Abstract
Study Design
Randomized controlled trial
Objective
The primary objective of this study was to compare the short-term clinical and radiological outcomes of full-endoscopic lumbar laminotomy (FEL) with those of subtotal lumbar laminectomy (STL) for lumbar spinal stenosis (LSS).
Methods
In this prospective randomized trial a total of 52 patients were enrolled from May 2016 to September 2021 after providing written informed consent. The authors investigated 45 patients who were followed up for more than 6 months.
Results
There were significant improvements in visual analogue scale (VAS) and Oswestry Disability Index (ODI) scores after the operation in both groups. The FEL group tended to have significantly shorter hospital stay. Interestingly, a statistically significant increase in postoperative lumbar lordosis and segmental angle was observed in the FEL group and both groups, respectively. Spondylolisthesis was exacerbated or newly developed in five of the 21 patients (24%) in the STL group. In contrast, improvement in spondylolisthesis was observed in two of the 24 patients (8%) in the FEL group. There were no complications that resulted in fatal sequelae and no significant difference in the complication rate.
Conclusions
The clinical results of FEL were similar to those of STL. In addition, the results of FEL were superior to those of STL in terms of a decrease in the postoperative length of stay and radiologic instability, such as iatrogenic spondylolisthesis. The results of this study indicate that FEL is a comparable surgical method to STL for LSS.
Keywords: spinal stenosis, laminectomy, spondylolisthesis, decompression, endoscopy, spine, full-endoscopy
Introduction
As the global society shifts toward an aging population, various degenerative diseases are emerging as major social problems. Recent research is focused on identifying more efficient approaches for the treatment of degenerative diseases. The use of current treatment methods not only increases social costs but also greatly affects the quality of life in the elderly population.1,2 Spinal stenosis, in which the spinal canal is narrowed due to degenerative changes in the spinal canal, such as discs, yellow ligaments, and facet joints, is a degenerative spinal disease that accounts for a significant proportion of the disease in the elderly. These degenerative changes cause dural sac and nerve root compression and various symptoms, such as low back pain, radiating pain, limb weakness, and/or neurogenic claudication.3,4
Surgical treatment is considered if symptoms persist or worsen and continue to impair the patient’s quality of life despite previous conservative treatment via various methods, such as medication, steroid injection, and physical therapy. In the past, classical open subtotal laminectomy (STL) was considered the treatment of choice for spinal stenosis, but it can damage paravertebral structures, such as muscles, ligaments, and facet joints, resulting in postoperative instability.5-9 As technology has developed, the choice of surgical treatment has expanded to include minimally invasive techniques using tubular retractors or full-endoscopic laminotomy (FEL).10,11 To date, a considerable number of studies have been conducted on the advantages of endoscopic surgery, including reduced blood loss, fast recovery, and short hospital stay. 12 Among the existing studies, there are few randomized controlled studies comparing FEL with other treatments. We hypothesized that FEL is not inferior to STL, and the primary outcome was visual analog scale (VAS)/Oswestry Disability Index (ODI) after 6 months. Here, we compare the early clinical results of FEL with STL for lumbar spinal stenosis (LSS).
Methods
Patients and Follow-Up
This prospective, randomized trial was approved by the Institutional Review Board of the Catholic University of Korea, Seoul, St. Mary’s Hospital, College of Medicine (KC15OISI0594). A total of 52 patients were enrolled from May 2016 to September 2021 in this study after providing written informed consent. The inclusion criteria were as follows: 1) symptomatic single-level LSS with symptoms, such as radiculopathy and neurogenic intermittent claudication, and 2) radiologically diagnosed lumbar spinal stenosis (LSS) based on magnetic resonance imaging (MRI). The exclusion criteria were 1) spondylolisthesis with slippage of 50% or greater, 2) previous surgery at the same level, 3) lumbar degenerative scoliosis (Cobb angle > 20°), 4) non-degenerative stenosis but intervertebral disc herniation, 5) additional spinal disease at the same level of stenosis (ankylosing spondylitis, tumor, compression fracture, etc.), and 6) psychiatric disease (dementia, mental retardation, severe drug addiction, etc.).
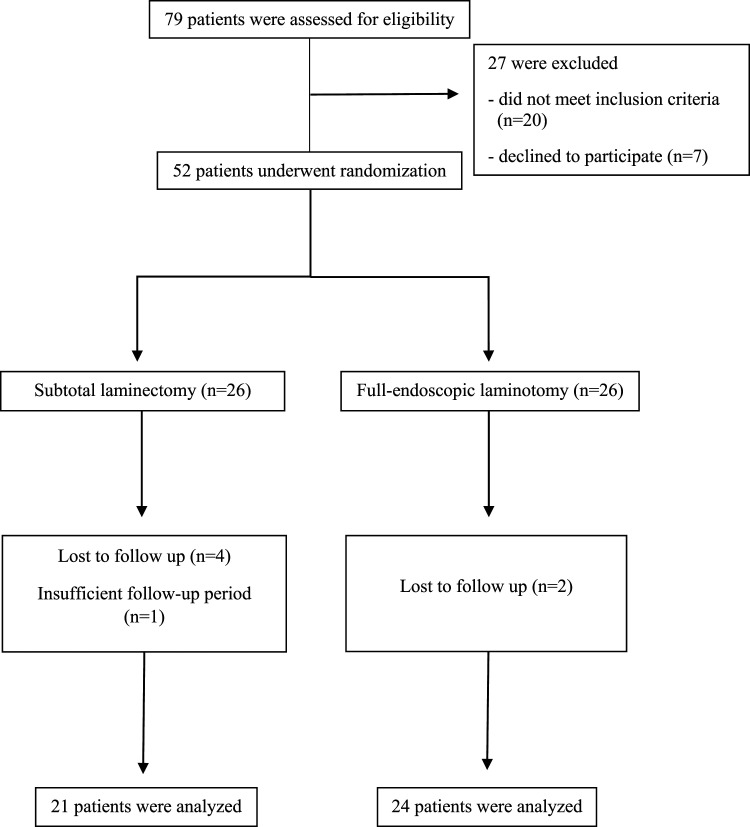
The authors investigated 45 patients who were followed up for more than 6 months (Figure 1). The preoperative VAS rating for the back and leg and ODI were recorded at the outpatient clinic. The clinical research coordinator (CRC), who was blinded to the allocation, recorded postoperative VAS of the back and leg) and ODI at 1, 3, 6 months and the final follow-up after surgery. In addition, the CRC investigated the following three items at the time of the final follow-up:1) satisfaction score, rated on a scale from 0 to 100; 2) ability to maintain daily activity; and 3) patients recommendation of surgery to others suffering from the same disease. Two spine clinical fellows investigated the radiologic features on the pre and postoperative follow-up radiographs and postoperative computed tomography (CT) and MRI at the last follow-up.
Figure 1.
Enrollment to follow-up flow diagram.
Randomization
Allocation of patients by the surgical method was performed through sealed envelopes 1 day before the surgery using a randomized method. The researcher performed the appropriate operation according to randomization. Randomization was performed by the CRC to minimize bias, and the operator was notified of the surgical assignment 1 day before surgery.
Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows (version 19.0; IBM Co. Somers, NY, USA). The Mann–Whitney U test was used to determine statistical differences in demographic data, preoperative clinical characteristics, and degree of clinical improvement between the groups. The Wilcoxon signed rank test was performed to compare pre and postoperative VAS and ODI scores in both groups to confirm surgical effectiveness. For radiological parameters, the intraclass correlation coefficient (ICC) was calculated to assess the reliability of the measurement. ICC for the intra- and inter-observer reliability varied within .88 – .93 (P < .01) and .91 – .95 (P < .01), respectively. Statistical significance was set at P < .05.
Surgical Technique
A single surgeon, who had sufficient experience with both endoscopic and open decompression surgeries, performed the operations under general anesthesia. STL was performed as a classic open laminectomy as previously described. 13 In STL differs from total laminectomy in that central laminectomy is performed while preserving both facet joints as much as possible while leaving the upper part of the spinous process and lamina. FEL was performed as previously described.14-17 Briefly, a skin incision of less than 1 cm was made on the symptomatic or severe side, the obturator and the working cannula were docked in the interlaminar space in sequence, and laminotomy was performed for the stenotic lesion using an endoscope.
Results
Patient Demographics
A total of 79 patients were assessed for eligibility; 20 patients did not meet the inclusion criteria and seven patients declined to participate. Finally, 52 patients were enrolled and underwent a randomization procedure for inclusion in either the STL or FEL surgical groups. Clinical and radiological analyses were performed in 45 patients (21 with STL and 24 with FEL). Six patients were lost to follow-up and one patient was excluded due to insufficient follow-up period. The characteristics of the two groups were assessed preoperatively (Table 1). At the time of surgery, the average age of the patients in the STL group was 66.4 ± 10.1 years, and the average age of patients in the FEL group was 64.3 ± 11.7 years. There were no significant differences in the characteristics between the two groups (P > .05). VAS scores for back and leg pain and ODI in the STL group before surgery were 5.0, 6.7, and 42.6, respectively. In the FEL group, the VAS scores for back and leg pain and ODI were 5.3, 7.3, and 52.9, respectively.
Table 1.
Patient demographics.
| STL | FEL | P-value a | |
|---|---|---|---|
| Number of patients | 21 | 24 | |
| Male/female ratio | 11/10 | 9/15 | |
| Age (years), mean±SD | 66.4 ± 10.1 | 64.3 ± 11.7 | .516 |
| Body mass index (kg/cm2), mean ± SD | 24.1 ± 3.4 | 26.1 ± 3.7 | .072 |
| Mean follow up period (months) | 21.2 ± 16.0 | 18.6 ± 11.8 | .845 |
| Operation level, N (%) | |||
| L3-4 | 0 | 4 (18%) | |
| L4-5 | 19 (95%) | 16 (73%) | |
| L5-S1 | 1 (5%) | 2 (9%) | |
| Charlson Comorbidity Index (CCI) | 1.1 ± 1.1 | 1.1 ± 1.5 | .549 |
| Preoperative VAS for back pain | 5.0 ± 2.7 | 5.3 ± 2.4 | .630 |
| Preoperative VAS for leg pain | 6.7 ± 1.7 | 7.3 ± 1.7 | .285 |
| Preoperative ODI | 42.6 ± 22.0 | 52.9 ± 16.3 | .185 |
| Preoperative lumbar lordosis (º) | 49.5 ± 10.0 | 44.0 ± 9.4 | .023 |
| Preoperative segmental lordosis (º) | 18.6 ± 4.5 | 15.8 ± 4.8 | .046 |
| Preoperative CSA (mm2) | 58.5 ± 21.6 | 60.4 ± 22.5 | .880 |
| b Preoperative central stenosis grade, N (%) | |||
| Grade B | 4 (19%) | 3 (13%) | |
| Grade C | 13 (62%) | 17 (71%) | |
| Grade D | 4 (19%) | 3 (13%) | |
aAll statistical analyses were performed by Mann– Whitney U-test.
bPreoperative central stenosis grading was classified based on Schizas grade.
Abbreviations: STL, subtotal laminectomy; FEL, full-endoscopic laminotomy; VAS, visual analogue scale; ODI, Oswestry Disability Index; CSA, cross-sectional area.
Clinical Outcomes
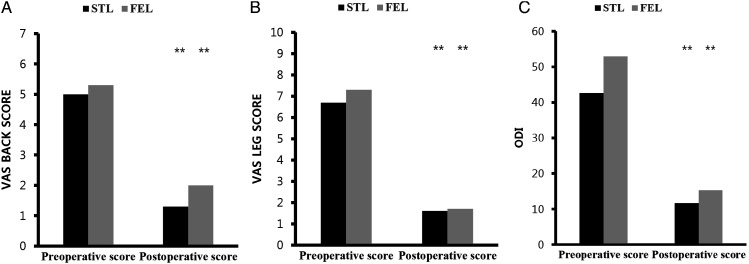
The mean follow-up duration was 21.2 months for the STL group and 18.6 months for the FEL group, respectively. There were significant improvements in the VAS and ODI scores after the operation in both the groups (Figure 2).
Figure 2.
Clinical status assessment. Graph showing preoperative and postoperative mean VAS back scores (A), VAS leg scores (B), and ODI scores (C) for both the STL (black) and FEL (gray) groups. Footnotes* Wilcoxon signed-rank test was used. ** Significant difference, P-value < .005. STL, subtotal laminectomy; FEL, full-endoscopic laminotomy; VAS, visual analogue scale; ODI, Oswestry Disability Index
After operation in the STL group, the mean pre- and postoperative VAS score changed from 5.0 ± 2.7 to 1.3 ± 1.3 (back) and 6.7 ± 1.7 to 1.6 ± 2.1 (leg), respectively, and the mean ODI changed from 42.6 ± 22.0 to 11.6 ± 15.0. Similar results were observed in the FEL group. The mean pre- and postoperative VAS score changed from 5.3 ± 2.4 to 2.0 ± 2.2 (back), 7.3 ± 1.7 to 1.7 ± 2.1 (leg), respectively, and the mean ODI improved from 52.9 ± 16.3 to 15.3 ± 15.3 (all P-value < .05). There was no significant difference between the two groups in terms of either VAS or ODI changes postoperatively (Table 2). However, there was a difference in the mean postoperative length of stay. There was no specific protocol for deciding when the patient should be discharged from the hospital; the patient was discharged with consent from the patient when they were judged to be clinically stable. The group of patients who underwent endoscopic surgery tended to have shorter hospital stays; mean postoperative length of stay was 4.8 ± 1.5 days in the STL group and 3.8 ± 1.8 days in the FEL group.
Table 2.
Clinical outcome VAS for back, leg pain and ODI.
| 1 month | STL | FEL | P-value a |
|---|---|---|---|
| VAS for back pain | 1.4 ± 1.9 | 1.5 ± 1.6 | .693 |
| VAS for leg pain | 1.8 ± 2.0 | 1.9 ± 2.0 | .988 |
| ODI | 27.0 ± 19.4 | 24.3 ± 11.7 | .919 |
| 3 months | |||
| VAS for back pain | 1.8 ± 2.0 | 2.4 ± 2.3 | .472 |
| VAS for leg pain | 1.9 ± 1.5 | 2.6 ± 2.8 | .821 |
| ODI | 22.8 ± 19.0 | 26.0 ± 18.5 | .596 |
| 6 months | |||
| VAS for back pain | 1.7 ± 1.7 | 1.3 ± 1.1 | .682 |
| VAS for leg pain | 2.0 ± 2.6 | 1.5 ± 1.6 | .984 |
| ODI | 20.4 ± 17.6 | 18.8 ± 14.0 | .984 |
| Last follow-up | |||
| VAS for back pain | 1.3 ± 1.3 | 2.0 ± 2.2 | .407 |
| VAS for leg pain | 1.6 ± 2.1 | 1.7 ± 2.1 | .649 |
| ODI | 11.6 ± 15.0 | 15.3 ± 15.3 | .220 |
| Changes after surgery | |||
| VAS for back pain | 3.6 ± 2.1 | 3.3 ± 3.4 | .776 |
| VAS for leg pain | 5.0 ± 2.6 | 5.6 ± 2.2 | .522 |
| ODI | 31.0 ± 22.6 | 36.8 ± 18.4 | .511 |
| Mean postoperative length of stay (days) | 4.8 ± 1.5 | 3.8 ± 1.8 | .033 |
| Satisfaction rate (0 – 100) | 87.1 ± 16.9 | 79.1 ± 24.8 | .343 |
| Return todaily activity (%) | 100 | 91 | |
| Recommendation to others (%) | 90 | 82 | |
aAll statistical analyses were performed by Mann– Whitney U test.
All results included in the table were expressed as mean ± standard deviation.
Abbreviations: STL, subtotal laminectomy; FEL, full-endoscopic laminotomy; VAS, visual analogue scale; ODI, Oswestry Disability Index.
Radiologic Outcomes
We compared the preoperative radiograph and the last radiograph that could be identified during postoperative follow-up in all patients included in the study. All radiographs were compared after at least 6 months, and the average follow-up period was 20.5 months for the STL group and 19.5 months for the FEL group. The mean follow-up duration for all the patients was 20 months.
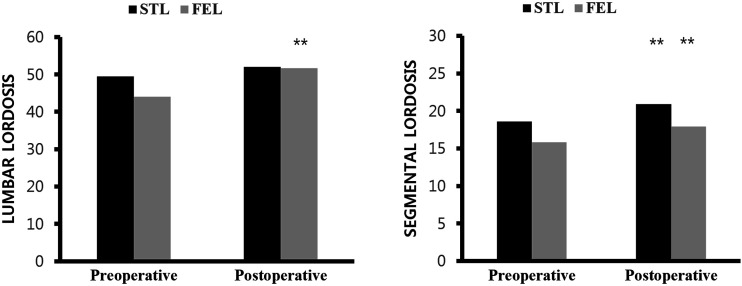
First, we measured and compared the pre and postoperative lumbar lordosis and segmental angles between the two groups (Table 3). Interestingly, a statistically significant increase in postoperative lumbar lordosis and segmental angle was observed in the FEL group and both the groups, respectively (Figure 3).
Table 3.
Radiologic outcome.
| STL | FEL | P-value a | |
|---|---|---|---|
| Preoperative LL (°) | 49.5 ± 10.0 | 44.0 ± 9.4 | .023 |
| Postoperative LL (°) | 52.0 ± 10.1 | 51.7 ± 7.3 | .799 |
| LL difference | 2.5 ± 5.3 | 7.7 ± 7.4 | .020 |
| Preoperative SL (°) | 18.6 ± 4.5 | 15.8 ± 4.8 | .046 |
| Postoperative SL (°) | 20.9 ± 5.0 | 17.9 ± 5.4 | .046 |
| SL difference | 2.3 ± 2.9 | 2.1 ± 2.7 | .295 |
| Preoperative DH (mm) | 10.3 ± 2.2 | 9.8 ± 2.6 | .540 |
| Postoperative DH (mm) | 9.8 ± 2.6 | 9.6 ± 2.6 | .604 |
| DH difference | .5 ± 0.9 | .2 ± 0.6 | .076 |
| Facet joint orientation (°) | 39.6 ± 10.7 | 35 ± 10.8 | .358 |
| Facet joint preservation rate (%) | 88.5 ± 7.3 | 93.3 ± 7.5 | .019 |
All statistical analyses were performed by Mann–Whitney U test.
All results included in the table were expressed as mean ± standard deviation.
Abbreviations: STL, subtotal laminectomy; FEL, full-endoscopic laminotomy; LL, Lumbar lordosis; SL, Segmental lordosis; DH, Disc height; LL difference = (postoperative LL – preoperative LL); SL difference = (postoperative SL – preoperative SL); DH difference = (preoperative DH – postoperative DH).
Figure 3.
Radiologic status assessment. Graph showing preoperative and postoperative mean LL (left), and SL (right) for both the STL (black) and FEL (gray) groups. Footnotes* Wilcoxon signed-rank test was used** Significant difference, p-value < 0.005.STL, subtotal laminectomy; FEL, full-endoscopic laminotomy; LL, Lumbar lordosis; SL, Segmental lordosis
In the STL group, although there was a tendency for increased postoperative lumbar lordosis, the result was not statistically significant. In addition, when comparing the difference in lumbar lordosis (LL difference = postoperative LL – preoperative LL), it was confirmed that lumbar lordosis improved by a significantly larger difference after surgery in the FEL group. We also investigated the presence of preoperative spondylolisthesis on patients’ radiographs and iatrogenic spondylolisthesis after surgery. Spondylolisthesis was defined as slippage of at least 2 mm on imaging.
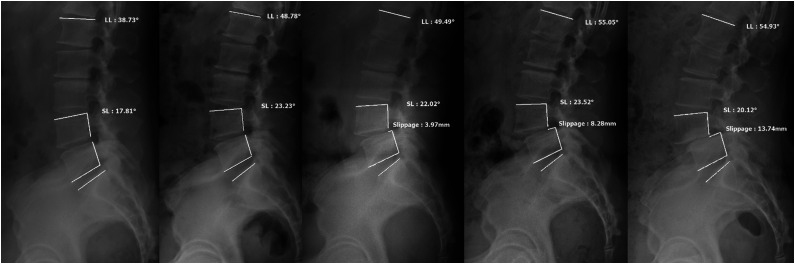
Fifteen of the 45 patients had preoperative spondylolisthesis (Table 4). Spondylolisthesis was exacerbated or newly developed in five of 21 patients (24%), and no patient showed improvement in slippage greater than 2 mm in the STL group (Figure 4). In contrast, improvement in spondylolisthesis was observed in two of 24 patients (8%), and no patient showed slippage worsening more than 2 mm in the FEL group. The degree of postoperative slippage decreased in two of 10 FEL patients (20%) who showed preoperative spondylolisthesis, including retrolisthesis (Figure 5).
Table 4.
The changes in spondylolisthesis.
| Group | Preoperative Spondylolisthesis | Postoperative Spondylolisthesis | |
|---|---|---|---|
| 1 | STL | None | Grade II (13.7 mm) |
| 2 | STL | None | Grade I (5.1 mm) |
| 3 | STL | None | Grade I (2.6 mm) |
| 4 | STL | 5.0 mm | 9.2 mm |
| 5 | STL | 8.6 mm | 10.7 mm |
| 6 | STL | 6.2 mm | 6.8 mm |
| 7 | STL | 4.9 mm | 4.9 mm |
| 8 | STL | 7.3 mm | 7.3 mm |
| 9 | FEL | 7.5 mm | 5.0 mm |
| 10 a | FEL | 7.5 mm | 5.5 mm |
| 11 | FEL | 4.0 mm | 4.0 mm |
| 12 | FEL | 3.3 mm | 4.7 mm |
| 13 | FEL | 3.2 mm | 1.7 mm |
| 14 | FEL | 5.3 mm | 5.2 mm |
| 15 | FEL | 5.5 mm | 5.7 mm |
| 16 | FEL | 6.4 mm | 6.4 mm |
| 17 | FEL | 7.4 mm | 6.0 mm |
| 18 | FEL | 4.5 mm | 3.1 mm |
aRetrolisthesis case.
Abbreviations: STL, subtotal laminectomy; FEL, full-endoscopic laminotomy.
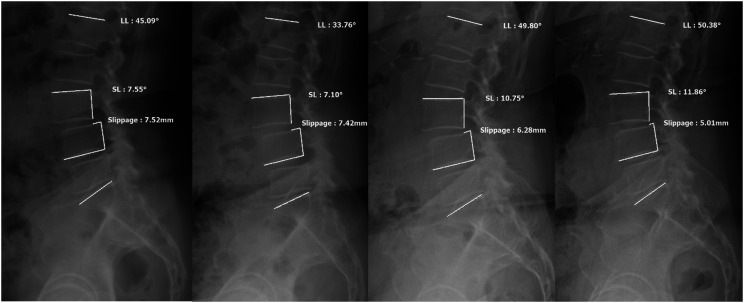
Figure 4.
One patient (serial number 3, subtotal laminectomy [STL] group) had no preoperative spondylolisthesis but grade I spondylolisthesis is newly observed after surgery (From the left, preoperative, postoperative, 6 months, 1 year, 5 years later. In a separate, visual analogue scale [VAS] back and leg, Oswestry Disability Index [ODI] improved from 6, 7, 52 to 0, 0, 4, respectively at the last follow-up).
Figure 5.
In one case (serial number 27, full-endoscopic laminotomy [FEL] group), spondylolisthesis was present before surgery, but slight improvement in spondylolisthesis is observed on serial follow-up images after surgery. (From the left, preoperative, postoperative, 3 months, 17 months later. In a separate, visual analogue scale [VAS] back, leg, and Oswestry Disability Index [ODI] improved from 2, 8, 52 to 3, 3, 14, respectively at the last follow-up).
In the STL group, the degree of slippage increased by an average of 3.6 mm after surgery, and the difference was statistically significant (P = .028). In the FEL group, a reduction of approximately 1 mm in slippage was observed after surgery, but the difference was not statistically significant (Table 5).
Table 5.
Comparison between groups: the changes in spondylolisthesis.
| STL (n = 8) | P-value a | FEL (n = 10) | P-value a | |||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | |||
| Slippage (mm) | 4.0 ± 3.5 | 7.6 ± 3.5 | .028 | 5.7 ± 1.6 | 4.7 ± 1.6 | .074 |
| Difference | 3.5 ± 4.5 | −1.0 ± 1.4 | 0.009‡ | |||
aWilcoxon signed rank test was used for comparing changes between pre and postoperative score within groups.
Mann–Whitney U test was used for comparing changes within groups.
Abbreviations: STL, subtotal laminectomy; FEL, full-endoscopic laminotomy.
We also confirmed that the disc height of the STL group and the FEL group decreased gradually from 10.3 and 9.8 mm, respectively, to 9.8 and 9.6 mm at the last follow-up after surgery, which was not statistically significant (Table 3).
We performed MRI scans after surgery and compared them with preoperative images (Table 6). To check the degree of dural sac expansion at the mid-disc level after surgery, we measured the cross-sectional area (CSA) and recorded the expansion rate compared to the preoperative value. Among the 45 patients, postoperative MRI was performed in 43 patients (one patient who could not be taken for MRI owing to personal reasons and another, who had an implantable pulse generator underwent a myelo CT scan instead). For 35 patients (78%), MRI or myelo CT scans were performed within 1 month. Due to personal reasons, five patients underwent MRI within 3 months and four between 1 and 2 years. In majority of the patients, overall central canal widening was assessed to confirm radiologic improvement based on the Schizas grade. 18 In both groups, the expansion of the CSA after surgery was statistically significant. When comparing the average expansion rates, it was confirmed that the STL group increased by approximately 51.1% more than the FEL group, but it wasn’t statistically significant. In addition, early complications, such as hematoma or recurrence, were identified. The authors investigated the orientation of the facet joint and facet preservation rate of the surgery through a CT comparison before and after surgery (Table 3). To confirm the orientation of the facet joint, the measurement method was selected according to a previously published paper. 19 The angles of the facet joints on both sides were measured and the average value was obtained. The angles of the facet joints in the STL group was confirmed to be 39.6 ± 10.7 °and the FEL group was 35 ± 10.8 °. In addition, the preoperative and postoperative areas of the facet joint were obtained and compared to determine the facet joint preservation rate according to the surgical method. The area of the inferior/superior articular process in the axial CT image, based on the upper endplate of the caudal level, was calculated. The facet preservation rate of the STL group was 88.5 ± 7.3%, and that in the FEL group was 93.3 ± 7.5%, and there was a statistically significant difference between the two groups. (P = .019).
Table 6.
The changes in central canal stenosis.
| STL | FEL | P-value | |||
|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | ||
| B a | 4 (19%) | 11 (55%) | 3 (13%) | 12 (55%) | |
| C a | 13 (62%) | 0 | 17 (72%) | 2 (9%) | |
| D a | 4 (19%) | 0 | 3 (13%) | 0 | |
| CSA (mm2) | 58.5 ± 21.6 | 119.0 ± 28.8 | 60.4 ± 22.5 | 102.8 ± 35.1 | < .005 b |
| CSA expansion rate (%) | 234.7 ± 116.4 | 183.6 ± 14.7 | .110‡ | ||
aThe degree of central canal stenosis was evaluated based on Schizas grade.
bWilcoxon signed rank test was used to confirm the CSA expansion effect of two surgeries.
Mann–Whitney U test was used for comparing changes between the two groups.
Abbreviations: STL, subtotal laminectomy; FEL, full-endoscopic laminotomy; CSA, cross-sectional area.
Complications
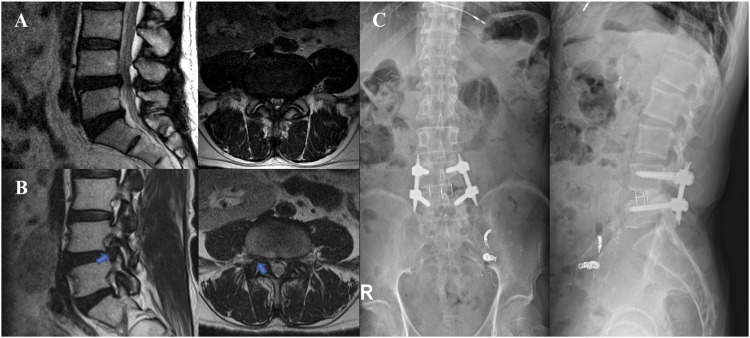
No dural tear occurred intraoperatively; however, some complications occurred. One patient (serial number 18, FEL group) was diagnosed with an asymptomatic hematoma on postoperative MRI one day after the operation, but the hematoma resolved spontaneously on follow-up MRI 4 months later. In one patient (serial number 25, FEL group), an operation-level mismatch occurred, and repeat surgery was performed. Acute embolic cerebral infarction occurred in one patient (serial number 23, STL group), but there were no persistent sequelae, and the patient was able to return to daily living without disability. In one patient in the STL group (serial number 43), an asymptomatic synovial cyst was identified at the same level on an MRI 1 year later. Also, two patients (1 from STL group and 1 from FEL group) underwent fusion surgery during the follow-up period. One patient (serial number 20, FEL group) received FEL for radiating pain in the left leg in 2016. After this radicular pain improved, the patient underwent fusion surgery after diagnosis of right foraminal disc extrusion with newly developed radiating pain in the right leg after 17 months (Figure 6). One patient (serial number 6, STL group) underwent open decompression surgery in 2016; after 2 years without pain, right leg pain reoccurred, for which fusion surgery was conducted 4 years later.
Figure 6.
A patient (serial number 20, full-endoscopic laminotomy [FEL] group) underwent FEL for the left leg radiating pain in 2016, which improved; however, he had to undergo fusion surgery after diagnosis of right foraminal disc extrusion with newly developed right leg radiating pain after 17 months. (A: preoperative magnetic resonance imaging, B: 17 months later, C: postoperative radiographs).
Discussion
Over the past decade, minimally invasive decompressive surgery has become popular for the treatment of various lumbar spinal disorders. Studies using various techniques have compared existing and new minimally invasive surgical methods, and many surgeons are now performing less invasive surgery.20,21 However, randomized controlled trials are relatively difficult to perform; hence, the actual number of studies that can clearly suggest treatment directions for surgeons is insufficient. In addition, there are studies comparing endoscopic and other surgical methods, but the number of randomized controlled trials comparing conventional subtotal laminectomy with endoscopic laminotomy is insufficient.
In this randomized controlled trial, which included 45 patients with single-level LSS, we compared the clinical outcomes between classic open STL and FEL more than 6 months after surgery. Significant postoperative improvements in low back and radiating pain, and ODI were confirmed in both the groups and within groups. In addition, there was no statistical difference in the degree of improvement after surgery between the two groups, confirming that FEL had a similar surgical effect as STL. In addition, the difference between the two groups was confirmed in the postoperative length of stay, which was 1 day shorter for FEL than STL. These results are consistent with the previous studies.14,22-25 However, we believe that the absence of a well-established discharge protocol can lead to a risk of bias. Recording and comparing postoperative progress, such as surgical site pain immediately after surgery, is required to explain this difference, and omission of this comparison is a limitation of this study.
The difference in lumbar lordosis after surgery was significantly larger in the FEL group. This is probably because of the large degree of improvement in sagittal alignment due to relatively low preoperative lumbar lordosis in the FEL group. Overall, lumbar lordosis and segmental angle increased after surgery, and when the Wilcoxon signed rank test was performed to determine significant differences in lumbar and segmental lordosis after surgery in each group, postoperative lumbar lordosis in the FEL group and segmental lordosis in both groups increased significantly. This finding is consistent with previously published studies.26-28 Hatakka et al. 26 concluded that decompression can have a small but statistically significant effect on sagittal alignment, including lumbar lordosis. However, they also reported that the clinical impact of this effect was probably insignificant. Considering studies28,29 that show a relationship between thoracolumbar spine alignment and the clinical course, including back pain, we believe that improvement of alignment is an indicator of clinical improvement.
It is not clear why positive changes in the overall global sagittal alignment were confirmed in both groups after surgery, but we suspect that these changes were due to changes in posture due to reduced pain. Additional studies focusing on this outcome are needed to confirm the exact relationship and provide evidence.
A few studies have analyzed the relational aspects of spondylolisthesis and decompressive surgery.9,30 Here, we attempted to indirectly confirm the benefits of FEL in light of the finding that conventional subtotal laminectomy can worsen spondylolisthesis. In this study, 15 of 45 patients had mild spondylolisthesis, all of which involved less than 25% slippage (Meyerding grade I). Majority of the patients experienced no aggravation of spondylolisthesis, but more than 2 mm of slippage aggravation was confirmed in five of 21 patients (24%) in the STL group. In addition, two patients in the STL group had no preoperative spondylolisthesis but developed grade I or II spondylolisthesis during the follow-up period. On the other hand, slippage improved by more than 2 mm in two of 24 patients (8%) in the FEL group. The study by Kim 31 indicated that minimally invasive spine surgery for lumbar decompression has advantages in terms of reducing muscle crush injury and minimizing osseotendinous complex disruption compared to conventional open surgery. In comparison of the facet joint preservation rates between the two groups, it was confirmed that the rate was significantly higher in the FEL group than in the STL group. Based on these results, we hypothesized that endoscopic lumbar laminotomy has an advantage over open subtotal laminectomy in terms of preventing iatrogenic spondylolisthesis after surgery by minimizing damage to facet joints and musculotendinous structures. However, since the number of samples was small, a study with a larger sample is needed.
In this study, complications occurring during the follow-up period were described for all eligible patients. There were no complications that resulted in fatal sequelae, and no significant difference in complication rates between the two groups.
Study Limitations
The limitations of this study are as follows:1) the relatively small sample size and as such these are preliminary results; 2) a short follow-up period (mean follow-up duration was 19.8 months, but some patients whose symptoms improved after surgery did not visit the hospital after 6 months); 3) unknown degree of early postoperative surgical site pain or difference in use of painkillers; and 4) unfortunately, the authors made a single-level mismatch error in the endoscopy group during this study. After a few days, surgery was performed on the right segment that was originally planned to correct this mistake, but this mistake will definitely affect the results and is a major limitation of this study. Further studies are required to address these limitations and reduce future confusion regarding the establishment of surgical methods.
Conclusions
In summary, FEL showed clinical results similar to STL in LSS, including the complication rate. In addition, the results of FEL were superior to those of STL in terms of a decrease in the postoperative length of stay and radiologic instability, such as iatrogenic spondylolisthesis. The results of this study indicate that FEL is a comparable surgical method to STL for LSS.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The corresponding author, Jin-Sung Kim, is a consultant of RIWOSPINE, Gmbh, Germany, Elliquence, LLC, USA. The other authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research is supported by a grant from Korea’s Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (Grant Number: HC20C0163).
ORCID iD
Jin-Sung Kim https://orcid.org/0000-0001-5086-0875
References
- 1.Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys. Spine (Phila Pa 1976). 2002;31(23):2724-2727. doi: 10.1097/01.brs.0000244618.06877.cd. [DOI] [PubMed] [Google Scholar]
- 2.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259-1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costa F, Sassi M, Cardia A, et al. Degenerative lumbar spinal stenosis: analysis of results in a series of 374 patients treated with unilateral laminotomy for bilateral microdecompression. J Neurosurg Spine. 2007;7(6):579-586. doi: 10.3171/SPI-07/12/579. [DOI] [PubMed] [Google Scholar]
- 4.Rosen DS, O'Toole JE, Eichholz KM, et al. Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery. 2007;60(3):503-509. doi: 10.1227/01.NEU.0000255332.87909.58. [DOI] [PubMed] [Google Scholar]
- 5.Demirayak M, Sisman L, Turkmen F, et al. Clinical and radiological results of microsurgical posterior lumbar interbody fusion and decompression without posterior instrumentation for lateral recess stenosis. Asian Spine J. 2015;9(5):713-720. doi: 10.4184/asj.2015.9.5.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uehara M, Takahashi J, Hashidate H, et al. Comparison of spinous process-splitting laminectomy versus conventional laminectomy for lumbar spinal stenosis. Asian Spine J. 2014;8(6):768-776. doi: 10.4184/asj.2014.8.6.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dohzono S, Toyoda H, Matsumura A, Terai H, Suzuki A, Nakamura H. Clinical and radiological outcomes after microscopic bilateral decompression via a unilateral approach for degenerative lumbar disease: minimum 5-Year follow-up. Asian Spine J. 2017;11(2):285-293. doi: 10.4184/asj.2017.11.2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mobbs RJ, Li J, Sivabalan P, Raley D, Rao PJ. Outcomes after decompressive laminectomy for lumbar spinal stenosis: comparison between minimally invasive unilateral laminectomy for bilateral decompression and open laminectomy: clinical article. J Neurosurg Spine. 2014;21(2):179-186. doi: 10.3171/2014.4.SPINE13420. [DOI] [PubMed] [Google Scholar]
- 9.Fox MW, Onofrio BM, Onofrio BM, Hanssen AD. Clinical outcomes and radiological instability following decompressive lumbar laminectomy for degenerative spinal stenosis: a comparison of patients undergoing concomitant arthrodesis versus decompression alone. J Neurosurg. 1996;85(5):793-802. doi: 10.3171/jns.1996.85.5.0793. [DOI] [PubMed] [Google Scholar]
- 10.Popov V, Anderson DG. Minimal invasive decompression for lumbar spinal stenosis. Adv Orthop. 2012;2012:645321-645325. doi: 10.1155/2012/645321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee CW, Yoon KJ, Jun JH. Percutaneous endoscopic laminotomy with flavectomy by uniportal, unilateral approach for the lumbar canal or lateral recess stenosis. World Neurosurg. 2018;113:e129-e137. doi: 10.1016/j.wneu.2018.01.195. [DOI] [PubMed] [Google Scholar]
- 12.McGrath LB, White-Dzuro GA, Hofstetter CP. Comparison of clinical outcomes following minimally invasive or lumbar endoscopic unilateral laminotomy for bilateral decompression. J Neurosurg Spine. 2019;30:1-9. doi: 10.3171/2018.9.SPINE18689. [DOI] [PubMed] [Google Scholar]
- 13.Ghogawala Z, Benzel EC, Amin-Hanjani S, et al. Prospective outcomes evaluation after decompression with or without instrumented fusion for lumbar stenosis and degenerative Grade I spondylolisthesis. J Neurosurg Spine. 2004;1(3):267-272. doi: 10.3171/spi.2004.1.3.0267. [DOI] [PubMed] [Google Scholar]
- 14.Komp M, Hahn P, Oezdemir S, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Physician. 2015;18(1):61-70. [PubMed] [Google Scholar]
- 15.Lim KT, Meceda EJA, Park CK. Inside-out approach of lumbar endoscopic unilateral laminotomy for bilateral decompression: a detailed technical description, rationale and outcomes. Neurospine. 2020;17(Suppl 1):S88-S98. doi: 10.14245/ns.2040196.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoshikane K, Kikuchi K, Okazaki K. Clinical outcomes of selective single-level lumbar endoscopic unilateral laminotomy for bilateral decompression of multilevel lumbar spinal stenosis and risk factors of reoperation. Global Spine J. 2021;1:21925682211033575. doi: 10.1177/21925682211033575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim HS, Wu PH, Jang I-T. Clinical results And review of techniques of lumbar endoscopic unilateral laminotomy with bilateral decompression (LE-ULBD) for lumbar stenosis. J Minim Invasive Spine Surg Tech. 2021;6(Suppl 1):S117-S122. doi: 10.21182/jmisst.2021.00038. [DOI] [Google Scholar]
- 18.Schizas C, Theumann N, Burn A, et al. Qualitative grading of severity of lumbar spinal stenosis based on the morphology of the dural sac on magnetic resonance images. Spine. 2010;35(21):1919-1924. doi: 10.1097/BRS.0b013e3181d359bd. [DOI] [PubMed] [Google Scholar]
- 19.Kong MH, He W, Tsai YD, et al. Relationship of facet tropism with degeneration and stability of functional spinal unit. Yonsei Med J. 2009;50(5):624-629. doi: 10.3349/ymj.2009.50.5.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thome C, Zevgaridis D, Leheta O, et al. Outcome after less-invasive decompression of lumbar spinal stenosis: a randomized comparison of unilateral laminotomy, bilateral laminotomy, and laminectomy. J Neurosurg Spine. 2005;3(2):129-141. doi: 10.3171/spi.2005.3.2.0129. [DOI] [PubMed] [Google Scholar]
- 21.Alimi M, Hofstetter CP, Pyo SY, Paulo D, Hartl R. Minimally invasive laminectomy for lumbar spinal stenosis in patients with and without preoperative spondylolisthesis: clinical outcome and reoperation rates. J Neurosurg Spine. 2015;22(4):339-352. doi: 10.3171/2014.11.SPINE13597. [DOI] [PubMed] [Google Scholar]
- 22.Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine. 2009;10(5):476-485. doi: 10.3171/2008.7.17634. [DOI] [PubMed] [Google Scholar]
- 23.Park SM, Park J, Jang HS, et al. Biportal endoscopic versus microscopic lumbar decompressive laminectomy in patients with spinal stenosis: a randomized controlled trial. Spine J. 2020;20(2):156-165. doi: 10.1016/j.spinee.2019.09.015. [DOI] [PubMed] [Google Scholar]
- 24.Kang T, Park SY, Kang CH, Lee SH, Park JH, Suh SW. Is biportal technique/endoscopic spinal surgery satisfactory for lumbar spinal stenosis patients?: A prospective randomized comparative study. Medicine (Baltimore). 2019;98(18):e15451. doi: 10.1097/MD.0000000000015451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heo DH, Lee DC, Park CK. Comparative analysis of three types of minimally invasive decompressive surgery for lumbar central stenosis: biportal endoscopy, uniportal endoscopy, and microsurgery. Neurosurg Focus. 2019;46(5):E9. doi: 10.3171/2019.2.FOCUS197. [DOI] [PubMed] [Google Scholar]
- 26.Hatakka J, Pernaa K, Rantakokko J, Laaksonen I, Saltychev M. Effect of lumbar laminectomy on spinal sagittal alignment: a systematic review. Eur Spine J. 2021;30(9):2413-2426. doi: 10.1007/s00586-021-06827-y. [DOI] [PubMed] [Google Scholar]
- 27.Fujii K, Kawamura N, Ikegami M, Niitsuma G, Kunogi J. Radiological improvements in global sagittal alignment after lumbar decompression without fusion. Spine (Phila Pa. 2015;40(10):703-709. doi: 10.1097/BRS.0000000000000708. [DOI] [PubMed] [Google Scholar]
- 28.Salimi H, Toyoda H, Yamada K, et al. The effect of minimally invasive lumbar decompression surgery on sagittal spinopelvic alignment in patients with lumbar spinal stenosis: a 5-year follow-up study. J Neurosurg Spine. 2021;1:1-8. doi: 10.3171/2020.11.SPINE201552. [DOI] [PubMed] [Google Scholar]
- 29.Hira K, Nagata K, Hashizume H, et al. Relationship of sagittal spinal alignment with low back pain and physical performance in the general population. Sci Rep. 2021;11(1):20604. doi: 10.1038/s41598-021-00116-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jonsson B, Annertz M, Sjoberg C, Stromqvist B. A prospective and consecutive study of surgically treated lumbar spinal stenosis. Part II: Five-year follow-up by an independent observer. Spine (Phila Pa. 1997;22(24):2938-2944. doi: 10.1097/00007632-199712150-00017. [DOI] [PubMed] [Google Scholar]
- 31.Kim CW. Scientific basis of minimally invasive spine surgery: prevention of multifidus muscle injury during posterior lumbar surgery. Spine (Phila Pa. 2010;35(26 Suppl):S281-S286. doi: 10.1097/BRS.0b013e3182022d32. [DOI] [PubMed] [Google Scholar]