Abstract
BACKGROUND
Patients with stroke frequently experience pulmonary dysfunction.
AIM
To explore the effects of information-motivation-behavioral (IMB) skills model-based nursing care on pulmonary function, blood gas indices, complication rates, and quality of life (QoL) in stroke patients with pulmonary dysfunction.
METHODS
We conducted a controlled study involving 120 stroke patients with pulmonary dysfunction. The control group received routine care, whereas the intervention group received IMB-model-based nursing care. Various parameters including pulmonary function, blood gas indices, complication rates, and QoL were assessed before and after the intervention.
RESULTS
Baseline data of the control and intervention groups were comparable. Post-intervention, the IMB model-based care group showed significant improvements in pulmonary function indicators, forced expiratory volume in 1 sec, forced vital capacity, and peak expiratory flow compared with the control group. Blood gas indices, such as arterial oxygen pressure and arterial oxygen saturation, increased significantly, and arterial carbon dioxide partial. pressure decreased significantly in the IMB model-based care group compared with the control group. The intervention group also had a lower complication rate (6.67% vs 23.33%) and higher QoL scores across all domains than the control group.
CONCLUSION
IMB model-based nursing care significantly enhanced pulmonary function, improved blood gas indices, reduced complication rates, and improved the QoL of stroke patients with pulmonary dysfunction. Further research is needed to validate these results and to assess the long-term efficacy and broader applicability of the model.
Keywords: Cerebrovascular accident rehabilitation, Respiratory function tests, Nursing methodology research, Behavioral medicine, Quality of life
Core Tip: Our study examined the impact of information-motivation-behavioral (IMB) model-based nursing on stroke patients with pulmonary dysfunction. The findings revealed that IMB care significantly improved pulmonary function and blood gas indices, reduced complications, and improved quality of life. The results highlight the potential of the IMB model to transform nursing practice and patient outcomes in cerebrovascular accident rehabilitation.
INTRODUCTION
Stroke, classified as either ischemic or hemorrhagic, is a significant global health burden and a leading cause of long-term disability. The global incidence has witnessed an upward trend, largely attributed to evolving lifestyle factors[1,2]. Ischemic strokes caused by cerebral infarction are more prevalent than their hemorrhagic counterparts and have seen considerable advancement in clinical management over the years[3]. Despite this progress, stroke remains an enduring illness, often with permanent neurological deficits and associated complications such as dysphagia, cognitive impairment, and pulmonary dysfunction that contribute to diminished quality of life (QoL)[4]. Regrettably, dysphagia and cognitive impairment have historically dominated the clinical focus and pulmonary dysfunction has been overlooked. Pulmonary dysfunction post-stroke refers to a range of respiratory complications that can arise after a cerebrovascular event. This may encompass decreased lung volumes, impaired gas exchange, reduced respiratory muscle strength, and ineffective airway clearance. These dysfunctions can result from a combination of neurological deficits affecting respiratory control, immobilization, and secondary complications like aspiration due to dysphagia. Studies have shown that stroke patients are at an increased risk of developing respiratory infections, atelectasis, and other complications that can lead to prolonged hospital stays and diminished QoL[5]. The significant repercussions of post-stroke pulmonary dysfunction make early identification and management imperative. However, post-stroke pulmonary dysfunction is not uncommon and poses a significant threat to pulmonary health, precipitating severe complications such as respiratory failure, with far-reaching implications on overall well-being[6]. This highlights the urgent need for a more robust and targeted focus on respiratory function in the clinical management of stroke patients, with the ultimate goal of improving pulmonary rehabilitation and QoL[7-9].
The information-motivation-behavioral skills (IMB) model of guided nursing care is a promising and innovative approach to address this unmet need. This model, characterized by interventions that involve information, motivation, and behavioral skills, allows comprehensive health guidance. The patient-centric approach ensures superior quality of care and has demonstrated promising results despite its relative novelty in clinical practice[9-11]. Although it has been widely adopted for the management of diverse health conditions, most research on the application of the IMB model involves patients with post-stroke cognitive impairment, post-stroke dysphagia, and cerebral hemorrhage. However, the application and effectiveness of this model in the context of stroke-induced pulmonary dysfunction is underreported[9]. This research gap necessitates further exploration and understanding of how the IMB model can guide nursing care and impact pulmonary function rehabilitation in patients with post-stroke pulmonary dysfunction.
Building on this context, our study aimed to contribute to the ongoing research in this field by investigating the effects of IMB-model-based guided nursing care on pulmonary function rehabilitation in stroke patients. We hypothesized that IMB-model-based guided nursing care would significantly improve pulmonary function, enhance blood gas indices, reduce complication rates, and improve QoL in stroke patients with pulmonary dysfunction. Our findings aim not only to fill the existing research gap, but also to provide valuable clinical insights that can improve nursing practice and patient outcomes in this underserved patient population.
MATERIALS AND METHODS
Study design
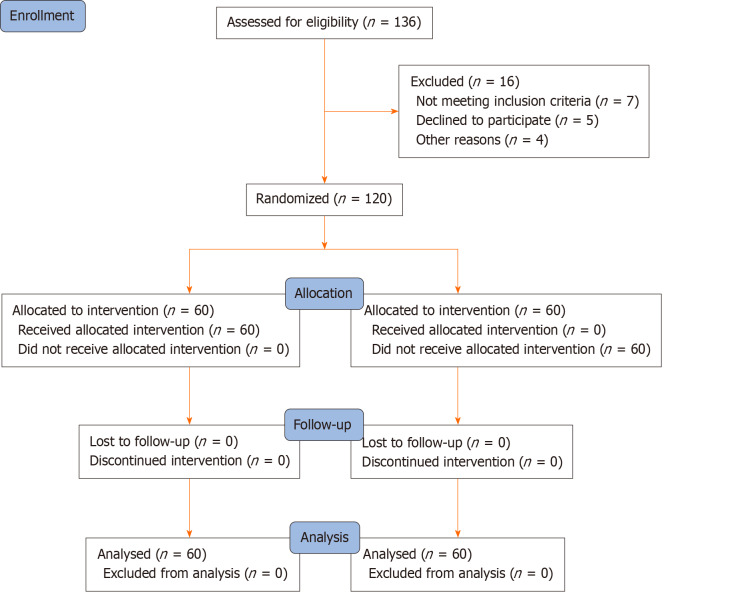
With the approval of the Yancheng First Hospital Affiliated to Nanjing University School of Medicine's Medical Ethics Committee (2021-059), we initiated the process of selecting stroke patients with pulmonary dysfunction treated at the hospital from May 2021 to December 2022 as study participants in this randomized controlled trial. Our inclusion criteria were: (1) Confirmed diagnosis of stroke (including cerebral infarction and cerebral hemorrhage); (2) First episode during the recovery period of stroke; (3) Impaired lung function characterized by notable deviations in parameters such as forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC), especially when considering the FEV1/FVC ratio in relation to established norms from clinical literature on respiratory complications; (4) Clear consciousness; and (5) Voluntary signing of the informed consent form. Potential participants were then assessed for eligibility. Those who met any of the following criteria were excluded: (1) Comorbidity with other severe nervous system disease; (2) Presence of cardiovascular disease; (3) Existing mental disorder; and (4) Inability to communicate normally. Following evaluation and application of the exclusion criteria, 120 eligible patients were randomized a control group and an intervention group, each consisting of 60 patients. Patient selection and allocation are illustrated in Figure 1.
Figure 1.
CONSORT flow diagram of patient selection and allocation.
Nursing intervention
Routine care was administered to the control group and included: (1) Health education and psychological intervention that introduced basic disease knowledge to patients, regularly monitored their emotional state, emphasized the importance of maintaining a positive attitude toward disease improvement, and used verbal soothing techniques to eliminate adverse psychological conditions. Family members were also instructed to encourage the patient to remain optimistic; (2) Dietary guidance by diet plans designed according to the patient's condition, emphasizing dietary restrictions, the importance of nutrition supplementation, and suggesting a light diet; (3) Regular sputum aspiration performed following the doctor's orders was followed by oxygen administration, generally for 2 min; and (4) Turning and. gentle back-tapping by the nursing staff once every 3 h to prevent secondary injuries, each session lasting 5-10 min. This was done 30 min before meals or 2 h after meals. The care was provided throughout the hospital stay.
The intervention group was given an IMB-model-based nursing intervention that included: (1) An informational intervention during which the medical staff engaged in regular communication with patients and their families, emphasizing targeted health education. The educational approach systematically addressed the etiology, clinical manifestations, risks, and preventive measures associated with post-stroke pulmonary dysfunction. Special emphasis was given to precautions during hospitalization and post-discharge. Guidance was also provided on adapting to a suitable lifestyle, dietary habits, the medication regimen, and engaging in respiratory muscle training exercises, including inspiratory muscle training and breathing retraining[5]; (2) A motivational intervention performed by nurses who introduced the prognosis of post-stroke pulmonary dysfunction, encouraged patients to set recovery goals, and provided positive psychological guidance. Rehabilitation case studies were used to boost confidence in recovery. Furthermore, emotional support from family members is also essential; and (3) Behavioral skills intervention that included deep breathing training in which patients were guided to engage in deep breathing exercises 2-3 times daily for 10 min each time. The exercise included slow, deep inhalation, followed by a 2-3 sec breath hold, followed by exhalation. Band-chest abdominal breathing intervention involved fastening strap around the chest and then inhaling deeply while expanding the abdomen, holding the breath for 1-2 sec and then exhaling. The exercise was repeated 3-5 times daily for approximately 3 mi each time. In relaxation training, patients were instructed to relax their muscles consciously to alleviate tension. During the exercise, the room was kept quiet with soft lighting, and light music was played. Patients were in a supine or semi-sitting position, closed their eyes, and consciously and systematically relaxed their muscles. This exercise was conducted twice daily for approximately 10 min each session. For posture control training patients were guided to frequently change their position, with sitting, standing, lying down, elbow stretching, and knee bending, to enhance their motor skills and respiratory function. The exercise was conducted once daily for 30-50 minutes. Complication prevention involved informing patients of potential complications and prevention methods. They were encouraged to exercise more, learn more about health-related knowledge, intensify self-health-condition monitoring, and informing the doctor promptly if any complication was observed.
Outcome measures
The primary observational indicators were: (1) Pulmonary function indicators, including FEV1, FVC, and peak expiratory flow (PEF) measured both before and after nursing care using a SENSOR MEDIC-6200 volumetric scanner; (2) Blood gas analysis by arterial oxygen pressure (PaO2), arterial oxygen saturation (SaO2), and arterial carbon dioxide pressure (PaCO2) measured before and after nursing care using a Medica blood gas analyzer, (3) Complications that occurred during the hospital stay; (4) QoL was assessed by the SF-36 scale before and after nursing care; and (5) Nursing satisfaction was rated by patients on the day of discharge as very satisfied, somewhat satisfied, or not satisfied using a questionnaire.
Statistical analysis
Statistical analysis was performed using IBM SPSS Windows version 26.0. Quantitative data were reported as means ± SD, and between-group comparisons were made using independent sample t-tests. For categorical data, between-group comparisons of proportions between were performed using the χ2 test. Ranked data were analyzed using the Wilcoxon rank-sum test for two independent samples. Statistical significance was set at P < 0.05.
RESULTS
Participant analysis
Our study included 120 stroke patients with pulmonary dysfunction. The patients were divided into observation and control groups of 60 each. The baseline data were similar, with the study groups well matched in age (P = 0.588), body mass index (P = 0.823), stroke duration (P = 0.885), pulmonary dysfunction duration (P = 0.941), and years of education (P = 0.759), ensuring between-group comparability. There were no statistically significant between-group differences of the baseline data (P > 0.05) (Table 1).
Table 1.
Comparison of baseline characteristics between the intervention and control groups
|
Group
|
Number of cases
|
Sex, male/female
|
Age, years
|
Body mass index
|
Stroke duration, days
|
Pulmonary dysfunction duration, days
|
Education years
|
| Intervention | 60 | 32/28 | 68.60 ± 5.77 | 24.89 ± 3.57 | 28.64 ± 3.57 | 25.58 ± 2.23 | 9.32 ± 1.26 |
| Control | 60 | 35/25 | 68.90 ± 5.88 | 25.01 ± 3.65 | 28.70 ± 3.62 | 25.73 ± 2.29 | 9.37 ± 1.30 |
| t value | - | 0.349 | 0.266 | 0.19 | 0.096 | 0.355 | 0.16 |
| P value | - | 0.588 | 0.823 | 0.885 | 0.941 | 0.759 | 0.494 |
Comparison of pulmonary function indicators
Before the nursing intervention, there were no significant differences (P > 0.05) between the observation and control groups in terms of pulmonary function indicators, such as FVC, FEV1, and PEF. The measurements showed post-intervention improvement of FVC, FEV1, and PEF in both groups. However, the improvement in all three parameters was significantly greater in the intervention group than in control group (P < 0.001). This reveals the effectiveness of the nursing intervention, particularly in the intervention group, in enhancing pulmonary function. The results are shown in Table 2.
Table 2.
Comparison of pulmonary function indicators in both groups
|
Group
|
Number of cases
|
FVC pre-intervention, L
|
FVC post-intervention, L
|
FEV1 pre-intervention, L
|
FEV1 post-intervention, L
|
PEF pre-intervention, L/s
|
PEF post-intervention, L/s
|
| Intervention | 60 | 2.38 ± 0.19 | 3.78 ± 0.25 | 1.78 ± 0.16 | 3.26 ± 0.19 | 5.27 ± 0.32 | 7.25 ± 0.25 |
| Control | 60 | 2.42 ± 0.21 | 3.07 ± 0.22 | 1.80 ± 0.19 | 2.28 ± 0.16 | 5.24 ± 0.36 | 5.83 ± 0.23 |
| t value | - | 0.868 | 16.605 | 0.665 | 30.908 | 0.499 | 32.288 |
| P value | - | 0.43 | < 0.001 | 0.553 | < 0.001 | 0.665 | < 0.001 |
FEV1: Forced expiratory volume in 1 second; FVC: Forced vital capacity; PEF: Peak expiratory flow.
Comparison of blood gas analysis indicators between the two groups
Table 3 is a comparative analysis of the blood gas indicators in the observation and control groups, both pre- and post-nursing interventions. It shows improvement of PaO2, PaCO2, and oxygen saturation SaO2 in both groups following the intervention. The intervention group had significant post-intervention increases of PaO2 and SaO2 and a decrease in PaCO2 compared with the control group. These differences were statistically significant, suggesting that the nursing intervention had a more substantial positive effect on the blood gas parameters in the intervention group.
Table 3.
Comparison of blood gas analysis indicators in t groups
|
Group
|
Number of cases
|
PaO2 pre-intervention, mmHg
|
PaO2 post-intervention, mmHg
|
PaCO2 pre-intervention, mmHg
|
PaCO2 post-intervention, mmHg
|
SaO2 pre-intervention, %
|
SaO2 post-intervention, %
|
| Intervention | 60 | 61.32 ± 6.35 | 79.21 ± 5.16 | 73.52 ± 5.46 | 58.14 ± 6.10 | 76.70 ± 7.15 | 93.66 ± 7.71 |
| Control | 60 | 61.24 ± 6.31 | 62.96 ± 5.34 | 73.60 ± 5.54 | 73.07 ± 5.84 | 77.34 ± 7.11 | 86.79 ± 7.62 |
| t value | - | 0.074 | 17.061 | 0.084 | 13.77 | 0.495 | 4.93 |
| P value | - | 0.941 | < 0.001 | 0.933 | < 0.001 | 0.671 | < 0.001 |
PaCO2: Partial pressure of carbon dioxide; PaO2: Arterial oxygen pressure; SaO2: Arterial oxygen saturation.
Comparison of complication rates
The monitored complications included aspiration, pulmonary atelectasis, pulmonary infection, and shoulder-hand syndrome. Following the nursing intervention, the intervention group experienced fewer complications than the control group, with overall incidence rates of 6.67% and 23.33%, respectively. This finding highlights the efficacy of nursing interventions in reducing the occurrence of complications, thereby enhancing patient care and recovery (Table 4).
Table 4.
Comparison of complication incidence rates in both groups
|
Group
|
Cases, n
|
Aspiration
|
Pulmonary atelectasis
|
Pulmonary infection
|
Shoulder-Hand syndrome
|
Total cases
|
Incidence rate, %
|
| Intervention | 60 | 2 | 1 | 1 | 0 | 4 | 6.67 |
| Control | 60 | 3 | 3 | 2 | 6 | 14 | 23.33 |
Comparison of quality of life scores between the two groups
Table 5 shows the quality of life scores across eight different domains of patients in the observation and control groups before and after nursing care. Each domain was considered as pre- and post-nursing care. After the nursing intervention, the intervention group scores in all domains were significantly improved compared with the control group. This suggests the effectiveness of nursing care in enhancing patient QoL in various aspects, further highlighting the benefits of such interventions.
Table 5.
Comparison of quality of life scores before and after nursing care in both groups
|
Group
|
Cases, n
|
Physical function
|
Social function
|
Mental health
|
Physiological role
|
Body pain
|
Energy
|
Emotional role
|
General health status
|
||||||||
|
Before
|
After
|
Before
|
After
|
Before
|
After
|
Before
|
After
|
Before
|
After
|
Before
|
After
|
Before
|
After
|
Before
|
After
|
||
| Intervention | 60 | 55.50 ± 4.15 | 78.05 ± 4.52 | 53.55 ± 4.89 | 77.30 ± 5.11 | 54.25 ± 4.94 | 78.35 ± 5.00 | 56.65 ± 4.10 | 78.76 ± 4.80 | 56.60 ± 4.24 | 80.12 ± 4.60 | 54.30 ± 4.93 | 79.30 ± 5.14 | 55.45 ± 4.95 | 78.80 ± 4.85 | 56.70 ± 4.08 | 79.05 ± 4.70 |
| Control | 60 | 55.46 ± 4.22 | 67.70 ± 4.56 | 53.81 ± 4.95 | 66.82 ± 5.40 | 54.58 ± 5.15 | 67.85 ± 5.00 | 56.90 ± 4.30 | 69.33 ± 4.60 | 56.05 ± 4.32 | 68.30 ± 4.56 | 53.90 ± 4.97 | 66.70 ± 5.25 | 55.60 ± 5.07 | 69.47 ± 5.00 | 56.98 ± 4.18 | 70.05 ± 4.60 |
| t value | 0.049 | 13.061 | 0.27 | 10.6 | 0.332 | 10.994 | 0.308 | 11.68 | 0.648 | 14.21 | 0.402 | 12.511 | 0.151 | 10.8 | 0.331 | 10.09 | |
| P value | 0.961 | 0 | 0.788 | 0 | 0.741 | 0 | 0.759 | 0 | 0.518 | 0 | 0.689 | 0 | 0.881 | 0 | 0.741 | 0 | |
DISCUSSION
This study introduced a novel IMB-model-based nursing intervention tailored specifically for stroke patients with pulmonary dysfunction. It distinguished itself by systematically incorporating informational, motivational, and behavioral strategies. Our findings demonstrate that this comprehensive approach significantly improved pulmonary function and QoL compared to conventional care. Particularly noteworthy is the substantial enhancement of FEV1, FVC, and PEF values in the intervention group, which are crucial metrics for assessing pulmonary efficacy. Additionally, our intervention notably reduced the incidence of common complications such as aspiration and pulmonary atelectasis, further underlining its potential to mitigate secondary health issues frequently encountered in post-stroke management. These results underscore the pivotal role of structured nursing interventions in the rehabilitation of stroke patients and highlight the potential for significant improvement of clinical outcomes, emphasizing the need for their integration into routine clinical practice. This study not only fills a critical gap in stroke rehabilitation but also sets a foundation for future research to explore the longitudinal impact of such interventions on the trajectory of patient recovery.
Stroke is a cerebrovascular event of profound medical significance that occurs with varying degrees of severity in affected individuals. The dysfunctions span limb motor impairment, linguistic incapability, and cognitive deficits, which in turn impose a significant burden on patient QoL and elevate the responsibilities shouldered by their caregivers[12]. The ongoing clinical quest for effective treatment modalities for stroke encompasses two main categories: Conservative management and surgical intervention. The selection of these therapeutic strategies depends on an individual patient-specific clinical profiles. Stroke patients often present with severe and complex disease manifestations, harboring high risks even with immediate medical rescue. Despite expedited treatment, a large proportion of stroke survivors encounter numerous complications, aggravating their condition and undermining their prognosis[13,14].
In this context, high-quality nursing services have been recognized as significant contributors to improved treatment outcomes and improve disease conditions in stroke patients[15]. Therefore, it is imperative that the role of nursing services in treating these patients should be thoroughly emphasized. One commonly associated complication in post-stroke patients is cardiopulmonary functional impairment, with pulmonary dysfunction playing a significant role in overall morbidity[16,17]. This functional limitation often affects physical ability, hinders daily activity, and consequently has a substantial negative impact on their QoL, which increases their psychological distress. For stroke survivors with pulmonary dysfunction, interventions, including respiratory training, aerobic exercise in conjunction with isotonic limb muscle training, abdominal breathing training, and combined respiratory muscle-swallowing training, have been recommended. However, despite their standard operational procedures and long-standing application history, traditional nursing models have increasingly evident shortcomings in the face of evolving patient needs. The main criticisms have focused on the lack of flexibility and specificity, together with an insufficiently humane approach.
The IMB model-based nursing paradigm, characterized by a shift from a disease-centric to a patient-centric approach, marks a transformative phase in the healthcare of stroke patients with pulmonary dysfunction. This innovative model emphasizes the delivery of high-quality nursing services during hospitalization, thereby enhancing the patient’s condition and QoL. The IMB-model-based nursing paradigm involves interventions for patient information processing, motivational aspects, and behavioral skills. Strengthening nurse-patient communication to enhance a patient’s understanding of their condition is a critical part of the informational intervention and aims to promoting their adherence to and outcomes of rehabilitation[18,19]. Motivational interventions primarily focus on providing positive psychological guidance to patients, instilling confidence in their ability to recover, and ensuring psychological wellbeing. Behavioral skill intervention, the crux of this nursing paradigm, involves guiding patients through systematic rehabilitation training and adopting targeted measures to prevent complications. The overarching goal is to gradually improve a patient's condition, ensure their physiological health, and enhance their QoL. Applying the IMB nursing model to patient care can effectively enhance physiological functions, thereby amplifying therapeutic outcomes, improving QoL, and offering advantages and utility over traditional care models.
The key findings of our study highlight the potential benefits of implementing the IMB skills model in nursing care for post-stroke patients with pulmonary dysfunction. The empirical evidence we accumulated points to the effectiveness of the model in fostering marked enhancement of pulmonary function and blood gas analysis indices. These improvements are not merely statistical figures; they represent substantial health advancements for patients who, in the aftermath of stroke, deal with complex and debilitating pulmonary dysfunction. The positive outcomes that we observed can be largely credited to the unique aspects of the IMB model, which includes informational and motivational interventions together with the development of key behavioral skills. The informational aspect of the IMB model empowers patients by providing comprehensive, comprehensible, and actionable health information. This approach aims to equip patients with knowledge about their condition, the importance of adhering to prescribed treatments, and the potential consequences of noncompliance.
Meanwhile, motivational interventions facilitate patients' internalization of the value and critical need to maintain their health and adhere to the prescribed regimen. These motivational interventions, which often involve counseling and emotional support, help patients foster the motivation to make positive health decisions. Behavioral skills interventions, the final component of the IMB model, focus on enhancing patients' capabilities to carry out necessary actions for their health maintenance. This might involve teaching them how to use medical equipment, adhere to medication schedules, or perform physical exercise. Our research further demonstrates that IMB-model-based nursing care significantly reduces the complication rates in patients. This reduction in complications can be seen as a testament to the IMB model's effectiveness as a proactive approach that not only manages the patient’s existing conditions but also pre-empts potential complications. An additional significant finding of our study was the apparent beneficial effect of the IMB model on the QoL of patients. The model's emphasis on the psychological health of patients, its focus on mitigating negative emotions, and its efforts to boost the physical capabilities all contribute to enhancing QoL. This improved QoL is vital because it allows patients to regain a semblance of normalcy in their post-stroke, lives, enabling them to more effectively reintegrate into society.
Despite these promising results, our study had several limitations. The findings were influenced by specific geographic and healthcare contexts that may have affected generalizability. The sample was relatively small and the follow-up duration was short, which means that the long-term effects of the IMB model remain unclear. We also primarily focused on quantitative health outcomes by downplaying the subjective experience of patients with the IMB model. These areas underline the necessity for more comprehensive research to validate our findings and assess the full potential of the IMB model in various contexts.
CONCLUSION
In conclusion, this study suggests that IMB model-based nursing care effectively enhanced pulmonary function, improved blood gas analysis indices, and boosted the QoL of patients with post-stroke pulmonary dysfunction. Our findings highlight the potential of this model for reducing complication rates. However, given the study's inherent limitations, more comprehensive research is warranted to further validate these results and assess the model's long-term efficacy and broader applicability.
ACKNOWLEDGEMENTS
We are grateful to the participants of this study for providing informed consent and enabling this study. We also extend our appreciation to the Yancheng First Hospital Affiliated to Nanjing University School of Medicine for their comprehensive review and endorsement of our study procedures. Their guidance was instrumental in ensuring that the study adhered to the highest ethical standard.
Footnotes
Institutional review board statement: The Ethical Committee of Yancheng First Hospital Affiliated to Nanjing University School of Medicine endorsed all of the study's procedures (2021-059).
Clinical trial registration statement: This RCT was not registered due to urgent clinical needs and regional procedural barriers. Despite this, the trial was rigorously conducted, adhering to ethical and scientific standards with informed consent obtained. Future trials will be registered in advance to ensure transparency.
Informed consent statement: All the patients and their families included in this retrospective analysis provided written informed consent for publication.
Conflict-of-interest statement: The authors declare that they have no competing interests.
CONSORT 2010 statement: The authors have read the CONSORT 2010 Statement, and the manuscript was prepared and revised according to the CONSORT 2010 Statement.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade A
Novelty: Grade A
Creativity or Innovation: Grade A
Scientific Significance: Grade A
P-Reviewer: Glumac S S-Editor: Qu XL L-Editor: Filipodia P-Editor: Zhao YQ
Contributor Information
Xia Peng, Department of Respiratory and Critical Care Medicine, Yancheng First Hospital Affiliated to Nanjing University School of Medicine, Yancheng 224006, Jiangsu Province, China.
Hui-Qin Ni, Department of Neurology, Yancheng First Hospital Affiliated to Nanjing University School of Medicine, Yancheng 224006, Jiangsu Province, China.
Yong-Mei Liu, Department of Nursing, Yancheng First Hospital Affiliated to Nanjing University School of Medicine, Yancheng 224006, Jiangsu Province, China.
Jin-Ling Zhu, Department of Neurology, Yancheng First Hospital Affiliated to Nanjing University School of Medicine, Yancheng 224006, Jiangsu Province, China.
Yu-Ting Bai, Department of Respiratory and Critical Care Medicine, Yancheng First Hospital Affiliated to Nanjing University School of Medicine, Yancheng 224006, Jiangsu Province, China. baiyuting19852023@163.com.
Data sharing statement
The datasets generated and analyzed during this study are not publicly available due to the proprietary data of Yancheng First Hospital Affiliated to Nanjing University School of Medicine. However, they can be made available upon request. Interested parties should contact the corresponding author for access to the data.
References
- 1.Feigin VL, Norrving B, Mensah GA. Global Burden of Stroke. Circ Res. 2017;120:439–448. doi: 10.1161/CIRCRESAHA.116.308413. [DOI] [PubMed] [Google Scholar]
- 2.Hostettler IC, Seiffge DJ, Werring DJ. Intracerebral hemorrhage: an update on diagnosis and treatment. Expert Rev Neurother. 2019;19:679–694. doi: 10.1080/14737175.2019.1623671. [DOI] [PubMed] [Google Scholar]
- 3.Feske SK. Ischemic Stroke. Am J Med. 2021;134:1457–1464. doi: 10.1016/j.amjmed.2021.07.027. [DOI] [PubMed] [Google Scholar]
- 4.Tjahjadi M, König R, Wirtz CR, Woischneck D, Kapapa T. Cerebral vasospasm and health-related quality of life after subarachnoid hemorrhage. World Neurosurg. 2013;80:113–120. doi: 10.1016/j.wneu.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 5.Sutbeyaz ST, Koseoglu F, Inan L, Coskun O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: a randomized controlled trial. Clin Rehabil. 2010;24:240–250. doi: 10.1177/0269215509358932. [DOI] [PubMed] [Google Scholar]
- 6.Battaglini D, Robba C, Lopes da Silva A, Dos Santos Samary C, Leme Silva P, Dal Pizzol F, Pelosi P, Rocco PRM. Brain-heart interaction after acute ischemic stroke. Crit Care. 2020;24:163. doi: 10.1186/s13054-020-02885-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spruit MA. Pulmonary rehabilitation. Eur Respir Rev. 2014;23:55–63. doi: 10.1183/09059180.00008013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liaw MY, Hsu CH, Leong CP, Liao CY, Wang LY, Lu CH, Lin MC. Respiratory muscle training in stroke patients with respiratory muscle weakness, dysphagia, and dysarthria - a prospective randomized trial. Medicine (Baltimore) 2020;99:e19337. doi: 10.1097/MD.0000000000019337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SR, Kim S, Kim HY, Cho KH. Predictive Model of Self-management in Patients With Stroke Based on the Information-Motivation-Behavioral Skills Model. J Cardiovasc Nurs. 2023;38:158–167. doi: 10.1097/JCN.0000000000000883. [DOI] [PubMed] [Google Scholar]
- 10.You H, Wang YY, Zhang C, Walker AN, Ge JJ, Zhao SQ, Peng XQ. Empirical validation of the information-motivation-behavioral skills model of gestational weight management behavior: a framework for intervention. BMC Public Health. 2023;23:130. doi: 10.1186/s12889-023-15067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lim KE, Kim SR, Kim HY, Kim SR, Lee YC. Self-management model based on information-motivation-behavioral skills model in patients with chronic obstructive pulmonary disease. J Adv Nurs. 2022;78:4092–4103. doi: 10.1111/jan.15371. [DOI] [PubMed] [Google Scholar]
- 12.Cai W, Zhang K, Li P, Zhu L, Xu J, Yang B, Hu X, Lu Z, Chen J. Dysfunction of the neurovascular unit in ischemic stroke and neurodegenerative diseases: An aging effect. Ageing Res Rev. 2017;34:77–87. doi: 10.1016/j.arr.2016.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Markus HS, Michel P. Treatment of posterior circulation stroke: Acute management and secondary prevention. Int J Stroke. 2022;17:723–732. doi: 10.1177/17474930221107500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Muresanu DF, Strilciuc S, Stan A. Current Drug Treatment of Acute Ischemic Stroke: Challenges and Opportunities. CNS Drugs. 2019;33:841–847. doi: 10.1007/s40263-019-00663-x. [DOI] [PubMed] [Google Scholar]
- 15.Camicia M, Lutz B, Summers D, Klassman L, Vaughn S. Nursing's Role in Successful Stroke Care Transitions Across the Continuum: From Acute Care Into the Community. Stroke. 2021;52:e794–e805. doi: 10.1161/STROKEAHA.121.033938. [DOI] [PubMed] [Google Scholar]
- 16.Dreyer P, Angel S, Langhorn L, Pedersen BB, Aadal L. Nursing Roles and Functions in the Acute and Subacute Rehabilitation of Patients With Stroke: Going All In for the Patient. J Neurosci Nurs. 2016;48:108–115. doi: 10.1097/JNN.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 17.Aadal L, Angel S, Dreyer P, Langhorn L, Pedersen BB. Nursing roles and functions in the inpatient neurorehabilitation of stroke patients: a literature review. J Neurosci Nurs. 2013;45:158–170. doi: 10.1097/JNN.0b013e31828a3fda. [DOI] [PubMed] [Google Scholar]
- 18.Pitthayapong S, Thiangtam W, Powwattana A, Leelacharas S, Waters CM. A Community Based Program for Family Caregivers for Post Stroke Survivors in Thailand. Asian Nurs Res (Korean Soc Nurs Sci) 2017;11:150–157. doi: 10.1016/j.anr.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 19.Ugur HG, Erci B. The Effect of Home Care for Stroke Patients and Education of Caregivers on the Caregiver Burden and Quality of Life. Acta Clin Croat. 2019;58:321–332. doi: 10.20471/acc.2019.58.02.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during this study are not publicly available due to the proprietary data of Yancheng First Hospital Affiliated to Nanjing University School of Medicine. However, they can be made available upon request. Interested parties should contact the corresponding author for access to the data.