Abstract
Importance:
Healthcare personnel (HCP) are important messengers for promoting vaccines, for both adults and children. Our investigation describes perceptions of fully vaccinated HCP about COVID-19 vaccine for themselves and primary series for their children.
Objective:
To determine associations between sociodemographic, employment characteristics and perceptions of COVID-19 vaccines among HCP overall and the subset of HCP with children, who were all mandated to receive a COVID-19 vaccine, in a large US metropolitan region.
Design:
Cross-sectional survey of fully vaccinated HCP from a large integrated health system.
Setting:
Participants were electronically enrolled within a multi-site NYS healthcare system from December 21, 2021, to January 21, 2022.
Participants:
Of 78,000 employees, approximately one-third accessed promotional emails; 6,537 employees started surveys and 4165 completed them. Immunocompromised HCP (self-reported) were excluded.
Exposure(s) (for observational studies):
We conducted a survey with measures including demographic variables, employment history, booster status, child vaccination status; vaccine recommendation, confidence, and knowledge.
Main outcome(s) and measures:
The primary outcome was COVID-19 vaccine hesitancy for all dose types − primary series or booster doses − among HCP.
Results:
Findings from 4,165 completed surveys indicated that almost 17.2 % of all HCP, including administrative and clinical staff, were hesitant or unsure about receiving a COVID-19 vaccine booster, despite the NYS recommendation to do so. Depending on age group, between 20 % and 40 % of HCP were hesitant about having their children vaccinated for COVID-19, regardless of clinical versus non-clinical duties. In multivariable regression analyses, lack of booster dose, unvaccinated children, females, income less than $50,000, and residence in Manhattan remained significantly associated with vaccine hesitancy.
Conclusions and relevance:
Despite mandated COVID-19 vaccination, a substantial proportion of HCP remained vaccine hesitant towards adult booster doses and pediatric COVID-19 vaccination. While provider recommendation has been the mainstay of combatting COVID-19 vaccine hesitancy, a gap exists between HCP—despite clinical or administrative status—and the ability to communicate the need for vaccination in a healthcare setting. While previous studies describe the HCP vaccine mandate as a positive force to overcome vaccine hesitancy, we have found that despite a mandate, there is still substantial COVID-19 vaccine hesitancy, misinformation, and reluctance to vaccinate children.
Keywords: Coronavirus disease 2019 (COVID-19), Vaccine hesitancy, Healthcare personnel, Employee health, Vaccine mandate, Vaccine education
1. Introduction
As demonstrated by a spike in hospitalizations in 2021–2022, coronavirus disease 20191 (COVID-19) Omicron wave disproportionately affected the pediatric population [1]. National pediatric COVID-19 vaccination rates for 5- to 11-year old children simultaneously remained low —approximately 30 %—despite availability since November 2021 [2]. Before the coronavirus disease 20191 (COVID-19) pandemic, studies of vaccine hesitancy focused on parental attitudes toward childhood immunizations and annual vaccinations such as influenza [3–5]. Because health care personnel2 (HCP) are important messengers to promote vaccines for both children and adults, vaccine hesitancy among HCP in the United States had focused on students and residents until the recent development of the COVID-19 vaccine [6]. Controversy existed among HCP regarding the New York State mandate to receive their primary COVID-19 vaccine series and an additional booster dose during the study period [7,8]. This study investigated the degree of and the contributing factors to vaccine hesitancy among HCP mandated to receive COVID-19 vaccine.
Vaccine hesitancy among HCP was initially described in France, highlighting the need for vaccine education to shift from patient to provider [9]. Several other studies from Finland, Netherlands, and Europe also revealed vaccine side effect concerns, lack of confidence discussing vaccines, and decreased vaccine acceptance by general practitioners and nurses [9–11]. General practitioners tend to readily vaccinate their own children yet are less likely to recommend vaccines for their patients [12,13]. Studies from France in early 2020 found discrepancies between type of HCP and vaccine acceptance; nurses and nurse assistants were less accepting than physicians [12]. Among pediatric HCP, decreased perception of risk of COVID-19 infection was noted among those who were most vaccine hesitant [14]. A survey of HCP in two US hospitals found that older age, Black or Hispanic race/ethnicity, history of COVID-19 testing, and less patient contact contributed to vaccine hesitancy [15]. In France, a lower medical literacy also contributed to vaccine hesitancy.
From 2020 to 2021, increased HCP COVID-19 vaccine uptake and acceptance was noted [16–18]. However, these studies do not address vaccine hesitancy among a population mandated to receive the COVID-19 vaccination. Intuitively, vaccine acceptance is equated with uptake; our study seeks to investigate if the data support this conclusion. In paradox to the healthy worker effect, HCP of minority racial and ethnic backgrounds are at increased risk for COVID-19 infection compared to the general community [19]. At the start of COVID-19 vaccine rollout, disparities in uptake was apparent. Nearly 20 % of Black adults said that they “definitely or probably would not get vaccinated.”[20] Young Black and Hispanic adults are less likely than Whites to have received a COVID-19 vaccine and are more likely to want to “wait and see.”[20] While initial trends in vaccine uptake were reduced in HCP generally and, notably, in people of color, overall acceptance improved with the US Food and Drug Administration’s emergency use authorization [21,22]. Race continued to be a factor for COVID-19 vaccination uptake as the pandemic progressed [23,24], with notable race/ethnicity differences among HCP who are fully vaccinated under COVID-19 vaccine mandates [20,25]. Our study further investigates the downstream effect of instituting mandates on the perception of COVID-19 vaccine.
Vaccine hesitancy among parents of patients in a children’s hospital found that social determinants of health, such as limited resources, impacted parental vaccine hesitancy for childhood vaccines but not for the influenza vaccine [26]. Over a quarter of mothers said that they were “extremely unlikely” to COVID-19 vaccinate their teenage children and parental attitudes around vaccinating their children were correlated with attitudes around vaccinating themselves [27]. What is unknown is whether HCP with children are as hesitant towards COVID-19 vaccine as the general population. With this study, our aim was to determine associations between sociodemographic, employment characteristics and perceptions of COVID-19 vaccines among HCP mandated to receive COVID-19 vaccine and the subset of HCP with children in a large US metropolitan region.
2. Material and methods
2.1. Study population
The study population was HCP and a subset of HCP with children, from New York State’s largest private employer and integrated health delivery system. This network comprises 23 hospitals and over 800 ambulatory facilities with over 78,000 employees serving over 2 million patients through 5.5 million patient encounters annually, across a large geographic area that includes northern New York, Long Island, and all boroughs of New York City. The health system serves a diverse patient population, with more than 170 languages spoken in Queens County, New York alone. New York State mandated that all personnel, regardless of job category and title, receive the first dose of the primary COVID-19 vaccine series by September 27th, 2021 as a requirement for employment. There were 85 medical and 153 religious exemptions granted in our study population. In addition, 1,152 HCP were terminated from employment due to the vaccine mandate by the end of the 2021. At the time of the study the booster dose was strongly recommended but not yet required; a mandate for requirement was scheduled at the end of the study period on January 21st, 2022 to be completed by February 21st. The mandate for booster was rescinded by March 17th, 2022. All HCP who self-identified as immunocompromised were excluded from this study, due to their higher risk of breakthrough infection and their ACIP-recommended, accelerated COVID-19 vaccination schedule [20,21,26]. This study has human subjects research approval from the Northwell Health Institutional Review Board (IRB).
2.2. Survey development and deployment
Questions from validated instruments [4,6] were used and some were adapted to address themes unique to COVID-19 HCP vaccine hesitancy. Likert-scaled, true/false/not sure, and yes/no responses were collected and managed using REDCap, a secure, web-based software platform designed to support electronic data capture tools for research [28]. Three major sections of the 116-item survey included the following: (1) sociodemographic variables (including 11 categories of languages spoken, co-morbidities for HCP and HCP with children, COVID-19 booster status for HCP and vaccination status of HCP children, duration of healthcare work experience, and duration of organization work experience); (2) perception of vaccines (confidence in COVID-19 vaccine recommendation, knowledge, and discussion) [6]; and (3) vaccine hesitancy determined by 3 variables (HCP COVID-19 vaccine hesitancy, parental attitude toward childhood vaccines as measured by the PACV survey, and HCP parent COVID-19 vaccine hesitancy for children) [4]. The PACV survey, a 15-item questionnaire scored from 0 to 100 with the higher number indicating more vaccine hesitancy. Exact survey instruments are available in supplemental material (Appendix A, B, and C). Participants were advised that the survey would take 5–10 min to complete.
The primary outcome, vaccine hesitancy among HCP was measured using the following question: “Overall, how hesitant towards COVID-19 vaccine do you consider yourself to be?” A secondary outcome, using the composite measure of general hesitancy among HCP parents toward childhood vaccination, was calculated from responses to the PACV survey. Finally, a third outcome addressing hesitancy specific to COVID-19 vaccines for children among HCP parents, was measured using the following question: “Overall, how hesitant towards COVID-19 vaccine for your children do you consider yourself to be?” The composite vaccine hesitancy surveys were deployed anonymously from December 21, 2021, to January 21, 2022, through a secure electronic link. Participants were recruited and consented via the internal communications and human resources departments using multiple sources, including the health system’s network intranet, Facebook employee page, newsletter emails, organizational meetings, promotions, and distribution by infection prevention specialists at each organizational location. In order to maintain anonymity and confidentiality, sending surveys directly to all HCP via email address was not included in our protocol.
2.3. Data analysis
Vaccine perception measures (confidence in discussion, COVID-19 vaccine recommendation, and knowledge) and booster shot status among HCP were explored for potentially significant associations with sociodemographic characteristics. Confidence in COVID-19 recommendation is a 6-item instrument from 1 to 6 with high numbers indicating more confidence. Confidence in vaccine discussion and knowledge are similarly structured and scored. The scores for each outcome measure (vaccine hesitancy, confidence in COVID-19 vaccine recommendation, confidence in vaccine knowledge and discussion) were analyzed on a discrete numeric scale. All sociodemographic characteristics were summarized as categorical variables using frequencies and proportions. For each vaccine hesitancy outcome measure, its association with sociodemographic variables and vaccination status was assessed using log binomial regression analyses in SAS 9.4 software (SAS Institute Inc.) to calculate unadjusted and adjusted prevalence ratios (PR) with 95 % confidence intervals (95 % CI).
3. Results
Based on the number of total unique instances of emails opened and links clicked, approximately 25,000 (about one third of) eligible HCP accessed the survey during deployment. Based on our internal metrics, there were 20,000–25,000 clicks, approximately a 33––38 % open rate of our survey. A total of 6,537 individuals began the survey, and of those, 4,165 participants completed the full survey with a response rate of 63.7 % for those interacting with the survey and 16.7 % for those who accessed the link. Respondents were mostly female (3449, 83.1 %) (Table 1), slightly higher than the 70 % female HCP among 70,000 employees in our health system. Age, race, and languages spoken by participants were evenly distributed. Although age and residential location were similar among survey participants to our general HCP population, slightly more respondents were white (63.4 % vs 47.7 %) or multi-racial (5.88 % vs 1.52 %). Hispanic ethnicity was self-identified by 553 (13.3 %) of participants. Career characteristics that were noted included income range (<$30,000–$300,000) with about 163 (5.2 %) of participants making more than $250,000 annually. One-quarter of participants were new to the healthcare system after having worked in healthcare for at least 10 years. There were 1767 (42.4 %) of respondents with high patient contact (clinical staff) and 953 (22.9 %) respondents with some patient contact (Table 1). Specifically, the largest proportion of respondents were nurses, 1052 (26 %) with clinicians 432 (10.46 %) and providers 182 (4.38 %) as the next largest groups respectively. (Table 1a – supplement).
Table 1.
Survey participant characteristics and associations with COVID-19 vaccine hesitancy among Healthcare Professionals (HCP) a (N = 4165).
| n (%) | PR (95 % CI), p-value | ||
|---|---|---|---|
|
|
|||
| Bivariate | Multivariable | ||
|
| |||
| Hesitant about COVID-19 vaccines a | |||
| No | 3420 (82.11) | ||
| Yes | 718 (17.24) | ||
| Missing | 27 (0.65) | ||
| Age | |||
| 18–25 years | 202 (4.85) | 3.06 (1.65–5.67), p < 0.01 | 1.20 (0.64–2.28), p = 0.57 |
| 26–35 years | 1041 (24.99) | 3.36 (1.92–5.89), p < 0.01 | 1.27 (0.71–2.24), p = 0.42 |
| 36–45 years | 838 (20.12) | 3.92 (2.24–6.87) p < 0.01 | 1.43 (0.80–2.53), p = 0.23 |
| 46–55 years | 861 (20.67) | 2.84 (1.61–5.00) p < 0.01 | 1.24 (0.70–2.19), p = 0.46 |
| 55–65 years | 1011 (24.27) | 1.61 (0.90–2.87) p = 0.11 | 1.11 (0.63–1.94), p = 0.72 |
| Older than 65 years (REFERENCE) | 195 (4.68) | 1.00 | 1.00 |
| Missing | 17 (0.41) | ||
| Sex | |||
| Female | 3459 (83.05) | 0.86 (0.49–1.59), p = 0.60 | |
| Male | 642 (15.41) | 0.65 (0.36–1.16), p = 0.15 | |
| Prefer not to answer (REFERENCE) | 49 (1.18) | 1.00 | |
| Missing | 15 (0.36) | ||
| Gender | |||
| Female | 3422 (82.16) | 0.60 (0.43–0.85), p < 0.01 | 0.74 (0.54–1.00), p = 0.05 |
| Male | 624 (14.98) | 0.45 (0.30–0.66), p < 0.01 | 0.70 (0.49–0.98), p = 0.04 |
| Non-Binary | 7 (0.17) | 0.98 (0.29–3.30), p = 0.97 | 1.25 (0.20–7.71), p = 0.81 |
| Prefer not to answer (REFERENCE) | 83 (1.99) | 1.00 | 1.00 |
| Missing | 29 (0.70) | ||
| Race | |||
| African Americans/Black | 475 (11.40) | 1.35 (1.04–1.75), p = 0.03 | 1.17 (0.90–1.52), p = 0.25 |
| Caucasian/White | 2641 (63.41) | 0.63 (0.50–0.81), p < 0.01 | 0.94 (0.73–1.20), p = 0.62 |
| Asian American | 631 (15.15) | 0.53 (0.39–0.72), p < 0.01 | 0.79 (0.57–1.10), p = 0.16 |
| American Indian/Alaska Native | 39 (0.94) | 1.74 (1.13–2.71), p < 0.01 | 1.48 (0.99–2.22), p = 0.057 |
| Native Hawaiian/Pacific Islander | 25 (0.60) | 1.19 (0.61–2.33), p = 0.60 | 1.06 (0.57–1.96), p = 0.86 |
| Multi-Racial (REFERENCE) | 245 (5.88) | 1.00 | 1.00 |
| Missing | 109 (2.62) | ||
| Ethnicity | |||
| Hispanic or Latinx | 553 (13.28) | 1.35 (1.14–1.60), p < 0.01 | 1.01 (0.82–1.24), p = 0.93 |
| Not Hispanic or Latinx (REFERENCE) | 3572 (85.76) | 1.00 | 1.00 |
| Missing | 40 (0.96) | ||
| Language c | |||
| English and Other Language(s) | 1029 (24.71) | 1.08 (0.93–1.26), p = 0.31 | 0.88 (0.75–1.02), p = 0.09 |
| Non-English Language(s) Only | 33 (0.79) | 2.53 (1.69–3.80), p < 0.01 | 1.44 (0.99–2.11), p = 0.06 |
| English Only (REFERENCE) | 3079 (73.93) | 1.00 | 1.00 |
| Missing | 24 (0.58) | ||
| County of Primary Residence | |||
| Bronx | 54 (1.30) | 1.00 (0.52–1.93), p = 0.99 | 0.62 (0.34–1.12), p = 0.11 |
| Kings | 101 (2.42) | 1.65 (1.09–2.52), p = 0.02 | 1.08 (0.76–1.55), p = 0.65 |
| Manhattan | 98 (2.35) | 0.12 (0.03–0.50), p < 0.01 | 0.18 (0.04–0.71), p = 0.01 |
| Nassau | 1396 (33.52) | 0.98 (0.73–1.33), p = 0.91 | 1.01 (0.77–1.32), p = 0.95 |
| Queens | 697 (16.73) | 1.03 (0.75–1.43), p = 0.84 | 0.86 (0.64–1.14), p = 0.30 |
| Richmond | 167 (4.01) | 1.27 (0.85–1.90), p = 0.24 | 0.86 (0.59–1.23), p = 0.40 |
| Suffolk | 1036 (24.87) | 1.14 (0.84–1.55), p = 0.41 | 1.04 (0.79–1.37), p = 0.77 |
| Westchester | 242 (5.81) | 0.76 (0.49–1.16), p = 0.20 | 0.91 (0.62–1.36), p = 0.66 |
| Other e (REFERENCE) | 243 (5.83) | 1.00 | 1.00 |
| Missing | 131 (3.15) | ||
| Chronic Lung Disease | |||
| No | 4087 (98.13) | 1.36 (0.76–2.44), p = 0.30 | |
| Yes (REFERENCE) | 78 (1.87) | 1.00 | |
| Missing | 0 | ||
| Heart Disease | |||
| No | 4060 (97.48) | 1.41 (0.84–2.36), p = 0.19 | |
| Yes (REFERENCE) | 105 (2.52) | 1.00 | |
| Missing | 0 | ||
| High Blood Pressure | |||
| No | 3457 (83.00) | 1.38 (1.12–1.68), p < 0.01 | 1.05 (0.84–1.33), p = 0.65 |
| Yes (REFERENCE) | 708 (17.00) | 1.00 | 1.00 |
| Missing | 0 | ||
| Obesity | |||
| No | 3657 (87.80) | 1.16 (0.93–1.44), p = 0.18 | |
| Yes (REFERENCE) | 508 (12.20) | 1.00 | |
| Missing | 0 | ||
| Other/None of the Above Comorbidity | |||
| No | 1142 (27.42) | 0.79 (0.68–0.93), p < 0.01 | 0.98 (0.83–1.17), p = 0.83 |
| Yes (REFERENCE) | 3023 (72.58) | 1.00 | 1.00 |
| Missing | 0 | ||
| Parent or Guardian | |||
| No | 2821 (67.73) | 0.61 (0.54–0.70), p < 0.01 | 0.78 (0.68–0.89), p < 0.01 |
| Yes (REFERENCE) | 1335 (32.05) | 1.00 | 1.00 |
| Missing | 9 (0.22) | ||
| Income | |||
| Less than $30,000 | 126 (3.03) | 13.38 (3.31–54.02), p < 0.01 | 4.60 (1.14–18.58), p = 0.03 |
| $30,000–$49,999 | 666 (15.99) | 11.76 (2.97–46.59), p < 0.01 | 4.03 (1.02–15.95), p = 0.05 |
| $50,000–$74,999 | 801 (19.23) | 8.12 (2.05–32.20), p < 0.01 | 3.25 (0.82–12.85), p = 0.09 |
| $75,000–$99,999 | 816 (19.59) | 8.20 (2.07–32.54), p < 0.01 | 3.69 (0.94–14.59), p = 0.06 |
| $100,000–$149,999 | 1042 (25.02) | 5.77 (1.45–22.92), p < 0.01 | 2.95 (0.75–11.68), p = 0.12 |
| $150,000–$199,999 | 297 (7.13) | 5.09 (1.25–20.77), p = 0.02 | 3.05 (0.75–12.35), p = 0.12 |
| $200,000–$249,999 | 127 (3.05) | 3.81 (0.87–16.78), p = 0.08 | 2.53 (0.58–11.08), p = 0.22 |
| $250,000–$299,999 | 74 (1.78) | 2.97 (0.59–14.89), p = 0.18 | 2.52 (0.51–12.33), p = 0.25 |
| $300,000 or more (REFERENCE) | 89 (2.14) | 1.00 | 1.00 |
| Missing | 127 (3.05) | ||
| Daily Job Function d | |||
| Minimal to no patient interaction | 1431 (34.36) | 0.99 (0.85–1.15), p = 0.91 | |
| Some patient interaction | 953 (22.88) | 0.96 (0.81–1.14), p = 0.66 | |
| High patient interaction (REFERENCE) | 1767 (42.42) | 1.00 | |
| Missing | 14 (0.34) | ||
| Duration of Employment | |||
| 0–2 years | 1079 (25.91) | 2.37 (1.59–3.55), p < 0.01 | 0.88 (0.56–1.40), p = 0.60 |
| 3–30 years | 2793 (67.06) | 2.06 (1.39–3.05), p < 0.01 | 0.90 (0.58–1.40), p = 0.65 |
| More than 30 years (REFERENCE) | 287 (6.89) | 1.00 | 1.00 |
| Missing | 6 (0.14) | ||
| Duration in Healthcare | |||
| 0–2 years | 385 (9.24) | 2.18 (1.58–3.01), p < 0.01 | 1.26 (0.82–1.92), p = 0.29 |
| 3–30 years | 3002 (72.08) | 2.45 (1.91–3.15), p < 0.01 | 1.38 (0.97–1.95), p = 0.07 |
| More than 30 years (REFERENCE) | 774 (18.58) | 1.00 | 1.00 |
| Missing | 4 (0.10) | ||
| Received Booster Shot | |||
| No | 1211 (29.08) | 5.27 (4.57–6.09), p < 0.01 | 4.43 (3.76–5.20), p < 0.01 |
| Yes (REFERENCE) | 2920 (70.11) | 1.00 | 1.00 |
| Missing | 34 (0.82) | ||
HCP = healthcare personnel; PR = prevalence ratio (estimates the relative risk in cross-sectional studies); 95 % CI = 95 % confidence interval.
Bolded values indicate significant associations.
HCP bivariate and multivariable regression is log binomial methods to model the probability of being “very hesitant” or “somewhat hesitant” (vs. not sure, not too hesitant, not at all hesitant) in response to “Overall, how hesitant about COVID-19 vaccines would you consider yourself to be?”.
Other Languages = Spanish (n=), Mandarin (n=), Cantonese (n=), Korean (n=), Hindi (n=), Punjabi (n=), Bengali (n=), Russian (n=), French/Creole (n=), Additional non-English (n=).
Daily job function as part of the daily/regular duties to provide health care = High patient interaction (Advanced Clinical Providers, Clinical Care, Clinical Professional, Nursing, Provider); Some patient interaction (Academia and Research, Clinical Laboratory, Clinical Support, Hospitality, Patient and Customer Experience, Pharmacy, Quality, Patient Safety and Infection Prevention, Rehabilitation Services, Social Services); Minimal to no patient interaction (Administrative Support, Analytics and Business Insights, Business Services, Business Strategy, Facilities and Support Services, Finance, Foundation, General Management, Human Resources, Information Technology and Services, Legal and Compliance, Marketing and Communications, Revenue Cycle, Risk Management, Supply chain).
Other County = outside of NYC metropolitan area and Long Island.
3.1. Vaccine hesitancy for HCP
In regression analyses that modeled the bivariate associations of sociodemographic characteristics with COVID-19 vaccine hesitancy (Table 1), African American (PR = 1.35, 95 % CI = 1.04–1.75), Hispanic (PR = 1.35, 95 % CI = 1.14–1.60), and American Indian/Alaska Native (PR = 1.74, 95 % CI = 1.13–2.71) were about one and half times more likely, while Caucasian/White (PR = 0.63, 95 % CI = 0.50–0.81) and Asian American (PR = 0.53, 95 % CI = 0.39–0.72) were about half as likely to be COVID-19 vaccine hesitant compared to HCP that identified as multi-racial. Those who were younger, earning lower wages and with fewer years on the job, and living in Manhattan were significantly more likely to be COVID-19 vaccine hesitant (Table 1). HCP who had not previously received a booster shot were more than five times as likely to be vaccine hesitant (PR = 5.27, 95 % CI = 4.57–6.09). Respondents were two and half times more likely to be COVID-19 vaccine hesitant if bilingual than only English-speaking PR = 2.53 (1.69–3.80), p < 0.0001.
3.2. Vaccine hesitancy for pediatric vaccines
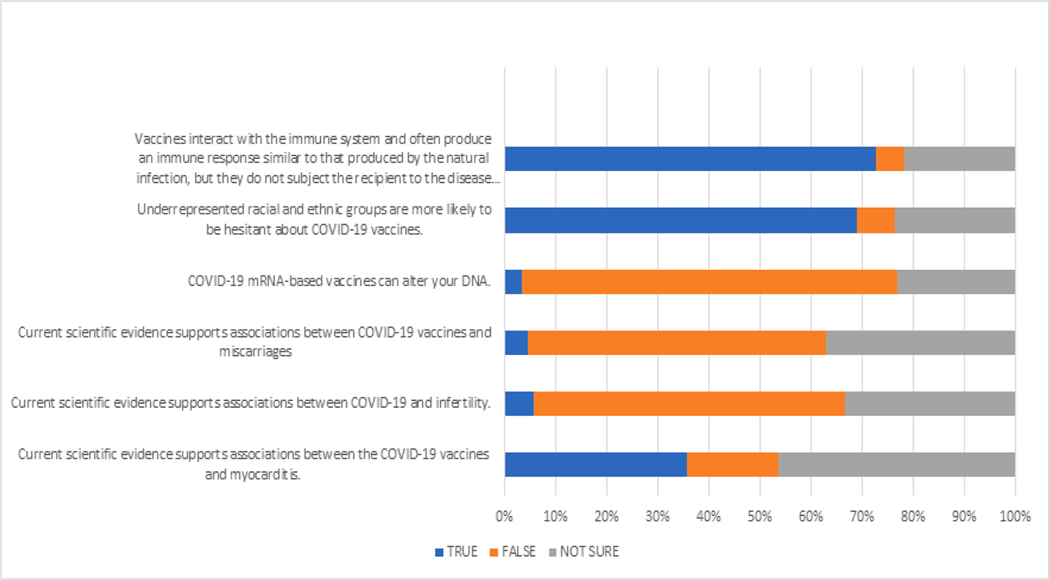
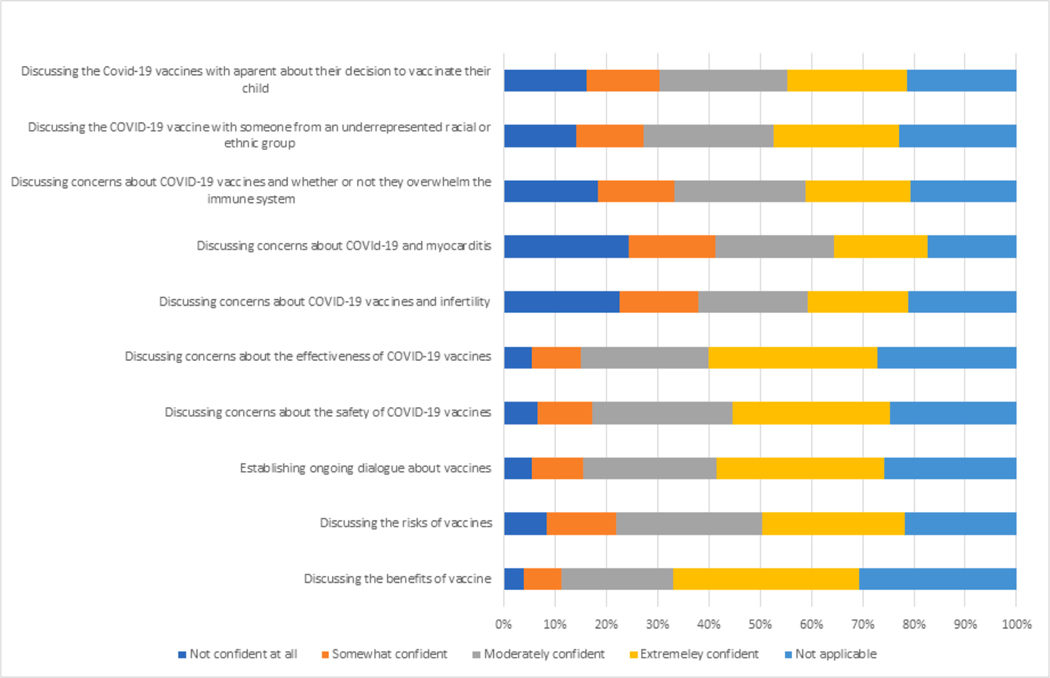
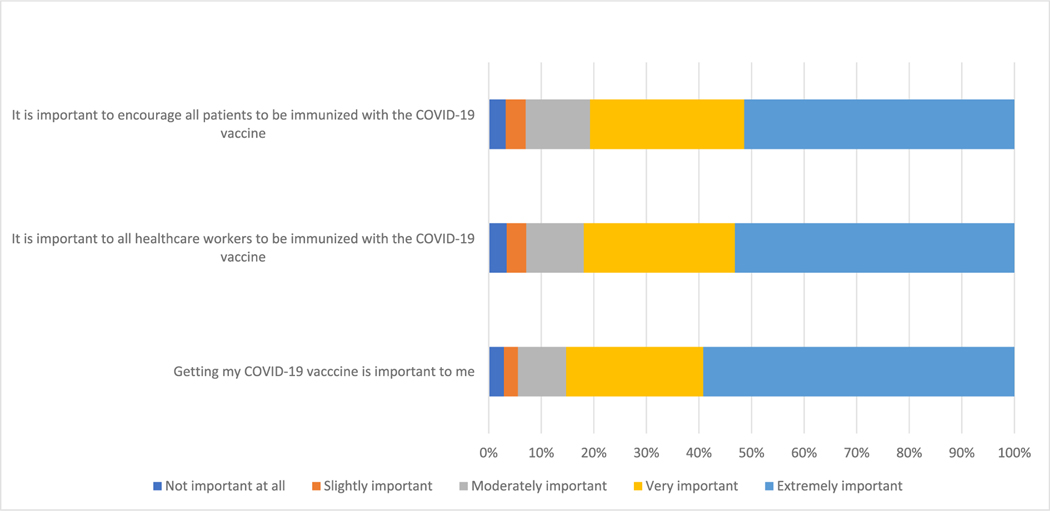
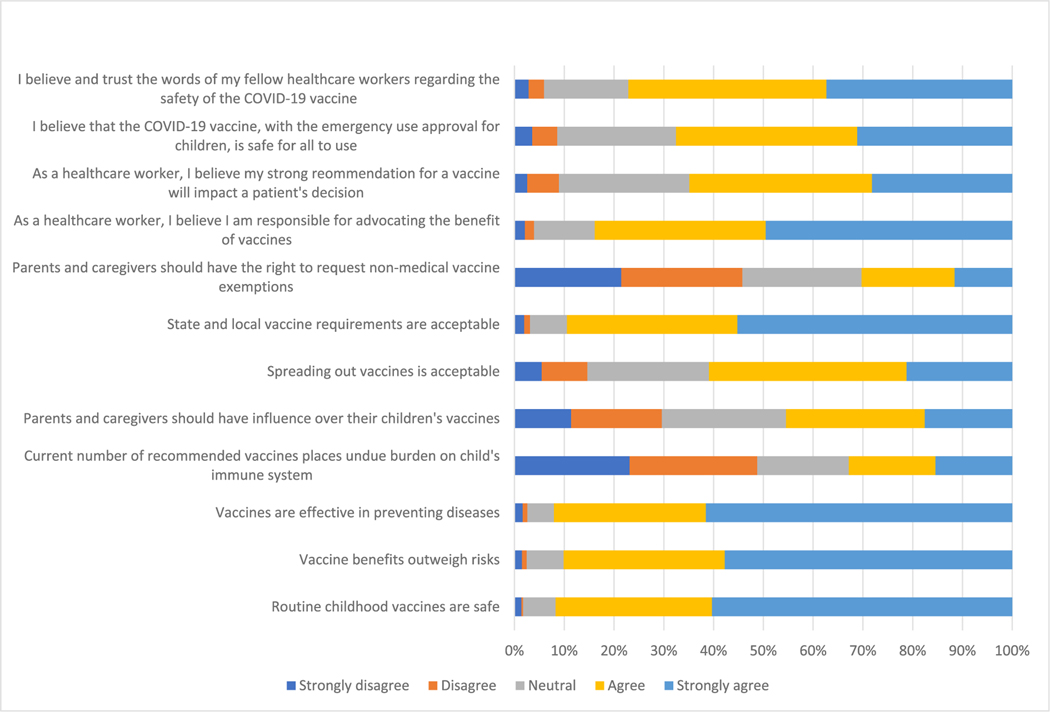
An estimated 718 (17.2 %) of HCP overall (Table 1) and 434 (32.6 %) of HCP with children (Table 2) reported being “unsure” or “hesitant” towards the COVID-19 vaccine for children. A large proportion of HCP were not sure about COVID-19 vaccine’s impact on infertility (1378, 33.3 %), miscarriages (1528, 37.0 %), changes in DNA (957, 23.1 %), and immune response (897, 21.7 %). Of all HCP, 1924 (46.4 %) were unsure about the current scientific evidence between COVID-19 vaccines and myocarditis (Fig. 1). Out of all survey respondents, 1949 (47.01 %) of HCP were moderately to extremely confident about discussing common concerns about vaccines (Fig. 2). A substantial number of HCP, 3541 (85.3 %) felt that COVID-19 vaccine was important to them (Fig. 3). Sixty percent (2672) believed that their strong recommendation for a vaccination would impact a patient’s decision on whether to vaccinate (Fig. 4). Sixty-eight percent (2790) of HCP believed that the COVID-19 vaccine, based on FDA emergency use authorization, was safe for kids to use (Fig. 4).Eight-hundred sixty-seven (64.9 %) HCP with children (Table 2) and 2920 (70.1 %) HCP without children, received their booster dose (Table 1) at higher rate than the general population at the time.
Table 2.
Characteristics of Healthcare Professionals (HCP) who are parents and associations with hesitancy about childhood vaccines from respondents of the Parental Attitudes About Childhood Vaccines (PACV) survey (N = 1335).b
| n (%) | PR (95 % CI), p-value | |||
|---|---|---|---|---|
|
|
||||
| Bivariate | Multivariable * | |||
|
|
||||
| Model I | Model II** | |||
|
| ||||
| Hesitant about COVID-19 vaccines for children (PACV) b | ||||
| No | 898 (67.27) | |||
| Yes | 434 (32.51) | |||
| Missing | 0 | |||
| Hesitant about COVID-19 vaccines | ||||
| No | 1000 (74.91) | |||
| Yes | 308 (23.07) | |||
| Missing | 27 (2.03) | |||
| Age | ||||
| 18–25 years | 5 (0.37) | 3.29 (undefined), p < 0.01 | ||
| 26–35 years | 268 (20.07) | 1.52 (0.59–3.92), p = 0.38 | ** model II with children’s | |
| 36–45 years | 550 (40.95) | 1.53 (0.60–3.93), p = 0.37 | vaccine status, does not | |
| 46–55 years | 387 (28.99) | 1.75 (0.68–4.49), p = 0.24 | converge | |
| 56–65 years | 101 (7.57) | 1.53 (0.59–4.00), p = 0.38 | ||
| Older than 65 years (REFERENCE) | 9 (0.67) | 1.00 | ||
| Missing | 5 (0.37) | |||
| Sex | ||||
| Female | 1092 (81.80) | 0.65 (0.49–0.87), p < 0.01 | ||
| Male | 222 (16.63) | 0.62 (0.45–0.85), p < 0.01 | ||
| Prefer not to answer (REFERENCE) | 16 (1.20) | 1.00 | ||
| Missing | 5 (0.37) | |||
| Gender | ||||
| Female | 1084 (81.20) | 0.64 (0.50–0.82), p < 0.01 | 0.65 (0.45–0.96), p = 0.03 | |
| Male | 216 (16.18) | 0.60 (0.44–0.79), p < 0.01 | 0.69 (0.47–1.02), p = 0.07 | |
| Non-Binary | 0 | − | − | |
| Prefer not to answer (REFERENCE) | 21 (1.57) | 1.00 | 1.00 | |
| Missing | 14 (1.05) | |||
| Race | ||||
| African Americans/Black | 189 (14.16) | 1.34 (1.07–1.67), p = 0.01 | 1.34 (1.02–1.76), p = 0.04 | |
| Caucasian/White | 741 (55.51) | 0.82 (0.66–1.02), p = 0.08 | 1.07 (0.83–1.39), p = 0.60 | |
| Asian American | 243 (18.20) | 1.00 (0.79–1.27), p = 0.99 | 1.26 (0.97–1.64), p = 0.08 | |
| American Indian/Alaska Native | 16 (1.20) | 1.48 (1.05–2.10), p = 0.03 | 1.61 (1.00–2.59), p = 0.05 | |
| Native Hawaiian/Pacific Islander | 9 (0.67) | 0.88 (0.41–1.88), p = 0.74 | 1.25 (0.61–2.56), p = 0.54 | |
| Multi-Racial (REFERENCE) | 91 (6.82) | 1.00 | 1.00 | |
| Missing | 46 (3.45) | |||
| Ethnicity | ||||
| Hispanic or Latinx | 213 (15.96) | 1.12 (0.98–1.30), p = 0.09 | ||
| Not Hispanic or Latinx (REFERENCE) | 1108 (83.00) | 1.00 | ||
| Missing | 14 (1.05) | |||
| Language | ||||
| English and Other Language(s) | 392 (29.36) | 1.13 (1.01–1.27), p = 0.03 | 1.12 (0.98–1.28), p = 0.11 | |
| Non-English Language(s) Only | 16 (1.20) | 1.75 (1.37–2.24), p < 0.01 | 1.55 (0.97–2.48), p = 0.07 | |
| English Only (REFERENCE) | 924 (69.21) | 1.00 | 1.00 | |
| Missing | 3 (0.22) | |||
| County | ||||
| Bronx | 19 (1.42) | 1.50 (0.94–2.40), p = 0.09 | 1.32 (0.70–2.49), p = 0.39 | |
| Kings | 32 (2.40) | 1.37 (0.90–2.11), p = 0.14 | 1.08 (0.72–1.60), p = 0.71 | |
| Manhattan | 16 (1.20) | 1.30 (0.74–2.27), p = 0.36 | 0.95 (0.44–2.04), p = 0.89 | |
| Nassau | 478 (35.81) | 1.23 (0.92–1.64), p = 0.16 | 1.07 (0.79–1.44), p = 0.65 | |
| Queens | 208 (15.58) | 1.48 (1.10–2.00), p < 0.01 | 1.10 (0.80–1.53), p = 0.55 | |
| Richmond | 46 (3.45) | 1.35 (0.92–1.99), p = 0.13 | 1.08 (0.73–1.60), p = 0.71 | |
| Suffolk | 351 (26.29) | 1.23 (0.92–1.65), p = 0.16 | 1.13 (0.83–1.53), p = 0.42 | |
| Westchester | 68 (5.17) | 1.09 (0.73–1.61), p = 0.66 | 1.06 (0.70–1.61), p = 0.77 | |
| Other (REFERENCE) | 83 (6.22) | 1.00 | 1.00 | |
| Missing | 33 (2.47) | |||
| Chronic Lung Disease | ||||
| No | 1315 (98.50) | 1.21 (0.71–2.09), p = 0.43 | ||
| Yes (REFERENCE) | 20 (1.50) | 1.00 | ||
| Missing | 0 | |||
| Heart Disease | ||||
| No | 1306 (97.83) | 0.83 (0.60–1.13), p = 0.23 | ||
| Yes (REFERENCE) | 29 (2.17) | 1.00 | ||
| Missing | 0 | |||
| High Blood Pressure | ||||
| No | 1137 (85.17) | 0.87 (0.76–1.00), p = 0.06 | ||
| Yes (REFERENCE) | 198 (14.83) | 1.00 | ||
| Missing | 0 | |||
| Obesity | ||||
| No | 1179 (88.31) | 1.04 (0.87–1.25), p = 0.63 | ||
| Yes (REFERENCE) | 156 (11.69) | 1.00 | ||
| Missing | 0 | |||
| Other/None of the Above Comorbidity | ||||
| No | 336 (25.17) | 1.05 (0.93–1.19), p = 0.40 | ||
| Yes (REFERENCE) | 999 (74.83) | 1.00 | ||
| Missing | 0 | |||
| Parent or Guardian | ||||
| No | 0 | |||
| Yes (REFERENCE) | 1335 (100.00) | |||
| Missing | 0 | |||
| Income | ||||
| Less than $30,000 | 29 (2.17) | 4.85 (2.11–11.15), p < 0.01 | 3.25 (1.24–8.48), p = 0.02 | |
| $30,000–$49,999 | 226 (16.93) | 4.16 (1.85–9.37), p < 0.01 | 3.01 (1.19–7.59), p = 0.02 | |
| $50,000–$74,999 | 214 (16.03) | 3.89 (1.72–8.77), p < 0.01 | 2.80 (1.11–7.05), p = 0.03 | |
| $75,000–$99,999 | 233 (17.45) | 3.16 (1.40–7.15), p < 0.01 | 2.63 (1.04–6.61), p = 0.04 | |
| $100,000–$149,999 | 370 (27.72) | 2.49 (1.10–5.63), p = 0.03 | 2.15 (0.85–5.40), p = 0.10 | |
| $150,000–$199,999 | 100 (7.49) | 2.75 (1.19–6.36), p = 0.02 | 243 (0.94–6.23), p = 0.07 | |
| $200,000–$249,999 | 54 (4.04) | 1.78 (0.71–4.43), p = 0.22 | 1.75 (0.64–4.82), p = 0.28 | |
| $250,000–$299,999 | 38 (2.85) | 1.52 (0.56–4.07), p = 0.41 | 1.68 (0.58–4.84), p = 0.34 | |
| $300,000 or more (REFERENCE) | 32 (2.40) | 1.00 | 1.00 | |
| Missing | 39 (2.92) | |||
| Daily Job Function c | ||||
| Minimal to no patient interaction | 426 (31.91) | 1.15 (1.01–1.31), p = 0.03 | 1.12 (0.98–1.29), p = 0.10 | |
| Some patient interaction | 306 (22.92) | 1.09 (0.94–1.26), p = 0.25 | 1.00 (0.85–1.16), p = 0.97 | |
| High patient interaction (REFERENCE) | 596 (44.79) | 1.00 | 1.00 | |
| Missing | 5 (0.37) | |||
| Duration of Employment | ||||
| 0–2 years | 301 (22.55) | 1.16 (0.83–1.63), p = 0.39 | ||
| 3–30 years | 988 (74.01) | 1.05 (0.75–1.46), p = 0.79 | ||
| More than 30 years (REFERENCE) | 44 (3.30) | 1.00 | ||
| Missing | 2 (0.15) | |||
| Duration in Healthcare | ||||
| 0–2 years | 74 (5.54) | 1.27 (0.92–1.76), p = 0.14 | ||
| 3–30 years | 1156 (86.59) | 1.22 (0.96–1.55), p = 0.11 | ||
| More than 30 years (REFERENCE) | 104 (7.79) | 1.00 | ||
| Missing | 1 (0.07) | |||
| Received Booster Shot | ||||
| No | 454 (34.01) | 1.84 (1.65–2.04), p < 0.01 | 1.65 (1.46–1.87), p < 0.01 | |
| Yes | 867 (64.94) | 1.00 | 1.00 | |
| Missing | 14 (1.05) | |||
| Children in Household (No / Yes = REFERENCE) | ||||
| Younger than 5 years old | 868 (65.02) / 366 (27.42) | 1.15 (1.00–1.31), p < 0.04 | 1.05 (0.92–1.22), p < 0.44 | |
| 5 to 11 years old | 687 (51.46) / 547 (40.97) | 0.96 (0.85–1.09), p = 0.52 | ||
| 12 to 17 years old | 620 (46.44) / 614 (45.99) | 0.91 (0.81–1.02), p = 0.10 | ||
| 18 years or older | 886 (66.37) / 348 (26.07) | 0.87 (0.77–0.98), p = 0.03 | 0.95 (0.83–1.08), p = 0.45 | |
|
COVID-19 Vaccination Status of 5- to 11-year-olds
(No / Yes = REFERENCE) | ||||
| Unvaccinated | 240 (17.98) / 304 (22.77) | 0.52 (0.42–0.64), p < 0.01 | ||
| Partially Vaccinated | 227 (17.00) / 317 (23.75) | 1.74 (1.46–2.07), p < 0.01 | ||
| Completely Vaccinated | 77 (5.78) / 240 (17.98) | 2.84 (1.70–4.72), p < 0.01 | ||
| COVID-19 Vaccination Status of 12- to 17-year-olds (No / Yes = REFERENCE) | ||||
| Unvaccinated | 501 (37.53) / 109 (8.16) | 0.58 (0.51–0.68), p < 0.01 | ||
| Partially Vaccinated | 94 (7.04) / 516 (38.65) | 1.65 (1.42–1.92), p < 0.01 | ||
| Completely Vaccinated | 15 (1.12) / 485 (36.33) | 1.81 (1.38–2.38), p < 0.01 | ||
| Child Neurodevelopmental Disorders | ||||
| No | 1292 (96.78) | 0.95 (0.70–1.28), p = 0.73 | ||
| Yes (REFERENCE) | 43 (3.22) | 1.00 | ||
| Missing | 0 | |||
| Child High Blood Pressure | ||||
| No | 1329 (99.55) | 2.93 (0.39–17.55), p = 0.24 | ||
| Yes (REFERENCE) | 6 (0.45) | 1.00 | ||
| Missing | 0 | |||
| Child Obesity | ||||
| No | 1308 (97.98) | 1.47 (0.86–2.51), p = 0.16 | ||
| Yes (REFERENCE) | 27 (2.02) | 1.00 | ||
| Missing | 0 | |||
| Child Other/None of the Above Comorbidity | ||||
| No | 132 (9.89) | 0.98 (0.81–1.18), p = 0.83 | ||
| Yes (REFERENCE) | 1203 (90.11) | 1.00 | ||
| Missing | 0 | |||
| Child Pregnancy | ||||
| No | 1333 (99.85) | Undefined p = 0.97 | ||
| Yes (REFERENCE) | 2 (0.15) | 1.00 | ||
| Missing | 0 | |||
n = frequency; % = proportion, SD = standard deviation, IQR = interquartile range.
HCP = healthcare personnel; PR = prevalence ratio (estimates the relative risk in cross-sectional studies); 95 % CI = 95 % confidence interval.
Bolded values indicate significant associations.
To avoid variable multicollinearity amongst childhood characteristics, number of children in household (Model I) and childhood vaccination status (Model II) and were run in separate models.
Daily job function as part of the daily/regular duties to provide health care = High patient interaction (Advanced Clinical Providers, Clinical Care, Clinical Professional, Nursing, Provider); Some patient interaction (Academia and Research, Clinical Laboratory, Clinical Support, Hospitality, Patient and Customer Experience, Pharmacy, Quality, Patient Safety and Infection Prevention, Rehabilitation Services, Social Services); Minimal to no patient interaction (Administrative Support, Analytics and Business Insights, Business Services, Business Strategy, Facilities and Support Services, Finance, Foundation, General Management, Human Resources, Information Technology and Services, Legal and Compliance, Marketing and Communications, Revenue Cycle, Risk Management, Supply chain).
Other County = outside of NYC metropolitan area and Long Island.
HCP parent bivariate and multivariable regression uses log binomial methods to model the probability of being hesitant about vaccines for children using a composite score from the Parental Attitudes About Childhood Vaccines (PACV) survey.
Other Languages = Spanish (n=), Mandarin (n=), Cantonese (n=), Korean (n=), Hindi (n=), Punjabi (n=), Bengali (n=), Russian (n=), French/Creole (n=), Additional non-English (n=).
Fig. 1.
HCP knowledge about COVID-19 vaccines (N = 4165)* HCP = Healthcare Personnel *Less than 1 % missing Please print in color.
Fig. 2.
HCP confidence about discussing COVIDE-19 vaccines (N = 4165)* HCP = Healthcare Personnel *Less than 1 % missing Please print in color.
Fig. 3.
HCP recommendations on the importance of COVID-19 vaccines (N = 4165) HCP = Healthcare Personnel *Less than 1 % missing Please print in color.
Fig. 4.
HCP beliefs about COVID-19 vaccine and all vaccines HCP = Healthcare Personnel *Less than 2 % missing.
A small group of HCP did not feel that childhood vaccines were safe (282, 6.9 %), felt that risk outweighed benefits (101, 2.5 %), or prevented diseases (107, 2.6 %) (Fig. 4). About one-third of HCP (1335, 32.8 %) felt that the current childhood vaccination schedule placed an undue burden on a child’s immune system (Fig. 4). Forty-five percent (1883) of HCP believed that parents and caregivers should have influence over what vaccines are given to their children, even if their opinions and beliefs were counter to scientific evidence currently available regarding vaccinations. Sixty-one percent (2506) believed that spreading out recommended vaccines over several visits following the ACIP and CDC recommended vaccine schedule was acceptable. Thirty percent (1248) believed that parents and caregivers should have the right to request non-medical exemptions for school entry requirements (Fig. 4).
In general, HCP who were not parents or guardians were far less likely to be hesitant about vaccinating themselves (PR = 0.61, 95 % CI = 0.54–0.70) compared to those who were parents/guardians. There was also a significant proportion of HCP with children over the age of five, who were hesitant about vaccinating their children in general (PR = 1.15, 95 % CI = 1.00–1.31) (Table 2). Confirming our hypothesis that HCP with lower vaccine hesitancy were more likely to vaccinate their children, among HCP with vaccinated children of any age in the household, hesitancy was about half that of HCP with unvaccinated children (PR = 0.52, 95 % CI = 0.42–0.6 for ages 5 to 11 years old; and PR = 0.58, 95 % CI = 0.51–0.68 for ages 12 to 17 years old) (Table 2).
In multivariable regression analyses that accounted for significant sociodemographic characteristics and COVID-19 vaccine booster status, most associations with vaccine hesitancy attenuated, becoming less significant, for both HCPs and HCPs with children, except for booster status, child vaccine status, gender, income, and primary county of residency in New York (Tables 1 and 2). These latter variables all remained significantly associated with vaccine hesitancy.
4. Discussion
Despite mandated primary series COVID-19 vaccination, approximately 20 % of a diverse, HCP population in a large metropolitan area were hesitant or unsure about COVID-19 vaccines. Vaccine hesitancy for the primary series correlated with vaccine hesitancy for the booster COVID-19 dose [4.43 (3.76–5.20), p < 0.0001]. An even larger proportion of HCP with children (40 %) were hesitant or unsure about their children being COVID-19 vaccinated. As a combination of clinical and non-clinical staff, common perceptions include the following: (1) childhood vaccines can be spread out over time and still be protective, (2) non-medical exemptions should be provided, (3) discussion regarding vaccines is imbued with a lack of knowledge and confidence. Surrounding the background of these phenomena are the underwhelming efforts to develop COVID-19 vaccines quickly and efficiently for children, mirroring the lack of urgency to immunized that is being reflected in HCP with children [8].
In general, older age has been noted with increased acceptance of COVID-19 vaccine, supported by previous findings in the literature. [29,30] In our population, HCP were more likely to accept vaccines when older than 55 years old, whereas, a systematic review noted this age cut-off to be 45 years old and another study used 50 years old; it appears the age range of increased hesitancy occurs below 45–55 years old. While there are differences based on physician, nurse, and environmental worker vaccine acceptance in Canadian studies of HCP prior to availability of COVID-19 vaccine, and US studies after primary series doses were administered, [24,25] our fully mandated vaccinated HCP showed no difference in hesitancy regardless of degree of clinical duties, demonstrating the continued doubt surrounding COVID-19 vaccination [30]. A global survey of HCP did not account for race/ethnicity/language in their analysis, but still found increased hesitancy in a younger age, pointing toward the need for increased HCP education in these populations [31]. Contributing to more hesitancy among younger employees may be less exposure to past severe disease outbreaks whereas older employees may be less hesitant due to higher risk of disease based on age or co-morbid conditions.
Our novel survey and analysis which accounted for bilingual differences observed HCP parents who are only English-speaking to be just as hesitant as HCP who did not identify as parents. However non-English speaking HCP were hesitant regardless of parental status, with HCP who did not identify as parents being twice as likely to be hesitant as parents. Hispanic HCP parents were not as vaccine hesitant compared to HCP who did not identify as parents. Despite the global data available, there is a paucity of evidence and data to describe cultural influences and the understanding of vaccines, science of immunization, and communication among HCP and to patients.
Disparities in parent COVID-19 acceptance for their children is known to be most prevalent in populations that were traditionally at highest risk for severe disease [32]. Parents more likely to consider vaccinating their children for COVID-19 are vaccinated themselves, including against influenza virus. Parent COVID-19 vaccine hesitancy was related to COVID-19 vaccine hesitancy for their child and did not appear to be impacted by child/adult co-morbid medical conditions [33–35]. Instead, COVID-19 vaccine acceptance is linked to voting preferences for presidential candidates and political affiliation, making vaccine hesitancy concerns particularly unique for the current pandemic [36,37]. Ultimately, our study identified the direct effect on vaccine hesitancy on HCP and their children as a subgroup, with particular concern in populations of color, youth, and low-income.
The fact that provider recommendation for vaccines is the most crucial factor in a parent’s acceptance of childhood immunizations is widely known, and this holds true for COVID-19 vaccine [8,38]. The most common method of intervention for vaccine hesitancy is motivational interviewing, which is also effective for COVID-19 vaccines [39]. Prior to COVID-19 vaccine FDA approval, experts believed that mandates for COVID-19 vaccine in schools will only further the negative perceptions of immunizations for children, stating the need for more safety and dosing data, to build confidence among parents [40]. In fact, incentivization to obtain COVID-19 vaccines for adolescents has created more hesitancy and the gap between provider and parent [41].
Limitations of our study include a modest response rate of 63.7 % for those who were able to access the survey and participants in a largely metropolitan area, which may limit generalizability. However, 16 % of the entire system HCP who opened the survey is comparable to other surveys in this population [42]. The response rate of approximately 5.33 % does indeed raise challenges related to non-response bias and reduced statistical power. Despite our efforts to reach a wide audience, we acknowledge that some HCP may not have been reached or may have chosen not to participate. Given the sensitive nature of the topic in the setting of employee termination due to vaccine refusal and stigma surrounding vaccine hesitancy as an HCP, the low response rate was expected. There may have been some selection bias towards participants who were not vaccine hesitant given the sensitive nature of the topic; for the counterargument, this may be balanced by disgruntled employees and their extreme responses. Additionally, the large representation of female HCP may reflect that of the greater HCP workforce but may limit generalizability to male HCP. Based on the low rate of medical and/or religious exemptions, the survey most likely represents the organization’s HCP population. Finally, we did not request access to vaccination records for children of HCP to maintain anonymity.
The strength of our survey is the use of a large HCP organization that was mandated to receive a primary series of COVID-19 vaccine. Additionally, our survey delved deep into the misperceptions of childhood and COVID-19 vaccination. Most striking is the finding that over 60 % of HCP feel that the CDC recommended schedule is modifiable to spread vaccines over several visits. We also demonstrated the encompassing effect of HCP COVID-19 vaccine hesitancy on their children. If there is HCP COVID-19 vaccine hesitancy, there will be hesitancy towards COVID-19 vaccination for children. We revealed that despite vaccination, hesitancy can still exist and impact future efforts to provide COVID-19 booster doses for both HCP and their children. Therefore, understanding the impact of missing mandates on future vaccination uptake and acceptance, as in the situation for COVID-19 boosters, lends credence to the public health and government efforts to protect a population.
The future of understanding vaccine hesitancy requires a more integrated rather than ‘top-down’ approach as the medical community is suffering from more hesitancy regarding vaccines than ever before. Provider recommendation is compromised at point of care when surrounding HCP, despite having already received their standard COVID-19 doses, still question the need for vaccination and subsequent booster doses. Furthermore, high vaccine hesitancy among HCP for COVID-19 vaccination and booster doses parallels high vaccine hesitancy for pediatric COVID-19 vaccination, thereby having a downstream community impact. Conversations surrounding vaccines continue beyond the provider-patient interactions as HCP speak to each other about their experiences among themselves and their peers. While our organization attempted town halls, webinars, emails, and other forms of education, a more grass-roots approach to education is in need. Our next step is to reach out to focus groups volunteered from this survey population and determine if this subpopulation will be instrumental in developing training modules for COVID-19 vaccination. As the pandemic continues to evolve into endemic status, our global approach to vaccine hesitancy requires diversification, innovation, and approaches yet to be discovered.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the contributions by the Northwell Health Human Resources and Internal Communications teams to launch our survey organization-wide and Andrew Dominello of the Northwell COVID-19 Consortium for his assistance with copy editing. This work was supported by grants R24AG064191 from the National Institute on Aging of the National Institutes of Health.
Footnotes
COVID-19: Coronavirus disease 2019.
HCP: Healthcare personnel.
Credit authorship contribution statement
Mundeep K. Kainth: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. Grace N. Sembajwe: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Heejoon Ahn: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Min Qian: Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Maxine Carrington: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. Donna Armellino: Conceptualization, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. Sophia Jan: Conceptualization, Data curation, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Mundeep K. Kainth reports statistical analysis and writing assistance were provided by This work was supported by grant R24AG064191 from the National Institute on Aging of the National Institutes of Health. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix. Supplementary data
Supplementary data, Appendices, A/B/C, Table 1a and 1b to this article can be found online at https://doi.org/10.1016/j.vaccine.2024.04.028.
Data availability
Data will be made available on request.
References
- [1].Marks KJ, Whitaker M, Anglin O, Milucky J, Patel K, Pham H, et al. Hospitalizations of children and adolescents with laboratory-confirmed COVID-19 - COVID-NET, 14 states, July 2021-January 2022. MMWR Morb Mortal Wkly Rep 2022;71:271–8. 10.15585/mmwr.mm7107e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].CDC A. https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-Jurisdi/unsk-b7fc; 2023.
- [3].Lin E et al. Lin EST, Fishbein J, Mensch D, Kainth MK. Social determinants of health influence vaccine hesitancy in a children’s hospital influenza order program. NFID (National Foundation for Infectious Diseases) virtual 2021 annual conference on vaccinology research. 2021. April 27. https://sidp.org/event-4279954. Last accessed December 22, 2022., n.d. [Google Scholar]
- [4].Opel DJ, Mangione-Smith R, Taylor JA, Korfiatis C, Wiese C, Catz S, et al. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum Vaccin 2011;7:419–25. 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schmid P, Rauber D, Betsch C, Lidolt G, Denker M-L. Barriers of influenza vaccination intention and behavior - a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS One 2017;12:e0170550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Dybsand LL, Hall KJ, Carson PJ. Immunization attitudes, opinions, and knowledge of healthcare professional students at two midwestern universities in the United States. BMC Med Educ 2019;19:242. 10.1186/s12909-019-1678-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].NYS. Governor Hochul announces new guidance on covid-19 booster doses www.governor.ny.gov/. https://www.governor.ny.gov/news/governor-hochul-announces-new-guidance-covid-19-booster-dose; 2022. [Google Scholar]
- [8].Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 2020;5:e475–83. 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Verger P, Fressard L, Collange F, Gautier A, Jestin C, Launay O, et al. Vaccine hesitancy among general PRACTITIONERS and its determinants during controversies: a national cross-sectional survey in France. EBioMedicine 2015;2: 891–7. 10.1016/j.ebiom.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Karlsson LC, Lewandowsky S, Antfolk J, Salo P, Lindfelt M, Oksanen T, et al. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among finnish healthcare workers. PLoS One 2019;14: e0224330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Visser O, Hulscher MEJL, Antonise-Kamp, Akkermans R, van der Velden K, Ruiter RAC, et al. Assessing determinants of the intention to accept a pertussis cocooning vaccination: a survey among healthcare workers in maternity and paediatric care. Vaccine 2018;36:736–43. 10.1016/j.vaccine.2017.12.021. [DOI] [PubMed] [Google Scholar]
- [12].Agrinier N, Le Maréchal M, Fressard L, Verger P, Pulcini C. Discrepancies between general practitioners’ vaccination recommendations for their patients and practices for their children. Clin Microbiol Infect 2017;23:311–7. 10.1016/j.cmi.2016.08.019. [DOI] [PubMed] [Google Scholar]
- [13].Karafillakis E, Dinca I, Apfel F, Cecconi S, Wűrz A, Takacs J, et al. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine 2016; 34:5013–20. 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- [14].Gagneux-Brunon A, Detoc M, Bruel S, Tardy B, Rozaire O, Frappe P, et al. Intention to get vaccinations against COVID-19 in french healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect 2021;108:168–73. 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kuter BJ, Browne S, Momplaisir FM, Feemster KA, Shen AK, Green-McKenzie J, et al. Perspectives on the receipt of a COVID-19 vaccine: a survey of employees in two large hospitals in Philadelphia. Vaccine 2021;39:1693–700. 10.1016/j.vaccine.2021.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Halbrook M, Gadoth A, Martin-Blais R, Gray AN, Kashani S, Kazan C, et al. Longitudinal assessment of coronavirus disease 2019 vaccine acceptance and uptake among frontline medical workers in Los Angeles. California Clin Infect Dis 2022;74:1166–73. 10.1093/cid/ciab614. [DOI] [PubMed] [Google Scholar]
- [17].Paris C, Bénézit F, Geslin M, Polard E, Baldeyrou M, Turmel V, et al. COVID-19 ´ vaccine hesitancy among healthcare workers. Infect Dis Now 2021;51:484–7. 10.1016/j.idnow.2021.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kociolek LK, Elhadary J, Jhaveri R, Patel AB, Stahulak B, Cartland J. Coronavirus disease 2019 vaccine hesitancy among children’s hospital staff: a single-center survey. Infect Control Hosp Epidemiol 2021;42:775–7. 10.1017/ice.2021.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Burger AE, Reither EN, Mamelund S-E, Lim S. Black-white disparities in 2009 H1N1 vaccination among adults in the United States: a cautionary tale for the COVID-19 pandemic. Vaccine 2021;39:943–51. 10.1016/j.vaccine.2020.12.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Shaw J, Hanley S, Stewart T, Salmon DA, Ortiz C, Trief PM, et al. Healthcare personnel (HCP) attitudes about coronavirus disease 2019 (COVID-19) vaccination after emergency use authorization. Clin Infect Dis 2022;75:e814–21. 10.1093/cid/ciab731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hamel L. KFF COVID-19 Vaccine Monitor: December 2020. Published: Dec 15, 2020. https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/. n.d. [Google Scholar]
- [22].Meyer MN, Gjorgjieva T, Rosica D. Trends in health care worker intentions to receive a COVID-19 vaccine and reasons for hesitancy. JAMA Netw Open 2021;4: e215344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Padamsee TJ, Bond RM, Dixon GN, Hovick SR, Na K, Nisbet EC, et al. Changes in COVID-19 vaccine hesitancy among black and white individuals in the US. JAMA Netw Open 2022;5:e2144470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Momplaisir FM, Kuter BJ, Ghadimi F, Browne S, Nkwihoreze H, Feemster KA, et al. Racial/Ethnic differences in COVID-19 vaccine hesitancy among health care workers in 2 Large academic hospitals. JAMA Netw Open 2021;4:e2121931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Green-McKenzie J, Shofer FS, Momplaisir F, Kuter BJ, Kruse G, Bialal U, et al. Factors associated with COVID-19 vaccine receipt by health care personnel at a major academic hospital during the first months of vaccine availability. JAMA Netw Open 2021;4:e2136582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Farah W, Breeher L, Shah V, Hainy C, Tommaso CP, Swift MD. Disparities in COVID-19 vaccine uptake among health care workers. Vaccine 2022;40:2749–54. 10.1016/j.vaccine.2022.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Simonson MD, Chwe H, Lazer D, Ognyanova K, Baum M, Perlis RH, et al. The COVID States Project #49: Vaccinating America’s youth 2021. DOI: 10.31219/osf.io/stacj. [DOI] [Google Scholar]
- [28].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42: 377–81. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Yasmin F, Najeeb H, Moeed A, Naeem U, Asghar MS, Chughtai NU, et al. COVID-19 vaccine hesitancy in the United States: a systematic review. Front Public Health 2021;9:770985. 10.3389/fpubh.2021.770985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Dzieciolowska S, Hamel D, Gadio S, Dionne M, Gagnon D, Robitaille L, et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: a multicenter survey. Am J Infect Control 2021;49:1152–7. 10.1016/j.ajic.2021.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Leigh JP, Moss SJ, White TM, Picchio CA, Rabin KH, Ratzan SC, et al. Factors affecting COVID-19 vaccine hesitancy among healthcare providers in 23 countries. Vaccine 2022;40:4081–9. 10.1016/j.vaccine.2022.04.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Alfieri NL, Kusma JD, Heard-Garris N, Davis MM, Golbeck E, Barrera L, et al. Parental COVID-19 vaccine hesitancy for children: vulnerability in an urban hotspot. BMC Public Health 2021;21:1662. 10.1186/s12889-021-11725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Balasuriya L, Santilli A, Morone J, Ainooson J, Roy B, Njoku A, et al. COVID-19 vaccine acceptance and access among black and latinx communities. JAMA Netw Open 2021;4:e2128575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Phan T-LT, Enlow PT, Wong MK, Lewis AM, Kazak AE, Miller JM. Medical factors associated with caregiver intention to vaccinate their children against COVID-19. Vaccine X 2022;10:100144. DOI: 10.1016/j.jvacx.2022.100144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Reitsma MB, Goldhaber-Fiebert JD, Salomon JA. Quantifying and Benchmarking Disparities in COVID-19 vaccination rates by race and ethnicity. JAMA Netw Open 2021;4:e2130343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Porteny T, Corlin L, Allen JD, Monahan K, Acevedo A, Stopka TJ, et al. Associations among political voting preference, high-risk health status, and preventative behaviors for COVID-19. BMC Public Health 2022;22:225. 10.1186/s12889-022-12633-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Ruiz JB, Bell RA. Parental COVID-19 vaccine hesitancy in the United States. Public Health Rep 2022;137:1162–9. 10.1177/00333549221114346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Szilagyi PG, Shah MD, Delgado JR, Thomas K, Vizueta N, Cui Y, et al. Parents’ intentions and perceptions about COVID-19 vaccination for their children: results from a national survey. Pediatrics 2021;148. 10.1542/peds.2021-052335.e2021052335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Gabarda A, Butterworth SW. Using best Practices to address COVID-19 vaccine hesitancy: the case for the motivational interviewing approach. Health Promot Pract 2021;22:611–5. 10.1177/15248399211016463. [DOI] [PubMed] [Google Scholar]
- [40].Moss WJ, Gostin LO, Nuzzo JB. Pediatric COVID-19 vaccines: what parents, practitioners, and policy makers need to know. JAMA 2021;326:2257–8. 10.1001/jama.2021.20734. [DOI] [PubMed] [Google Scholar]
- [41].Walkey AJ, Law A, Bosch NA. Lottery-based incentive in Ohio and COVID-19 vaccination rates. JAMA 2021;326:766–7. 10.1001/jama.2021.11048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Firew T, Sano ED, Lee JW, Flores S, Lang K, Salman K, et al. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers’ infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open 2020;10:e042752. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.