Abstract
Introduction
Textiloma is a rare surgical complication. The location in the renal compartment is exceptional. The diagnosis can be difficult due to its rarity and the absence of clinical signs. The best treatment remains preventive by carefully counting the compresses and the operating fields at the beginning and end of the procedure.
Presentation of case
We present a case report of a 71-year-old female patient with a high blood pressure under treatment. In this history, we noted a right nephrectomy by a lombotomy 6 years ago indicated for a mute kidney on a pyelo-ureteral junction syndrome and a drainage of a suppuration of this renal compartment a year after surgery. The patient was diagnosed with purulent discharge through the lombotomy site associated with lower back pain that had been present for 4 years. The patient then underwent an uro-CT scan which showed an oval formation of the right renal compartment suggestive of a textiloma. An exploratory right lombotomy was performed. And then the wetraction of the compresses followed by washing and closing had been done. The postoperative course was simple.
Discussion
The location in the renal compartment is exceptional. These may include compresses, surgical gauzes, sponges, cotton pads, etc. The inflammation caused by this foreign body will be responsible for an abscess in the event of infection. An evolution towards chronicity follows as long as the foreign body persists. Diagnosis and reoperation are often made during the same hospitalization period. Early imaging will help to make early diagnosis avoiding diagnostic wandering. The diagnosis was made late in our observation. However, the diagnosis can be difficult due to its rarity and the absence of clinical signs.
Conclusion
Textiloma is a rare surgical complication. Renal localization, although rare, is “exceptional” of consequence. The best treatment remains preventive by carefully counting the compresses and the operating fields at the beginning and end of the procedure.
Keywords: Gossypiboma, Retained foreign body, Textiloma, Renal compartment
Highlights
-
•
Renal localization, although rare, is “exceptional” of consequence.
-
•
Questionnaire remains the pillar of diagnosis because the clinical and radiological manifestations are not specific.
-
•
Early imaging will help to make early diagnosis avoiding diagnostic wandering.
-
•
The surgical procedure is, however, very laborious in advanced stages due to fibrosis and adhesions resulting from the inflammatory process
1. Introduction
Textiloma, also called Gossybipoma, is a rare postoperative complication. It comes from the word gossypium meaning cotton in Latin and boma meaning place of hiding in Swahili [1]. The textiloma then corresponds to a foreign body composed of compress(es) or surgical gauze left in the operating site. Its incidence is reported at 1 in 1000–1500 operations [2]. Its site can be ubiquitous with a predominant location in the abdominopelvic region [1,3]. The location in the renal compartment is exceptional. The clinical and radiological manifestations are not specific. The foreign body will trigger an inflammatory reaction with the formation of a perirenal abscess in the event of acute sur infection. Few cases of renal compartment textilloma have been published in the literature. We report a case of textilloma. This article has been reported in line with the SCARE criteria [4].
2. Case presentation
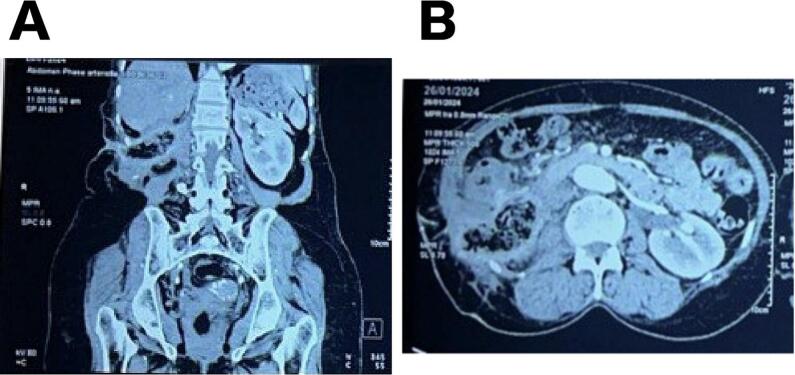
Mrs. A.D is a 71-year-old patient with a high blood pressure under treatment. In this history, we noted a right nephrectomy by a lombotomy 6 years ago indicated for a mute kidney on a pyelo-ureteral junction syndrome in a structure of the place and a drainage of a suppuration of this renal compartment a year after surgery. She was admitted to our facility for purulent discharge through the lombotomy site associated with lower back pain that had been present for 4 years. The examination noted a fairly good general condition, pale mucous membranes, a nephrostomy and right lombotomy scar, a skin break with central ulceration next to the lombotomy scar of approximately 3 to 4 cm leaving pus on the expression (Fig. 1). Uro-CT scan showed an oval formation of the right renal compartment suggestive of a textiloma with an appearance of peritonitis localized subhepatic and infiltration of the muscular plane and the adjacent subcutaneous tissue (Fig. 2a and b). We noted a hypochromic microcytic anemia at 8.9 g/dl and a non-specific biological inflammatory syndrome. Renal assessment was normal. Cytobacteriological examination of the pus was negative. An exploratory right lombotomy was performed. Exploration of the renal compartment showed two almost intact compresses surrounded by gelatinous substances (Figs. 3a and b). Extraction of the compresses was removed with some difficulties because of the presence of an intense fibrotic reaction. There were many fibrosis and adhesions due to the long period of time the foreign body has been left indwelling. Blood loss was minimal and no intraoperative or perioperative complications occurred. The drain was removed on postoperative day 2. The patient received triple antibiotherapy according to the antibiogram. The length of hospital was 16 days. The postoperative course was simple. The patient was seen again at M2 post-operatively with a good clinical outcome (Fig. 4).
Fig. 1.

Preoperative photograph showing skin breakout with central ulceration next to the lombotomy scar.
Fig. 2.
(A) coronal section and (B) axial section of the uro CT scan showing an oval formation of the right renal compartment suggestive of a textiloma.
Fig. 3.
Intraoperative photograph showing (A) the extraction of the first compress and (B) two compresses extracted from the right renal compartment.
Fig. 4.
Postoperative photograph showing a complete healing.
3. Discussion
Textiloma is a complication occurring approximately one to three times in 10,000 surgical procedures [3]. Intraperitoneal and gynecological textilomas are the most frequently reported [1,3]. The location in the renal compartment is exceptional [5]. These may include compresses, surgical gauzes, sponges, cotton pads, etc. The inflammation caused by this foreign body will be responsible for an abscess in the event of infection. An evolution towards chronicity follows as long as the foreign body persists. Diagnosis and reoperation are often made during the same hospitalization period. Early imaging will help to make early diagnosis avoiding diagnostic wandering. The diagnosis was made late in our observation. However, the diagnosis can be difficult due to its rarity and the absence of clinical signs. It can be asymptomatic and discovered incidentally or manifest as hematuria, abdominal pain or inexhaustible suppuration as in our observation. The imaging findings of a retained surgical sponge in an asymptomatic 61-year-old man by a follow-up computed tomography performed 4 months after the emergency surgery was reported. [6]. An insidious progression is possible and the disease is discovered years later accidentally or in a “tumor syndrome” [[3], [4], [5], [6], [7]]. The duration of evolution of the symptoms and the causal intervention are variable. With a review of the literature, José B. reported three cases of textiloma in patients undergoing renal surgery. Two of them had undergone surgery at other hospitals 26 and 4 years earlier. The third patient had undergone transplantation at their hospital and was reoperated 4 months later for a purulent cutaneous fistula caused by the textiloma. [8]. On imaging, radiography of the abdomen without preparation can reveal the appearance of a spongiform mass with the presence of small air bubbles [8,9]. Ultrasound can show a cystic mass often encapsulated with a heterogeneous internal structure, a hypoechoic wall and an intense posterior shadow cone [10,11]. For CT, other authors have reported a case of renal textilloma imitating a renal tumor in the form of a superior polar cyst classified as Bosniak III [12]. Pierluigi Bove reported a case of textiloma mimicking renal cancer recurrence. The CT presentation was suggestive of a tumor recurrence with a hyperdense irregular aspect and a rim of contrast enhancement. This heterogeneous internal aspect may be related to a partial absorption of the hemostatic mesh while the peripheral rim of contrast enhancement could be present in the case of granulomatous reaction. The final pathologic examination revealed fibromuscular tissue with modest chronic flogosis associated with the presence of an amorphous material (hemostatic mesh partially absorbed) [13]. According to our observation, the diagnosis to be made in case of inexhaustible right lumbar suppuration associated with a history of renal surgery on the homologous side is a renal textiloma until proven otherwise. The best treatment is prevention by counting the number of gauze pads before and after surgery must be appropriate. There is a need for gauze to be marked so that it can be immediately identified via X-ray before the patient leaves the operating room or before the incision is closed. Otherwise, surgical treatment is necessary because the inflammatory process will persist if the foreign body remains. The surgical procedure is, however, very laborious in advanced stages due to fibrosis and adhesions resulting from the inflammatory process and due to the long period of time the foreign body has been left indwelling [[5], [6], [7]].
4. Conclusion
Textiloma is a rare surgical complication. Renal localization, although rare, is “exceptional” of consequence. Questionnaire remains the pillar of diagnosis because the clinical and radiological manifestations are not specific. The best treatment remains preventive by carefully counting the compresses and the operating fields at the beginning and end of the procedure.
Ethical approval
Ethical approval for this study (Ethical Committee N° 002015) was provided by the Ethical Committee of Cheikh Anta Diop University, Dakar, Senegal on 11 September 2012.
Funding
The authors declare they have received no funding for the preparation of this document.
Author contribution
These authors participated in the making and correction of this document. All authors agreed with the publication of the document.
Martin Randriantsalama: study concept, data collection, data analysis or interpretation, writing the paper.
Modou Ndiaye: study concept, data collection, data analysis or interpretation, writing the paper
Oumar Gaye: contributor
Alioune Sarr: contributor
Ibrahima Cisse: contributor
Papa Ahmed Fall: contributor
Guarantor
Dr. Randriantsalama Jacques Martin
Research registration number
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of interest statement
The authors declare that they have no conflict of interests.
Contributor Information
Martin Randriantsalama, Email: martinrandr@gmail.com.
Ibrahima Cissé, Email: ibrahima2.cisse@ucad.edu.sn.
Papa Ahmed Fall, Email: papaahmed.fall@ucad.edu.sn.
References
- 1.Hammoud D., Ammouri N., Rouhana G., Saad H., Husseini H., Abou Sleimane C., et al. Radiological aspects of textilomas. J. Radiol. 2001;82:913–916. [PubMed] [Google Scholar]
- 2.Sugano S., Suzuki T., Iinuma M., Mizugami H., Kagesawa M., Ozawa K., et al. Gossypiboma: diagnosis with ultrasonography. J. Clin. Ultrasound. May 1993;21(4):289–292. doi: 10.1002/jcu.1870210415. (PMID: 8478466) [DOI] [PubMed] [Google Scholar]
- 3.Saadi A, Bouzouita A, Kerkeni W, Ayed H, Ben Miled A, Cherif M et al. Une masse abdominale [An abdominal mass]. Rev Med Interne. 2017 May;38(5):347–348. French. doi: 10.1016/j.revmed.2016.02.005. (Epub 2016 May 24. PMID: 27228791). [DOI] [PubMed]
- 4.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zango B., Rizet D., Canabiols L., Laffargue G. Case report: renal textiloma about a case. Afr. J. Urol. 2005;11(1):66–68. [Google Scholar]
- 6.Luis G., María C., Javier G., Isabel G., Raquel G. Gossypiboma following emergency nephrectomy for Wunderlich syndrome. Urology. 2017;99:e9–e10. doi: 10.1016/j.urology.2016.09.028. ISSN 0090-4295, [DOI] [PubMed] [Google Scholar]
- 7.Dimitriadis G., Prousalidis I., Tahmatzopoulos A., Radopoulos D. A rare case of retroperitoneal gossypiboma mimicking renal tumor. European J Radiol. 2007;61:31–32. [Google Scholar]
- 8.Ballesteros J, Alameda F, Parés M. Tres raros casos de textilomas tras cirugía renal. Revisión de la literatura [3 rare cases of textiloma after renal surgery. Review of the literature]. Arch Esp Urol. 2002 Jan-Feb;55(1): 25–9. (Spanish. PMID: 11957747). [PubMed]
- 9.Sheward S, Williams A, Mettler F, Lacey S. CT appearance of a surgically retained towel (gossypiboma). J. Comput. Assist. Tomogr. 1986 Mar-Apr;10(2):343–5. doi: 10.1097/00004728-198603000-00038. (PMID: 3512642). [DOI] [PubMed]
- 10.Liessi G., Semisa M., Sandini F., Roma R., Spaliviero B., Marin G. Retained surgical gauzes: acute and chronic CT and US findings. Eur. J. Radiol. Aug 1989;9(3):182–186. (PMID: 2680489) [PubMed] [Google Scholar]
- 11.Mochizuki T., Takehara Y., Ichijo K., TNishimura T, Takahashi M, Kaneko M. Case report: MR appearance of a retained surgical sponge. Clin. Radiol. 1992;46(1):66–67. doi: 10.1016/S0009-9260(05)80041-8. ISSN 0009-9260, [DOI] [PubMed] [Google Scholar]
- 12.Doh K., Thiam I., Takin R., Bassirou I., Woto G. A case of renal textiloma simulating a tumor of anatomopathological discovery, African. J. Urol. 2017;23:364–367. [Google Scholar]
- 13.Bove Pierluigi, Cindolo Luca. Case study textiloma mimicking renal cancer recurrence. AUA news articles. 29 Jan 2021 [Google Scholar]