Abstract
Background
Spinal Infection (SI) is associated with various comorbidities. The interaction of these comorbidities and their impact on costs and complexity of care has not been fully assessed.
Methods
This is a retrospective cohort study of SI patients in an urban hospital system to characterize comorbidities and outcomes in adult patients with SI. Adult patients in our hospital system who were hospitalized with an initial diagnosis of SI between July 1, 2017 and June 30, 2019 were included. Outcomes measures included length of stay (LOS) of the index hospitalization for SI, charges and payments for the index hospitalization, and hospital readmissions within one year after discharge from the index hospitalization. Data was obtained by querying our Electronic Data Warehouse (EDW) using ICD-10-CM and CPT procedure codes. Spearman's correlation was used to summarize the relationships between LOS, charges, and payments. Multivariable linear regression was used to evaluate associations of demographics, comorbidities, and other factors with LOS. Multivariable Cox regression was used to evaluate associations of demographics, comorbidities, and other factors with hospital readmissions.
Results
403 patients with a first diagnosis of SI were identified. The average number of comorbidities per patient was 1.3. 294 (73%) had at least 1 medical comorbidity, and 54 (13%) had 3 or more comorbidities. The most common medical comorbidities were diabetes mellitus (26%), intravenous drug use (IVDU, 26%), and malnutrition (20%). 112 patients (28%) had a surgical site infection (SSI). DM (p<.001) and SSI (p=.016) were more common among older patients while IVDU was more common among younger patients (p<.001). Median LOS was 12 days. A larger number of medical comorbidities was associated with a longer LOS (p<.001) while the presence of a SSI was associated with a shorter LOS (p=.007) after multivariable adjustment. LOS was positively correlated with both charges (r=0.83) and payments (r=0.61). Among 389 patients discharged after the index hospitalization, 36% had a readmission within 1 year. The rate of readmission was twice as high for patients with three or more comorbidities than patients with zero comorbidities (hazard ratio: 1.95, p=.017).
Conclusions
Patients with SI often have multiple comorbidities, and the specific type of comorbidity is associated with the patient's age. The presence of multiple comorbidities correlates with initial LOS, cost of care, and readmission rate. Readmission in the first year post-discharge is high.
Keywords: Spinal infection, Hospital readmission, Length of stay, Comorbidity, IVDU, Diabetes
Background
Spinal infection (SI), a complex disease process which includes vertebral osteomyelitis, discitis, and epidural abscess, has been shown to be increasing in both regional and national evaluations [1,2]. Risk factors associated with SI include opioid substance abuse (OSA), multiple drug substance abuse (MDSA), diabetes mellitus (DM), prior spinal surgery, endocarditis, chronic kidney disease (CKD), cirrhosis, malnutrition, and HIV [[3], [4], [5], [6], [7], [8]]. Rising rates of OSA, MDSA, malnutrition, and DM since 2003 have been suggested as factors in the concurrent increased frequency of hospitalizations for SI [1,2]. These correlations were drawn based on state and national level information, compiled from large summary databases. A patient level analysis of the factors behind this increase has not been performed.
The clinical presentation, risk factors, initial treatment, and final outcome of patients with SI form the basis of many prior clinically focused papers [[9], [10], [11], [12]]. Less robustly evaluated in these studies are the effects of multiple comorbidities and complexity of care in these patients. Most patients with SI initially require hospitalization to treat the infection. Some of these hospitalizations may be prolonged and complex, requiring surgical intervention and high level of care. All patients require close monitoring and extended outpatient follow-up: 4–8 weeks of antibiotics, lab testing, and, often, imaging. Despite regular outpatient clinic visits, these patients are at risk for hospital readmissions. The likelihood of readmission following the initial hospitalization has not been assessed to our knowledge. Given the initial hospitalization and extended follow-up care, costs of care in this population can be great. This component has also not been evaluated to our knowledge.
We performed a retrospective review of patients with SI in our hospital system over a 3-year period. Our primary aim was to assess the comorbidities and their potential effects in this population. Did our local population comorbidity profile mirror that documented in the literature? What risk factors or comorbidities increase the complexity of care in this patient population? Secondary aims explored the charges and costs associated with hospitalization for SI and risk factors for rehospitalization.
Methods
Patient cohort
This was an IRB-approved retrospective review of patients in our hospital system who were hospitalized with an initial diagnosis of SI (index hospitalization) between July 1, 2017 and June 30, 2019. Our hospital system includes a level I trauma center serving a five-state region, a university tertiary/quaternary care referral hospital, a community hospital, and multiple primary care clinics. The level I trauma hospital is also a safety net hospital and a referral center for complex spine and neurosurgical cases.
The primary data source was the local hospital system Enterprise Data Warehouse (EDW), a centralized data system that stores current and historical data reflecting a patient's use of our hospital system. Patients with SI were identified by their discharge ICD-10-CM codes (Supplemental Table 1). Codes were verified by an internal audit of a test cohort hospitalized between January-June 2017 and correlated with codes documented in the literature. Each patient's earliest hospitalization for SI within the baseline study period was selected as the index hospitalization. All patients identified by the initial EDW query underwent a subsequent chart review to confirm the presence of SI and date of the index hospitalization. Patients found to not have SI or whose identified hospitalization was not the index hospitalization were excluded.
Medical comorbidities and risk factors
The following information from the index hospitalization was extracted from the EDW or chart review: dates of admission and discharge, length of stay (LOS), discharge status, age, sex, race, ethnicity, primary spoken language, insurance status, spinal surgery during index hospitalization, whether the current SI was associated with a surgical site infection (SSI), medical comorbidities, and hospital charges. Most medical comorbidities were identified using ICD-10-CM codes present in the patient's chart up to 1 year prior to the index hospitalization, including cirrhosis, CKD, endocarditis, HIV, malnutrition, and MDSA (Supplemental Table 1). Additional medical comorbidities were identified through an independent chart review that could identify comorbidities that were either not easily identified by the available ICD-10-CM or procedure codes or were not emphasized risk factors reported in the literature. These included chronic spinal cord injury with associated decubitus ulcers and intravenous drug use (IVDU). Spinal cord injury/decubitus ulcers were present in 10% of our cohort, so this was included as a comorbidity. IVDU does not have an assigned ICD-10-CM code so was only discovered on the individual chart review. SSI was also identified during the chart review as patients with SSI were not fully captured using the EDW alone. The reason for this may be multi-factorial, but likely due in part to the different coding systems in place to identify these patients. Additionally, patients whose surgery was performed at an outside facility did not have the CPT4 code in our system, so these patients were missed.
Outcomes after index hospitalizations
Hospital readmissions within one year after discharge from the index hospitalization were also collected from the EDW. Time to readmission was defined as the time between the date of discharge from the index hospitalization and the date of first readmission. Each readmission was associated with one or more ICD-10-CM codes indicating the reason(s) for the hospitalization. Each readmission was classified based on the presence of an ICD-10-CM code indicating SI (Supplemental Table 1). There were three tiers of coding: SI was coded as the primary cause for readmission (SI primary diagnosis), SI was coded as present but not as the primary cause for readmission, and SI was not included among the reasons for readmission. We did not evaluate the outpatient clinic visits.
Statistical analysis
Categorical variables were summarized as count (percentage) and continuous variables as median (range). Medical comorbidities were analyzed individually and after grouping patients by the number of medical comorbidities, i.e., patients with no comorbidities, 1 comorbidity, 2 comorbidities, or 3 or more comorbidities. SSI was treated as a separate characteristic or risk factor and not grouped with the medical comorbidities. Trends in the presence of comorbidites with increasing age group were tested using univariable logistic regression. Univariable and multivariable linear regression were used to evaluate associations of demographics, comorbidities, and other factors with LOS during the index hospitalization. LOS was log-transformed to reduce right skewness. The Kaplan-Meier product-limit estimator was used to estimate cumulative rates of readmission after the index hospitalization. Readmission rates were each summarized for all readmissions (any cause), readmissions with SI as one of the causes (SI present), and readmissions with SI identified as the primary cause (SI primary diagnosis). Univariable and multivariable Cox regression were used to evaluate associations of demographics, comorbidities, and other factors with readmissions within 365 days after the index hospitalization. Mulitvariable analysis of readmissions when SI was the primary diagnosis was not conducted due to a relatively small number of events. All statistical calculations were conducted with the statistical computing language R (version 4.0.3; R Foundation for Statistical Computing, Vienna, Austria). Statistical significance defined as 2-sided p<.05.
Results
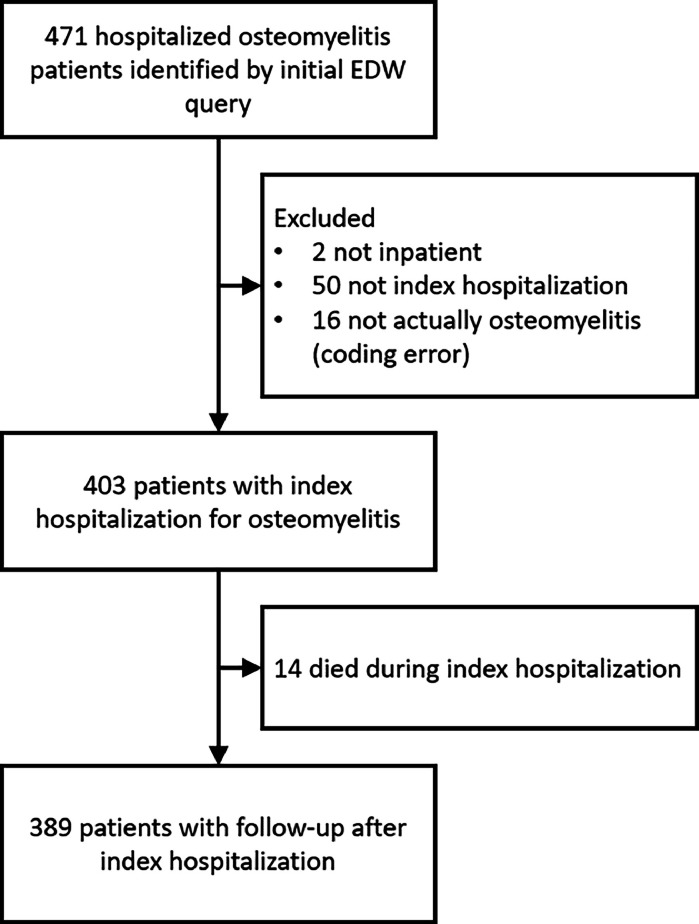
471 patients were initially identified who had a discharge diagnosis of SI from the EDW. As shown in the flow chart (Fig. 1), we excluded patients if they were not inpatients (2), if they were found to not have SI at chart review (16 or 3.4%), or if this was not their first hospitalization for SI at chart review (50 or 10.6%). This left 403 patients with an identified index hospitalization for SI. 14 (3%) patients died during the initial hospitalization. The remaining 389 patients were evaluated for hospital readmissions during the year following the index hospitalization.
Fig. 1.
Patient flowchart. EDW, electronic data warehouse.
Of 403 patients, 58% were male, 83% were white, 4% were Hispanic or Latino, and 97% spoke English as a primary language (Table 1). The median age was 56 years (range: 20 - 96 years) of whom 105 were 18-44 years (26%), 176 were 45-64 years (44%), 116 were 65-84 years (29%), and 6 were 85+ years (1.5%). Insurance coverage for the majority of patients was either Medicaid (38%) or Medicare (40%). 14% had commercial insurance and 7% had other insurance. The majority of patients were treated medically during their index hospitalization, while 135 (33%) required surgical intervention.
Table 1.
Baseline characteristics.
| Variable | Value* |
|---|---|
| Male sex | 232/403 (58%) |
| Age, years | 56 (20-96) |
| White race | 330/396 (83%) |
| Hispanic or Latino ethnicity | 15/392 (4%) |
| Non-Hispanic/Latino White | 309/390 (79%) |
| English PSL | 391/402 (97%) |
| Insurance | |
| Commercial | 58/403 (14%) |
| Medicaid | 155/403 (38%) |
| Medicare | 162/403 (40%) |
| Other | 28/403 (7%) |
| SSI | 112/403 (28%) |
| Medical comorbidities | |
| Cirrhosis | 22/403 (5%) |
| CKD | 64/403 (16%) |
| DM | 105/403 (26%) |
| Endocarditis | 46/403 (11%) |
| Chronic SCI/decubitus ulcer | 40/403 (10%) |
| HIV | 6/403 (1%) |
| Malnutrition | 82/403 (20%) |
| Non-IV drug use | 48/403 (12%) |
| IVDU | 103/403 (26%) |
| Number of medical comorbidities | |
| 0 | 109/403 (27%) |
| 1 | 156/403 (39%) |
| 2 | 84/403 (21%) |
| 3+ | 54/403 (13%) |
PSL, primary spoken language; SSI, surgical site infection; CKD, chronic kidney disease; DM, diabetes mellitus; SCI, spinal cord injury; HIV, human immunodeficiency virus; IV, intravenous; IVDU, intravenous drug user;
Values are no. (%) or median (range).
Overall, the average number of medical comorbidities per patient was 1.3. There were 294 patients (73%) with 1 or more medical comorbidity and there were 54 (13%) with 3 or more medical comorbidities. The most common medical comorbidities were DM (26%), IVDU (26%), and malnutrition (20%). There were 40 patients (10%) with chronic spinal cord injury/decubitus ulcer. A total of 112 patients (28%) had SSI, of whom 50/112 (45%) had at least one medical comorbidity. The pattern of comoribidities differed significantly between patients with and without an SSI. Most patients with an SSI did not have an identified medical comoribidiy (62/112 [55%]). The most common comorbidities among patients with an SSI were DM (24/112 [21%]) and non-IV drug use (16/112 [14%]), while all other comorbidities had a prevalence 0%-7% among these patients. There were 47/403 patients (12%) who did not have any of the medical comorbidities considered nor had an SSI.
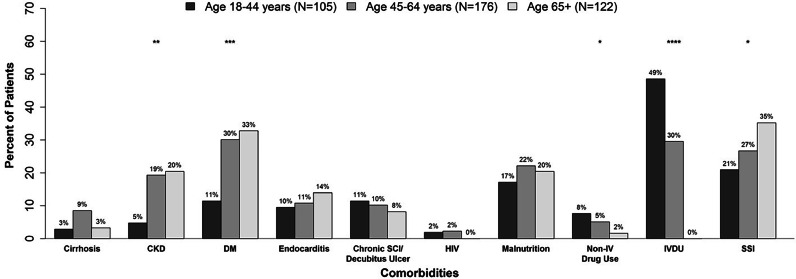
Prevalence of medical comorbidities varied by age group (Fig. 2). In 18-44 year-old patients, IVDU was the most common medical comorbidity (49%), while DM (11%) and CKD (5%) were uncommon. In contrast, patients 65 years and older had significantly higher rates of DM (33%) and CKD (20%) and significantly lower rates of IVDU (0%) than the 18-44 year-old group (p<.001 for each comparison). The 45-64 year-old patients had similar rates of DM (30%) and CKD (19%) as the 65 years+ group and intermediate rates of IVDU (30%) compared to the youngest and oldest groups. Prevalence of malnutrition was similar in all age groups (17-22%, p=.56). SSI became more prevalent with increasing age (21% in patients 18-44 years old to 35% in patients 65 years or older, p=.016).
Fig. 2.
Prevalence of medical comorbidities and SSI by age group. * = statistically significant trends with increasing age group with p<.05; *** = statistically significant trends with increasing age group with p<.001; **** = statistically significant trends with increasing age group with p<.00001. SSI, surgical site infection; CKD, chronic kidney disease; DM, diabetes mellitus; SCI, spinal cord injury; HIV, human immunodeficiency virus; IV, intravenous; IVDU, intravenous drug user.
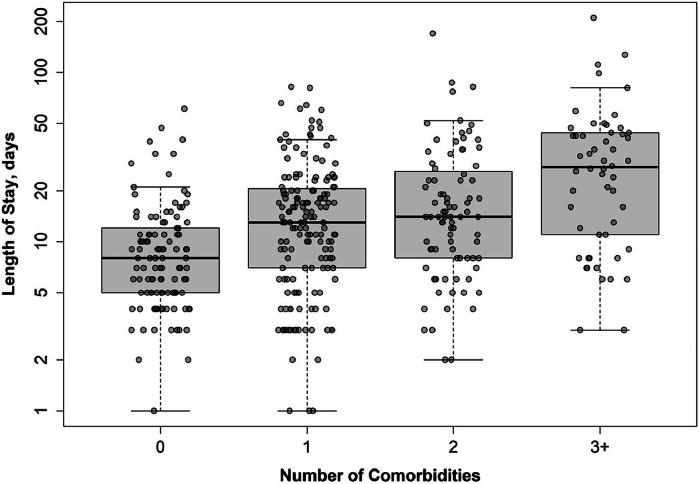
LOS for the index hospitalization was used as a proxy for complexity of care. Median LOS was 12 days (inter-quartile range: 6-23 days). After multivariable adjustment, a higher number of comorbidities was independently associated with longer LOS (mean difference between 0 and 3+ comorbidities: 141.5%, 95% CI: 76.7%-229.9%, p<.001) (Fig. 3, Table 2). Furthermore, patients with SSI had a shorter LOS than those without SSI after controlling for medical comorbidities and other characteristics (mean difference: 25.4%, 95% CI: 7.9-39.5%, p=.007) (Table 2). The individual medical comorbidities independently associated with longer LOS in the multivariable analysis included malnutrition (mean difference: 64.8%, 95% CI: 31.8-106.1, p<.001), chronic spinal cord injury/decubitus ulcer (mean difference: 41.8%, 95% CI: 4.8-91.7%, p=.024), and CKD (mean difference: 27.7%, 95% CI: -0.9-64.4%, p=.058) (Table 2). Median charges for index hospitalization were $128,917 (IQR: $68,344, $254,625) and median payments were $36,635 (IQR: $19,175, $73,449). LOS was significantly correlated with both higher charges (Spearman's r=0.83) and higher payments (Spearman's r=0.61). 135 patients (33%) had spinal surgery during the index hospitalization, and they tended to have a longer LOS than those who did not have spinal surgery (median: 15 vs. 10 days, p<.001).
Fig. 3.
Length of stay of the index hospitalization for SI by the number of medical comorbidities. More comorbidities were significantly associated with a longer length of stay (p<.001). The solid black lines indicate the median values and the boxes indicate the inter-quartile range (IQR). The whiskers indicate the range of the data within 1.5 x IQR of the upper and lower quartiles.
Table 2.
Associations of baseline characteristics with the LOS for the index hospitalization.
| Variable | Univariable Models |
Multivariable Model 1* |
Multivariable Model 2* |
||||||
|---|---|---|---|---|---|---|---|---|---|
| %Δ† | (95% CI) | p-value | %Δ† | (95% CI) | p-value | %Δ† | (95% CI) | p-value | |
| Male sex | 20.8 | (0.8, 44.7) | .041 | 3.4 | (-13.2, 23.2) | .71 | 3.5 | (-13.2, 23.4) | .70 |
| Age, per 10-year increase | -4.8 | (-10.1, 0.8) | .093 | 0.5 | (-6.0, 7.4) | .89 | -0.1 | (-6.7, 7.0) | .98 |
| White race | -22.2 | (-39.0, -0.9) | .042 | -15.7 | (-32.9, 5.9) | .14 | -14.2 | (-31.8, 7.9) | .19 |
| Insurance | .006 | ||||||||
| Commercial | (ref) | ||||||||
| Medicaid | 47.8 | (12.4, 94.4) | 12.1 | (-14.9, 47.7) | .42 | 26.0 | (-6.4, 69.6) | .13 | |
| Medicare | 8.3 | (-17.6, 42.2) | -7.7 | (-30.1, 21.8) | .57 | -1.1 | (-25.2, 30.7) | .94 | |
| Other | 13.4 | (-24.7, 70.9) | 1.8 | (-31.4, 51.0) | .93 | 6.6 | (-28.3, 58.3) | .75 | |
| SSI | -43.5 | (-53.4, -31.5) | <.001 | -25.4 | (-39.5, -7.9) | .007 | -26.6 | (-41.0, -8.7) | .006 |
| Medical comorbidities | |||||||||
| Cirrhosis | 42.2 | (-4.1, 111.0) | .080 | 1.1 | (-30.8, 47.5) | .96 | |||
| CKD | 56.8 | (23.1, 99.7) | <.001 | 27.7 | (-0.9, 64.4) | .058 | |||
| DM | 16.4 | (-5.1, 42.8) | .14 | 7.8 | (-12.4, 32.6) | .48 | |||
| Endocarditis | 52.8 | (15.5, 102.1) | .003 | 15.4 | (-13.0, 53.1) | .32 | |||
| Chronic SCI/decubitus ulcer | 49.8 | (11.2, 101.9) | .008 | 41.8 | (4.8, 91.7) | .024 | |||
| HIV | 66.5 | (-20.6, 249.4) | .18 | 23.3 | (-38.6, 147.6) | .55 | |||
| Malnutrition | 101.3 | (62.7, 148.9) | <.001 | 64.8 | (31.8, 106.1) | <.001 | |||
| Non-IV drug use | 27.2 | (-16.8, 94.2) | .27 | 18.8 | (-21.0, 78.5) | .41 | |||
| IVDU | 35.1 | (10.2, 65.7) | .004 | 6.8 | (-19.0, 40.8) | .64 | |||
| Number of comorbidities | <.001 | <.001 | |||||||
| 0 | (ref) | ||||||||
| 1 | 49.9 | (21.5, 84.9) | 29.9 | (3.0, 63.7) | |||||
| 2 | 82.8 | (43.2, 133.5) | 54.6 | (18.2, 102.1) | |||||
| 3+ | 194.0 | (122.1, 289.0) | 141.5 | (76.7, 229.9) | |||||
LOS, length of stay; PSL, primary spoken language; SSI, surgical site infection; CKD, chronic kidney disease; DM, diabetes mellitus; SCI, spinal cord injury; HIV, human immunodeficiency virus; IV, intravenous; IVDU, intravenous drug user.
396 patients without any missing characteristics were included in the multivariable models;
Percent difference in geometric mean of LOS or charges per change in variable.
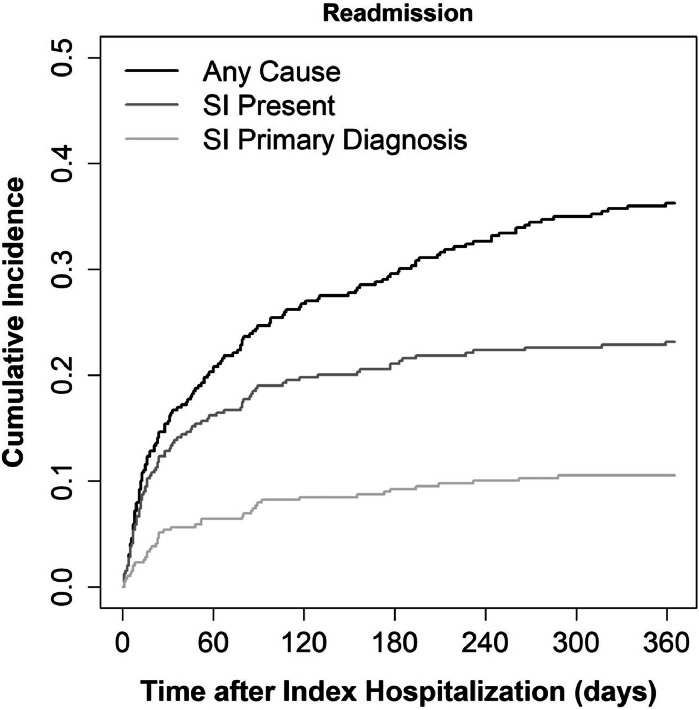
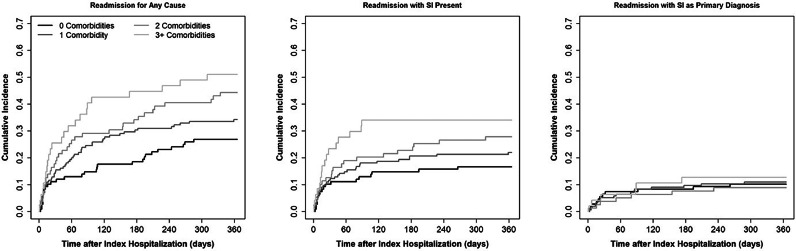
Hospital readmission within 365 days following discharge from the index hospitalization was frequent in this population (Fig. 4). Of the 389 patients who survived the index hospitalization, the rate of readmission for any cause (SI present or absent) was 30% at 180 days (115 events) and 36% at 365 days after index hospitalization (141 events). The rate of readmission with SI present was 21% at 180 days (82 events) and 23% at 365 days (90 events). The rate of readmission with SI as the primary cause was 9% at 180 days (36 events) and 11% at 365 days (41 events).
Fig. 4.
Cumulative incidence of hospital readmission after the index hospitalization for SI. Readmissions were counted for any cause, when SI was present (one of the diagnoses included SI), and when SI was the primary diagnosis.
After adjusting for other factors, those with 3 or more medical comorbidities had a nearly 2-fold higher rate of readmission for any cause than those with no medical comorbidities (HR: 1.95, 95% CI: 1.01-3.79, p=.017 for overall association with comorbidities; rate at 365 days: 51% vs. 27%; Table 3, Fig. 5). Similarly, the rate of readmission when SI was present was approximately twice as high in those with 3 or more medical comorbidities than those with no medical comorbidities (HR: 1.88, 95% CI: 0.82-4.27, p=.077 for overall association with comorbidities; rate at 365 days: 34% vs. 17%; Supplemental Table 2). However, readmission with SI as the primary diagnosis was not significantly associated with the number of medical comorbidities (p=.91, Fig. 5).
Table 3.
Associations of baseline and index hospitalization characteristics with hospital readmissions after the index hospitalization.
| Variable | Univariable Models |
Multivariable Model 1* |
Multivariable Model 2* |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | (95% CI) | p | HR | (95% CI) | p | HR | (95% CI) | p | |
| Male sex | 1.64 | (1.15, 2.33) | .006 | 1.50 | (1.04, 2.17) | .031 | 1.50 | (1.04, 2.18) | .032 |
| Age, per 10-year increase | 0.92 | (0.83, 1.01) | .093 | 0.88 | (0.78, 1.00) | .053 | 0.87 | (0.76, 0.99) | .041 |
| White race | 0.84 | (0.55, 1.30) | .44 | 0.88 | (0.57, 1.37) | .58 | 0.89 | (0.57, 1.40) | .62 |
| Insurance | .35 | .34 | .37 | ||||||
| Commercial | (ref) | (ref) | (ref) | ||||||
| Medicaid | 1.31 | (0.76, 2.24) | 0.90 | (0.50, 1.62) | 1.00 | (0.53, 1.88) | |||
| Medicare | 1.24 | (0.73, 2.13) | 1.12 | (0.62, 2.04) | 1.23 | (0.67, 2.26) | |||
| Other | 0.65 | (0.26, 1.66) | 0.52 | (0.20, 1.35) | 0.58 | (0.22, 1.50) | |||
| Index SI was a SSI | 0.76 | (0.52, 1.12) | .17 | 1.07 | (0.68, 1.67) | .78 | 0.93 | (0.59, 1.48) | .76 |
| Spine surgery during index hospitalization | 0.71 | (0.49, 1.02) | .067 | 0.73 | (0.50, 1.07) | .10 | 0.71 | (0.48, 1.05) | .089 |
| Medical comorbidities | |||||||||
| Cirrhosis | 1.74 | (0.91, 3.31) | .092 | 1.32 | (0.66, 2.63) | .43 | |||
| CKD | 1.19 | (0.76, 1.86) | .45 | 0.98 | (0.59, 1.65) | .95 | |||
| DM | 1.09 | (0.75, 1.59) | .64 | 1.02 | (0.67, 1.55) | .92 | |||
| Endocarditis | 1.44 | (0.88, 2.36) | .15 | 1.20 | (0.69, 2.08) | .51 | |||
| Chronic SCI/decubitus ulcer | 1.34 | (0.82, 2.20) | .25 | 1.03 | (0.58, 1.82) | .91 | |||
| HIV | 2.16 | (0.80, 5.85) | .13 | 1.33 | (0.46, 3.85) | .60 | |||
| Malnutrition | 1.40 | (0.95, 2.06) | .086 | 1.27 | (0.82, 1.96) | .29 | |||
| Non-IV drug use | 1.54 | (0.98, 2.43) | .063 | 1.43 | (0.86, 2.39) | .17 | |||
| IVDU | 1.08 | (0.75, 1.57) | .67 | 0.93 | (0.53, 1.62) | .79 | |||
| Number of comorbidities | .009 | .017 | |||||||
| 0 | (ref) | (ref) | |||||||
| 1 | 1.36 | (0.87, 2.14) | 1.19 | (0.72, 1.97) | |||||
| 2 | 1.85 | (1.13, 3.03) | 1.70 | (0.97, 3.00) | |||||
| 3+ | 2.33 | (1.36, 4.01) | 1.95 | (1.01, 3.79) | |||||
| LOS of index hospitalization, per 2-fold increase | 1.06 | (0.94, 1.20) | .37 | 1.00 | (0.87, 1.14) | .99 | 1.01 | (0.88, 1.15) | .94 |
HR, hazard ratio; CI, confidence interval; SI, spinal infection; SSI, surgical site infection; CKD, chronic kidney disease; DM, diabetes mellitus; SCI, spinal cord injury; HIV, human immunodeficiency virus; IV, intravenous; IVDU, intravenous drug user; LOS, length of stay.
383 patients who survived the index hospitalization and did not have any missing characteristics were included in the multivariable models.
Fig. 5.
Cumulative incidence of hospital readmission after the index hospitalization for any cause (left panel), when SI was present (middle panel) and when SI was the primary diagnosis (right panel), grouped by number of medical comorbidities.
In the multivariable models, none of the individual medical comorbidities were significantly associated with readmission, independent of the other comorbitidies, except endocarditis appeared to be associated with a higher rate of readmission with SI present (HR: 1.96, 95% CI: 1.04, 3.67, p=.036, Supplemental Table 2). There was no significant difference in readmission rates between patients whose index SI was an SSI and patients whose index SI was not an SSI (HR: 1.07, 95% CI: 0.68-1.67, p=.78, Table 3). There was a trend towards those undergoing spinal surgery during the index hospitalization having a lower rate of readmission than those who did not undergo spinal surgery during the index hospitalization (HR: 0.73, 95% CI: 0.50-1.07, p=.10, Table 3). None of the other factors considered were statistically significantly associated with readmission except that male sex was associated with a higher rate of readmission for any cause (HR: 1.50, 95% CI: 1.04-2.17, p=.031, Table 3) and there was a trend towards a lower rate of readmission for any cause among older patients (HR: 0.88 per 10-year increase in age, 95% CI: 0.78, 1.00, p=.053, Table 3).
Discussion
SI is a complex disease process which is associated with a number of comorbidities [7]. Increasing frequency of OSA and malnutrition has been linked to the documented increase in SI in the US since 2003 [1,2]. The effects of the presence of multiple medical comorbidities on the complexity and costs of care of these patients have not been previously explored.
Our medical system consists of a level I trauma center/safety net hospital, a tertiary/quaternary care university hospital, and a community hospital serving a 5-state region which occupies a quarter of the land mass of the US. Our trauma center is a major referral center for spine-related disease, with specific expertise in the treatment of SI and spine trauma. Given the large catchment area and specialized expertise, the patients in our study tended to be medically complex. This is reflected in identification of 403 patients with an initial (index) diagnosis of SI between July 1, 2017 and June 30, 2019. 48.8% of patients had two or more medical comorbidities at the time of the index hospitalization.
An additional comorbidity, not previously well-documented in the literature, was spinal cord injury and associated decubitus ulcer. These patients comprised 10% of our cohort. This may reflect our unique patient population as a large referral center for complex spinal patients but represents an important comorbidity to be considered in SI patients, nonetheless. The remaining comorbidities in our population mirrored those reported in the literature, however, the relationship of comorbidities to age has not been previously described. In our population, IVDU was the primary comorbidity in patients between 18-44 years of age. In patients 65–84 years of age, DM followed by malnutrition and CKD were most common, with very low rates of IVDU in this age group. It is possible that this relationship is a reflection of the safety net status of our hospital system, however, the low rate of OSA and MDSA and the high rate of DM and CKD in the 65-84 year-old age group is striking. SSI was also common, with increasing prevalence with patient age.
Index hospitalization LOS was used as a proxy for complexity of care. The number of medical comorbidities at the time of index hospitalization was positively associated with average LOS, even after accounting for other risk factors and patient characteristics. In our population, CKD, spinal cord injury/decubitus ulcer, and malnutrition were each independently associated with longer LOS. Patients who had spinal surgery to treat their SI during the index hospitalization also tended to have longer LOS than those patients who did not require surgery. Patients with SSI had a 25% shorter LOS on average than non-SSI patients, after accounting for comorbidities and other factors. Costs for SI patients were considerable. The number of comorbidities in a single patient and longer LOS correlated with higher costs of initial care.
Hospital readmission for any cause, both related and unrelated to SI, within the first 365 days after discharge for the index hospitalization was frequent. Higher number of comorbidities was significantly associated with a higher rate of readmission: those with 3 or more medical comorbidities had a nearly 2-fold higher rate of readmission for any cause those those with no medical comorbidities. Readmission did not significantly correlate with age, type of insurance, or surgery during the index hospitalization, though there were non-significant trends toward older age and surgery being associated with lower readmissions. This propensity for readmission following index hospitalization has had limited discussion, often related to outcomes from surgical treatment of SI and not to impact of medical comorbidities.
A strength of our study is the large catchment area and specialized spinal referral center of our hospital system. However, this wide geographic base also posed limitations, namely, a disproportionate number of patients with Medicaid and Medicare insurance and difficulty determining costs of care following the index hospitalization, as outpatient clinic visits not provided within our system are not tracked in our database. Additionally, the extensive geographic referral to our system results in many follow-up clinic appointments occurring out of our network, which are unable to be captured in EDW. Therefore, we are unable to accurately assess compliance of care following hospitalization, such as completion of prescribed antibiotic course. While this limited the evaluation of outpatient visits, the assessment of hospital readmission in this cohort is likely accurate. Internal auditing has shown that the majority of patients initially hospitalized in our system who require readmission are referred back to our system, irrespective of geographic location of the patient. Another limitation of the study is the use of ICD-10-CM and procedure codes to identify our patient cohort. Chart audit of the initial group of patients identified strictly by ICD-10-CM codes revealed inclusion of some patients without SI, though this subset of patients was quite small (Fig. 1). Conversely, it is possible that miscoding may have prevented identification of additional patients with SI. ICD-10-CM and procedure codes did not capture all patients with SSI, which is likely multifactorial, due in part to the complexity of the multiple coding systems and patients having surgery outside of our institution. Coding errors may also have affected our data regarding readmissions, as these were not assessed on the individual chart. It is possible that the diagnosis code may have been missed or misattributed the cause for the event. ICD-10-CM coding also did not allow us to determine and account for the indication for surgery among our surgical patient cohort. This cohort included patients who underwent elective surgery and emergent surgery, the latter of which may be at higher risk for complications. Lastly, LOS may be affected by patient discharge disposition, with an artificially longer LOS for patients requiring additional resources to facilitate discharge. While this likely affected a minority of patients, our EDW data capture was unable to accurately delineate this cohort.
Conclusion
This is one of the largest group of patients with SI identified to date within a single center. Our study shows similar comorbidities of this patient population to those well-documented in the literature, with the addition of spinal cord injury/decubitus ulcer to the list of known comorbidities. Not previously demonstrated in the literature is the relationship of specific comorbidities to patients based on age. IVDU is the chief comorbidity in younger patients (18-44 years-old) and uncommon in older patients (65+ years). DM and CKD tend to predominate in older age groups. The presence of multiple comorbidities correlates with initial LOS and complexity and cost of care. Additionally, this population has a high frequency of readmission in the first year following index hospitalization and discharge.
By understanding the comorbidities that place SI patients at higher risk for complication, extended length of stay, and hospital readmission, clinicians can better identify vulnerable patient populations and potentially mitigate risk. While more work is needed to understand outpatient care and its effect on readmission rates, close outpatient monitoring for patients with multiple comorbidities may help reduce readmission rates and complications. Targeted follow-up care pathways after discharge may be warranted, aligned with healthcare goals associated with accountable care and safe healthcare transitions.
Declaration of competing interest
One or more of the authors declare financial or professional relationships on ICMJE-NASSJ disclosure forms.
Acknowledgments
This research was supported in part by the University of Washington Clinical Learning, Evidence, And Research (CLEAR) Center for Musculoskeletal Disorders, Administrative, Resource and Methodologic Cores and NIAMS/NIH grant P30AR072572. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. DSH reports grant funding from GE Healthcare, Philips Healthcare, and Canon Medical Systems USA outside of the submitted work. The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: CMR: Grants: CLEAR Center (C, Paid directly to institution/employer). DSH: Grants: CLEAR Center (B, Paid directly to institution/employer), GE Healthcare (C, Paid directly to institution/employer), Philips Healthcare (B, Paid directly to institution/employer), Canon Medical Systems USA (B, Paid directly to institution/employer). TP: Nothing to disclose. EH: Nothing to disclose. KS: Research Support (Investigator Salary, Staff/Material)^: Bayor (Amount not disclosed). WC: Grants: CLEAR Center (C, Paid directly to institution/employer). BB: Grants: UW CLEAR Center(U.S. NIH funding) (B, Paid directly to institution/employer).
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2024.100335.
Appendix. Supplementary materials
References
- 1.Blecher R, Yilmaz E, Ishak B, Drazin D, Oskouian RJ, Chapman JR. Recent increase in the rate of spinal infections may be related to growing substance-use disorder in the state of washington: wide population-based analysis of the comprehensive hospital abstract reporting system (CHARS) database. Spine. 2019;44(4):291–297. doi: 10.1097/BRS.0000000000002819. [DOI] [PubMed] [Google Scholar]
- 2.Ronan MV, Herzig SJ. Hospitalizations related to opioid abuse/dependence and associated serious infections increased sharply, 2002-12. Health Affairs. 2016;35(5):832–837. doi: 10.1377/hlthaff.2015.1424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiGiorgio AM, Stein R, Morrow KD, Robichaux JM, Crutcher CL, Tender GC. The increasing frequency of intravenous drug abuse-associated spinal epidural abscesses: a case series. Neurosurg Focus. 2019;46(1):E4. doi: 10.3171/2018.10.FOCUS18449. [DOI] [PubMed] [Google Scholar]
- 4.Huyskens J, Van Goethem J, Faure M, et al. Overview of the complications and sequelae in spinal infections. Neuroimaging Clin N Am. 2015;25(2):309–321. doi: 10.1016/j.nic.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Rigamonti D, Liem L, Sampath P, et al. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999;52(2):189–196. doi: 10.1016/s0090-3019(99)00055-5. [DOI] [PubMed] [Google Scholar]
- 6.Park K-H, Cho OH, Jung M, et al. Clinical characteristics and outcomes of hematogenous vertebral osteomyelitis caused by gram-negative bacteria. J Infect. 2014;69:42–50. doi: 10.1016/j.jinf.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 7.Chang W-S, Ho M-W, Lin P-L, et al. Clinical characteristics, treatments, and outcomes of hematogenous pyogenic vertebral osteomyelitis, 12-year experience from a tertiary hospital in central Taiwan. J Microbiol, Immunol Infect. 2018;51:235–242. doi: 10.1016/j.mii.2017.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Ziu M, Cordell BB, Bartanusz D. Diagnosis and management of primary pyogenic spinal infections in intravenous recreational drug users. Neurosurg Focus. 2014;37(2):1–8. doi: 10.3171/2014.6.FOCUS14148. [DOI] [PubMed] [Google Scholar]
- 9.Bhavan KP, Marschall J, Olsen MA, Fraser VJ, Wright NM, Warren DK. The epidemiology of hematogenous vertebral osteomyelitis: a cohort study in a tertiary care hospital. BMC Infect Dis. 2010;10:158. doi: 10.1016/j.spinee.2013.10.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loibl M, Stoyanov L, Doenitz C, et al. Outcome-related co-factors in 105 cases of vertebral osteomyelitis in a tertiary care hospital. Infection. 2014;42(3):503–510. doi: 10.1007/s15010-013-0582-0. [DOI] [PubMed] [Google Scholar]
- 11.Alton TB, Bransford RJ, Bellabarba C, Lee MJ, Chapman JR. Is there a difference in neurologic outcome in medical versus early operative management of cervical epidural abscesses? Spine J. 2015;15:10–17. doi: 10.1016/j.spinee.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Rossbach BP, Niethammer NR, Paulus AC, et al. Surgical treatment of patients with spondylodiscitis and neurological deficits caused by spinal epidural abscess (SEA) is a predictor of clinical outcome. J Spinal Disord Tech. 2014;27(7):395–400. doi: 10.1097/BSD.0000000000000030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.