Abstract
Lacrimal sac tumors are rare with epithelial tumors being the most common type. Melanoma of the lacrimal sac is an exceptional finding. Few cases have been reported so far in the literature. We report the case of a sixth year old male, with no pathological background, who was referred to the hospital for chronic dacryocystitis resistant to treatment. Computed tomography dacryocystography and magnetic resonance imaging were performed, in favor of a large mass of the lacrimal sac and lacrimal canal suggestive of melanoma. Biopsy confirmed the diagnosis. PET-CT was positive and showed abnormal activity in the lung, liver and bones, in favor of metastasis.
Keywords: Melanoma, Lacrimal sac, Computed tomography dacryocystography, Magnetic resonance imaging
Key points.
Chronic dacrocystitis resisting to treatment should raise the awareness of a possible underlying tumor and MRI must be performed.
A mass in the lacrimal sac with a hypersignal in T1 weighted images, hyposignal in T2 weighted images and enhancement after contrast administration is highly suggestive of a melanoma.
Diagnosis must be confirmed by biopsy.
Alt-text: Unlabelled box
Introduction
Lacrimal sac tumors are rare, and melanoma of the lacrimal sac is even rarer. Its physiopathology is not fully understood. It suggests an abnormal migration of melanocytes during embryological migration of neural crest cells. Diagnosis is often delayed because clinical symptoms are not specific. It is usually discovered upon a chronic dacryocystitis resistant to treatment. Computed tomographic dacryocystography and magnetic resonance imaging are the key imaging modalities to explore lacrymal sac masses, but definitive diagnosis remains histopathological. Prognosis is poor with a low survival rate especially if the disease has already spread by the time of the diagnosis.
Case report
We report the case of a 60-year-old male who was referred to the hospital for chronic dacryocystitis. He complained of epiphora and nasal obstruction for 3 months resisting to treatment. He had taken several courses of antibiotics and topic treatments with no benefit. The patient then developed a left medial canthus region swelling with epistaxis.
Physical examination revealed a firm and painless mass at left internal canthus, with no other systemic abnormal finding.
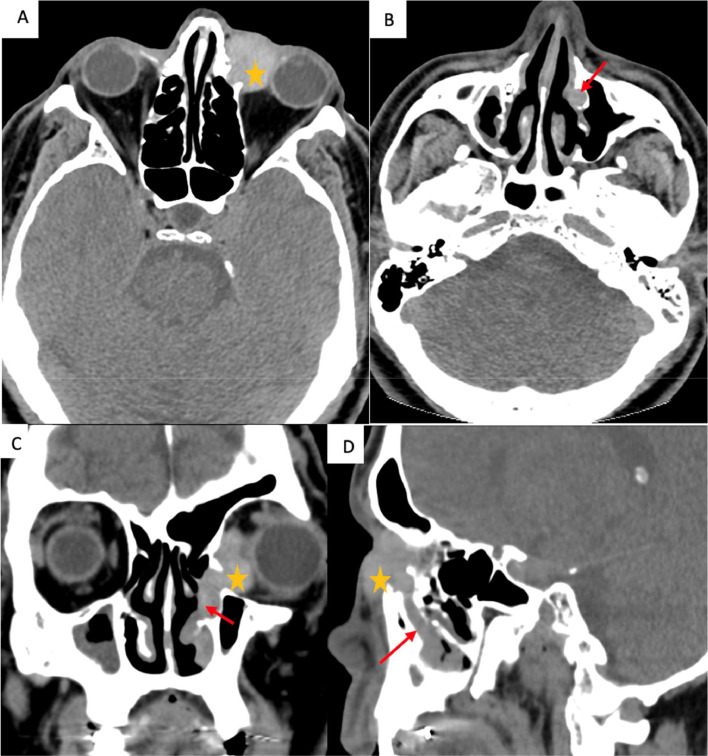
The patient first underwent a computed tomography dacryocystography that revealed a left proximal nasolacrimal duct obstruction caused by a mass at the lacrimal fossa, with absence of contrast in nasolacrimal duct. After intravenous contrast administration, we noted an enhancement of the mass who was well defined with lobulated contours. It was expanding and extending through the nasolacrimal duct, with discrete bony erosion. There was no orbital or sinusal involvement (Figs. 1 and 2).
Fig. 1.
Contrast enhanced CT in the axial (A, B), coronal (C) and sagittal (D) planes, in soft tissue window.
Solid well defined mass ( ) in the fossa of left lacrimal sac, extending through and enlarging the nasolacrimal canal (arrow in B,C and D) with partial invasion of the left nasal fossa.
) in the fossa of left lacrimal sac, extending through and enlarging the nasolacrimal canal (arrow in B,C and D) with partial invasion of the left nasal fossa.
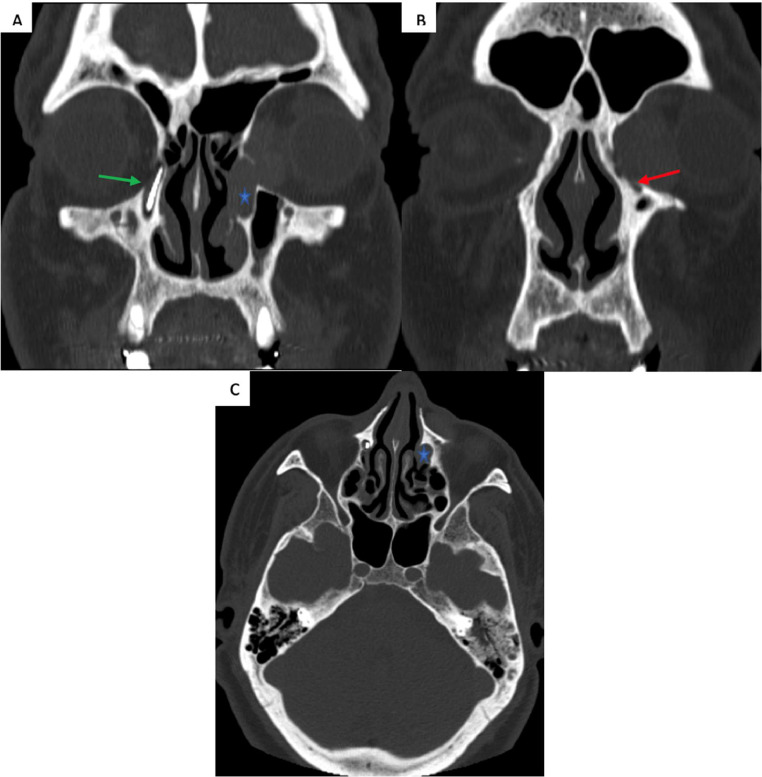
Fig. 2.
Computed tomography dacryocystography in bone window in coronal (A, B) and axial (C) planes, showing a complete obstruction of the left lacrimal pathway ath the level of the mass. Enlarged nasolacrimal canal ( ). The green arrow in A indicated normal right lacrimal pathway. Discrete bone erosion was noted (red arrow in B).
). The green arrow in A indicated normal right lacrimal pathway. Discrete bone erosion was noted (red arrow in B).
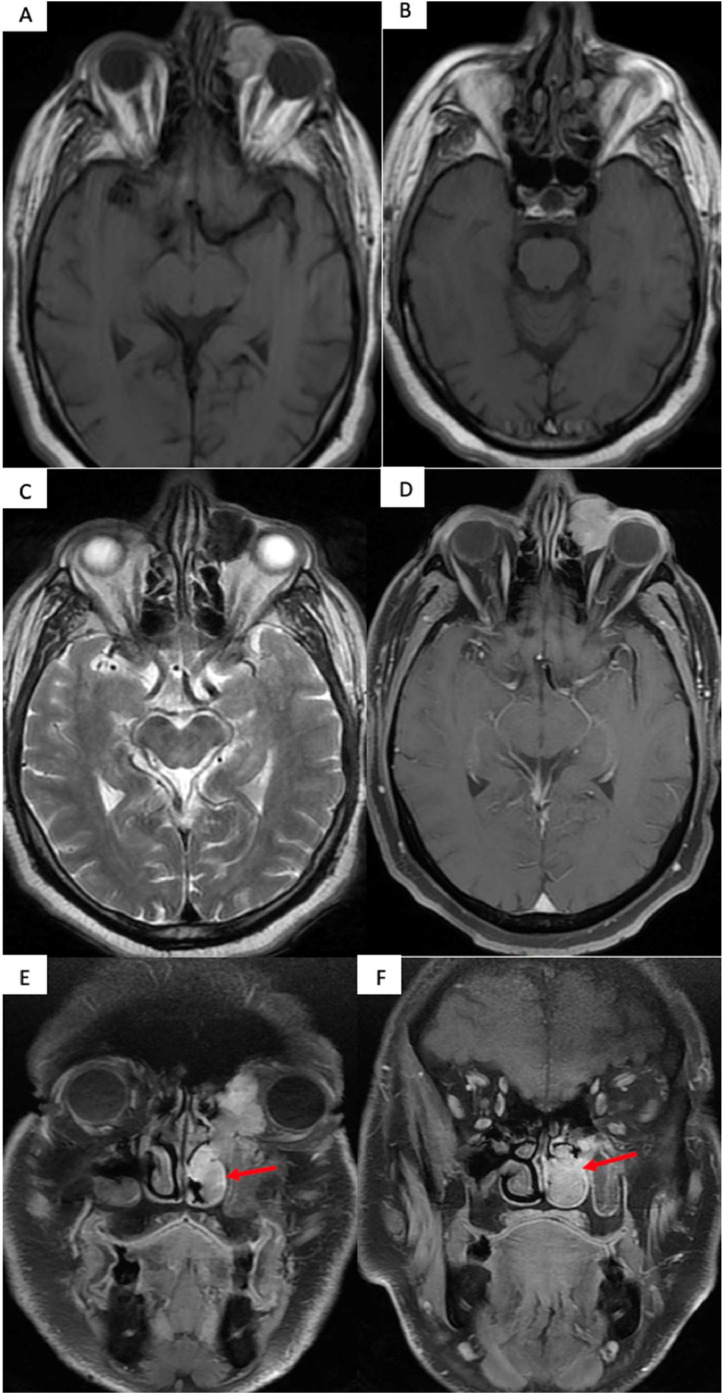
Magnetic resonance imaging revealed that the mass was in hypersignal on T1 weighted images, hyposignal in T2 weighted images, with intense and homogeneous enhancement after contrast administration. There were no enlarged lymph nodes (Fig. 3).
Fig. 3.
Axial T1 weighted images without fat saturation without contrast administration (A and B), axial T2 weighted image without fat saturation (C), T1 weighted images with fat saturation post contrast administration in the axial (D) and coronal planes (E, F).
The mass presents with a typical paramagnetic signal appearing hypersignal on T1 and hypointense on T2. It enhances avidly and homogeneously after contrast administration. Red arrows indicates extension into the left nasal fossa.
Direct biopsy of the lacrimal sac was performed and histopathological examination confirmed malignant melanoma. Positive immunoreactivity for HMB-45 and S-100 on histochemical examination supported the diagnosis.
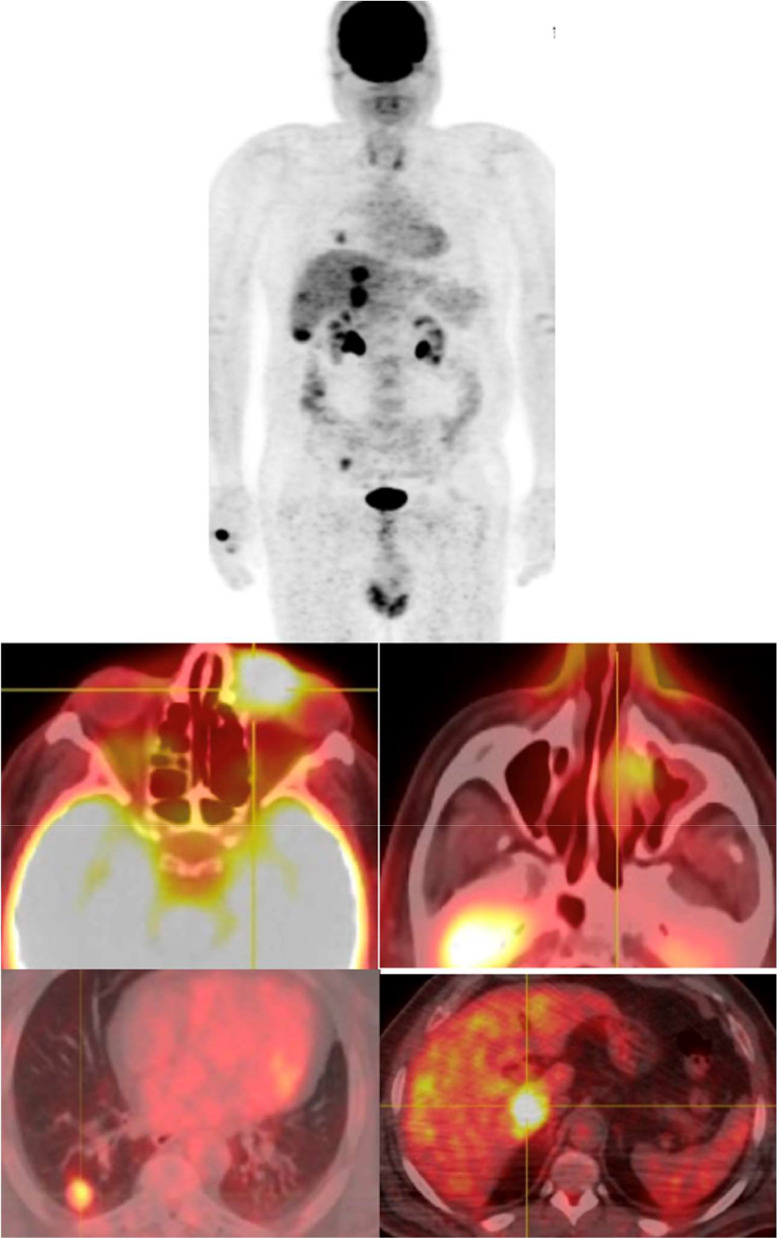
For further work up, the patient underwent a PET CT that showed abnormal activity is the liver, lung and bones, in favor of metastasis (Fig. 4).
Fig. 4.
PET-FDG of the same patient revealing abnormal FDG uptake in the mass, as well as in pulmonary nodules, livers nodules and right iliac bone, in favor of metastases of his melanoma.
Discussion
Malignant lacrimal sac tumors and infrequent, and primary malignant melanoma of the lacrimal sac is even an extremely rare finding, with few cases reported in the literature. Mucosal melanoma of the head and neck encounter approximatively 8% of all melanoma's locations [1,2]. The diagnosis of lacrymal sac melanoma is often delayed and therefore the prognosis poorer.
Clinically, the disease has an insidious onset presenting in most cases as a chronic dacryocystitis [3,4].
Imaging is an effective tool to guide the diagnosis but is not sufficient on its own. Computed tomography dacryocystography is the method of first line to explore nasolacrimal drainage pathway. In early stages, it shows an obstruction of lacrimal pathway by a well-defined mass at the projection of the lacrymal sac extending through the nasolacrimal duct. At first in most cases there is no bone erosion or orbital and sinus involvement. Later on, the tumor margins become irregular and the tumor invades adjacent structures: the orbit, maxillary sinus and nasal fossa. Computed tomography raises the suspiscion of a lacrimal malignany but not the final diagnosis. Magnetic resonance imaging is indicated for further characterization of the mass. In case of melanoma, a typical signal suggesting this tumor may be found, like in our case: a hypersignal on T1 weighted images and a hyposignal on T2 weighted images. This is related to the paramagnetic properties of melanin. This finding is not always found and the tumor may present with an intermediate signal on T1 and T2 weighted images. The higher the melanin content, the more typical the signal is [3,4].
The coronal plane displays the entire lacrymal pathway and shows regional extension of the tumor.
Careful examination of the infra-orbital canal is warranted to assess for perineural spread.
Assessment of pathological lymph nodes is also important as lacrimal tumors can spread via lymphatic vessels, particularly pre auricular, submandibular, and cervical lymph nodes.
Differentials include: dacryocystocele and other malignant tumors of the lacrimal sac. Dacryocystocele appears in computed tomography as a homogeneous well defined mass with fluid attenuation, with a hypersignal on magnetic resonance T2 weighted images. Contrast administration may reveal discrete wall enhancement more pronounced in case of dacryocystitis. In other primary malignant tumors of the lacrimal sac, neither the magnetic resonance signal nor the enhancement can distinguish the histological type. Finally, voluminous tumors may be difficult to distinguish from sinonasal tumors extending to this region [6,7].
Biopsy is necessary to confirm the diagnosis. Histopathological examination with immunoreactivity for HMB-45 and S-100 is in favor for the diagnosis [5,7].
If the disease has not spread yet, surgery is recommended with a wide-field excision of the whole lacrimal system and surrounding tissues, aiming a disease-free surgical margins. Neck dissection is indicated in case of lymphe nodes metastasis. Various combinations of adjuvant radiotherapy, chemotherapy, and immunotherapy are also used. Local recurrence is a major factor in treatment failure [3,6,7].
Poor prognosis is related to hematogenous and lymphatic spread as well as the impossibility of achieving safe surgical margins [3].
Conclusion
Melanoma of the lacrimal sac is an extremely rare tumor and a clinically challenging case. Signal intensity on MRI may be suggestive of the diagnosis but biopsy remains necessary. Prognosis is poor with a risk of metastasis.
Patient consent
The authors have informed patient consent for publication.
I give my consent upon 2 conditions: my identity will be protected at all times, and I have the time to withdraw my consent at any time before the publication of the article by contacting the corresponding author.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Tello JS, Campillo NS, Rodriguez-Peralto JS. Malignant melanoma of the lacrimal sac. Otorhinolaryngol Head Neck Surg. 2004;131(3) doi: 10.1016/j.otohns.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 2.Fishman G, Ophir D. Malignant melanoma of the lacrimal sac: a case study. Am J Otorhinolaryngol. 1999;20(5) doi: 10.3904/kjm.2006.21.4.248. [DOI] [PubMed] [Google Scholar]
- 3.Gleizal A, Kodjikian L, Lebreton F, Beziat JL. Early CT scan for chronical lacrimal symptoms: case report of a malignant melanoma of the lacrimal sac and review of the litterature. J Cranio-maxillofac Surg. 2005;33(3):201–204. doi: 10.1016/j.jcms.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 4.Shao JW, Yin JH, Xiang ST, He Q, Zhou H, Su W, et al. CT and MRI findings in relapsing primary malignant melanoma of the lacrimal sac: a case report and brief review of the literature. BMC Ophthalmology. 2000;20:191. doi: 10.1186/s12886-020-01356-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar VA, Esmaeli B, Gogia AB, Debnam JM, Ginsberg LE. Imaging features of lacrimal sac and nasolacrimal duct tumors. AJNR. 2016;37(11):2134–2137. doi: 10.3174/ajnr.A4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ren M, Zeng JH, Luo QL, Bi F, Chen J. Primary malignant melanoma of lacrimal sac. International J Ophtalmol. 2014;7(6):11069–11070. doi: 10.3980/j.issn.2222-3959.2014.06.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vinciguerra A, Rampi A, Giordano Resti A, Barbieri D, Bussi M, Trimarchi M, et al. Melanoma of the lacrimal drainage system: a systematic review. Clin Rev. 2021;43(7):2240–2252. doi: 10.1002/hed.26705. [DOI] [PubMed] [Google Scholar]