. Int J Environ Res Public Health. 2021;18(8):4096. 10.3390/ijerph18084096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gómez-Costa D, San-Roman-Montero J, Rojo R, Gil Á, Gómez de Diego R, López-Sánchez AF. Self-reported prevalence of periodontal disease among the Spanish population and immigrants: 2006, 2011/12 and 2017: a population-based study. BMC Oral Health. 2021;21(1):1–10. [DOI] [PMC free article] [PubMed]
- 42.Rodriguez-Alvarez E, Borrell LN, Marañon E, Lanborena N. Immigrant status and ethnic inequities in dental caries in children: Bilbao, Spain. Int J Environ Res Public Health. 2022;19(8):4487. 10.3390/ijerph19084487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Veloso Duran A, Framis-de-Mena B, Vázquez Salceda MC, Guinot JF. Evaluation and comparison of oral health status between spanish and immigrant children residing in Barcelona, Spain. Children. 2022;9(9):1354. 10.3390/children9091354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Olerud E, Hagman-Gustavsson ML, Gabre P. Oral health status in older immigrants in a medium-sized Swedish city. Spec Care Dentist. 2016;36(6):328–34. 10.1111/scd.12195 [DOI] [PubMed] [Google Scholar]
- 45.Thorbert-Mros S, Ali N, Ali M, Ayas M, Trullenque-Eriksson A, Dahlén G. A comparative study on periodontitis and periodontitis-associated bacteria in Somali and non-Somali children and adolescents living in Trollhättan, Sweden. Eur J Oral Sci. 2022;130(2): e12843. 10.1111/eos.12843 [DOI] [PubMed] [Google Scholar]
- 46.Baggio S, Abarca M, Bodenmann P, Gehri M, Madrid C. Early childhood caries in Switzerland: a marker of social inequalities. BMC Oral Health. 2015;15(1):1–9. 10.1186/s12903-015-0066-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lin Y, Yen Y, Chang C, Ting C, Chen P, Chen C, et al. Oral health disparities of children among Southeast Asian immigrant women in arranged transnational marriages in Taiwan. Caries Res. 2014;48(6):575–83. 10.1159/000351680 [DOI] [PubMed] [Google Scholar]
- 48.Lin Y-C, Chang C-S, Ho P-S, Lee C-H, Chen J-H, Huang H-L. Immigrant-native differences in sugar-sweetened beverage and snack consumption and preventive behaviors associated with severe early childhood caries: a large-scale survey in Taiwan. Int J Environ Res Public Health. 2019;16(6):1047. 10.3390/ijerph16061047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Traisuwan W. Oral health status and behaviors of pregnant migrant workers in Bangkok, Thailand: A cross-sectional study. BMC Oral Health. 2021;21:1–8. 10.1186/s12903-021-01732-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Altaş ZM, Sezerol MA. Prevalence and associated factors of dental caries in syrian immigrant children aged 6–12 Years. Children. 2023;10(6):1000. 10.3390/children10061000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson FA, Wang Y, Borrell LN, Bae S, Stimpson JP. Disparities in oral health by immigration status in the United States. J Am Dental Assoc. 2018;149(6):414–21. e3. [DOI] [PubMed]
- 52.Kabani FA, Stockbridge EL, Berly Varghese B, Loethen AD. Acculturation and the oral health of a nationally representative sample of Hispanic children in the United States: An analysis of 2011–2012 National Survey of Children’s Health data. BMC Public Health. 2020;20(1):1–12. 10.1186/s12889-019-8045-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pitts NB, Ekstrand KR, Foundation I. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)–methods for staging of the caries process and enabling dentists to manage caries. Commun Dent Oral Epidemiol. 2013;41(1):e41–52. 10.1111/cdoe.12025 [DOI] [PubMed] [Google Scholar]
- 54.Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Commun Dent Oral Epidemiol. 2007;35(3):170–8. 10.1111/j.1600-0528.2007.00347.x [DOI] [PubMed] [Google Scholar]
- 55.Bahannan SA, Eltelety SM, Hassan MH, Ibrahim SS, Amer HA, El Meligy OA, Al-Johani KA, Kayal RA, Mokeem AA, Qutob AF, Mira AI. Oral and Dental Health Status among Adolescents with Limited Access to Dental Care Services in Jeddah. Dent J (Basel). 2018;6(2):15. 10.3390/dj6020015. [DOI] [PMC free article] [PubMed]
- 56.Gao X-L, McGrath C. A review on the oral health impacts of acculturation. J Immigr Minor Health. 2011;13:202–13. 10.1007/s10903-010-9414-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cohen L, Dahlen G, Escobar A, Fejerskov O, Johnson N, Manji F. Dentistry in crisis: time to change. La Cascada Declaration Australian Dental Journal. 2017;62(3):258–60. 10.1111/adj.12546 [DOI] [PubMed] [Google Scholar]
- 58.Fejerskov O, Escobar G, Jøssing M, Baelum V. A functional natural dentition for all–and for life? The oral healthcare system needs revision. J Oral Rehabil. 2013;40(9):707–22. 10.1111/joor.12082 [DOI] [PubMed] [Google Scholar]
- 59.Watt RG, Daly B, Allison P, Macpherson LM, Venturelli R, Listl S, et al. Ending the neglect of global oral health: time for radical action. Lancet. 2019;394(10194):261–72. 10.1016/S0140-6736(19)31133-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Any data that support the findings of this study are available from the corresponding author, upon reasonable request.