Abstract
Background
Traumatic brain injury (TBI) can be life threatening depending on the severity of the insult to the brain. It can also cause a range of debilitating sequelae which require cognitive, motor, communication, emotional, or behavioral rehabilitation of varying intensity and duration. A number of studies conducted and published in China have suggested that acupuncture may be beneficial in the acute treatment and rehabilitation of TBI.
Objectives
To determine the efficacy and safety of acupuncture in the acute management or rehabilitation (or both) of patients with a TBI, including cognitive, neurological, motor, communication, emotional, or behavioral complications, or a combination of such complications.
Search methods
We searched the Cochrane Injuries Group Specialised Register, Cochrane Central Register of Controlled Trials (The Cochrane Library), MEDLINE, EMBASE, CINAHL, AMED, PsycINFO and others. We also searched the Chinese Acupuncture Studies Register, the Studies Register of the Cochrane Complementary Medicine Field, NCCAM, and NIH Clinical Studies Database. Three major Mainland Chinese academic literature databases (CNKI, VIP and Wang Fang Data) were also searched using keywords in simplified Chinese. We searched all databases through December 2009, and some searches have been updated to October 2012.
Selection criteria
Randomized controlled studies evaluating different variants of acupuncture and involving participants of any age who had suffered a TBI. Included trials compared acupuncture with placebo or sham treatment, or acupuncture plus other treatments compared with the same other treatments. We excluded trials that only compared different variants of acupuncture or compared acupuncture alone against other treatments alone, as they did not yield the net effect of acupuncture.
Data collection and analysis
Two review authors identified potential articles from the literature search and extracted data independently using a data extraction form. We performed methodological assessment of included studies using the Cochrane Collaboration's tool for assessing risk of bias. We were unable to perform quantitative data analysis due to insufficient included studies and available data.
Main results
Four RCTs, including 294 participants, reported outcomes specified by this review. Three investigated electro‐acupuncture for TBI while one investigated acupuncture for acute TBI. The results seem to suggest that acupuncture is efficacious for these indications, however the low methodological quality of these studies renders the results questionable. No adverse effects of acupuncture were reported in any of the studies.
Authors' conclusions
The low methodological quality of the included studies does not allow us to make conclusive judgments on the efficacy and safety of acupuncture in either the acute treatment and/or rehabilitation of TBI. Its beneficial role for these indications remains uncertain. Further research with high quality trials is required.
Keywords: Humans, Acupuncture Therapy, Acupuncture Therapy/methods, Brain Injuries, Brain Injuries/rehabilitation, Brain Injuries/therapy, Electroacupuncture, Electroacupuncture/methods, Glasgow Coma Scale, Randomized Controlled Trials as Topic
Plain language summary
Acupuncture for acute management and rehabilitation of traumatic brain injury
Acupuncture used for the acute treatment, rehabilitation (or both) of traumatic brain injury (TBI) has been studied in China. We conducted a systematic review to evaluate the efficacy and safety of acupuncture for these conditions. Four randomized controlled trials were eligible for inclusion in this review, involving 294 patients. Three investigated electro‐acupuncture for TBI while one investigated acupuncture for acute TBI. The studies were of low methodological quality and were diverse in their objectives, participant characteristics, acupuncture modalities and strategies, and outcome measures. The small number of studies together with their low methodological quality means that they are inadequate to allow any conclusion to be drawn about the efficacy and safety of acupuncture in the treatment of TBI. Further methodologically robust studies are needed to generate evidence‐based conclusions.
Background
Traumatic brain injury (TBI) is defined as a blow to the head, or a penetrating head injury, that disrupts the function of the brain. Not all blows to the head result in a TBI. The severity of a TBI may range from mild (a brief change in mental status or consciousness) to severe (an extended period of unconsciousness or amnesia after the injury) (CDC 2008).
Signs of and symptoms resulting from a TBI depend upon the severity of the injury, the location of the injury and the type of TBI (diffuse or focal). A person with a mild TBI may remain conscious or may experience a loss of consciousness for a few seconds or minutes. Other symptoms of mild TBI include headache, confusion, lightheadedness, dizziness, blurred vision or tired eyes, ringing in the ears, bad taste in the mouth, fatigue or lethargy, a change in sleep patterns, behavioral or mood changes, or trouble with memory, concentration, attention, or thinking. A person with a moderate or severe TBI may show these same symptoms, but may also have a headache that gets worse or does not go away, repeated vomiting or nausea, convulsions or seizures, an inability to awaken from sleep, dilation of one or both pupils of the eyes, slurred speech, weakness or numbness in the extremities, loss of co‐ordination, and increased confusion, restlessness, or agitation (CDC 2008).
Management of TBI can be classified as acute management and rehabilitation. Acute management consists of maintenance of adequate pulmonary gas exchange and brain perfusion to avoid secondary brain damage. This is supplemented by early management of hypoxia, hypercapnia, hypotension, and increased intracranial pressure. Bleeding from injuries is controlled as required and intravascular volume is promptly replaced with crystalloid or blood transfusion to maintain cerebral perfusion. Other complications to monitor for and prevent include hyperthermia, hyponatraemia, hyperglycaemia, and fluid imbalance (Parikh 2007).
Subsequent to acute TBI, patients may develop complications manifesting in different forms of disability. These include cognitive, neurological, motor, emotional, or behavioral problems. Rehabilitation is, therefore, essential and aims to reduce disabilities and enable the patient to achieve the maximum degree of pre‐injury function, within the limits imposed by their residual cognitive, neurological, and motor functions (Chua 2007). TBI rehabilitation may consist of two phases. The inpatient phase may span one to three months, and include the acute neurosurgical and early rehabilitation phase prior to transfer to some form of specialized Traumatic Brain Injury unit. The outpatient or community phase may continue for one to two years or even longer depending on the age of the patient, severity of injury and residual disability (Khan 2003).
Description of the condition
Traumatic brain injuries (TBIs) represent a serious public health problem world wide. According to the National Center for Injury Prevention and Control, which is a part of the US Centers for Disease Control and Prevention, TBI accounts for 50,000 deaths, 235,000 hospitalizations, and 1.1 million emergency department visits annually (Langlois 2006). It has been estimated that in the European Union, TBI accounts for one million hospital admissions per year (Hyder 2007). Recent estimates suggest that there are about 25,000 people with TBI admitted to Australian hospitals annually (Rosso 2007). These figures probably underestimate the true incidence of TBI because of classification and diagnostic errors, as well as under‐reporting of mild injury. Males are around twice as likely as females to experience TBI (Langlois 2006). Combining deaths, hospitalizations, and emergency department visits, children aged 0 to 4 years and adolescents aged 15 to 19 years are more likely to sustain TBI than individuals in other age groups. For hospitalization alone, adults aged over 75 years have a higher incidence of TBI (Langlois 2006). The etiology of TBI is very diverse and includes falls (28%), motor vehicle traffic crashes (20%), being struck by/against something (19%), assault (11%), unknown (9%), other (7%), bicycle (3%), other transport (2%), and suicide attempts (1%) (Langlois 2006). Apart from injuries of domestic origin, blasts are a major contributor to TBI among active duty military personnel in war zones (Scott 2005). After acute treatment, rehabilitation can be required for a number of years. TBI therefore represents a public health concern in terms of loss of, and/or reduction in, workforce economic productivity (or both) and an increase in utilization of healthcare resources in the treatment and rehabilitation of those who survive the injuries.
Description of the intervention
Acupuncture is one of the best known complementary and alternative medicines (CAM). Its use can be traced back more than 2000 years in China (Wu 1996). Acupuncture is commonly used as a routine treatment in China, Japan, Korea, and Taiwan, and has been gaining popularity in the United States and other parts of the western world (Ernst 2001). Acupuncture involves the stimulation of specific points on the skin, the acupoints or meridian points, by the insertion of fine needles. Similar to other forms of Traditional Chinese Medicine (TCM) treatment modalities, the application of acupuncture is based on the principles of TCM in terms of a vital force or energy named 'Qi' which circulates between organs along channels called meridians. 'Qi' energy must flow at the appropriate strength and quality through each of these meridians and organs for health to be maintained. The acupoints are located along these meridians and act as a means of altering the flow of 'Qi' (Kaptchuk 2002).
How the intervention might work
The mechanisms underlying the effects of acupuncture remain poorly defined. Extensive research has shown that acupuncture analgesia may be initiated by stimulation, in the muscles, of high‐threshold small‐diameter nerves. These nerves are able to send messages to the spinal cord and then activate the spinal cord, brain stem (periaqueductal grey area), and hypothalamic (arcuate) neurons, which in turn trigger endogenous opioid mechanisms. The responses include changes in levels of endogenous opioids (e.g. endorphins and enkephalins) or stress‐related hormones (e.g. adrenocorticotropic hormone) in the plasma or corticospinal fluid (Pomeranz 1989).
Studies in animals and humans have demonstrated that acupuncture can cause multiple biological responses, including circulatory and biochemical effects. These responses can occur locally or close to the site of application, or at a distance. They are mediated mainly by sensory neurons to many structures within the central nervous system. This can lead to activation of pathways affecting various physiological systems in the brain as well as in the periphery (Jansen 1989; Johansson 1993; Magnusson 1994; Sun 2001).
Why it is important to do this review
Based on our preliminary search on the use of Traditional Chinese Medicine in TBI, we found that there are more than 30 studies in Chinese databases of the clinical efficacy of acupuncture in the acute management or rehabilitation (or both) of TBI. In order to provide the best available evidence to guide good clinical practice and planning of acute management and rehabilitation for TBI, a systematic analysis of all randomized controlled trials of acupuncture for TBI is needed.
The application of acupuncture in neurological conditions has been reviewed in a number of Cochrane systematic reviews, although these reviews reported that trials of acupuncture efficacy are equivocal or contradictory. These reviews were on topics including idiopathic headache (Melchart 2008), insomnia (Cheuk 2007), Bell's palsy (He 2008), epilepsy (Cheuk 2006), stroke rehabilitation (Wu 2008), and acute stroke (Zhang 2005). Given that TBI also shares a neurological pathophysiology, acupuncture may have a role in TBI treatment or rehabilitation (or both) and is therefore worthy of a systematic review in its own right.
Acupuncture is widely used in China and is increasingly used by people in other countries. The report from the Consensus Development Conference on Acupuncture held at the National Institutes of Health (NIH) in 1997 stated that acupuncture is being "widely" practised "by thousands of physicians, dentists, acupuncturists, and other practitioners" for the relief or prevention of pain, and for various other health conditions. According to the 2002 National Health Interview Survey, which is the largest and most comprehensive survey of complementary and alternative medicines used by American adults to date, an estimated 8.2 million American adults had used acupuncture at some time, and an estimated 2.1 million American adults had used acupuncture in the previous year (NIHCP 1997). A telephone interview‐based study (UMHS 2003) conducted by the University of Michigan Medical School revealed that 80% of TBI patients believed that complementary and alternative medicines, ranging from massage to herbal medicine, were effective. As such, many patients suffering from TBI approach complementary and alternative medicine themselves, in addition to conventional medical treatment or a rehabilitation program.
There is increasing interest in the use of acupuncture as a treatment modality for different neurological disorders (Ernst 2001). A number of Chinese studies have suggested good therapeutic effects of acupuncture on TBI (Ding 2007; Li 2003). We therefore formulated the following research question for which we performed a systematic review to rigorously assess whether acupuncture is efficacious and safe in the acute treatment or rehabilitation (or both) of patients suffering from TBI.
Objectives
To determine the efficacy and safety of acupuncture in the acute management or rehabilitation (or both) of patients with a traumatic brain injury (TBI). This includes cognitive, neurological, motor, emotional, or behavioral complications, or a combination of such complications.
We investigated the following hypotheses.
Acupuncture is efficacious in the treatment of acute TBI.
Acupuncture can enhance the speed and extent of rehabilitation of TBI complications.
Acupuncture can reduce the occurrence and recurrence of TBI complications.
Acupuncture can improve the quality of life of TBI patients.
Acupuncture is safe.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials.
Types of participants
People who have a traumatic brain injury (TBI) ranging from mild to severe (Kay 1993; Rosenthal 1990) who are of any age and of either gender.
Types of interventions
We included trials evaluating all forms of acupuncture therapy, which involves the penetration of the skin with needles, including scalp acupuncture, body acupuncture, auricular acupuncture, tongue acupuncture, injection acupuncture or electro‐acupuncture, or any combination of the above, regardless of frequency of treatment, duration of treatment period and location(s) of stimulation (e.g. scalp, body, tongue, or ear). We excluded other forms of acupuncture therapy which did not involve penetration of the skin with a needle, such as acupressure, laser acupuncture, and percutaneous neuromodulation.
Acupuncture can be given alone or in combination with conventional medical treatment for TBI. The control intervention may be no treatment, placebo acupuncture, sham acupuncture, or conventional medical treatment (which may be baseline treatment) for TBI. We planned to analyse these control groups separately. Placebo acupuncture refers to a needle attached to the skin surface (not penetrating the skin but at the same acupoints) (White 2001). Sham acupuncture refers to a needle placed in an area close to, but not in, acupuncture points (Lund 2006; Streitberger 1998; White 2001) or subliminal skin electro‐stimulation via electrodes attached to the skin (SCSSS 1999).
Acute management involves the stabilization of the patient immediately after the injury; the time frame may be from the onset of injury to one month following injury. Rehabilitation involves the treatment of long‐term impairments and the return of the patient to the community; the time frame may be from one month to two years following injury.
The treatment comparisons investigated in this review are listed below.
Acupuncture alone versus no treatment.
Acupuncture alone versus placebo or sham treatment.
We excluded studies comparing different forms of acupuncture only (different manipulation methods or different acupoints), since these studies cannot yield the net effect of acupuncture and hence cannot demonstrate the efficacy of acupuncture per se.
Types of outcome measures
Primary outcomes
Functional outcome assessed by objective, validated, reliable scales, e.g. Barthel Index (BI), Functional Independence Measurement (FIM) or Fugl‐Meyer assessment (FMA).
Glasgow Outcome Score (GOS).
Morbidity.
Mortality.
Secondary outcomes
Validated quality of life (QOL) measures, e.g. SF‐36 questionnaire.
Adverse effects.
Search methods for identification of studies
We aimed to identify all relevant trials regardless of date, language, or publication status.
Electronic searches
We searched the following electronic databases:
Cochrane Injuries Group Specialised Register (December 2009);
Cochrane Central Register of Controlled Trials 2012, Issue 11 (The Cochrane Library);
MEDLINE (OVID) (1948 to Week 4 Oct 2012);
EMBASE (OVID) (1980 to Week 4 30 Oct 2012);
PsycINFO (ProQuest) (1960 to Week 4 Oct 2012);
CINAHL (EBSCOhost) (1982 to Week 4 Oct 2012);
AMED (OVID) (the Allied and Complementary Medicine Database, 1985 to Week 4 Oct 2012);
TCMLARS Traditional Chinese Medical Literature Analysis and Retrieval System (1984 to Week 4 Oct 2012);
Chinese Clinical Trials Registry (Week 4 Oct 2012);
China Journal Full‐text Database (Week 4 Oct 2012);
China Master Theses Full‐text Database (Week 4 Oct 2012);
China Doctor Dissertation Full‐text Database (Week 4 Oct 2012);
China Proceedings of Conference Database via CNKI (Week 4 Oct 2012);
Index to Taiwan Periodical Literature System (Week 4 Oct 2012);
China Biological Medicine Database (Week 4 Oct 2012);
Chinese Medical Current Contents (Week 4 Oct 2012);
CNKI (China National Knowledge Infrastructure, 1979 to Week 4 Oct 2012);
VIP (Wei Pu Information, 1989 to Week 4 Oct 2012);
Wang Fang Data (1980 to Week 4 Oct 2012);
Cochrane Complementary Medicine Field Specialised Register (Week 4 Oct 2012);
NCCAM (National Center for Complementary and Alternative Medicine, Week 4 Oct 2012);
NIH (National Institute of Health Clinical Trials Database, Week 4 Oct 2012).
The search strategies are reported in Appendix 1 and Appendix 2.
Searching other resources
We searched the reference lists of all relevant papers for further studies.
Data collection and analysis
Lee S and Chu V ran the searches and collated the search results.
Selection of studies
We performed double data extraction. Two review authors (Lee S, Chu V) independently examined titles and abstracts retrieved from the search and selected all potentially relevant studies. We retrieved the full text of these articles, and the same review authors evaluated them independently against the inclusion criteria. Review authors were not blinded to the names of the authors, institutions, or journal of publication of potentially relevant trials. The review authors then extracted data from included trials. We resolved all disagreements by discussion to reach consensus. Where disagreement occurred, the third review author (Wong V) considered the article and contributed to the discussion.
Data extraction and management
The following information was extracted.
Study methods:
design (for example, randomized controlled trial);
randomization method (including sequence generation);
method of allocation concealment;
blinding method;
type of informed consent;
stratification factors.
Participants:
inclusion and exclusion criteria;
number (total and per group);
age and sex distribution;
types of traumatic brain injury (TBI);
Glasgow Coma Scale (GCS) for TBI severity;
post‐TBI complications.
Intervention and control:
type of acupuncture;
details of treatment modalities and strategies including duration of treatment;
type of control(s);
details of control treatment (e.g. in line with Standards for Reporting Trials of Acupuncture (STRICTA) reporting system for acupuncture studies).
Follow‐up data:
duration of follow up;
numbers of treatment withdrawal and reasons for treatment withdrawal;
recurrence of TBI complications after treatment.
Outcome data:
as described in the 'Types of outcome measures' section.
Analysis data:
methods of analysis (intention‐to‐treat or per protocol analysis, or both);
comparability of groups at baseline (yes/no);
statistical methods used.
One author entered the information into Review Manager 5.0 (RevMan 2008) and the other authors checked.
Assessment of risk of bias in included studies
Two authors (Lee S, Chu V) independently assessed the methodological quality of each eligible trial using the Cochrane Collaboration's tool for assessing risk of bias (Higgins 2008). A third author (Wong V) resolved any discrepancies regarding the methodological quality.
We examined the risk of bias based on the methods used to generate the allocation sequence, the concealment of allocation, blinding, incomplete outcome data, selective outcome reporting and other sources of bias. We came to a judgment relating to the risk of bias for each domain as follows: 'Low risk' indicates low risk of bias, 'High risk' indicates high risk of bias, and 'Unclear risk' indicates unclear or unknown risk of bias (Higgins 2008).
Measures of treatment effect
We used odds ratios (OR) with 95% confidence intervals (CI) for binary outcomes. We used weighted mean difference (WMD) with 95% CI for continuous outcomes.
Unit of analysis issues
The patient was the unit of analysis.
Dealing with missing data
We contacted the authors of all the included studies to supply missing data. We assessed missing data and drop‐outs/attrition for each included study, and discussed and assessed the extent to which the results and conclusions of the review could be altered by the missing data. If, for a particular outcome, fewer than 70% of patients allocated to the treatment were reported on at the end of the trial, we did not use that outcome due to potential bias.
Assessment of heterogeneity
We assessed clinical heterogeneity by comparing the distribution of important participant factors between trials (age, gender, specific types of TBI), and trial factors (treatment type, co‐interventions). We planned to assess statistical heterogeneity by examining the I2 statistic (Higgins 2008), a quantity which describes approximately the proportion of variation in point estimates that is due to heterogeneity rather than sampling error. If significant heterogeneity was present (i.e. I2 >= 50% (Higgins 2008)), we planned to investigate trials for possible explanations.
Assessment of reporting biases
We planned to draw funnel plots (estimated differences in treatment effects against their standard error) if sufficient studies were found. Asymmetry could be due to publication bias, but could also be due to a relationship between trial size and effect size. In the event that a relationship was found, we intended to examine the clinical diversity of the studies (Egger 1997).
Data synthesis
Where the interventions were the same or similar enough, we intended to synthesize results in a meta‐analysis where there was no important clinical heterogeneity. If no significant statistical heterogeneity was present, we planned to synthesize the data using a fixed‐effect model, otherwise we would use a random‐effects model in the meta‐analysis.
Subgroup analysis and investigation of heterogeneity
If data permitted, we planned to conduct subgroup analyses for the different interventions' objectives (acupuncture for acute management, acupuncture for rehabilitation), different types of TBI (mild, moderate, severe), and different age groups, to assess whether the treatment effects varied between subgroups.
Sensitivity analysis
We planned to perform sensitivity analyses to assess the impact of study quality, assessing:
all studies;
only those with low risk of bias.
Results
Description of studies
See the 'Characteristics of included studies' and 'Characteristics of excluded studies' tables.
Results of the search
We identified no randomized controlled trials (RCTs) in the western medical literature databases. We retrieved three English language studies; two were single patient case reports (Donnellan 2006; Mukkamala 2003) while the other was a case series of 12 patients (and included a literature search in Chinese medical literature databases) (Li 1993). All three studies were excluded from the review. We retrieved 34 RCTs from the Chinese medical literature databases, of which 30 (Chen 2007; Gao 2007; Gu 2004; Guo 2006; Han 2005; He 2004; Huang 2006; Jia 2001; Li 1993; Li 2003; Li 2005; Liang 2000; Liao 2006; Liu 2006; Lu 2007; Shi 2004; Sun 2005; Tian 2007; Wang 2007; Wei 2001; Wei 2007; Wu 2007; Xiang 2007; Xu 2006; Xu 2007; Yang 2004; Zhang 1996; Zhang 2005; Zhao 2000; Zheng 2005) were excluded from the review. Reasons for exclusion are shown in the 'Characteristics of excluded studies' table.
Included studies
General characteristics
Four studies, including 294 participants (159 in treatment groups and 135 in control groups), fulfilled the inclusion criteria (Cao 2001; Chang 2005; Ding 2002; Song 2007) and employed an objective, validated scale or scoring system for outcome measures. Details of these four trials are shown in the 'Characteristics of included studies' table. All included studies were conducted in China and published in Chinese. We translated these reports ourselves for use in this review. The smallest trial included 50 patients (Chang 2005; Song 2007) and the largest 134 patients (Cao 2001). None of the studies provided information on sample size calculation.
Design
No trial described the method of randomization. All trials used parallel‐group design. All trials had two groups (one acupuncture treatment group and one control group). None of the studies used sham or placebo as control. One trial focused on acupuncture for comatose TBI patients (Song 2007), one studied acupuncture for acute treatment (Ding 2002) and the remaining two trials studied acupuncture for TBI rehabilitation (Cao 2001; Chang 2005).
Participants
Participants were recruited from inpatients in the trial by Ding (Ding 2002) and both inpatient and outpatient clinics in the trial by Cao (Cao 2001). The remaining two trials did not give recruitment information (Chang 2005; Song 2007). The subjects' age ranged from 3 to 71 years. None of the studies reported whether their protocol was reviewed by an institutional review board or whether adequate informed consent was obtained from the participants. Two of the four studies (Ding 2002; Song 2007) included patients with acute severe TBI and a Glasgow Coma Score (GCS) below 8. One trial (Ding 2002) enrolled patients after stabilization, with CT confirmation and a baseline phase period, while the other study (Song 2007) admitted comatose patients with coma status continuing over 7 to 10 days with a further 3 to 10 days comatose after medical stabilization. Neither study mentioned the etiology of the patients' TBI. One study (Cao 2001) defined entry criteria as CT confirmed TBI, with the course of the disease persisting for 6 hours to 17 months, but did not define the TBI etiology. One study included patients with TBI confirmed on CT or MRI (Chang 2005). This is the only study that reported the etiology of the patients' TBI (Chang 2005). Three trials (Chang 2005; Ding 2002; Song 2007) reported that there were no statistical differences in the baseline scores between the groups. The remaining study did not specify comparability of the baseline characteristics (Cao 2001).
Interventions
All four studies assessed acupuncture in addition to the same treatment modality/modalities used in the comparator arm:
electro‐acupuncture plus hyperbaric oxygen and rehabilitation training versus hyperbaric oxygen and rehabilitation training (Cao 2001);
needle acupuncture plus conventional medical intervention versus conventional medical intervention alone (Ding 2002);
electro‐acupuncture plus conventional medical intervention versus medical intervention alone (Song 2007); and
electro‐acupuncture plus rehabilitation training versus rehabilitation training alone (Chang 2005).
In one study (Ding 2002), acupuncture treatments were given uniformly to all participants in the treatment group. In the remaining three studies (Cao 2001; Chang 2005; Song 2007), acupuncture treatments were semi‐standardized (either all patients were treated at some basic points and additional individualized points, or there were different predefined needling schemes depending on patterns of symptoms). Only one trial (Ding 2002) reported the frequency and duration of needling, which was once daily for ten days for the first course and once daily for fifteen days for the second course. The authors, however, did not indicate any interval between the first and the second course or the total number of courses administered before assessment. All studies reported that needles were left in place for 30 minutes for body acupuncture. Two trials reported scalp acupuncture needles left in place for 6 to 8 hours (Cao 2001; Song 2007). None of the studies reported the qualification or clinical experience of the acupuncturists. The treatment modalities and strategies of acupuncture needling used in each study varied (see 'Characteristics of included studies').
Outcomes
Each of the four trials used some form of objective instrument to measure outcomes: Modified Barthel Index (Chang 2005), Fugl‐Meyer Assessment (Chang 2005), Barthel Index (Cao 2001), Glasgow Coma Score (Ding 2002), Glasgow Outcome Score (Ding 2002; Song 2007), grading of muscle strength (Cao 2001) and a scoring table for measuring recovery of motor function and speech function (Ding 2002). Two of the four studies followed up patients after the treatment period, at 1 month (Chang 2005; Song 2007) and 3 months (Chang 2005). None of the studies reported whether the trial investigators and the outcome assessors were the same people. Bias may potentially arise when trial investigators also assess the outcome measures of participants.
Excluded studies
32 studies were excluded as they did not fulfill the inclusion criteria for various reasons (See 'Characteristics of excluded studies').
Risk of bias in included studies
The trials did not provide an adequate description of the methods used for generating the allocation sequence, but all were described as randomized. We contacted the Journal to ask the authors, none of them replied as of 13 Oct 2010. We considered all included studies carried a high risk of bias (Figure 1; Figure 2).
1.
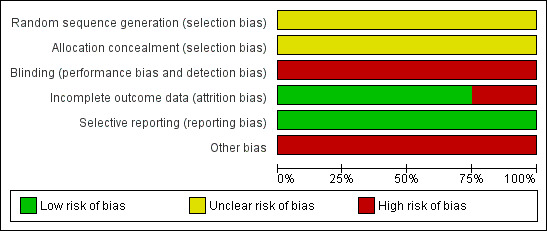
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies. Please note that there are four studies included in this review.
2.
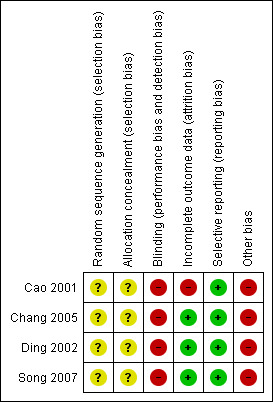
Risk of bias summary: review authors' judgements about each risk of bias item for each included study. Please note that there are four studies included in this review.
Allocation
Randomization procedures were not described in any of the studies. Therefore, sequence generation and allocation concealment were rated as unclear for all studies.
Blinding
No information on blinding was available in any of the included trials. Since none of the trials involved placebo or sham acupuncture, it is highly likely that the treating physicians and patients were not blinded and therefore all studies were rated as non‐blind.
Incomplete outcome data
One study (Cao 2001) reported that 67 participants were recruited in each group but outcome data were only available for 61 participants in each group. The reasons for dropout of the 12 participants were not specified. None of the remaining studies had any losses to follow up, or reported any violation of allocated treatment.
Selective reporting
We were unable to find the protocol for any of the studies, and were therefore unable to assess reporting bias.
Other potential sources of bias
In three trials (Cao 2001; Chang 2005; Song 2007) the acupuncture treatments varied among different participants and were not uniform or standardized, and this might introduce bias. In one study (Cao 2001), it appeared that the control group had more patients with good upper limb muscle power (grade IV to VI) at baseline compared to the treatment group, casting doubts on the comparability of the treatment groups at baseline which might introduce bias. This trial categorized the Barthel Index to 3 categories. The rationale behind and appropriateness of categorizing this continuous variable was unclear and might introduce bias. In another study (Ding 2002), the validity of the motor and speech function scores were questionable and might introduce bias. In 2 studies (Chang 2005; Song 2007), outcome was assessed after 1 month of study treatments. Additional treatments that patients received between study treatment completion and outcome assessments were not mentioned, but these might contribute to the effects observed at assessments and cause bias. In addition, none of the trials employed placebo or sham control, which might also cause bias with placebo effect.
Effects of interventions
Acupuncture plus other treatment versus same other treatment
Primary Outcomes:
Post‐treatment Glascow Coma Score
One study (Ding 2002) compared needle acupuncture plus conventional medical intervention with conventional medical intervention alone and reported this outcome and found that people in the treatment group had significantly higher Glascow Coma Score compared to the control group (MD 2.00, 95% CI 0.27 to 3.73, P=0.02) (Analysis 1.1).
1.1. Analysis.
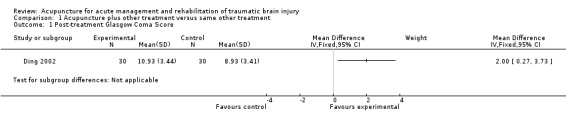
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 1 Post‐treatment Glasgow Coma Score.
Post‐treatment Glascow Outcome Score
The same study (Ding 2002) also reported significantly better Glascow Outcome Score in the treatment group compared to the control group (MD 1.00, 95% CI 0.60 to 1.40, P<0.00001) (Analysis 1.2).
1.2. Analysis.
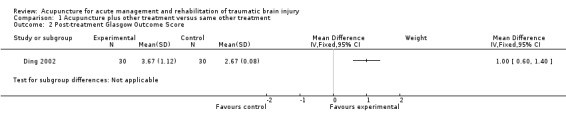
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 2 Post‐treatment Glasgow Outcome Score.
Frequency of normal post‐treatment Glasgow Outcome Score
Another study (Song 2007) compared electro‐acupuncture plus conventional medical intervention with conventional medical intervention alone and reported that the number of subjects with normal Glascow Outcome Score was significantly higher in the treatment group compared to the control group (OR 3.50, 95% CI 1.07 to 11.48, P=0.04) (Analysis 1.3).
1.3. Analysis.
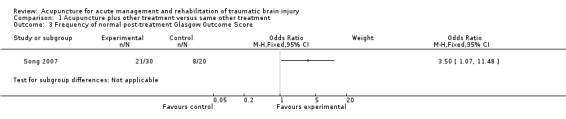
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 3 Frequency of normal post‐treatment Glasgow Outcome Score.
Frequency of post‐treatment Barthel Index above 60
One study (Cao 2001) compared electro‐acupuncture plus hyperbaric oxygen and rehabilitation training with hyperbaric oxygen and rehabilitation training and reported the post‐treatment Barthel Index. The study categorized Barthel Index into 3 groups: <=40, 40‐60, and >60. The treatment group had significantly more subjects achieving Barthel Index above 60 compared to the control group (OR 2.91, 95% CI 1.36 to 6.21, P=0.006) (Analysis 1.4).
1.4. Analysis.
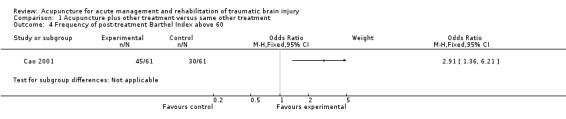
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 4 Frequency of post‐treatment Barthel Index above 60.
Frequency of post‐treatment Barthel Index above 40
In the same study (Cao 2001), however, the number of patients with Barthel Index above 40 was not significantly higher in the treatment group (Analysis 1.5).
1.5. Analysis.
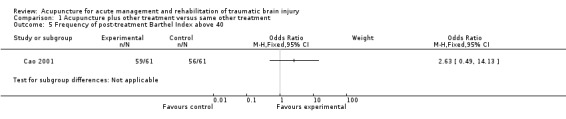
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 5 Frequency of post‐treatment Barthel Index above 40.
Post‐treatment Modified Barthel Index
One study (Chang 2005) compared electro‐acupuncture plus rehabilitation training with rehabilitation training alone and reported the Modified Barthel index at 1 and 3 months post‐treatment and found that the treatment group had a significantly higher score at 1 month (MD 11.24, 95% CI 8.52 to 13.96, P<0.00001) but a lower score at 3 months (MD ‐26.21, 95% CI ‐31.54 to ‐20.88, P<0.00001) post‐treatment (Analysis 1.6).
1.6. Analysis.
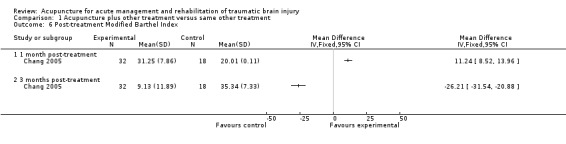
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 6 Post‐treatment Modified Barthel Index.
Post‐treatment Fugl‐Meyer assessment
The same study (Chang 2005) also reported post‐treatment Fugl‐Meyer assessment and found that the treatment group had a significantly higher score at 1 month (MD 11.98, 95% CI 7.54 to 16.42, P<0.00001) and 3 months (MD 52.32, 95% CI 47.7 to 56.94, P<0.00001) post‐treatment (Analysis 1.7).
1.7. Analysis.
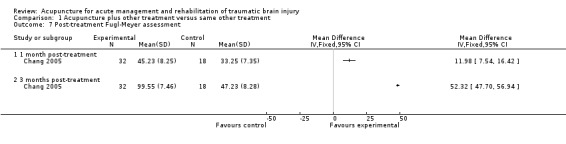
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 7 Post‐treatment Fugl‐Meyer assessment.
Mortality
One study (Song 2007) reported mortality in the treatment and the control groups and there was no significant difference (Analysis 1.8).
1.8. Analysis.
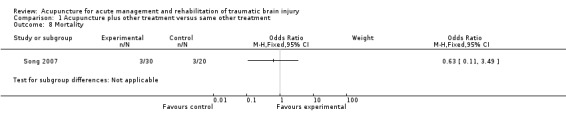
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 8 Mortality.
Secondary outcomes:
None of the included trials reported quality of life assessments.
Adverse effects
No adverse effects of acupuncture were reported by any of the included studies.
Additional outcomes:
Post‐treatment Speech Function Score
The study by Ding (Ding 2002) reported this outcome and found that the treatment group had significantly higher post‐treatment Speech Function Score compared to the control group (MD 1.06, 95% CI 0.49 to 1.63, P=0.0002) (Analysis 1.9).
1.9. Analysis.
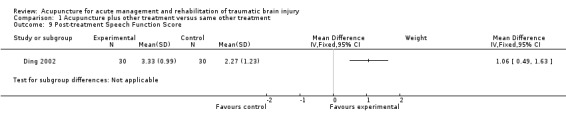
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 9 Post‐treatment Speech Function Score.
Post‐treatment Motor Function Score
The same study (Ding 2002) also reported significantly higher post‐treatment Motor Function Score in the treatment group compared to the control group (MD 1.43, 95% CI 0.83 to 2.03, P=0.0002) (Analysis 1.10).
1.10. Analysis.
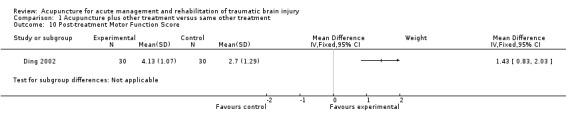
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 10 Post‐treatment Motor Function Score.
Post‐treatment muscle strength grade IV to VI
The study by Cao (Cao 2001) also reported the muscle strength after treatment and categorized it to 2 groups: grade I to III, and grade IV to VI. The number of patients achieving muscle strength grade IV to VI was significantly higher in the treatment group compared to the control group, in both upper limbs (OR 4.65, 95% CI 2.10 to 10.29, P=0.0001) and lower limbs (OR 4.67, 95% CI 1.82 to 11.98, P=0.001) (Analysis 1.11).
1.11. Analysis.
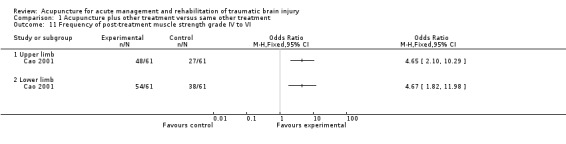
Comparison 1 Acupuncture plus other treatment versus same other treatment, Outcome 11 Frequency of post‐treatment muscle strength grade IV to VI.
Assessment of heterogeneity
All included trials were heterogeneous with respect to characteristics of participants, interventions, co‐interventions, comparators, duration of treatment, and outcome measures. Since no common outcome was available, meta‐analysis and statistical test of heterogeneity was not performed.
Publication bias
We did not produce a funnel plot to check for publication bias because of the limited number of trials for each outcome.
Subgroup analysis
Since none of the trials contained stratified data and individual raw data were not available (although requests were made to the authors of all the included studies), we could not perform subgroup analyses to assess the impact of acupuncture on different types of TBI or in different age groups.
Sensitivity analysis
Since all studies had high risk of bias, we did not perform a sensitivity analysis.
Discussion
Summary of main results
Four randomized controlled trials with a total of 294 participants, comparing needle acupuncture or electro‐acupuncture plus additional therapy with the same additional therapy for traumatic brain injury (TBI), met the inclusion criteria for this review. All 4 RCTs were considered to carry a high risk of bias and therefore no firm conclusion can be drawn. They all used different outcome measures and therefore the results could not be combined in meta‐analysis. After acute TBI, acupuncture might improve overall functional outcome as measured by the Glasgow Coma Score (Ding 2002) and Glasgow Outcome Score (Ding 2002; Song 2007), and motor and speech functions (Ding 2002). In the rehabilitation phase after TBI, acupuncture might improve overall functional outcome as measured by the Barthel Index (Cao 2001) and Modified Barthel Index (Chang 2005), and motor function as measured by the Fugl‐Meyer Assessment (Chang 2005) and muscle strength grading (Cao 2001).
Overall completeness and applicability of evidence
This review suggests that the existing evidence on effectiveness of acupuncture for treatment of TBI, whether in the acute phase or the rehabilitation phase, is far from complete, since there are only a limited number of randomized controlled trials with a small number of patients. The generalizability of the findings is limited.
Since the trials were all heterogeneous with respect to the characteristics of participants (different age groups with variable diagnostic criteria, and phase and severity of TBI), acupuncture methods (needle acupuncture or electroacupuncture, different acupoints in different parts of the body), duration of treatment, co‐interventions (different types of additional therapies), and outcome measures (variable scores), none of the outcomes could be combined in meta‐analysis and no robust conclusion could be drawn. The acupuncture treatments used in the included studies were all different, and were combined with different additional treatments and therefore we were unable to conclude which regimen of acupuncture treatment is effective or whether it works synergistically with the combined treatments.
Although acupuncture appeared to produce favorable results in most outcomes reported in the included trials, some results were not entirely consistent. For example, scores of the Modified Barthel Index were significantly worse in the treatment group compared to the control group at 3 months post‐treatment and such results were unexplained. In addition, there was no significant difference in mortality or the number of patients with Barthel Index above 40 whether the patients received acupuncture or not. On the other hand, none of the trials reported quality of life of the participants, which is an important outcome for this group of neurologically impaired or disabled individuals.
Furthermore, the included RCTs were of short duration and short follow‐up. Although short‐term outcome of acupuncture seems favorable, it remains uncertain whether the effect could be maintained in the long‐term with or without continuous acupuncture treatment.
Although no adverse effects were reported in the trial, we were not entirely confident about the safety of acupuncture as rare adverse effects might have escaped detection due to insufficient statistical power resulting from the small sample sizes.
Quality of the evidence
Overall the evidence supporting any form of acupuncture for treatment of TBI, whether in the acute phase or rehabilitation phase, is weak, as all included trials were assessed to carry a high risk of bias. All trials did not report randomization sequence generation and allocation concealment, and none of the trials attempted to blind the participants or physicians or study personnel. None of the trials employed a placebo or sham control group to minimize the placebo effect.
Potential biases in the review process
The process of searching for studies was thorough. We strictly followed the review protocol in the process of study selection, data extraction, and analysis. However, the trial reports were brief and some important information was unclear or missing and we were unable to get any response to our queries from the trial investigators. This may result in bias in the review.
Agreements and disagreements with other studies or reviews
As far as we are aware, this is the only systematic review on acupuncture for traumatic brain injury.
Authors' conclusions
Implications for practice.
There are no high quality randomized clinical studies supporting acupuncture for treatment of TBI. The current evidence in this review fails to provide solid grounds on which to base conclusions about the efficacy and safety of acupuncture in the acute treatment and rehabilitation of TBI. The current evidence is still far from sufficient to support recommendations for acupuncture as a standard procedure for TBI in clinical practice, although it may be used in experimental investigations. The potential side effects of acupuncture in the context of TBI treatment and rehabilitation remain unclear as these were not reported in any of the clinical trials reviewed. The sustainability of the effects of acupuncture in the long‐term during and after TBI rehabilitation is also unclear as this was rarely investigated.
Implications for research.
Future research may evaluate acupuncture for different TBI sequelae (e.g. headache, seizures, aphasia, facial paralysis, and hemiplegia). There are only a few RCTs investigating its application in each of these complications. Furthermore, the number of RCTs of good methodological quality is limited. Therefore, there is a need for more high quality RCTs to be conducted which investigate the potential effect of acupuncture when used for each of these complications, with the aim of generating evidence to either support or refute its application in these clinical contexts. In particular, more attention and effort should be dedicated to improving the methodological quality of trials to enhance internal validity. For example, there should be unified inclusion criteria, sample size determination to ensure the study is sufficiently powered, truly randomized methods of treatment allocation, adequate concealment of allocation, blinding of investigators, participants and outcome assessors to minimize performance and assessment bias, and use of widely recognized and commonly adopted standard validated outcome measures (e.g. Glasgow Coma Score, Glasgow Outcome Score, Barthel Index) to ensure validity, reliability and comparability, report any losses to follow up with reasons, conduct intention‐to‐treat analysis, and present results clearly in sufficient detail. Trials should include long‐term follow up at specific time points, especially for rehabilitation studies, to determine long‐term effects (e.g. survival, disability, and quality of life). Furthermore, it is unclear which treatment modalities and strategies (e.g. conventional needling, needling with electro‐pulsation, site(s) of needling, the combination of acupoints to be stimulated, the frequency and duration of needling) are efficacious for each of the TBI complications. To reduce heterogeneity, trials may consider focusing on a more restricted and homogeneous subset of TBI patients and evaluating a single uniform acupuncture protocol. When reporting acupuncture studies, it is important to adhere to widely accepted standards, e.g., the STRICTA criteria, in order to facilitate interpretation of the trial report and comparison between acupuncture studies. The STRICTA criteria stipulated that acupuncture trials should adequately report the following: acupuncture rationale, details of needling, treatment regimen, other components of treatment, practitioner background, and control or comparator interventions (MacPherson 2010).
What's new
| Date | Event | Description |
|---|---|---|
| 30 October 2012 | New search has been performed | The search has been updated to 30 October 2012. No new studies were identified. The results and conclusions remain the same. |
| 30 October 2012 | New citation required but conclusions have not changed | The search has been updated to 30 October 2012. No new studies were identified. The results and conclusions remain the same. |
Acknowledgements
We are grateful to the staff of the Department of Paediatric and Adolescent Medicine, the University of Hong Kong, for their help in analyzing the results of this review.
Appendices
Appendix 1. Search strategies
MEDLINE
1. exp acupuncture analgesia/ 2. exp acupuncture, ear/ 3. exp electroacupuncture/ 4. exp meridians/ 5. exp acupuncture points/ 6. Acupuncture Therapy/ 7. (meridian point* or meridian* or (ching adj2 lo) or (jing adj2 luo) or jingluo or acu point* or acu‐point* or acupoint*).ab,ti. 8. (acupuncture or electroacupuncture or electro‐acupuncture or electro acupuncture or Zhenjiu or Zhenci or Cizhen or Dianzhen).ab,ti. 9. 6 or 3 or 7 or 2 or 8 or 1 or 4 or 5 10. exp Craniocerebral Trauma/ 11. exp Brain Edema/ 12. exp Glasgow Coma Scale/ 13. exp Glasgow Outcome Scale/ 14. exp Unconsciousness/ 15. exp Cerebrovascular Trauma/ 16. ((head or crani* or cerebr* or capitis or brain* or forebrain* or skull* or hemispher* or intra‐cran* or inter‐cran*) adj3 (injur* or trauma* or damag* or wound* or fracture* or contusion*)).ab,ti. 17. ((head or crani* or cerebr* or brain* or intra‐cran* or inter‐cran*) adj3 (haematoma* or hematoma* or haemorrhag* or hemorrhag* or bleed* or pressure)).ti,ab. 18. (Glasgow adj3 (coma or outcome) adj3 (scale* or score*)).ab,ti. 19. "rancho los amigos scale".ti,ab. 20. ("diffuse axonal injury" or "diffuse axonal injuries").ti,ab. 21. ((brain or cerebral or intracranial) adj3 (oedema or edema or swell*)).ab,ti. 22. ((unconscious* or coma* or concuss* or 'persistent vegetative state') adj3 (injur* or trauma* or damag* or wound* or fracture*)).ti,ab. 23. or/10‐22 24. 9 and 23 25. randomi?ed.ab,ti. 26. randomized controlled trial.ab,ti. 27. controlled clinical trial.ab,ti. 28. placebo.ab,ti. 29. clinical trials.ab,ti. 30. randomly.ab,ti. 31. trial.ab,ti. 32. or/25‐31 33. humans.ab,ti. 34. 24 and 32 and 33
EMBASE
1. exp acupuncture analgesia/ 2. exp acupuncture, ear/ 3. exp electroacupuncture/ 4. exp meridians/ 5. exp acupuncture points/ 6. Acupuncture Therapy/ 7. (meridian point* or meridian* or (ching adj2 lo) or (jing adj2 luo) or jingluo or acu point* or acu‐point* or acupoint*).ab,ti. 8. (acupuncture or electroacupuncture or electro‐acupuncture or electro acupuncture or Zhenjiu or Zhenci or Cizhen or Dianzhen).ab,ti. 9. or/1‐8 10. exp Craniocerebral Trauma/ 11. exp Brain Edema/ 12. exp Glasgow Coma Scale/ 13. exp Glasgow Outcome Scale/ 14. exp Unconsciousness/ 15. exp Cerebrovascular Trauma/ 16. ((head or crani* or cerebr* or capitis or brain* or forebrain* or skull* or hemispher* or intra‐cran* or inter‐cran*) adj3 (injur* or trauma* or damag* or wound* or fracture* or contusion*)).ab,ti. 17. ((head or crani* or cerebr* or brain* or intra‐cran* or inter‐cran*) adj3 (haematoma* or hematoma* or haemorrhag* or hemorrhag* or bleed* or pressure)).ti,ab. 18. (Glasgow adj3 (coma or outcome) adj3 (scale* or score*)).ab,ti. 19. "rancho los amigos scale".ti,ab. 20. ("diffuse axonal injury" or "diffuse axonal injuries").ti,ab. 21. ((brain or cerebral or intracranial) adj3 (oedema or edema or swell*)).ab,ti. 22. ((unconscious* or coma* or concuss* or 'persistent vegetative state') adj3 (injur* or trauma* or damag* or wound* or fracture*)).ti,ab. 23. or/10‐22 24. 9 and 23 25. randomi?ed.ab,ti. 26. randomized controlled trial.ab. 27. controlled clinical trial.ab. 28. placebo.ab. 29. clinical trials.ab. 30. randomly.ab. 31. trial.ti. 32. or/25‐31 33. humans.tw. 34. 32 and 33 35. 34 and 24
AMED
1. exp acupuncture analgesia/ 2. exp acupuncture, ear/ 3. exp electroacupuncture/ 4. exp meridians/ 5. exp acupuncture points/ 6. Acupuncture Therapy/ 7. (meridian point* or meridian* or (ching adj2 lo) or (jing adj2 luo) or jingluo or acu point* or acu‐point* or acupoint*).ab,ti. 8. (acupuncture or electroacupuncture or electro‐acupuncture or electro acupuncture or Zhenjiu or Zhenci or Cizhen or Dianzhen).ab,ti. 9. 6 or 3 or 7 or 2 or 8 or 1 or 4 or 5 10. exp Craniocerebral Trauma/ 11. exp Brain Edema/ 12. exp Glasgow Coma Scale/ 13. exp Glasgow Outcome Scale/ 14. exp Unconsciousness/ 15. exp Cerebrovascular Trauma/ 16. ((head or crani* or cerebr* or capitis or brain* or forebrain* or skull* or hemispher* or intra‐cran* or inter‐cran*) adj3 (injur* or trauma* or damag* or wound* or fracture* or contusion*)).ab,ti. 17. ((head or crani* or cerebr* or brain* or intra‐cran* or inter‐cran*) adj3 (haematoma* or hematoma* or haemorrhag* or hemorrhag* or bleed* or pressure)).ti,ab. 18. (Glasgow adj3 (coma or outcome) adj3 (scale* or score*)).ab,ti. 19. "rancho los amigos scale".ti,ab. 20. ("diffuse axonal injury" or "diffuse axonal injuries").ti,ab. 21. ((brain or cerebral or intracranial) adj3 (oedema or edema or swell*)).ab,ti. 22. ((unconscious* or coma* or concuss* or 'persistent vegetative state') adj3 (injur* or trauma* or damag* or wound* or fracture*)).ti,ab. 23. or/10‐22 24. 9 and 23 25. randomi?ed.ab,ti. 26. randomized controlled trial.ab,ti. 27. controlled clinical trial.ab,ti. 28. placebo.ab,ti. 29. clinical trials.ab,ti. 30. randomly.ab,ti. 31. trial.ab,ti. 32. or/25‐31 33. humans.ab,ti. 34. 24 and 32 and 33
CINAHL
S1. acupuncture analgesia or acupuncture or electroacupuncture or eletrco‐acupuncture or meridians or acupuncture points or Acupuncture Therapy or meridian point or meridian or acu‐point or acupoint or Zhenjiu or Zhenci or Cizhen or Dianzhen
S2. Traumatic brain injury or Craniocerebral Trauma or Brain Edema or Cerebrovascular Trauma
S3. AB (randomized controlled trial or controlled clinical trial or placebo or clinical trials or randomly or trial) or TI (randomized controlled trial or controlled clinical trial or placebo or clinical trials or randomly or trial)
S4. S1 and S2 and S3
Appendix 2. Search strategy for TCMLARS, Chinese Clinical Trials Registry, China Journal Full‐text Database, China Master Theses Full‐text Database, China Doctor Dissertation Full‐text Database, China Proceedings of Conference Database via CNKI, and Index to Taiwan Periodical Literature System
We also searched the Chinese academic literature databases using keywords in simplified Chinese, and using synonyms of
1. 腦外傷 "Nao Wai Shang" (traumatic brain injury )
2. 針灸"ZhenJiu" (Acupuncture) or 針刺"ZhenCi" (Acupuncture) or 電針"DianZhen" (Electro‐acupuncture) or 針壓"ZhenYa" (Acupressure) or 耳穴"ErZhen" (Ear Acupuncture) or 體針"TiZhen" (Body acupuncture) or 舌針"SheZhen" (Tongue acupuncture) or 頭皮針"TouPiZhen" (Scalp acupuncture) or 穴位"XueWei" (acupoint)
3. 1 and 2
We also searched the Chinese academic literature databases using keywords in simplified Chinese, and using synonyms of acupuncture (針灸'Zhenjiu', 針刺'Zhenci', 施針'Cizhen') and synonyms of traumatic brain injury (腦外傷'Nao Wai Shang').
Data and analyses
Comparison 1. Acupuncture plus other treatment versus same other treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Post‐treatment Glasgow Coma Score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2 Post‐treatment Glasgow Outcome Score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3 Frequency of normal post‐treatment Glasgow Outcome Score | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Frequency of post‐treatment Barthel Index above 60 | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Frequency of post‐treatment Barthel Index above 40 | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6 Post‐treatment Modified Barthel Index | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 1 month post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 3 months post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Post‐treatment Fugl‐Meyer assessment | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 1 month post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 3 months post‐treatment | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Mortality | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9 Post‐treatment Speech Function Score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10 Post‐treatment Motor Function Score | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11 Frequency of post‐treatment muscle strength grade IV to VI | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.1 Upper limb | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 Lower limb | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cao 2001.
| Methods | RCT Randomization method: not specified Blinding: not specified Informed consent: not specified |
|
| Participants | Treatment group: 67 Comparator group: 67 Age: from 3 to 71 years old Sex: male: 81, female: 53 Inclusion: CT confirmation Exclusion: not specified Patient characteristics: hemiplegia: 122; aphasia: 67; blindness: 4; facial paralysis: 32; mental retardation: 16; traumatic seizure: 6; ataxia: 5 Duration of TBI: 17 days to 17 months |
|
| Interventions |
Treatment: scalp acupuncture + body electro‐acupuncture + hyperbaric oxygen + rehabilitation training Scalp acupuncture: Selection of points according to syndrome: Hemiplegia: motor cortex, Ding‐pang xian I and II (MS8 and MS9), foot motor‐sensory area Hemiplegia with convulsion: pre‐motor cortex (non‐affected side) Blindness: olfactory cortex Limbs thumbing: somatic sensory cortex (non‐affected side) Distortion of face: the lower 2/5 of the motor cortex, Tou‐wei (ST8) Nie‐qian‐xian (MS10) (non‐affected side) Mental retardation: 5 forehead points, 3 temporal points; Aphasia: visual cortex (affected side) Ataxia: balance division Needle: 1.5 to 3 cun Angle of needle insertion: 30 Needle retention time: 6 to 8 hours Additional needling was used for severe or slow recovery patients 0.5 to 1 cm next to the pertinent stimulation zone Body electro‐acupuncture: Hemiplegia: Qu‐chi (LI11), Wai‐guan (TE5), He‐gu (LI4), Huan‐tiao (GB30), Bi‐guan (ST31), Fu‐tu (ST32), Yang‐ling‐quan (GB34), Xuan‐zhong (GB39), Zu‐san‐li (ST36), Jie‐xi (ST41) Distortion of face: Di‐cang (ST4), Shui‐gou (GV26), Cheng‐jiang (CV24), Yi‐feng (TE17), Si‐ban (ST2), He‐gu (LI4), Tai‐chong (LR3) Mental retardation: Si‐shen‐cong (EXHN1), Shui‐gou (GV26), Nei‐guan (PC6), Shen‐men (HT7), Tai‐chong (LR3) Aphasia: Ya‐men (GV14), Lian‐quan (CV23), Tong‐li (HT5), Zhao‐hai (KI6) Blindness: Jing‐ming (BL1), Qiu‐hou (EX‐HN7), Feng‐chi (GB20), Guang‐ming (GB37) Epilepsy: Da‐zhui (GV14), Yao‐qi (EX‐B9) Giggle: Nei‐guan (PC6), Feng‐long (ST40) Convulsion of limbs: Chi‐ze (LU5), Shou‐san‐li (LI10), Wei‐zhong (BL40), San‐yin‐jiao (S6P) Needle length: 1 to 3 cun Method: Twirling and lifting‐thrusting method Electric stimulation after obtaining Qi Current: maximum tolerance of the patient Amplitude: disperse dense waves Electro‐acupuncture machine: G6805‐II Needle retention time: 30 minutes, no needle retention for child Control: hyperbaric oxygen + rehabilitation training |
|
| Outcomes | 1. Post‐treatment Barthel Index (BI) 2. Post‐treatment muscle strength grading |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not specified. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding was not specified. Since treatment involves an invasive procedure (acupuncture) and no placebo or sham control was employed, it is highly likely that the patients and physicians were not blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were 6 dropouts in each group. The reasons were not provided and they were excluded from analyses. This might introduce bias. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | The treatment and the control groups might not be comparable at baseline as the control group appeared to have more patients with good upper limb muscle power at baseline, which might introduce bias. Acupoints varied among patients and might introduce bias. No placebo or sham control was used and hence there might be placebo effect. The continuous outcome variable Barthel Index was categorized to 3 grades and might cause bias. |
Chang 2005.
| Methods | RCT Randomization method: not specified Blinding: not specified Informed consent: not specified |
|
| Participants | Treatment group: 32 Comparator group: 18 Age: 7 to 58 years old Inclusion: CT confirmation, TBI patients, conscious Exclusion: not specified Etiology: combat: 21; traffic: 23; fall: 4; others: 21 Patient characteristics: severe brain contusion: 7; epidural hematoma: 12; subdural hematoma: 4; intracerebral hematoma: 5; cerebellar hematoma: 4; coexistence of a variety of intracranial injuries: 16 Unilateral limb motor disorder: 6; bilateral limb motor disorder: 7; hemiplegia: 37 Duration of TBI: not specified |
|
| Interventions |
Treatment group: electro‐acupuncture + rehabilitation training (physiotherapy + occupational therapy) Electro‐acupuncture for two stage: Non‐convulsion period: electro‐acupuncture at 10 acupoints (HT1, LU5, HT2, PC3, PC6, GB30, ST32, ST36, SP9. ST41) Convulsion period: electro‐acupuncture at 8 acupoints (LI11, SI17, TE5, BL40, SP9, SP6, BL37, BL69), twirling and lifting‐thrusting, needle retained for 30 minutes, once daily Needle length: not specified Electric stimulation after obtaining Qi Amplitude: consistence waves Current: maximum tolerance of the patient Electro‐acupuncture machine: G6805‐II Control group: rehabilitation training Duration of treatment: 3 months |
|
| Outcomes | 1. Post‐treatment Modified Barthel Index (MBI) at 1 and 3 months 2. Post‐treatment Fugl‐Meyer Assessment (FMA) at 1 and 3 months |
|
| Notes | Duration of follow up: 3 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not specified. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding was not specified. Since treatment involves an invasive procedure (acupuncture) and no placebo or sham control was employed, it is highly likely that the patients and physicians were not blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | Acupoints varied among patients and might introduce bias. No placebo or sham control was used and hence there might be placebo effect. Outcomes were measured at 1 and 3 months after treatment. Additional treatments that patients received between study treatment completion and outcome assessments were not mentioned, but these might contribute to the effects observed at assessments and cause bias. |
Ding 2002.
| Methods | RCT Randomization method: not specified Blinding: not specified Informed consent: not specified |
|
| Participants | Treatment group (male): 30 (23) Control group: 30 (25) Age: 37.15 ± 14.11 (treatment group), 35.87 ± 13.93 (control group) Inclusion: GCS ≤ 8, confirmation by CT, hospital admission within 24 hours after injury, medically stable Exclusion: not specified Duration of TBI: within 24 hours after injury |
|
| Interventions |
Treatment: 2 courses of acupuncture + conventional medical intervention First course of acupuncture: Acupuncture at 3 ear acupoints, filiform needling; acupuncture at 7 body acupoints: Shui‐gou (GV26), pecking sparrow moxibustion; Lao‐gong (PC8), Yong‐quan (KI11), twirling draining; Zhao‐hai (KI6), Shen‐mai (BL62), Jiao‐xin (KI8), Fu‐yang (BL59), twirling and lifting‐thrusting draining; needle retained for 30 minutes, once daily for 10 days Second course of acupuncture: Acupuncture at 12 acupoints: Shui‐gou (GV26), pecking sparrow moxibustion; Yong‐quan (KI1), Lao‐gong (PC8), twirling draining, needle retained for 1 minute; Jian‐yu (LI12), Nao‐shu (SI10), Qu‐chi (LI11), Wai‐guan (TE5), He‐gu (LI4), Huan‐tiao (GB30), San‐yin‐jiao (SP6), Yang‐ling‐quan (GB34), Tai‐chong (LR3), twirling and lifting‐thrusting supplementation; Feng‐chi (GB20), twirling supplementation, needle retained for 30 minutes, once daily for 15 days. Control: conventional medical intervention |
|
| Outcomes | 1. Post‐treatment Glasgow Coma Score 2. Post‐treatment Glasgow Outcome Score 3. Post‐treatment Motor Function Score 4. Post‐treatment Speech Function score |
|
| Notes |
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not specified. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding was not specified. Since treatment involves an invasive procedure (acupuncture) and no placebo or sham control was employed, it is highly likely that the patients and physicians were not blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | No placebo or sham control was used and hence there might be placebo effect. The validity of motor and speech function scores were questionable and might introduce bias. |
Song 2007.
| Methods | RCT Randomization method: not specified Blinding: not specified Informed consent: not specified |
|
| Participants | Treatment group: 30 Control group: 20 Age: 12 to 70 years old Sex: not specified Inclusion:
Duration of TBI: within 6 hours after injury |
|
| Interventions |
Treatment: body electro‐acupuncture + scalp electro‐acupuncture + conventional medical intervention Body acupuncture: acupuncture at 7 points, additional acupuncture at 1 or 2 points depending on TCM diagnosis. Electro‐stimulation in 8 to 13 Hz for 30 minutes. Daily for 10 days. Scalp acupuncture: acupuncture at 4 points with length 25 to 40 mm needles; until the practitioner felt needle sensation, electro‐stimulation for 30 minutes, needle retained for 6 to 8 hours. Daily for 10 days. Electro acupuncture machine: G6805‐II Control: conventional medical intervention Duration of treatment: 1 month |
|
| Outcomes | Post‐treatment Glasgow Outcome Score at 1 month Mortality |
|
| Notes | Duration of follow up: 1 month | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sequence generation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not specified. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding was not specified. Since treatment involves an invasive procedure (acupuncture) and no placebo or sham control was employed, it is highly likely that the patients and physicians were not blind to treatment allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no dropouts. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | High risk | Acupoints varied among patients and might introduce bias. No placebo or sham control was used and hence there might be placebo effect. Outcomes were measured at 1 month after treatment. Additional treatments that patients received between study treatment completion and outcome assessments were not mentioned, but these might contribute to the effects observed at assessments and cause bias. |
CT = computed tomography GCS = Glasgow Coma Score GOS = Glasgow Outcome Score TBI = traumatic brain injury TCM = traditional Chinese medicine
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Chen 2007 | Acupuncture combined with Tui Na and baseline medication compared to baseline medication. Effect of the combination of interventions was investigated rather than that of acupuncture per se. Outcome measures over‐simplified, not currently recognised and did not provide strong objective data. |
| Donnellan 2006 | Case report |
| Gao 2007 | No indication that treatment and comparator are demographically and clinically comparable. Outcome measures over‐simplified, not currently recognized and did not provide strong objective data. |
| Gu 2004 | Compared different forms of acupuncture |
| Guo 2006 | Over simple method of randomization. Outcome measures over‐simplified, not currently recognized and did not provide strong objective data. |
| Han 2005 | Acupoint catgut‐embedding therapy combined with Chinese Herbal Medicine and baseline medication compared to western medicine Effect of the combination of interventions was investigated rather than that of acupuncture per se |
| He 2004 | Overall outcome measures over‐simplified and did not provide strong objective data |
| Huang 2006 | Acupuncture combined with hyperbaric oxygen compared to baseline medication Effect of the combination of interventions was investigated rather than that of acupuncture per se |
| Jia 2001 | Acupuncture compared to western medicine Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Li 1993 | Case series |
| Li 2003 | Acupuncture combined with Chinese Herbal Medicine compared to western conventional medication |
| Li 2005 | Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Liang 2000 | Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Liao 2006 | Acupuncture was only a component of a bundle of interventions. Effect of the combination of interventions was investigated rather than that of acupuncture per se. |
| Liu 2006 | The dosage of the painkiller in the 2 groups in baseline medication is different |
| Lu 2007 | Electro‐acupuncture combined with baseline medication compared to hyperbaric oxygen with baseline medication |
| Mukkamala 2003 | Case report |
| Shi 2004 | Acupuncture using plum blossom needle therapy compared to oral Rotundin |
| Sun 2005 | Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Tian 2007 | Acupuncture combined with Chinese Herbal Medicine and baseline medication compared to intravenous injection. Effect of the combination of interventions was investigated rather than that of acupuncture per se. |
| Wang 2007 | Patients included stroke and/or TBI induced trunk/limb seizures |
| Wei 2001 | Acupuncture in combination with acupoint injection versus acupuncture alone |
| Wei 2007 | Electro‐acupuncture combined with Chinese Herbal Medicine compared to baseline medication |
| Wu 2007 | Acupuncture combined with Chinese Herbal Medicine and baseline medication compared to baseline medication. Effect of the combination of interventions was investigated rather than that of acupuncture per se. |
| Xiang 2007 | Acupuncture combined with Tui Na, hyperbaric oxygen and baseline medication compared to baseline medication and hyperbaric oxygen. Effect of the combination of interventions was investigated rather than that of acupuncture per se. |
| Xu 2006 | Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Xu 2007 | Acupuncture was only a component of a bundle of interventions. Effect of the combination of interventions was investigated rather than that of acupuncture per se. |
| Yang 2004 | Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Zhang 1996 | Acupuncture compared to physiotherapy |
| Zhang 2005 | No detailed information for analysis |
| Zhao 2000 | Outcome measures over‐simplified, not currently recognized and did not provide strong objective data |
| Zheng 2005 | The report indicated the use of Barthel Index without providing pre‐ and post‐intervention data |
Contributions of authors
VW and KLC led the preparation of the review. SW and VC assessed the eligibility of identified studies and extracted data from included studies. VW, SL and VC wrote the first draft of the review, and all authors commented on the paper.
Sources of support
Internal sources
-
Hospital Authority, Hong Kong.
Funding for development of 'Integration of Chinese Medicine and Western Medicine in Acute Rehabilitation of Traumatic Brain Injury and Other Neurological Disorders'.
External sources
No sources of support supplied
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Cao 2001 {published data only}
- Cao WS, Qin YX, Hou QX. Acupuncture combined with hyperbaric oxygen treatment for post‐traumatic brain injury syndrome (Translation). Modern Rehabilitation, Journal of Clinical Rehbilitative Tissue Engineering 2001;5(8):110. [cnki:ISSN:1007‐5496.0.2001‐16‐117] [Google Scholar]
Chang 2005 {published data only}
- Chang ZJ, Liu P. (Translation) Rehabilitation and acupuncture treatment for patients with traumatic brain injury. Chinese Journal of Medical Device 2005;18(5):38‐9. [cnki:ISSN:1002‐2376.0.2005‐05‐026] [Google Scholar]
Ding 2002 {published data only}
- Ding J, Dong GF, Song YX, Xu YC. Control observation on therapeutic effects of acupuncture treatment on acute severe craniocerebral injury. Chinese Acupuncture & Moxibustion 2002;22(7):445‐7. [cnki:ISSN:0255‐2930.0.2002‐07‐006] [Google Scholar]
Song 2007 {published data only}
- Song YJ, Zhang L, Zhang L. Observations on the efficacy of electroacupuncture‐assisted treatment for resuscitating coma patients with serious brain trauma. Shanghai Journal of Acupuncture and Moxibustion 2007;26(4):11‐2. [CNKI:ISSN:1005‐0957.0.2007‐05‐005] [Google Scholar]
References to studies excluded from this review
Chen 2007 {published data only}
- Chen YL, Zhou GL. Therapeutic effect of acupuncture and Tui na treatment for post TBI syndrome 42 cases (Translation). Jilin Journal of Traditional Chinese Medicine 2007;27(12):38‐9. [Google Scholar]
Donnellan 2006 {published data only}
- Donnellan CP. Acupuncture for central pain affecting the ribcage following traumatic brain injury and rib fractures ‐ a case report. Acupuncture in Medicine 2006;24(3):129‐33. [DOI] [PubMed] [Google Scholar]
Gao 2007 {published data only}
- Gao ZY. Observation of the efficacy of using brain‐activating and orifice‐opening acupuncture combined with ear‐points acupressure in treating traumatic brain injury (Translation). Journal of New Chinese Medicine 2007;39(3):29‐30. [CNKI:ISSN:0256‐7415.0.2007‐03‐019] [Google Scholar]
Gu 2004 {published data only}
- Gu Q. (Translation) Compare the therapeutic effects of acupoint inject and acupuncture for severe TBI patients. Jiangxi Journal of Traditional Chinese Medicine 2004;259(7):57‐8. [cnki:ISSN:0411‐9584.0.2004‐07‐039] [Google Scholar]
Guo 2006 {published data only}
- Guo Y. Acupuncture for patients with traumatic brain injury 42 cases (Translation). Shanxi Journal of Traditional Chinese Medicine 2006;22(5):40‐1. [cnki:ISSN:1000‐7156.0.2006‐05‐025] [Google Scholar]
Han 2005 {published data only}
- Han GZ, Han YB. (Translation) Observation on therapeutic effect of integrated treatment of traditional Chinese medicine and Western medicine in post traumatic brain injury seizure 268 cases. Chinese Community Doctors 2005;50(4):42‐3. [cnki:ISSN:1007‐614X.0.2005‐04‐050] [Google Scholar]
He 2004 {published data only}
- He J, Wu B, Zhang YL. Therapeutic effect of acupuncture combined with acupoint injection for patient with coma after traumatic brain injury 15 cases (Translation). Journal of Traditional Chinese Medicine 2004;45(7):504‐5. [cnki:ISSN:1001‐1668.0.2004‐07‐018] [Google Scholar]
Huang 2006 {published data only}
- Huang XL, Lai XH. (Translation) The therapeutic effect of hyperbaric oxygen combined with acupuncture for treating patient with traumatic brain injury hemiplegia. Journal of Qilu Nursing 2006;12(4):736. [cnki:ISSN:1006‐7256.0.2006‐08‐059] [Google Scholar]
Jia 2001 {published data only}
- Jia J, Hu SH, Mao GL. Clinical observations on acupuncture treatment of post‐traumatic cervicocranial syndrome. Shanghai Journal of Acupuncture and Moxibustion 2001;20(2):7‐8. [cnki:ISSN:1005‐0957.0.2001‐02‐003] [Google Scholar]
Li 1993 {published data only}
- Li Y, Wang XY, Li TL. Acupuncture therapy for 12 cases of cranial trauma. Journal of Traditional Chinese Medicine 1993;13(1):5‐9. [PubMed] [Google Scholar]
Li 2003 {published data only}
- Li ZZ, Sun XD, Zhang XJ, Cao R, Qi BG, Liu SS. Observation on therapeutic effect of integrated treatment of traditional Chinese medicine and western medicine in promoting revival of coma for the patient of severe craniocerebral trauma. Chinese Acupuncture and Moxibustion 2003;23(7):380‐2. [cnki:ISSN:0255‐2930.0.2003‐07‐001] [Google Scholar]
Li 2005 {published data only}
- Li HY, Yang L, Sun HX. (Translation) Therapeutic effect of acupuncture for post traumatic brain injury headache 62 cases. Hubei College of Traditional Chinese Medicine 2005;27(5):46. [cnki:ISSN:1000‐0704.0.2005‐05‐028] [Google Scholar]
Liang 2000 {published data only}
- Liang W. (Translation) Acupuncture for 24 patients with traumatic brain injury and aphasia. New Journal of Traditional Chinese Medicine 2000;32(12):21. [cnki:ISSN:0256‐7415.0.2000‐12‐010] [Google Scholar]
Liao 2006 {published data only}
- Liao L, Xu YL. (Translation) Effects of movement function in TBI patients treated by acupuncture and rehabilitation training. Chinese Journal of Physical Medicine and Rehabilitation 2006;28(2):124‐6. [cnki:ISSN:0254‐1424.0.2006‐02‐022] [Google Scholar]
Liu 2006 {published data only}
- Liu HR, Fu RH, Liu XM, Shi YL, Su ZW, Zhang ZW, et al. Clinical study on treatment of cerebral post‐traumatic intractable headache by tapping scalp specific points with plum‐blossom needle. Shanghai Journal of Acupuncture and Moxibustion 2006;25(10):5‐7. [Google Scholar]
Lu 2007 {published data only}
- Lu YZ, Zhou JH, Lu W, Chen G, Tang ZF, Wu WJ, et al. (Translation) Electro acupuncture for 32 patients with post TBI persistent vegetative status. Jiangsu Journal of Traditional Chinese Medicine 2007;39(2):43‐5. [CNKI:ISSN:1672‐397X.0.2007‐02‐027] [Google Scholar]
Mukkamala 2003 {published data only}
- Mukkamala S, Tambay N. Acupuncture for persistent symptoms in a patient with mild traumatic brain injury: a case report. Archives of Physical Medicine and Rehabilitation 2003;84:A7. [Google Scholar]
Shi 2004 {published data only}
- Shi YL, Fu RH, Fang MZ. Clinical study on Cixue Tongjing Jiannao method for treatment of headache after head injury. Chinese Acupuncture & Moxibustion 2004;24(10):670‐2. [cnki:ISSN:0255‐2930.0.2004‐10‐001] [Google Scholar]
Sun 2005 {published data only}
- Sun Y. Therapeutic effect of acupuncture for post traumatic brain injury depression (Translation). Journal of Clinical Acupuncture and Moxibustion 2005;21(9):25. [cnki:ISSN:1005‐0779.0.2005‐09‐016] [Google Scholar]
Tian 2007 {published data only}
- Tian XG, Tian JP, Wan XW. (Translation) Electro‐acupuncture combined with Chinese herbal medicine for treating patient with traumatic brain injury paralysis 98 cases. Gansu Journal of Traditional Chinese Medicine 2007;20(1):40‐1. [ CNKI:ISSN:1004‐6852.0.2007‐01‐027 ] [Google Scholar]
Wang 2007 {published data only}
- Wang JC, Yang ZH, Zhang L. Integrated Chinese and western medicine for treating limb convulsion caused by stroke and TBI (Translation). Journal of Traditional Chinese Medicine 2007;48(2):149. [CNKI:ISSN:1001‐1668.0.2007‐02‐023] [Google Scholar]
Wei 2001 {published data only}
- Wei L. Therapeutic effect of acupuncture combined with acupoint‐injection on post‐traumatic brain syndrome. Chinese Acupuncture & Moxibustion 2001;21(8):483‐4. [cnki:ISSN:0255‐2930.0.2001‐08‐018] [Google Scholar]
Wei 2007 {published data only}
- Wei YX, Yu YC. Observation of therapeutic effect of integrated treatment for traumatic cerebral infarction 21 cases (Translation). Guangxi Journal of Traditional Chinese Medicine 2007;30(5):20‐1. [CNKI:SUN:GXZY.0.2007‐05‐009] [Google Scholar]
Wu 2007 {published data only}
- Wu YF, Liang L, He J, Guo YF. (Translation) Observation on therapeutic effect of integrated treatment of traditional Chinese medicine and Western medicine in post traumatic brain injury seizure 30 cases. Chinese Journal of Modern Drug Application 2007;1(4):43. [CNKI:SUN:ZWYY.0.2007‐04‐034] [Google Scholar]
Xiang 2007 {published data only}
- Xiang GB, Deng Y, Wu XW, Zhang GX, Fei QY, Ding X. The clinical evaluation of hyperbaric oxygen and acupuncture massage of TCM therapy in gravis type craniocerebral trauma. Journal of Anhui Traditional Chinese Medical College 2007;26(1):27‐9. [CNKI:ISSN:1000‐2219.0.2007‐01‐011] [Google Scholar]
Xu 2006 {published data only}
- Xu XL, Xiao MR. Electro‐acupuncture combined with electro‐pulsation for treating patients with traumatic brain injury (Translation). Journal of Clinical Acupuncture and Moxibustion 2006;22(7):39. [cnki:ISSN:1005‐0779.0.2006‐07‐025] [Google Scholar]
Xu 2007 {published data only}
- Xu YL, Huang RX. Effects of movement and cognition function in TBI patients treated by acupuncture and rehabilitation training. Chinese Journal of Practical Nervous Diseases 2007;10(7):19. [CNKI:SUN:HNSJ.0.2007‐07‐011] [Google Scholar]
Yang 2004 {published data only}
- Yang XH, Wang XL. Effectiveness of treating aphemia with acupuncture and moxibustion in combination with speaking training. Journal of Nursing Science 2004;19(15):30‐1. [cnki:ISSN:1001‐4152.0.2004‐15‐017] [Google Scholar]
Zhang 1996 {published data only}
- Zhang AR, Pan ZW, Luo F, Yang XD. Effect of acupuncturing Houxi (SI3) and Shenmen (HT7) in treating cerebral traumatic Dementia. Chinese Journal of Integrative Medicine 1996;15(4):262‐265. [cnki:ISSN:10035370.0.1995‐09‐001] [PubMed] [Google Scholar]
Zhang 2005 {published data only}
- Zhang JH, Fan JZ, Qi ZQ. Brainstem auditory evoked potentials of patients with mild to moderate traumatic brain injury during acupuncture. Chinese Journal of Rehabilitation 2005;20(1):23‐4. [Google Scholar]
Zhao 2000 {published data only}
- Zhao JP. Clinical observation of 50 patients with craniocerebral traumatic facial paralysis treated by acupuncture. Shanghai Journal of Traditional Chinese Medicine 2000;16(8):35. [cnki:ISSN:31‐1276.0.2000‐08‐016] [Google Scholar]
Zheng 2005 {published data only}
- Zheng JJ, Fi JZ, Wu HY. Activating brain and repairing consciousness needling method combined with rehabilitation training for patients with closed cranial injury 73 cases (Translation). Journal of Clinical Acupuncture and Moxibustion 2005;21(7):38‐9. [cnki:ISSN:1005‐0779.0.2005‐07‐033] [Google Scholar]
Additional references
CDC 2008
- Centers for Disease Control and Prevention. Traumatic brain injury. Available at http://www.cdc.gov/ncipc/tbi/TBI.htm (accessed 21 Nov 2008).
Cheuk 2006
- Cheuk DKL, Wong V. Acupuncture for epilepsy. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD005062.pub3] [DOI] [PubMed] [Google Scholar]
Cheuk 2007
- Cheuk DKL, Yeung WF, Chung KF, Wong V. Acupuncture for insomnia. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD005472.pub2] [DOI] [PubMed] [Google Scholar]
Chua 2007
- Chua KSG, Ng YS, Yap SGM, Bok CW. A brief review of traumatic brain injury rehabilitation. Annals of Academy of Medicine Singapore 2007;36:31‐42. [PubMed] [Google Scholar]
Ding 2007
- Ding J, Dong GF, Song YX. Control observation on therapeutic effects of acupuncture treatment on acute severe craniocerebral injury. Zhongguo Zhenjiu 2002;22(7):445‐7. [Google Scholar]
Egger 1997
- Egger M, Davey‐Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphic test. BMJ 1997;315(7):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ernst 2001
- Ernst E. The desktop guide to complementary and alternative medicine. An evidence based approach. New York: Mosby, 2001. [Google Scholar]
He 2008
- He L, Zhou MK, Zhou D, Wu B, Li N, Kong SY. Acupuncture for Bell's palsy. Cochrane Database of Systematic Reviews 2010, Issue 8. [DOI: 10.1002/14651858.CD002914.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.0. The Cochrane Collaboration 2008. Available from www.cochrane‐handbook.org.
Hyder 2007
- Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation 2007;22:341‐53. [PubMed] [Google Scholar]
Jansen 1989
- Jansen G, Lundeberg T, Kjartansson S, Samuelson UE. Acupuncture and sensory neuropeptides increase cutaneous blood flow in rats. Neuroscience Letters 1989;97:305‐9. [DOI] [PubMed] [Google Scholar]
Johansson 1993
- Johansson K, Lindgren I, Widner H, Wiklund I, Johansson BB, Johansson K, et al. Can sensory stimulation improve the functional outcome in stroke patients?. Neurology 1993;43:2189‐92. [DOI] [PubMed] [Google Scholar]
Kaptchuk 2002
- Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Annals of Internal Medicine 2002;136(5):374‐83. [DOI] [PubMed] [Google Scholar]
Kay 1993
- Kay T, Harrington DE, Adams R. Definition of mild traumatic brain injury. Journal of Head Trauma and Rehabilitation 1993;8:86‐7. [Google Scholar]
Khan 2003
- Khan F, Baguley IJ, Cameron ID. Rehabilitation after traumatic brain injury. Medical Journal of Australia 2003;178:290‐5. [DOI] [PubMed] [Google Scholar]
Langlois 2006
- Langlois JA, Rutland‐Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. Journal of Head Trauma and Rehabilitation 2006;21(5):375‐8. [DOI] [PubMed] [Google Scholar]
Lund 2006
- Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls?. Acupuncture in Medicine 2006;24(1):13‐5. [DOI] [PubMed] [Google Scholar]
MacPherson 2010
- MacPherson H, Altman DG, Hammerschlag R, Li Y, Wu T, White A, et al. Revised Standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Acupuncture in Medicine 2010;28(2):83‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Magnusson 1994
- Magnusson M, Johansson K, Johansson BB. Sensory stimulation promotes normalization of postural control after stroke. Stroke 1994;25:1176‐80. [DOI] [PubMed] [Google Scholar]
Melchart 2008
- Melchart D, Linde K, Berman B, White A, Vickers A, Allais G, et al. Acupuncture for idiopathic headache. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD001218] [DOI] [PubMed] [Google Scholar]
NIHCP 1997
- National Institutes of Health Consensus Panel. Acupuncture: National Institutes of Health Consensus Development Conference Statement. National Institutes of Health http://consensus.nih.gov/1997/1997Acupuncture107html.htm (accessed 21 Nov 2008).
Parikh 2007
- Parikh S, Koch M, Narayan R. Traumatic brain injury. International Anesthesiology Clinics 2007;45(3):119‐35. [DOI] [PubMed] [Google Scholar]
Pomeranz 1989
- Pomeranz B. Acupuncture analgesia for chronic pain: brief survey of clinical trials. In: Pomeranz B, Stux G editor(s). Scientific Basis of Acupuncture. Berlin: Springer‐Verlag, 1989:197‐9. [Google Scholar]
RevMan 2008 [Computer program]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2008.
Rosenthal 1990
- Rosenthal M, Griffith ER, Bond MR. Rehabilitation of the adult and child with traumatic brain injury. 2nd Edition. Philadelphia: FA Davis, 1990. [Google Scholar]
Rosso 2007
- Rosso A, Brazinova A, Janciak I, Wilbacher I, Rusnak M, Mauritz W. Severe traumatic brain injury in Austria II: epidemiology of hospital admissions. Wiener Klinische Wochenschrift 2007;119(1‐2):29‐34. [DOI] [PubMed] [Google Scholar]
Scott 2005
- Scott SG, Vanderploeg RD, Belager HG, Scholten JD. Blast injuries: evaluating and treating the postacute sequelae. Federal Practitioner 2005;22(1):67‐75. [Google Scholar]
SCSSS 1999
- Swedish Collaboration on Sensory Stimulation in Stroke (SCSSS). Sensory stimulation after stroke: a randomized controlled trial. Cerebrovascular Disease 1999;9 (Suppl 1):28. [Google Scholar]
Streitberger 1998
- Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. The Lancet 1998;352:364‐5. [DOI] [PubMed] [Google Scholar]
Sun 2001
- Sun HL, Li XM. Clinical study on treatment of cerebral apoplexy with penetration needling of scalp acupoints. Chinese Acupuncture and Moxibustion 2001;21(5):275‐8. [Google Scholar]
UMHS 2003
- University of Michigan Health System. Brain injury patients now turning to alternative medicine for treatment. Available at: http://www.med.umich.edu/opm/newspage/2003/tbicam.htm (accessed 4 July 2008).
White 2001
- White AR, Filshie J, Cummings TM. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complementary Therapies in Medicine 2001;9(4):237‐45. [DOI] [PubMed] [Google Scholar]
Wu 1996
- Wu JN. A short history of acupuncture. Journal of Alternative and Complementary Medicine 1996;2(1):19‐21. [DOI] [PubMed] [Google Scholar]
Wu 2008
- Wu HM, Tang JL, Lin XP, Lau J, Leung PC, Woo J. Acupuncture for stroke rehabilitation. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD004131.pub2] [DOI] [PubMed] [Google Scholar]
Zhang 2005
- Zhang SH, Liu M, Asplund K, Li L. Acupuncture for acute stroke. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD003317.pub2] [DOI] [PubMed] [Google Scholar]


