Key Features.
The Extramural Leiden University Medical Center Academic Network (ELAN) dynamic data infrastructure, based on routine healthcare data of general practitioners, hospitals and mental healthcare, linked to municipal and national data sources from Statistics Netherlands, was established with the aim to facilitate broad research topics to improve integrated patient care and health outcomes.
The dynamic data infrastructure comprises 2.6 million individuals spanning all age groups residing in South Holland province from 2007 onwards, with a diverse mix of urban and rural residents. This data infrastructure is updated on an annual basis. If residents relocate out of the area, information on death diagnoses, medication and morbidity is still accessible through national data sources.
ELAN has coded clinical measurements, laboratory findings, morbidities, medication use, healthcare contacts and referrals. By pseudonymized linkage procedures, claims data, death diagnoses and social determinants of health are also included. Although free text is not readily available in the data set, lifestyle information data have been extracted by applying text mining and natural language processing within the separate data sources (e.g. electronic patient files).
ELAN represents a collaborative effort of the regional academic and regional healthcare organizations.
Requests for research collaborations and questions regarding procedures for data access, can be addressed to ELAN@LUMC.NL.
Data resource basics
The Extramural Leiden University Medical Center Academic Network (ELAN) was developed to facilitate healthcare research concerning the major sustainable healthcare challenges Europe and the Netherlands face due to increasing healthcare costs, shortages in healthcare workers, an ageing population and persisting health disparities.1–4
These health disparities remain within and among European countries, with differences in healthy life years between countries reaching up to 20 years.2,5 The European Union considers these health disparities an important population health challenge for Europe and reported ‘a need for improved data, measurements, reporting, and comparisons; and for dedicated, collaborative research’.6,7
Health disparities are difficult to capture through traditional prospective cohorts because of an underrepresentation of low socio-economic groups and ethnic minorities, and due to healthy applicant bias or exclusion of patients based on (non-native) language difficulties.8 Also, although routine healthcare combined with national data sources have their limitations, routine healthcare and national data sources are more inclusive of patients of different socio-economic and ethnic backgrounds. Routine healthcare databases and registries are increasingly employed by healthcare organizations and governmental bodies for research and monitoring of healthcare and health policy improvement programmes.9–12 The Netherlands is a country with a universal healthcare system, in which all citizens are registered with a general practitioner (GP) and all registered citizens are eligible for healthcare coverage in primary and secondary care, leading to a potential integral data source of information from routine healthcare. However, routine healthcare information on individual patients in the Netherlands is dispersed in separate data information systems of municipal, primary, secondary healthcare and national data sources. Apart from linkage based on hospital and death diagnoses, these separate routine healthcare systems were previously not linked across their silo boundaries for monitoring healthcare changes or research purposes.
To study these healthcare challenges in the whole spectrum of primary and secondary routine healthcare data across the silo boundaries, ELAN was established in 2019 by the regional healthcare organizations of primary and secondary care and public health organizations.3 When available, data of regional routine healthcare data sources were retrospectively included from the year 2007 onwards. ELAN is funded by regional healthcare organizations, Leiden University and Leiden University Medical Centre.
ELAN is sourced from various data sets to form a dynamic population-based data infrastructure in the Netherlands containing information of 2.6 million individuals from the cities of The Hague, Zoetermeer, Leiden and the surrounding more rural areas (the middle and northern part of South Holland province) (Figure 1). ELAN includes regional routine healthcare information from different sources: GP practices, hospitals and mental healthcare linked to national data sources from Statistics Netherlands and information from municipalities. ELAN includes individuals from a large variety of areas, ranging from extremely urbanized areas (the cities of The Hague and Zoetermeer), suburban areas (e.g. Rijswijk) and also a rural area (e.g. the Dune and Flower bulb area). Compared with the Dutch average, the urban population is relatively oversampled within ELAN (in the ELAN area, 97% of the population live in an address-dense area compared with the Dutch average of 67%) (Table 1). The population in ELAN is more ethnically diverse than that in the Netherlands in general. In comparison with the national average, the proportion of the highest income group is larger compared with national data (quintile groups based on national disposable household income) and the proportion of the lowest income group in ELAN is smaller, except for the data from the cities of The Hague and Zoetermeer, where the lowest income group is larger (Supplementary Table S1, available as Supplementary data at IJE online). Regarding comorbidities, mortality by grouped major causes of death in ELAN is comparable with the Netherlands as a whole, although cardiovascular mortality and mortality due to neoplasms are somewhat lower (potentially because the population is younger) (Table 2).
Figure 1.
Region of the Extramural Leiden University Medical Center Academic Network (ELAN) in the Netherlands, middle and northern parts of the province of South Holland
Table 1.
Characteristics of the Extramural Leiden University Medical Center Academic Network (ELAN) population, by data source, 2007–22, and the population of the Netherlands, 2014
| ELAN |
|||||||
|---|---|---|---|---|---|---|---|
| Characteristic | SN a | GPs b | Hospitals c | MHC d | Perined children e | Perined mothers e | The Netherlands f |
| Total populationg | 2 611 953 | 734 519 | 2 168 282 | 409 020 | 371 035 | 239 615 | 16 829 289 |
| Mid-year population 2021h | 1 719 617 | 572 930 | 1 595 887 | 286 572 | 316 760 | 183 964 | 17 533 043 |
| Women (%) | 50.0 | 51.5 | 51.2 | 54.1 | 49.0 | 100.0 | 50.0 |
| Age (years) [mean (SD)] | 31.7 (22.6) | 32.1 (23.6) | 32.3 (23.0) | 33.0 (20.0) | 2.1 (4.1) | 29.2 (7.8) | 41.0 |
| Person-years [median (IQR)] | 12.4 (3.7–16.0) | 16.0 (8.1–16.0) | 15.4 (6.5–16.0) | 16.0 (7.6–16.0) | 10.7 (5.5–16.0) | 16.0 (8.7–16.0) | NA |
| Age category (years) (%) | |||||||
| <18 | 27.8 | 32.4 | 28.9 | 23.6 | 96.9 | 6.9 | 20.2 |
| 18–65 | 63.1 | 57.6 | 61.4 | 68.2 | 3.1 | 93.1 | 61.9 |
| ≥65 | 9.1 | 10.0 | 9.7 | 8.3 | NA | NA | 17.9 |
| Urbanization (addresses/km2)i (%) | |||||||
| Extremely urbanized (>2500) | 66.6 | 58.2 | 64.8 | 69.7 | 66.0 | 68.8 | 21.0 |
| Strongly urbanized (1500–2500) | 17.1 | 32.5 | 18.4 | 16.6 | 19.7 | 18.8 | 24.1 |
| Moderately urbanized (1000–1500) | 13.0 | 6.8 | 13.1 | 11.1 | 11.4 | 9.8 | 17.9 |
| Hardly urbanized (500–1000) | 3.3 | 2.3 | 3.6 | 2.7 | 3.0 | 2.6 | 18.5 |
| Not urbanized (<500) | 0.0 | 0.2 | 0.0 | 0.0 | 0.0 | 0.0 | 18.5 |
| Disposable household incomej (%) | |||||||
| 1st quintile (lowest) | 23.7 | 17.4 | 21.8 | 26.9 | 22.4 | 23.3 | 20.0 |
| 2nd quintile | 15.6 | 16.4 | 15.7 | 17.4 | 16.2 | 15.2 | 20.0 |
| 3rd quintile | 17.9 | 19.5 | 18.5 | 18.6 | 20.7 | 18.8 | 20.0 |
| 4th quintile | 20.0 | 22.3 | 20.8 | 19.0 | 20.8 | 21.0 | 20.0 |
| 5th quintile (highest) | 22.8 | 24.4 | 23.3 | 18.0 | 19.9 | 21.8 | 20.0 |
| Education levelk (%) | |||||||
| Primary to lower secondary | 37.9 | 40.3 | 36.8 | 27.0 | 80.2 | 16.3 | 33.2 |
| Higher secondary or vocational | 28.6 | 30.3 | 29.4 | 38.5 | 18.0 | 34.0 | 38.6 |
| Bachelor’s or master’s | 33.5 | 29.4 | 33.8 | 34.4 | 1.8 | 49.7 | 28.2 |
| Country of originl (%) | |||||||
| The Netherlands | 58.5 | 67.5 | 66.2 | 66.9 | 64.9 | 60.5 | 78.6 |
| Surinam | 3.6 | 3.7 | 4.1 | 5.6 | 3.5 | 5.0 | 2.1 |
| Morocco | 2.6 | 2.9 | 2.9 | 3.6 | 5.0 | 4.5 | 2.2 |
| Indonesia | 2.6 | 2.9 | 2.7 | 2.9 | 0.6 | 2.9 | 2.2 |
| Middle or eastern Europe | 5.6 | 2.7 | 3.3 | 1.8 | 3.0 | 4.0 | 1.2 |
| Turkey | 2.9 | 2.3 | 3.0 | 3.6 | 4.1 | 4.1 | 2.4 |
| Antillean isles | 1.8 | 1.7 | 1.8 | 2.0 | 2.0 | 2.1 | 1.0 |
| UK | 1.3 | 1.0 | 0.9 | 0.9 | 0.9 | 0.8 | 0.5 |
| Germany | 0.8 | 1.0 | 0.9 | 0.9 | 0.1 | 0.5 | 2.2 |
| Other countries | 20.2 | 14.3 | 14.2 | 11.9 | 15.9 | 15.8 | 10.9 |
GP, general practice; IQR, interquartile range; MHC, mental healthcare; NA, not available (unavailable or undisclosed due to low numbers); SN, Statistics Netherlands.
Data on the citizens of the ELAN area from SN and the municipalities.
Data on the citizens of the ELAN area from the affiliated GPs.
Data on citizens of the ELAN area with a hospital claims declaration.
Data on the citizens of the ELAN area with a mental healthcare claims declaration.
Data on the citizens of the ELAN area from the Perined population (national data source with information on pregnancy and perinatal care).
Open-source data on the population of the Netherlands from SN (year 2014 and mid-year population 2021) [13,14].
Total population for years 2007–22.
Population on 1 July 2021.
Urbanization defined by number of addresses per squared kilometre.
Quintile boundaries of disposable household income by the quintile distribution of the Netherlands.
Highest attained and followed education level.
Country of origin of individual or one/both parents (nine largest subgroups of the area).
Table 2.
Mortality grouped by main causes of death in the Extramural Leiden University Medical Center Academic Network (ELAN) population by data source, 2021
| ELAN |
|||||||
|---|---|---|---|---|---|---|---|
| Mortality | SN a | GPs b | Hospitals c | MHC d | Perined children e | Perined mothers e | The Netherlands f |
| Mid-year population | 1 719 617 | 572 930 | 1 595 887 | 286 572 | 316 760 | 183 964 | 17 533 043 |
| Causes of death (deaths/100 000 mid-year population)g | |||||||
| Neoplasms | 239 | 266 | 256 | 216 | NA | 46 | 268 |
| Diseases of the circulatory system | 181 | 174 | 193 | 177 | NA | 8 | 213 |
| Diseases not elsewhere classified | 60 | 51 | 62 | 71 | NA | 8 | 52 |
| Mental and behavioural disorders | 57 | 41 | 60 | 134 | NA | NA | 67 |
| External causes of morbidity and mortality | 54 | 52 | 57 | 103 | NA | 7 | 52 |
| Diseases of the respiratory system | 50 | 45 | 53 | 61 | NA | NA | 57 |
| Diseases of the nervous system | 40 | 33 | 43 | 80 | NA | NA | 47 |
| Diseases of the digestive system | 26 | 24 | 28 | 34 | NA | NA | 28 |
| Endocrine and metabolic diseases | 21 | 18 | 23 | 27 | NA | NA | 20 |
| Diseases of the genitourinary system | 20 | 19 | 21 | 21 | NA | NA | 20 |
| Certain infectious and parasitic diseases | 14 | 12 | 15 | 19 | NA | NA | 16 |
| Diseases of the musculoskeletal system | 6 | 4 | 7 | 8 | NA | NA | 6 |
| Perinatal period | 3 | NA | 1 | NA | NA | NA | 2 |
| Congenital malformations | 3 | NA | 3 | NA | NA | NA | 2 |
| Diseases of the blood (-forming organs) | 3 | 3 | 3 | NA | NA | NA | 3 |
| Diseases of the skin | 2 | 2 | 2 | NA | NA | NA | 2 |
GP, general practice; MHC, mental healthcare; NA, not available (unavailable or undisclosed due to low numbers); SN, Statistics Netherlands.
Data on the citizens of the ELAN area from SN and the municipalities.
Data on the citizens of the ELAN area from the affiliated general practices.
Data on citizens of the ELAN area with a hospital claims declaration.
Data on the citizens of the ELAN area with a mental healthcare claims declaration.
Data on the citizens of the ELAN area from the Perined population (national data source with information on pregnancy and perinatal care).
Open-source data on the population of the Netherlands from SN [13].
Mortality from the Dutch National Death Registry, grouped by main causes of death according to the International Classification of Diseases, 10th revision (Grouping, Supplementary Table S2, available as Supplementary data at IJE online).
The participating GP practices, hospitals and other data suppliers inform their patients about pseudonymized use of their healthcare data for research purposes, and individuals can withdraw via an informed opt-out procedure. Opt-out preference is digitally marked in the records of patients, and these data are excluded from data sharing. For each new study, consent is required from the ELAN research board and from the data suppliers (e.g. GP network, hospitals, municipality, mental healthcare, Statistics Netherlands). Data are analysed in a data-secured environment of Statistics Netherlands, facilitating that health can be studied prospectively over a lifetime across data sources.
In summary, with ELAN, the collaborating regional healthcare organizations aim to facilitate (epidemiological) research on many different topics (e.g. etiological, prediction, diagnostic, descriptive, syndemics, healthcare costs, disease trends) in order to help improve integrated patient care, health outcomes, cost-effective person-centred healthcare and alignment of health policies across care settings.3
Data collected
The number of individuals in the data infrastructure is increasing. At present, ELAN GP contains information on 734 000 individuals, but it is anticipated to surpass >1 million participants in 2024. ELAN contains data from regional routine healthcare from GPs, hospitals, mental healthcare organizations on medical information (e.g. diagnoses, medical history, laboratory findings, measurements, medication prescriptions, referral information) and information on pregnancies, births and first 28 days of newborn children (Perined).15 Medical information is combined with data from national data sources and municipal registries, with, among others, information on demographics, mortality, health expenditure, COVID-19, social determinants of health (SDOH; income, education, ethnicity by country of origin, urbanization), claims-based diagnoses (mental healthcare, hospital and chronic care) and municipal information on the utilization of the social support act (broad categories; see Table 3). Data were collected from 2007 onwards, with an ongoing annual update. Via a secure link, data are uploaded to Statistics Netherlands, which functions as the trusted third party, meaning that this organization pseudonymizes the data and attaches a unique number to individuals, which allows individual linkage across the different sources. Harmonizing the data happens at various stages in the process. Data are uploaded by the (healthcare) organizations to the data safe at Statistics Netherlands. Different health organizations with different information systems may deliver data in different formats and with different structures. These data are stored as is, and harmonization takes place when data sets for the various research projects are compiled by data managers.
Table 3.
Measurements available in the Extramural Leiden University Medical Center Academic Network
| Source | Measurements |
|---|---|
| GPs and hospitals | Laboratory findings and measurements (e.g. glucoses, creatinine, haemoglobin, cholesterol and lipids) |
| Information in structured fields (e.g. smoking status, blood pressure, oxygen level, alcohol use) | |
| Diagnoses (ICPC/ICD-10/DBC) | |
| Referral information | |
| Medication (ATC8) | |
| Contraindication for medications (ATC8) | |
| Contact information (e.g. frequencies, GP, emergency room visits, in- and outpatients) | |
| Procedures [diagnoses–treatment combinations (DBC), hospital care] | |
| Custom (e.g. results calcium score, text-mining smoking information) | |
| SN | Demographic information (e.g. country of origin, marital status, number of household members) |
| DBC, hospital care | |
| Healthcare costs (long-term care act and health insurance act; e.g. GP, hospital, physiotherapy, specialized psychiatric care) | |
| Medication (ATC4) | |
| National cause-of-death registry (ICD-10) | |
| Socio-economic information (e.g. household/personal income, debts, highest attained education, occupation, socio-economic area code) | |
| Health monitor (survey, random population samples 2012, 2016, 2021) | |
| Other (youth disability aid, parenting support, children’s psychiatric care 2016 and onward) | |
| Environment (sewage measurements, air pollution) | |
| Municipal health service | COVID-19 |
| Municipal social support | Disability tools and support in the domain of the Social Support Act (2017–present) |
| Open source | Neighbourhood quality-of-life ranking meter (every other year), criminality (2010–present) |
| Psychiatry | Diagnoses (DSM 5/DBC), GAF scores |
| Perined | Information on pregnancies and births from gynaecologists and midwives (e.g. hypertensive disorders of pregnancy, gestational diabetes, birthweight) |
ATC, Anatomical Therapeutic Chemical code; DBC, diagnosis–treatment combination; DSM, Diagnostic and Statistical Manual of Mental Disorders; GAF, Global Assessment of Functioning; GP, general practice; ICD-10, International Classification of Diseases 10th Revision; ICPC, International Classification of Primary Care; SN, Statistics Netherlands.
In an online repository, code for ingestion, cleaning, imputation and pre-processing is standardized and available to the public. Code for common analysis task is also gradually added to this repository, as will code for the complete reproduction of results presented in future publications based on ELAN data. All analyses are done within the secured data environment of Statistics Netherlands and, after analyses, Statistics Netherlands performs an output check; this check certifies that data are non-retraceable to individuals (anonymized).
Updates and known information on missing data
Information on Statistics Netherlands and from regional routine healthcare data from GPs, hospitals, Perined and mental healthcare are annually updated.
For new data sources, when available, data from 2007 onwards are retrospectively included.
When individuals move out of the area, information on important outcome measures such as medical diagnoses and mortality are available in national registries (medical diagnoses from a declaration-based register and national cause-of-death register). Approximately 1% of the Dutch population emigrates, with no follow-up information on diagnoses and deaths.16
When Dutch citizens die in another country, the cause of death remains unknown (registered by the National death national data sources as ‘unknown cause of death’, ICD10 R99); in 2018, this was 1.2% of all deaths.16
Known information on missing data in GP files is described in Table 4.
Table 4.
Percentages of missing data in the general practice total population and subgroups in the Extramural Leiden University Medical Center Academic Network
|
Age (years)
b
|
|||||
|---|---|---|---|---|---|
| Characteristic | Overall GP | Diabetes a | <18 | 18–65 | ≥65 |
| N | 734 519 | 49 689 | 238 282 | 422 807 | 73 430 |
| Demographics (%)c | |||||
| Sex | 0 | 0 | 0 | 0 | 0 |
| Age | 0 | 0 | 0 | 0 | 0 |
| Person-years | 0 | 0 | 0 | 0 | 0 |
| Disposable household income | 4.5 | 1.6 | 6.7 | 3.5 | 3.2 |
| Education | 34.4 | 64.4 | 4.4 | 40.9 | 94.0 |
| Country of origin | 0 | 0 | 0 | 0 | 0 |
| Municipality | 0 | 0 | 0 | 0 | 0 |
| Laboratory findings and measurements (%)c | |||||
| ALAT | 56.0 | 16.7 | 78.4 | 47.6 | 32.1 |
| Creatinine | 49.7 | 6.4 | 76.0 | 39.6 | 23.0 |
| Haemoglobin | 43.1 | 11.4 | 62.1 | 35.7 | 24.1 |
| Sedimentation rate | 48.6 | 16.4 | 68.8 | 41.0 | 26.7 |
| Total cholesterol | 64.3 | 9.8 | 95.7 | 51.7 | 34.9 |
| TSH | 51.6 | 20.3 | 72.3 | 43.2 | 32.9 |
| Smoking status | 69.3 | 17.1 | 91.6 | 60.0 | 50.2 |
| Systolic blood pressure | 54.5 | 7.6 | 81.7 | 44.1 | 26.2 |
| Weight | 64.9 | 12.3 | 75.0 | 62.6 | 44.6 |
ALAT, alanine aminotransferase; GP, general practice; TSH, thyroid-stimulating hormone.
Population with a type 2 diabetes diagnosis before or during follow-up.
Age when entering the data infrastructure (entry date before 2007; date was capped at 1 January 2007).
Percentage of missing data.
Data resource use
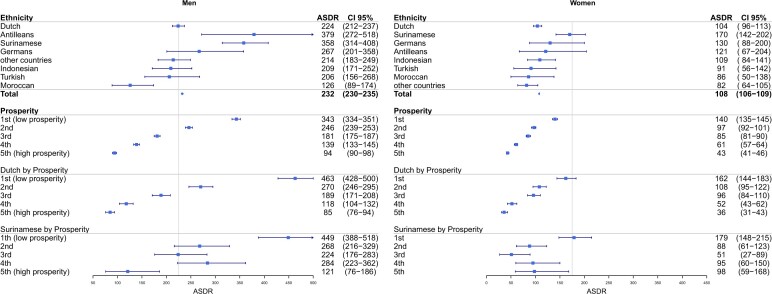
The ELAN data infrastructure has been used for a wide range of research projects. A list of publications can be found on the ELAN research website (www.elanresearch.nl). Research projects showed large health disparities in cardiovascular death and morbidity in ethnic and socio-economic subgroups, with the number of cardiovascular deaths 5 times higher in low socio-economic groups compared with high socio-economic subgroups, and a 2–3.5 times higher occurrence of cardiovascular death in Surinamese (mainly South Asian) and Caribbeans (Figure 2).17 In the external validation of the primary care prediction models (SCORE2 and SCORE2-DM), cardiovascular events were underpredicted in Surinamese-South Asians and low socio-economic subgroups.18 In a multi-ethnic diabetes study, a non-Western origin was positively associated with the development of diabetes complications.19 Another study performed with ELAN data found that people with diabetes with and without a registered mental disorder showed no difference in the achievement of diabetes treatment targets.20 Two descriptive studies on antibiotics use showed a lack of registration of side effects and lower prescription of antibiotics during the SARS-CoV-2 wave compared with the 2020 influenza season.21,22 Another two studies explored the relationship between persistent somatic symptoms and symptoms, medication use and referrals.23,24 A study explored the predictors of inappropriate proton pump inhibitor use.25 There was a natural language-processing study on lifestyle characteristics.26 Also, choices made in pre-processing (Dutch) routine healthcare data for research were described.27
Figure 2.
Age-standardized cardiovascular death rates in the city of The Hague, the Netherlands, reproduced from Kist et al.17 ASDR, age-standardized cardiovascular death rate (/100 000 person-years), standardization to the World population, 2007–18 (with 95% CI). Cut-off line, European Society of Cardiology-determined ASDR cut-off for high- and low-risk countries, cut-off men 225/100 000, women 175/100 000. Cardiovascular deaths, International Classification of Diseases 10th Revision diagnoses I00–I99. Ethnicity, according to country of birth (person or parent). Prosperity, disposable household income combined with household wealth, in quintiles of the population, 2012–18
Ongoing research projects focus on a large variety of topics, namely cardiometabolic, SDOH, mental healthcare, surgery, orthopaedics, infectious diseases, antibiotic use, lifestyle interventions, neighbourhood interventions, pollution and diseases, kidney diseases, sex, age and gender differences, ageing population, syndemics in vulnerable populations, mental health disorders and cognitive impairment. Other projects concentrate on developing a transmural benchmark, tracking disease occurrences, monitoring disease trends and conducting implementation research to assess the impact of population health management and prevention projects. Current international collaborative efforts with similar data infrastructures in Australia, Scotland and Denmark will allow cross-border comparisons on diabetes care and health outcomes.
Strengths and weaknesses
ELAN has various strengths. First, traditional cohorts usually have an underrepresentation of individuals from a low socio-economic background and/or with different ethnicities, whereas routine healthcare databases and registries are inclusive of all individuals in countries with a universal healthcare system (as the Netherlands is). Second, the combination of multilevel routine healthcare data from GPs, hospitals and mental healthcare, linked with the wealth of information on Statistics Netherlands, is unique, making ELAN the only data infrastructure so far in the Netherlands in which detailed information from these sources is combined for research on health inequities/disparities and other topics. Last, in order to follow trends after healthcare changes, next to information on determinants of health, healthcare costs are also available in the data set (albeit currently with a delay of 2–3 years).
This data infrastructure also has several limitations. First, routine healthcare data are recorded for patient care, not for research. Research biases can partly be mitigated by combining the variables and outcomes from different sources longitudinally. Second, in routine healthcare data, information on variables, such as smoking, cholesterol and blood pressure, is often missing. Missingness is comparable with those of other established observational routine healthcare data infrastructures such as QResearch Practices and Clinical Practice Research Datalink, and work is being done on improving data quality through complementing coded data using free text analytical techniques (text mining and natural language processing).28–30 Finally, the country of origin is the only available source as a proxy for ethnicity. Information on self-perceived ethnicity is not available in the data set.
Data resource access
ELAN is governed by the ELAN LUMC Management Team. Requests for collaborations by national and international academic parties are welcomed on broad topics and can be addressed to ELAN at the Leiden University Medical Centre (www.elanresearch.nl or D.O.Mook-Kanamori@LUMC.nl).
Research proposals are assessed on scientific quality; public benefit; medical ethical considerations; adherence to Dutch legislation, General Data Protection Regulation, Statistics Netherlands legislation and risk for study patients, according to the ELAN Scientific Research Process.
The data underlying this article cannot be shared publicly due to Dutch legislation to ensure the privacy of individuals. For approved collaborative projects, data will be shared.
Ethics approval
ELAN adheres to Dutch and European privacy and research legislation, and procedures have been implemented to protect patient confidentiality. Routinely collected data were anonymized through a trusted third party and Statistics Netherlands to prevent identification of individuals by researchers. In accordance with Dutch legislation, GPs and hospitals informed individuals about the use of their anonymized data for research purposes and individuals could withdraw via an informed opt-out procedure; informed consent from individuals in the study was waived and not obtained. For this waiver, the appropriate approval that the study is not subject to the Medical Examination Act was granted, after evaluation of the research protocol by the authority of the area (Medical Ethical Committee LUMC Leiden, under reference number G18.070).
Supplementary Material
Acknowledgements
We are grateful to the patients, GPs, hospitals, Mental Health Care and Statistics Netherlands for allowing us to access their anonymized health data. We acknowledge all funders and collaborators for making ELAN possible.
Contributor Information
Janet M Kist, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Hedwig M M Vos, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Rimke C Vos, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Albert T A Mairuhu, Department of Internal Medicine, HAGA Teaching Hospital, The Hague, The Netherlands.
Jeroen N Struijs, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands; Department of National Health and Healthcare, National Institute for Public Health and the Environment, Bilthoven, The Netherlands.
Robert R J M Vermeiren, Department of Child and Adolescent Psychiatry LUMC Curium, Leiden University Medical Centre, Leiden, The Netherlands; Parnassia Psychiatric Institute, The Hague, The Netherlands.
Petra G van Peet, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Hendrikus J A van Os, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Frank H Ardesch, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Edith D Beishuizen, Department of Internal Medicine, HMC Hospital, The Hague, The Netherlands.
Yvo W J Sijpkens, Department of Internal Medicine, HMC Hospital, The Hague, The Netherlands.
Margot W M de Waal, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Marcel R Haas, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Rolf H H Groenwold, Department of Clinical Epidemiology, Leiden University Medical Centre, Leiden, The Netherlands; Department of Biomedical Data Science, Leiden University Medical Centre, Leiden, The Netherlands.
Mattijs E Numans, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Dennis Mook-Kanamori, Department of Public Health & Primary Care, National eHealth Living Lab and Health Campus, Leiden University Medical Center, The Hague and Leiden, The Netherlands.
Supplementary data
Supplementary data are available at IJE online.
Author contributions
J.K., H.V., R.V., A.M., J.S., R.V., P.P., H.D., F.A., E.B., Y.S., M.W., M.H., R.G., M.N. and D.M. contributed to the conception and design of the study. The data were analysed by J.K., and the underlying data were accessed and verified by J.K. and D.M. J.K. drafted the manuscript and figures. All authors critically revised the manuscript. All authors read and approved the final version.
Funding
This work was supported by academic resources of Leiden University Medical Center and University Leiden.
Conflict of interest
None declared.
References
- 1. Directorate-General for Economic and Financial Affairs. The 2018 Ageing Report: Economic and Budgetary Projections for the EU Member States (2016–2070). 2018. https://economy-finance.ec.europa.eu/publications/2018-ageing-report-economic-and-budgetary-projections-eu-member-states-2016-2070_en (28 December 2023, date last accessed).
- 2. Cristea M, Noja GG, Stefea P, Sala AL.. The impact of population aging and public health support on EU labor markets. Int J Environ Res Public Health 2020;17:1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ardesch FH, Meulendijk MC, Kist JM. et al. The introduction of a data-driven population health management approach in the Netherlands since 2019: the Extramural LUMC Academic Network data infrastructure. Health Policy 2023;132:104769. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organisation. Left Behind: Inequalities in the Negative Impacts of the COVID-19 Pandemic among Adolescents in the WHO European Region: Impact of the COVID-19 Pandemic on Young People’s Health and Well-Being from the Findings of the HBSC Survey Round 2021/2022. https://www.who.int/europe/publications/i/item/WHO-EURO-2023-8920-48692-72363 (7 February 2024, date last accessed).
- 5. Communication from the Commission to the European Parliament, The Council, The European Economic and Social Committee and the Committee of the Regions. Solidarity in Health: Reducing Health Inequalities in the EU. 2009. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A52009DC0567 (29 December 2023, date last accessed).
- 6. European Parliament. Directorate General for Parliamentary Research Services. Addressing Health Inequalities in the European Union: Concepts, Action, State of Play: In Depth Analysis. LU: Publications Office, 2020. https://data.europa.eu/doi/10.2861/567478 (29 December 2023, date last accessed).
- 7. European Commission. Supporting Mental Health and Care for the Wellbeing of Vulnerable Children and Young Peoplehttps://reform-support.ec.europa.eu/what-we-do/labour-market-social-protection-and-migration/supporting-mental-health-and-care-wellbeing-vulnerable-children-and-young-people_en (28 December 2023, date last accessed).
- 8. Lash TL, VanderWeele TJ, Haneuse S, Rothman KJ.. Modern Epidemiology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2021. [Google Scholar]
- 9. Laugesen K, Ludvigsson JF, Schmidt M. et al. Nordic Health Registry-based research: a review of health care systems and key registries. Clin Epidemiol 2021;13:533–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hildebrandt H, Hermann C, Knittel R, Richter-Reichhelm M, Siegel A, Witzenrath W.. Gesundes Kinzigtal Integrated Care: improving population health by a shared health gain approach and a shared savings contract. Int J Integr Care 2010;10:e046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Schmidt M, Schmidt SAJ, Adelborg K. et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol 2019;11:563–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Koebnick C, Coleman KJ, Black MH. et al. Cohort Profile: The KPSC Children’s Health Study, a population-based study of 920 000 children and adolescents in southern California. Int J Epidemiol 2012;41:627–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Statistics Netherlands, Centraal Bureau voor de Statistiek. Doodsoorzakenstatistiek. https://www.cbs.nl/nl-nl/onze-diensten/methoden/onderzoeksomschrijvingen/korte-onderzoeksomschrijvingen/doodsoorzakenstatistiek (4 Januari 2024, date last accessed).
- 14. Statistics Netherlands. StatLine. https://opendata.cbs.nl/statline/#/CBS/en/ (28 April 2024, date last accessed).
- 15. Perined. https://www.perined.nl/ (28 April 2024, date last accessed).
- 16. Statistics Netherlands. StatLine—Overledenen; Belangrijke Doodsoorzaken (Korte Lijst), Regio. https://opendata.cbs.nl/#/CBS/nl/dataset/80202ned/table?ts=1684925282672 (4 January 2024, date last accessed).
- 17. Kist JM, Smit GWG, Mairuhu ATA. et al. Large health disparities in cardiovascular death in men and women, by ethnicity and socioeconomic status in an urban based population cohort. EClinicalMedicine 2021;57:101120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kist JM, Vos RC, Mairuhu ATA. et al. SCORE2 cardiovascular risk prediction models in an ethnic and socioeconomic diverse population in the Netherlands: an external validation study . EClinicalMedicine 2023;57:101862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nieuwenhuijse EA, Van Hof TB, Numans Mattijs E, Struijs JN, Vos RC.. Are social determinants of health associated with the development of early complications among young adults with type 2 diabetes? A population based study using linked databases. Prim Care Diabetes 2023;17:168–74. [DOI] [PubMed] [Google Scholar]
- 20. Nieuwenhuijse EA, Struijs JN, Sutch SP, Numans Mattijs E, Vos RC.. Achieving diabetes treatment targets in people with registered mental illness is similar or improved compared with those without: analyses of linked observational datasets. Diabet Med 2022;39:e14835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sijbom M, Büchner FL, Saadah NH, de Boer MG, Numans ME.. Comparing antibiotic prescriptions in primary care between SARS-CoV-2 and influenza: a retrospective observational study. BJGP Open 2022;6(4):BJGPO.2022.0049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sijbom M, Braun KK, Büchner FL. et al. Cues to improve antibiotic-allergy registration: a mixed-method study. PLoS One 2022;17:e0266473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kitselaar WM, Büchner FL, van der Vaart R. et al. Early identification of persistent somatic symptoms in primary care: data-driven and theory-driven predictive modelling based on electronic medical records of Dutch general practices. BMJ Open 2023;13:e066183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kitselaar WM, Numans ME, Sutch SP, Faiq A, Evers AW, van der Vaart R.. Identifying persistent somatic symptoms in electronic health records: exploring multiple theory-driven methods of identification. BMJ Open 2021;11:e049907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Koggel LM, Lantinga MA, Büchner FL. et al. Predictors for inappropriate proton pump inhibitor use: observational study in primary care. Br J Gen Pract 2022;72:e899–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Muizelaar H, Haas M, van Dortmont K, van der Putten P, Spruit M.. Extracting patient lifestyle characteristics from Dutch clinical text with BERT models. BMC Med Inform Decis Mak 2024;24:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Os HJA, Kanning JP, Wermer MJH. et al. Developing clinical prediction models using primary care electronic health record data: the impact of data preparation choices on model performance. Front Epidemiol 2022;2:871630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hippisley-Cox J, Coupland C, Brindle P.. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357:j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. University of Oxford, EMIS Health, QResearch. https://www.qresearch.org/ (24 January 2024, date last accessed).
- 30. Herrett E, Gallagher AM, Bhaskaran K. et al. Data Resource Profile: Clinical Practice Research Datalink (CPRD). Int J Epidemiol 2015;44:827–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.