Abstract
Background:
About 10% of Indians have common mental disorders (CMDs) which include depression and anxiety. These disorders are common in women, which not only impacts on their quality of life but also their family members. The objective of the study was to estimate the prevalence of CMDs, and factors associated with them among women residing in coastal Karnataka.
Methods:
A cross-sectional study was carried out among 980 women aged between 18 and 60 years from 2019 to 2021. Women were administered a baseline questionnaire along with Patient Health Questionnaire-9 (PHQ-9), Generalised Anxiety Disorder questionnaire-7 (GAD-7) and Cohen’s Perceived Stress Scale-4 (PSS-4). Data were collected using Epi-info and were analysed using SPSS version 15.0. Association between CMDs and socio-demographic, reproductive health and behavioural factors were expressed as crude and adjusted odds ratio (OR) with 95% confidence intervals (CI).
Results:
The prevalence of CMDs among women was 5.7%, with 4.6% having depression and 3.37% with anxiety disorders. Multivariate logistic regression analysis showed that residing in urban areas (OR = 2.15; 95% CI:1.10–4.17), having a chronic illness (OR = 2.38; 95% CI:1.14–4.97), history of recent bereavement in the family (OR = 2.20; 95% CI:1.02–4.75), early marriage (OR = 2.63; 95% CI:1.09–6.33), history of abortion (OR = 2.89; 95% CI:1.42–5.92), and exposure to domestic violence (OR = 3.08; 95% CI:1.14–8.33) were significantly correlated with CMDs in this sample.
Conclusions:
The study revealed that CMDs were prevalent among the surveyed women, which calls for routine screening of women for CMDs in primary care settings for early identification and appropriate interventions.
Keywords: Anxiety, depression, CMDs, women, India
Key Messages:
Mental health is a vital component of health of an individual. The burden of psychiatric disorders is distributed unevenly across all sections of society with women being more vulnerable. The prevalence of CMDs was 5.7% among the surveyed women in the coastal region of southern Karnataka. It was comparable with other community-based surveys conducted across the country.
The term common mental disorders (CMDs) was coined by Goldberg and Huxley in 1992 to explain mental health conditions that are generally seen in community settings which include depression and anxiety. 1
Globally, about 792 million (10.7%) people are living with mental health disorders with females (11.9%) outnumbering males (9.3%). Of these conditions, depression (3.4%) and anxiety (3.8%) are the common disorders with female preponderance being exhibited. 2 Recent data from the National Mental Health Survey (NMHS) 2015–2016 estimated that about 10% of the 150 million Indians were suffering from common mental disorders (CMDs). The burden of CMDs was two to three times greater in urban areas in comparison to rural settings. Earlier mental health services were available only in the urban settings thereby depriving the rural population of it. The national mental health policy which came into existence in 2002 ensured that the mental health facilities were incorporated into the primary health care settings. 3
The burden of psychiatric disorders is unevenly distributed across all sections of the society in India with CMDs affecting women almost twice as compared to men. 4 This could be due to various biological, psychological and social factors coupled with hormonal changes during puberty, pregnancy, postpartum and menopause which increases women’s vulnerability to poor mental health. Also, women are constantly subjected to gender inequity, social omission and gender disadvantage like early marriage, early pregnancy, and domestic violence, especially in rural India. 5 Women who suffer from CMDs usually present with symptoms such as tiredness, absent-mindedness, sleeplessness, bad temper, difficulty in focusing, headaches and psychosomatic complaints. 6
As women are the backbone of their families, a minor mental health issue with them can disturb the family dynamics to a large extent. Families can also experience the financial burden from direct and indirect economic costs that could arise from loss of employment and decreased productivity. Hence, it is crucial to identify the symptoms of CMDs especially among women and intervene at the earliest.
Most of the studies on CMDs were limited to women in the reproductive age group, or conducted in hospital settings, which makes it difficult to make realistic estimates of the burden of CMDs in the community. As there is a scarcity of data on mental health status of women aged between 18 and 60 years, the present study was undertaken to estimate the prevalence of CMDs and their associated risk factors among women residing in coastal region of southern Karnataka.
Material and Methods
This cross-sectional study was carried out to determine the prevalence of CMDs among women aged between 18 and 60 years residing in the rural and urban localities of the field practice area of a medical college in southern Karnataka, India from 2019 to 2021. In this study, CMDs included common mental health conditions prevailing in community settings which include depression and anxiety. 1 Women who were severely ill (those who were suffering from a debilitating illness), physically disabled, or bed-ridden or those who were pregnant/in post-partum period at the time of survey were excluded.
The study area covers a population of approximately 40,000 individuals residing across 15 villages, with 13,763 women aged between 18 and 60 years. Primary health care services to this population are provided through a network of four rural health centres and one urban health centre. These outreach centres provide comprehensive health care services, including management of non-communicable diseases, maternal and child health services, and geriatric care through regular clinics. Furthermore, mental health care, dental, and occupational health care services are provided regularly.
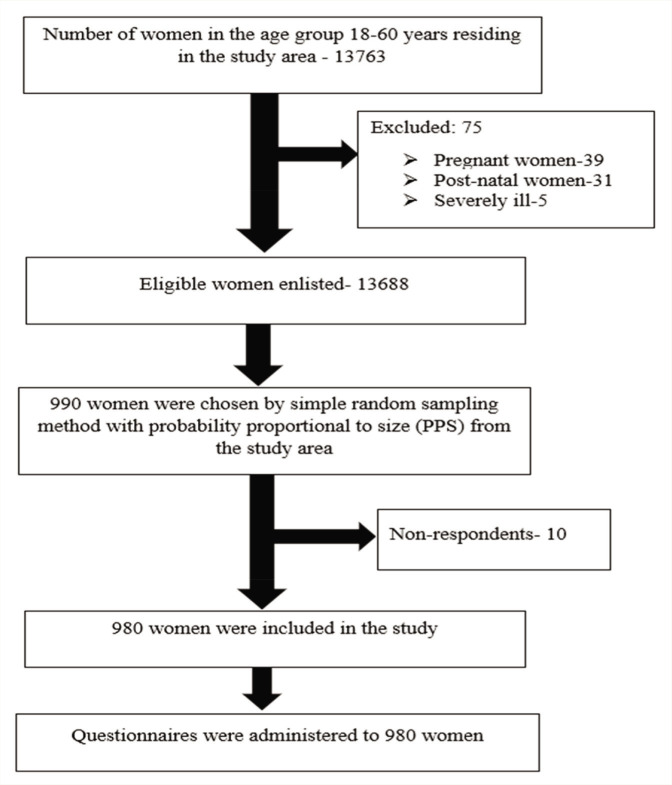
The sample size was estimated to be 990, considering a prevalence of CMDs at 10%, with an allowable error of 20%, a confidence interval of 95%, and accounting for a non-response rate of 10%. 7 Households were chosen by simple random sampling method with probability proportional to size (PPS) from the field practice area as the participants were from a homogenous community (Figure 1). The household data used for sampling were obtained from the health and demographic surveillance system maintained at the outreach centres.
Figure 1. Flow Diagram Depicting Recruitment of Participants.
The study protocol received approval from the institutional ethics committee (IEC: 631/2019) prior to the initiation of the study. Written informed consent was obtained from all participating women before their recruitment into the study. They were assured that their personal information would be kept anonymous and confidential.
During the household visits, all recruited women were administered a predesigned questionnaire to capture data on their socio-demographic profile, behavioural characteristics, chronic illness (broadly defined as conditions that last one year or more and require ongoing medical attention or limit activities of daily living or both), reproductive health characteristics, family-related factors, and physical activity. 8 To assess the stress level of the participants which could be one of the risk factors for CMDs, Cohen’s Perceived Stress Scale-4 (PSS-4) was translated to the local language (Kannada) and administered by the trained doctor. 9 This scale has four questions; and each item is rated on a five-point Likert scale, resulting in a total score ranging from zero to sixteen. Using the tertile method in SPSS, the total score was categorized into mild, moderate, and severe, with the higher scores indicating higher perceived stress in individuals. Depression was assessed using Patient Health Questionnaire-9 (PHQ-9), which consists of nine questions. Every question was scored from zero to three, and the total scores varied between zero and twenty-seven. 10 Similarly, the Generalised Anxiety Disorder-7 scale (GAD-7) was administered to screen for anxiety. It consists of seven questions and total scores range from zero to twenty-one. 11 A score of ≥10 on either PHQ-9 or GAD-7 or both was considered positive for CMDs. Both the scales were translated into the local language and administered by a trained doctor for screening depression and anxiety respectively in the community settings. Women who screened positive for CMDs were referred to the Psychiatry outpatient department at the medical college or the outreach health centres on specified days depending on the psychiatrist’s availability for confirmation of diagnosis.
Data were collected using Epi-info application version 7.2.2.6, and analysis was done using Statistical Package for the Social Sciences (SPSS) version 15.0. Univariate logistic regression analysis was done and variables with a p < 0.01 were selected for multivariate analysis to identify the independent predictors of CMDs. The results were presented as crude and adjusted odds ratio (OR) with 95% confidence intervals. A p < 0.05 was considered statistically significant.
Results
The study was conducted on 980 women aged between 18 and 60 years, residing in the study area for more than one year. All the 980 proforma had complete data and were considered for the data analysis. The overall prevalence of CMDs among the surveyed women was found to be 5.7%, with the prevalence of depression and anxiety being 4.60% and 3.37%, respectively.
The mean age of women was 45.93 (SD ± 12.42) years, and only 279 participants (28.5%) had more than 10 years of schooling. Out of the total participants, 820 (83.77%) were Hindus, and 678 (69.18%) were currently married. There were 404 (41.22%) women who belonged to joint families, followed by 370 (37.76%) from nuclear families, and 206 (21%) from three-generation families. Nearly three-fourths (72.96%) of the respondents resided in rural areas.
About 876 women (89.38%) belonged to the middle socio-economic class based on the modified BG Prasad scale. 12 Only 218 (22.24%) were employed, with 66 (6.73%) of them engaged in white-collar or skilled jobs (Table 1).
Table 1.
Socio-demographic Characteristics of the Study Participants (n = 980).
| Characteristics | Frequency (%) | |
| Age in years | 18–45 | 427 (43.57) |
| 46–60 | 553 (56.43) | |
| Religion | Hindu | 820 (83.67) |
| Muslim | 123 (12.55) | |
| Christian | 37 (3.78) | |
| Marital status | Unmarried | 64 (6.53) |
| Currently married | 678 (69.18) | |
| Separated/divorced/widowed | 238 (24.29) | |
| Literacy status | Illiterate | 95 (9.69) |
| 1–4 years of schooling | 102 (10.41) | |
| 5–10 years of schooling | 504 (51.43) | |
| Above 10 years of schooling | 279 (28.47) | |
| Occupation | Professional/white collar/skilled | 66 (6.73) |
| Semi-skilled/unskilled | 152 (15.51) | |
| Homemaker | 687 (70.11) | |
| Student/unemployed/retired | 75 (7.65) | |
| Type of family | Nuclear | 370 (37.76) |
| Three generation | 206 (21.02) | |
| Joint | 404 (41.22) | |
| Socioeconomic status | Upper class (I) | 91 (9.29) |
| Upper middle class (II) | 359 (36.63) | |
| Middle class (III) | 376 (38.37) | |
| Upper lower class (IV) | 141 (14.38) | |
| Lower class (V) | 13 (1.33) | |
| Area | Urban | 265 (27.04) |
| Rural | 715 (72.96) | |
Out of the total 916 ever-married women, 73 (7.97%) had married before completing 18 years of age. About 48 (4.89%) study participants reported experiencing domestic violence in the past four weeks from the time of survey. Among the 678 currently married participants, 669 (98.67%) reported a good psychosocial relationship with their spouse, while 9 (1.33%) reported having frequent fights with their spouse.
In the univariate analysis, the odds of having CMDs were found to be 2.43 times higher (p < 0.005) among women aged 46–60 years compared to those between 18 and 45 years of age. Participants who attended 1–4 years of schooling and 5–10 years of schooling had 3.68 (p < 0.08) and 2.22 (p < 0.048) times higher odds of having CMDs, respectively, than those who had more than 10 years of schooling. Women from three-generation families and urban areas were twice as likely to have CMDs. Women with unemployed spouses were six times more likely to have CMDs. However, there was no significant association found between marital status, religion, socio-economic status and participant’s work status (Table 2).
Table 2.
Association of Socio-demographic Characteristics with Common Mental Disorders Among Women.
| Characteristics | Common Mental Disorders | Unadjusted OR (95% CI) | P Value | ||
| Present (n = 56) |
Absent (n = 924) |
||||
| Frequency (%) | Frequency (%) | ||||
| Age in years (n = 980) | 18–45 | 14 (25.00) | 413 (44.70) | 1 | |
| 46–60 | 42 (75.00) | 511 (55.30) | 2.43 (1.31–4.50) | 0.005* | |
| Literacy status (n = 980) | Illiterate | 7 (12.50) | 88 (9.52) | 2.69 (0.95–7.64) | 0.062 |
| 1–4 years of schooling | 10 (17.86) | 92 (9.96) | 3.68 (1.41–9.61) | 0.008* | |
| 5–10 years of schooling | 31 (55.36) | 473 (51.19) | 2.22 (1.01–4.89) | 0.048* | |
| Above 10 years of schooling | 8 (14.28) | 271 (29.33) | 1 | ||
| Marital status (n = 980) | Unmarried | 3 (5.36) | 61 (6.60) | 1 | |
| Married | 27 (48.21) | 651 (70.45) | 0.84 (0.25–2.86) | 0.784 | |
| Separated/Divorced/Widowed | 26 (46.43) | 212 (22.95) | 2.49 (0.73–8.52) | 0.145 | |
| Religion (n = 980) | Hindu | 47 (83.93) | 773 (83.66) | 1 | |
| Muslim | 7 (12.50) | 116 (12.55) | 0.99 (0.44–2.25) | 0.986 | |
| Christian | 2 (3.57) | 35 (3.79) | 0.94 (0.22–4.03) | 0.933 | |
| Type of family (n = 980) | Nuclear | 25 (44.64) | 345 (37.34) | 1.88 (0.98–3.62) | 0.060 |
| Joint | 15 (26.79) | 389 (42.10) | 1 | ||
| Three generation | 16 (28.57) | 190 (20.56) | 2.18 (1.06–4.51) | 0.035* | |
| Socioeconomic status (n = 980) | Upper class | 4 (7.15) | 87 (9.42) | 1 | |
| Middle class | 39 (69.64) | 696 (75.32) | 1.22 (0.42–3.49) | 0.713 | |
| Lower class | 13 (23.21) | 141 (15.26) | 2.01 (0.63–6.35) | 0.237 | |
| Type of area (n = 980) | Urban | 23 (41.07) | 242 (26.19) | 1.96 (1.31–3.41) | 0.017* |
| Rural | 33 (58.93) | 682 (73.81) | 1 | ||
| Working status of participants (n = 980) | Working | 13 (23.21) | 205 (22.19) | 1.15 (0.59–2.20) | 0.681 |
| Currently not working | 7 (12.50) | 68 (7.36) | 1.86 (0.79–4.34) | 0.151 | |
| Homemaker | 36 (64.29) | 651 (70.45) | 1 | ||
| Spouse’s working status (n = 678) | Employed | 15 (55.55) | 521 (80.03) | 1 | |
| Unemployed | 8 (29.63) | 45 (6.91) | 6.18 (2.48–15.35) | <0.001* | |
| Retired | 4 (14.82) | 85 (13.06) | 1.64 (0.53–5.04) | 0.393 | |
*Bold fonts indicate that the values are statistically significant.
Participants who had a chronic illness were found to have 2.86 times higher odds of having CMDs, and women who reported death in their family in the past year had 2.31 times higher odds of having CMDs. Among the reproductive characteristics that were assessed, CMDs showed a significant association with irregular menstrual cycles, early marriage, teenage pregnancy (<18 years of age), having three or more children, a history of abortion, attaining menopause, and experiencing perimenopausal symptoms.
On univariate analysis, CMDs were found to have a statistically significant association with exposure to domestic violence (p < 0.001), psychosocial relationship with family (p < 0.001), women’s autonomy in decision-making (p < 0.05), and stress level (p < 0.05) (Table 3)
Table 3.
Association of General Health, Reproductive Health and Behavioural Factors with Common Mental Disorders.
| Characteristics | Common mental disorders | Unadjusted OR (95% CI) | P Value | ||
| Present | Absent | ||||
| Frequency (%) | Frequency (%) | ||||
| Chronic illness (n = 980) | Yes | 37 (66.07) | 374 (40.48) | 2.86 (1.62–5.06) | <0.001* |
| No | 19 (33.93) | 550 (59.52) | 1 | ||
| Recent bereavement (n = 980) | Yes | 13 (23.21) | 107 (11.58) | 2.31 (1.20–4.43) | 0.012* |
| No | 43 (76.79) | 817 (88.42) | 1 | ||
| Menstruation (n = 470) | Regular | 10 (55.56) | 396 (87.61) | 1 | |
| Irregular | 8 (44.44) | 56 (12.39) | 5.66 (2.14–14.94) | <0.001* | |
| Age at marriage in years (n = 916) | <18 | 11 (20.75) | 62 (7.18) | 3.49 (1.70–7.17) | 0.001* |
| 18–30 | 38 (71.70) | 748 (86.68) | 1 | ||
| >30 | 4 (7.55) | 53 (6.14) | 1.49 (0.51–4.32) | 0.467 | |
| Age at first pregnancy in years (n = 868) | <18 | 7 (14.58) | 23 (2.80) | 5.74 (2.32–14.20) | <0.001* |
| 18–30 | 38 (79.17) | 716 (87.32) | 1 | ||
| Above 30 | 3 (6.25) | 81 (9.88) | 0.69 (0.21–2.31) | 0.556 | |
| Number of children (n = 868) | 0 | 1 (2.08) | 18 (2.20) | 1.09 (0.14–8.44) | 0.930 |
| 1–3 | 35 (72.92) | 690 (84.15) | 1 | ||
| Above 3 | 12 (25.00) | 112 (13.65) | 2.11 (1.06–4.19) | 0.032* | |
| History of abortion (n = 868) | Yes | 17 (35.42) | 108 (13.17) | 3.62 (1.94–6.76) | <0.001* |
| No | 31 (64.58) | 712 (86.83) | 1 | ||
| Attained menopause (n = 980) | Yes | 38 (67.86) | 472 (51.08) | 2.02 (1.14–3.59) | 0.017* |
| No | 18 (32.14) | 452 (48.92) | 1 | ||
| Peri-menopausal symptoms (n = 250) | Yes | 10 (90.91) | 108 (45.19) | 12.13 (1.53–96.26) | 0.018* |
| No | 1 (9.09) | 131 (54.81) | 1 | ||
| Substance use by participants (n = 980) | Yes | 8 (14.29) | 72 (7.79) | 1.97 (0.89–4.33) | 0.090 |
| No | 48 (85.71) | 852 (92.21) | 1 | ||
| Exposed to domestic violence (n =4 8) | Yes | 11 (19.64) | 37 (4.00) | 5.86 (2.81–12.24) | <0.001* |
| No | 45 (80.36) | 887 (96.00) | 1 | ||
| Psychosocial relationship with family members (n = 980) | Good | 52 (92.86) | 919 (99.46) | 1 | |
| Bad | 4 (7.14) | 5 (0.54) | 14.14 (3.69–54.22) | <0.001* | |
| Autonomy in decision making (n = 980) | Yes | 49 (87.50) | 887 (96.00) | 1 | |
| No | 7 (12.50) | 37 (4.00) | 3.43 (1.45–8.07) | 0.005* | |
| Stress level (n = 980) | Mild | 2 (3.57) | 407 (44.05) | 1 | |
| Moderate | 23 (41.07) | 424 (45.89) | 11.04 (2.59–47.12) | 0.001* | |
| Severe | 31 (55.36) | 93 (10.06) | 67.83 (15.95–288.47) | <0.001* | |
*Bold fonts indicate that the values are statistically significant.
In the multivariate logistic regression analysis, living in urban localities, having chronic morbidities, history of a recent bereavement in the family, getting married before 18 years of age, a history of abortions, and exposure to domestic violence were identified as independent predictors of CMDs among the surveyed women (Table 4).
Table 4.
Multivariate Logistic Regression Analysis for Association of Various Factors with Common Mental Disorders (n = 868).
| Variable | Adjusted OR (95% CI) | P Value | |
| Age in years | 18–45 | 1 | |
| 46–60 | 2.19 (0.65–7.37) | 0.207 | |
| Literacy status | Illiterate | 0.71 (0.16–3.26) | 0.663 |
| 1–4 years of schooling | 1.70 (0.49–5.87) | 0.401 | |
| 5–10 years of schooling | 1.24 (0.44–3.45) | 0.684 | |
| Above 10 years of schooling | 1 | ||
| Type of family | Nuclear | 1.92 (0.87–4.22) | 0.105 |
| Joint | 1 | ||
| Three generation | 1.78 (0.76–4.13) | 0.183 | |
| Area | Urban | 2.15 (1.10–4.17) | 0.024* |
| Rural | 1 | ||
| Chronic illness among the participants | Yes | 2.38 (1.14–4.97) | 0.020* |
| Death in the family in past one year | Yes | 2.20 (1.02–4.75) | 0.044* |
| Age at marriage in years | <18 | 2.63 (1.09–6.33) | 0.031* |
| 18–30 | 1 | ||
| >30 | 0.96 (0.26–3.55) | 0.946 | |
| Number of children among conceived | 0 | 0.53 (0.58–4.78) | 0.567 |
| 1–3 | 1 | ||
| >3 | 1.52 (0.66–3.47) | 0.325 | |
| History of abortion | Yes | 2.89 (1.42–5.92) | 0.004* |
| Attained menopause | Yes | 0.60 (0.19–1.90) | 0.387 |
| Substance use by the participants | Yes | 1.62 (0.59–4.38) | 0.352 |
| Experienced domestic violence | Yes | 3.08 (1.41–8.33) | 0.026* |
| Psychological relationship with family | Good | 1 | |
| Not good | 3.43 (0.48–24.51) | 0.219 | |
| Autonomy in decision-making | Yes | 1 | |
| No | 1.12 (0.33–3.81) | 0.851 | |
*Bold fonts indicate that the values are statistically significant.
Discussion
In this community-based cross-sectional survey conducted among 980 women aged 18–60 from Udupi taluk, we observed an overall prevalence of CMDs at 5.7%. This finding aligns with the NMHS findings (conducted in 2015–2016), which reported a similar CMDs prevalence of 6.96% among women from 12 states across six regions in India. 7 However, there were contrasting findings in other Indian studies. For example, Sathyanarayana et al. in Bengaluru reported a much higher prevalence of 33.5%, Agarwal et al. in Meerut found a prevalence of 19.8%, and Fahey et al. in rural Gujarat reported a prevalence of 23.8% for CMDs among women.13, 14, 15 These discrepancies in prevalence rates could be attributed to differences in the screening tools used. The current study used PHQ-9 and GAD-7, while the other three studies used Self Reporting Questionnaire-20. The choice of screening tool may impact the reported prevalence rates due to variations in the assessment and identification of CMDs among the study participants.
The present study found that the prevalence of depression and anxiety among the participants was 4.60% and 3.37%, respectively. These findings are in concordance with the WHO Mental Health Report 2019, which reported a prevalence of 6% for depression and 5.9% for anxiety among women aged above 20 years. 16 However, lower prevalence rates were reported in other studies. For example, Kallakuri et al. from Andra Pradesh reported a prevalence of 3% for depression and 1.8% for anxiety, and the NMHS 2015–2016 reported a prevalence of 2.97% for depression and 0.76% for anxiety.7, 17 These variations in prevalence rates across studies could be due to several factors, including differences in the study populations, sample sizes, cultural factors, and specific assessment tools used in the studies.
In the current study, more than half of the participants (56%) belonged to the age group of 46–60 years. This contrasts with a study by Deswal et al. in Pune, in which almost half (48%) of the participants belonged to age group 18–34 years. 18 The disparity in the study findings could be attributed to differences in the age criteria used to recruit women for the studies. The majority of the participants in the current study were Hindus (84%), similar to the study findings by Sathyanarayana et al. 13 However, in the present study, a higher proportion of women had more than five years of schooling (80%) compared to the study report from Pune (66%). This difference could be because Udupi, where the current study was conducted, is one of the districts in Karnataka with a high literacy rate (male:91.40%; female:81.58%). Regarding employment, only 22% of women were employed, which is comparable to prior Indian studies conducted in Goa (21%) and Pune (32%).5, 18 In the present study, almost an equal proportion of participants belonged to joint families (41%) and nuclear families (38%), while in the study by Sathyanarayana et al. in Bengaluru the majority belonged to nuclear families (70%). 13 This difference could be due to variations in the study settings. Regarding socio-economic status, predominantly the surveyed women in the current study belonged to middle class (89%) according to the modified BG Prasad scale. This is in agreement with the study results of Agarwal et al. in Meerut, where 81% of participants belonged to middle class. 14
The prevalence of CMDs in the present study was higher in those with lower literacy levels; however, literacy level was not an independent predictor of CMDs. This finding is consistent with the study done in rural Puducherry by Srinivasan et al. where the risk of CMDs was six times higher among women with low literacy. 19 The explanation for this could be that literate women are economically independent and have greater decision-making power in their families, which may have a protective effect against CMDs. In the present study, the likelihood of CMDs was two times higher among residents of urban areas as compared to those in rural areas. This finding is in congruence with the NMHS report (2015–2016) where the prevalence of CMDs was higher in Urban-metro areas (14.7%) compared to rural areas (9.6%). 7 The higher odds in urban settings could be due to busy schedules, increased stress levels, and the existence of more number of nuclear families where women may get less support in executing family responsibilities.
In our study, we found that the risk of having CMDs was 2.38 times higher among women with chronic illnesses compared to healthy participants. A similar association was found in a study done by Nair et al. in Vellore, although it did not reach statistical significance. 20 Furthermore, the odds of having CMDs doubled among women who experienced a recent bereavement within the family compared to those without any such history; this finding is in concordance with the study by Keyes et al. in USA. 21
This study found that women who were married before 18 years of age were at almost three times higher risk of developing CMDs compared to rest of the population. This finding is supported by the results of the study by Patel et al. where the prevalence of CMDs decreased as the age of marriage increased. 5 The risk of CMDs increased by three-fold among women who had undergone abortions in the past as compared to those who had uneventful pregnancies. This was in line with the study conducted by Mota et al. in the USA, which reported a higher burden of any mood disorders (34%) and anxiety disorders (16%) among women who underwent an abortion. 22 A significant association was observed between CMDs and exposure to domestic violence among the surveyed women (OR = 3.08; 95% CI: 1.14–8.33) which substantiates the reports of the study conducted by Srinivasan et al. (OR = 3.20; 95% CI:1.20–8.40), though it did not remain significant on multivariate analysis. 19
In the present study, the odds of having CMDs were three times higher among women who had a poor relationship with their family, although this association was not significant. Similar findings were seen in the study conducted by Patel et al. where the prevalence of CMDs was higher among women who had little or no support from their family (OR=2.70; 95%CI: 1.80-4.00). 5 The present study showed a significant association between lack of women’s autonomy in decision-making and CMDs, although it was not significant in multivariate analysis. A similar association was observed in the prior studies conducted by Patel et al. (OR = 2.20; 95% CI: 1.40–3.40) and Panigrahi et al.6, 23
Our study identified some key socio-economic, general health, reproductive health and behavioural factors for CMDs among women. These are extremely important in planning strategies for CMDs prevention at primary care level.
Strengths and Limitations
This study is valuable as it provides a community-based estimate of CMDs among women aged 18–60 years, which helps in understanding the mental health challenges faced by women in this age group. The use of validated PHQ-9 and GAD-7 administered by a trained doctor for screening depression and anxiety in the community settings is strength of the study. Considering the homogenous nature of the socio-demographic, reproductive and behavioural characteristics of women across the district, the study findings could be generalised to this region. Most research on CMDs among women has focused on a limited number of behavioural factors and reproductive health conditions while the present study has been an effort to study the association between risk factors from multiple domains and CMDs comprehensively among the surveyed women.
The study is not without limitations. Despite efforts to maintain privacy and confidentiality during interviews, sensitive questions like substance use and domestic violence may still lead to under-reporting due to stigma and fear of consequences. Further due to the cross-sectional nature of the study, the temporal association between various reproductive and behavioural factors and CMDs could not be ascertained.
Conclusions
In the present study, the prevalence of CMDs among the surveyed women was found to be 5.7% with that of depression and anxiety being 4.60% and 3.37%, respectively. Several factors were identified as significant predictors of CMDs, including residing in urban areas, having a chronic illness, history of recent bereavement in the family, early marriage, history of abortion, and exposure to domestic violence.
This calls for regular screening of mental health issues at the primary healthcare level to ensure timely identification and interventions for women with CMDs. Addressing gender disadvantage is essential in promoting women’s mental health. Empowering women through self-help groups and other community-based organizations can provide them with a sense of security and support, which can be beneficial in managing mental health issues. Furthermore, a public-private partnership approach may be explored for implementing suitable preventive and curative mental health strategies for women in this region.
Acknowledgments
We thank all the women who participated in the study and provided the information. It would not have been possible to complete this study without their support, co-operation and active participation.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical Approval: Kasturba Medical College and Kasturba Hospital Institutional Ethics Committee, Manipal.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
References
- 1.Goldberg D. A bio-social model for common mental disorders. Acta Psychiatr Scand Suppl, 1994; 385: 66–70. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Depression and other common mental disorders: global health estimates. World Health Organization; 2017. Available at https://apps.who.int/iris/handle/10665/254610. Accessed on 20 October 2021 [Google Scholar]
- 3.Ministry of Health and Family Welfare. New pathways new hope. National Mental Health Policy of India. Government of India; 2014. Available at https://nhm.gov.in/images/pdf/National_Health_Mental_Policy.pdf. Accessed on 12 November 2022. . [Google Scholar]
- 4.Shidhaye R, Patel V. Association of socio-economic, gender and health factors with common mental disorders in women: a population-based study of 5703 married rural women in India. Int J Epidemiol, 2010; 39(6): 1510–1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel V, Kirkwood BR, Pednekar S, et al. Gender disadvantage and reproductive health risk factors for common mental disorders in women: a community survey in India. Arch Gen Psychiatry, 2006; 63(4): 404–413. [DOI] [PubMed] [Google Scholar]
- 6.Tawar S, Bhatia SS, Ilankumaran M. Mental health, are we at risk? Indian J Community Med, 2014; 39(1): 43–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gururaj G, Varghese M, Benegal V. et al. National Mental Health Survey of India, 2015-16: prevalence, patterns and outcomes. Bengaluru, National Institute of Mental Health and Neuro Sciences, NIMHANS Publication No. 129, 2016. [Google Scholar]
- 8.Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion; 2022. Available at https://www.cdc.gov/chronicdisease/index.htm. Accessed on 20 September 2023.
- 9.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav, 1993; 24(4): 385–396. [PubMed] [Google Scholar]
- 10.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 2001; 16(9): 606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med, 2006; 166(10): 1092–1097. [DOI] [PubMed] [Google Scholar]
- 12.Khairnar MR, Kumar PG, Kusumakar A. Updated BG prasad socioeconomic status classification for the year 2021. J Indian Assoc Public Health Dent, 2021; 19(2): 154–155. [Google Scholar]
- 13.Sathyanarayana RK, Manjunatha S. Common mental disorders among women of reproductive age group in an urban area in Bengaluru. Int J Community Med Public Health, 2019; 6(4): 1768–1773. [Google Scholar]
- 14.Agarwal V, Jain S, Garg SK, et al. Common mental disorders and its socio-demographic correlates among women of reproductive age in urban and rural area of Meerut. Indian J Community Health, 2020; 32(2): 359–364. [Google Scholar]
- 15.Fahey N, Soni A, Allison J, et al. Education mitigates the relationship of stress and mental disorders among rural Indian women. Ann Glob Health, 2016; 82(5): 779–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. World mental health report: transforming mental health for all; 2014. Available at https://www.who.int/publications/i/item/9789240049338. Accessed on 27 May 2023.
- 17.Kallakuri S, Devarapalli S, Tripathi AP, et al. Common mental disorders and risk factors in rural India: baseline data from the SMART mental health project. BJPsych Open. 2018. 4(4): 192–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deswal BS, Pawar A. An epidemiological study of mental disorders at Pune, Maharashtra. Indian J Community Med, 2012; 37(2): 116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Srinivasan M, Reddy MM, Sarkar S, et al. Depression, anxiety, and stress among rural south Indian women-prevalence and correlates: a community-based study. J Neurosci Rural Pract, 2020; 11(1): 78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nair AR, Shivanna YKG, Illimoottil JP, et al. Common mental disorders among women and its social correlates in an urban marginalized populace in South India. Int J Soc Psychiatry, 2022; 68(7): 1394–1402. [DOI] [PubMed] [Google Scholar]
- 21.Keyes KM, Pratt C, Galea S, et al. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. Am J Psychiatry, 2014; 171(8): 864–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mota NP, Burnett M, Sareen J. Associations between abortion, mental disorders, and suicidal behaviour in a nationally representative sample. Can J Psychiatry, 2010; 55(4): 239–247. [DOI] [PubMed] [Google Scholar]
- 23.Panigrahi A, Padhy AP, Panigrahi M. Mental health status among married working women residing in Bhubaneswar city, India: a psychosocial survey. Biomed Res Int, 2014: Article ID 979827. [DOI] [PMC free article] [PubMed] [Google Scholar]