Abstract
Background
Restless legs syndrome (RLS) is a common movement disorder for which patients may seek treatment with acupuncture. However, the benefits of acupuncture in the treatment of RLS are unclear and have not been evaluated in a systematic review until now.
Objectives
To evaluate the efficacy and safety of acupuncture therapy in patients with RLS.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1, 2007), MEDLINE (January 1950 to February 2007), EMBASE (January 1980 to 2007 Week 8), Chinese Biomedical Database (CBM) (1978 to February 2007), China National Knowledge Infrastructure (CNKI) (1979 to February 2007), VIP Database (1989 to February 2007), Japana Centra Revuo Medicina (1983 to 2007) and Korean Medical Database (1986 to 2007). Four Chinese journals, relevant academic conference proceedings and reference lists of articles were handsearched.
Selection criteria
Randomized controlled trials and quasi‐randomized trials comparing acupuncture with no intervention, placebo acupuncture, sham acupuncture, pharmacological treatments, or other non‐acupuncture interventions for primary RLS were included. Trials comparing acupuncture plus non‐acupuncture treatment with the same non‐acupuncture treatment were also included. Trials that only compared different forms of acupuncture or different acupoints were excluded.
Data collection and analysis
Two authors independently identified potential articles, assessed methodological quality and extracted data. Relative risk (RR) was used for binary outcomes and weighted mean difference for continuous variables. Results were combined only in the absence of clinical heterogeneity.
Main results
Fourteen potentially relevant trials were identified initially, but twelve of them did not meet the selection criteria and were excluded. Only two trials with 170 patients met the inclusion criteria. No data could be combined due to clinical heterogeneity between trials. Both trials had methodological and/or reporting shortcomings. No significant difference was detected in remission of overall symptoms between acupuncture and medications in one trial (RR 0.97, 95% CI 0.76 to 1.24). Another trial found that dermal needle therapy used in combination with medications and massage was more effective than medications and massage alone, in terms of remission of unpleasant sensations in the legs (RR 1.36, 95% CI 1.06 to 1.75; WMD ‐0.61, 95% CI ‐0.96 to ‐0.26) and reduction of RLS frequency (WMD ‐3.44, 95% CI ‐5.15 to ‐1.73). However, there was no significant difference for the reduction in either the longest or the shortest duration of RLS (WMD ‐2.58, 95% CI ‐5.92 to 0.76; WMD ‐0.38, 95% CI ‐1.08 to 0.32).
Authors' conclusions
There is insufficient evidence to determine whether acupuncture is an efficacious and safe treatment for RLS. Further well‐designed, large‐scale clinical trials are needed.
Keywords: Humans, Acupuncture Therapy, Acupuncture Therapy/methods, Randomized Controlled Trials as Topic, Restless Legs Syndrome, Restless Legs Syndrome/therapy
Plain language summary
There is insufficient evidence to support the use of acupuncture for the symptomatic treatment of restless legs syndrome.
Restless legs syndrome (RLS) is a sensorimotor movement disorder characterized by uncomfortable sensations in the legs and an urge to move them. The syndrome is very common and its lifestyle impacts justify a search for more effective and acceptable interventions.
Acupuncture is an ancient Chinese therapeutic method. It regulates the function of internal organs and rebalances body energies by stimulating certain acupoints. As a non‐pharmacological therapy, it would be of potential value in the treatment of RLS.
This review investigated the efficacy and adverse effects of acupuncture in treating RLS. The review did not find consistent evidence to determine whether acupuncture is effective and safe in the treatment of RLS, based on the two trials identified. More high quality trials are warranted before the routine use of acupuncture can be recommended for patients suffering from RLS.
Background
Restless legs syndrome (RLS), a common sensorimotor movement disorder first described in detail by Ekbom (Ekbom 1945), ranges in severity from merely causing annoyance in the patient to affecting sleep and quality of life severely enough to warrant medical treatment (Allen 2005). Although its negative impact is beyond doubt, RLS is still widely under‐diagnosed and inadequately treated (Hogl 2005b).
Remarkable differences in prevalence rates of RLS can be observed across countries and geographic regions. Epidemiological research demonstrates that the prevalence of RLS in adults (18 years or more) ranges from less than 1% (Tan 2001) in Singapore to approximately 10% in Europe and the United States (Hogl 2005a). Such differences may be caused by variations in study methods. Racial and genetic factors may also play a role in such discrepancies (Tison 2005).
In 1995, a uniform diagnosis of RLS was made possible worldwide, based on the criteria proposed by the International RLS Study Group (IRLSSG) (Walters 1995). According to the most recently revised diagnostic criteria (Allen 2003), the four clinical manifestations mandatory for the diagnosis are:
(1) an urge to move the legs, accompanied or caused by uncomfortable and unpleasant sensations in the legs;
(2) the urge to move or the unpleasant sensations begin or worsen during periods of rest or inactivity;
(3) the urge to move or the unpleasant sensations are partially or totally relieved by movement;
(4) the urge to move or the unpleasant sensations are worse in the evening or night or only occur in the evening or night.
Another associated sleep disorder, periodic leg movements during sleep (PLMS), is observed in about 85% of patients with RLS (Wong 2006). PLMS are repetitive, stereotypical movements and include extension of the big toe with fanning of the small toes accompanied by flexion at the ankles, knees and thighs. They can cause significant disruption of sleep with decreased total sleep time and a consequent increase in daytime sleepiness (Schapira 2004). Though not specific to RLS, PLMS can be supportive in its diagnosis (Allen 2003).
Etiology
The etiology of RLS is still not completely understood. Iron deficiency, renal failure and pregnancy may actually contribute to RLS, which is then considered secondary RLS (Harrison's 2001). Apart from the above established causes, there are no known physical abnormalities associated with the disorder (Hornyak 2006). A hypothesis of primary RLS etiology is associated with brain iron homeostasis (Bogan 2006; Hogl 2005a). A study using magnetic resonance imaging has demonstrated reduced levels of iron in the substantia nigra and putamen of patients with primary RLS (Allen 2001). Interestingly, iron is a co‐factor for tyrosine hydroxylase, the rate‐limiting enzyme in dopamine production (Schapira 2004).
Although the exact role of dopamine in the pathogenesis of RLS remains ill‐defined (Lin 1998), positive results have been demonstrated by several double‐blind clinical trials, in which the dopamine precursor Levodopa (L‐dopa) or dopamine agonists were applied (Allen 1998; Bogan 2006; Brodeur 1988; Montplaisir 1999; Walters 1988), thus implicating that both the dysfunction of dopaminergic systems and brain iron homeostasis may cause the condition of RLS (Bogan 2006).
Treatment
A shift from L‐dopa toward dopamine agonists as the first‐line treatment for RLS had been suggested by the Medical Advisory Board of the Restless Legs Syndrome Foundation (Silber 2004). Dopamine agonists are less likely to cause augmentation and rebound. Augmentation has been defined as an earlier onset of RLS symptoms during the day, more rapid onset of symptoms when at rest, together with increased severity and shorter symptomatic relief from dopaminergic therapy (NINDS 2006; Schapira 2004). Rebound is the appearance of RLS symptoms when the effects of the drug are wearing off (Trenkwalder 2005). In 2005, ropinirole, a nonergot‐based dopamine agonist, became the only drug approved by the U.S. Food and Drug Administration specifically for the treatment of moderate to severe RLS (Bogan 2006; NINDS 2006).
Apart from medications, certain lifestyle changes, decreased use of caffeine, alcohol, and tobacco, maintaining a regular sleep pattern and regular moderate exercise might also provide some relief for patients with RLS, but rarely do these efforts completely eliminate symptoms (NINDS 2006).
Acupuncture, an ancient Chinese medical therapy used in the prevention and treatment of disease, is another useful method for treating RLS (Wang 2001). It involves inserting needles into specific points (acupoints or Xue Wei) on the human body to bring about its therapeutic effects. Conventional science suggests that acupuncture works by neurological, neurohormonal as well as psychological mechanisms (Smith 2006), and it is thought to confer an analgesic effect (Green 2006). Several kinds of acupuncture methods, such as body acupuncture, auricular acupuncture, scalp acupuncture, electro‐acupuncture, laser acupuncture, acupressure, acupoint injection therapy (injection of drugs into acupoints) or a combination of the approaches mentioned above, are used in the treatment of RLS (Sun 2002; Wang 1994; Wen 2000; Zhao 2005a).
The mechanism of acupuncture treatment for RLS is still ill‐defined. According to our preliminary research, the current practice of acupuncture for RLS is mainly based on principles of Traditional Chinese Medicine (TCM) rather than conventional science. The traditional explanation, based on TCM theory, is that acupuncture restores the balance between Yin and Yang and regulates Qi (the essence) and blood so that integral unity can be maintained and miscellaneous diseases cured (Yang 1997).
Some clinical trials have examined the efficacy of acupuncture in the treatment of RLS and demonstrated that it was able to alleviate the clinical symptoms (Qiao 1997; Song 2004; Wang 2005). To our knowledge, however, no systematic review has been published addressing the effectiveness and safety of acupuncture for relief of RLS symptoms. Therefore, this review focused on investigating the therapeutic efficacy and safety of acupuncture for RLS.
Objectives
The objectives of this systematic review are to evaluate the efficacy and safety of acupuncture therapy in patients with RLS.
The following hypotheses are to be tested:
(1) acupuncture is more effective than placebo acupuncture, sham acupuncture or no treatment in treating RLS;
(2) acupuncture is more effective than Western medicine or herbal medicine in treating RLS;
(3) there are fewer adverse effects in the acupuncture group than in the Western medicine or herbal medicine group.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs) and quasi‐randomized trials (i.e., trials that used odd‐even numbers or patient medical record numbers etc. as methods of allocation).
Studies were single or double blind or unblinded.
Types of participants
Inclusion criteria
We included patients with primary RLS consistent with the diagnostic criteria defined by IRLSSG (Allen 2003; Walters 1995) irrespective of gender, race, age and setting.
Exclusion criteria
We excluded patients with any signs of psychiatric or organic disorders.
Types of interventions
We included trials evaluating all forms of acupuncture therapy including body acupuncture, auricular acupuncture, scalp acupuncture, electro‐acupuncture, laser acupuncture, dermal needle therapy, acupoint injection therapy, acupressure therapy and other acupuncture interventions.
The control interventions were: (1) no intervention, placebo acupuncture or sham acupuncture;
(2) pharmacological treatments (Western medicine or herbal medicine or combination of them);
(3) other non‐acupuncture interventions.
We also included trials that compared acupuncture therapy plus non‐acupuncture treatment with the same non‐acupuncture treatment.
We excluded trials that only compared different forms of acupuncture or different acupoints.
Types of outcome measures
Primary outcomes (1) Unpleasant sensations of RLS measured by any type of validated scale (for example, visual analog scale (VAS)). (2) Improvement of overall symptoms measured as a dichotomous outcome (remission versus no remission).
Secondary outcomes
We also considered the following outcome measures:
(1) periodic leg movements during sleep (PLMS) index;
(2) absolute or percentage reduction in RLS frequency and duration;
(3) sleep disturbance measured on a scale (for example, sleep onset latency (SOL));
(4) wakefulness after sleep onset (WASO) or by reported total sleep time;
(5) daytime functioning;
(6) quality of life measures (e.g. SF‐36);
(7) frequency and types of adverse effects.
Search methods for identification of studies
(1) Electronic searches
We searched the following electronic databases irrespective of language and publication status: the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 1, 2007), MEDLINE (January 1950 to February 2007), EMBASE (January 1980 to 2007 Week 8), Chinese Biomedical Database (CBM) (1978 to February 2007), China National Knowledge Infrastructure (CNKI) (1979 to February 2007), and VIP Database (1989 to February 2007). In addition, we checked Japana Centra Revuo Medicina (http://www.jamas.gr.jp/) (1983 to 2007) and Korean Medical Database (http://kmbase.medric.or.kr/) (1986 to 2007) for trials published in Japanese and Korean respectively.
We also checked the reference lists of all included studies for other potentially relevant publications.
CENTRAL (Ovid), MEDLINE (Ovid), EMBASE (Ovid)
Search strategy to locate RLS:
#1 restless legs syndrome
#2 RLS
#3 periodic leg movements
#4 PLM or PLMS
#5 Ekbom
#6 or/1‐5
Search Strategy to locate acupuncture interventions:
#7 acupuncture
#8 electroacupuncture
#9 electro‐acupuncture
#10 acupuncture points
#11 body acupuncture
#12 auricular acupuncture
#13 ear acupuncture
#14 scalp acupuncture
#15 laser acupuncture
#16 acupoint injection
#17 dermal needle
#18 acupressure
#19 or/7‐18
#20 6 and 19
The search strategy was translated accordingly for the databases in Chinese, Japanese and Korean.
A record of the electronic searches conducted above was kept for future review.
(2) The following journals were handsearched from the first issue to February 2007: Chinese Acupuncture & Moxibustion, Shanghai Journal of Acupuncture and Moxibustion, Acupuncture Research and Journal of Clinical Acupuncture and Moxibustion.
(3) We handsearched acupuncture and movement disorders conference abstracts over the past five years for further eligible studies.
(4) We contacted researchers in the field of acupuncture and movement disorders for unpublished and ongoing studies.
(5) We consulted leading Chinese experts in RLS to ascertain that no trial was missed.
Data collection and analysis
Study identification
Two review authors (Cui and Wang) independently screened and identified all potentially relevant studies, and then selected the trials that fulfilled the inclusion criteria. Disagreements between review authors were resolved by consensus with the arbitrator (Liu).
Quality assessment
Two review authors (Cui and Wang) independently assessed the methodological quality of the included trials. Disagreements between review authors were resolved by consensus with the arbitrator (Liu).
According to the empirical evidence (Jadad 1996; Kjaergard 2001; Moher 1998; Schulz 1995), we assessed the methodological quality of each trial based on the recommendations in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005).
1. Method of randomization: A method to generate the sequence of randomization was regarded as adequate (computer‐generated random numbers, table of random numbers etc.) if it allowed each study participant to have the same chance to receive each intervention and the investigators could not predict which was the next treatment.
2. Allocation concealment: Adequate (central randomization; serially numbered, opaque, sealed envelopes) or inadequate (open list enrolment).
3. Blinding: The method of trials using blinding for outcome assessors alone or together with blinding for participants was considered as adequate, because it was unlikely for acupuncture practitioners to be blinded.
4. Follow‐up: Adequate (number and reasons for dropouts and withdrawals described) or inadequate (number or reasons for dropouts and withdrawals not described). If there were no withdrawals, it should be stated in the article.
Based on the criteria above, the quality of a trial fell into one of the following three categories:
A ‐ Low risk of bias: all criteria met.
B ‐ Moderate risk of bias: One or more criteria partly met or if it was unclear if all the criteria were met.
C ‐ High risk of bias: One or more criteria not met.
Data extraction
Two review authors (Cui and Wang) independently extracted data from included trials using a piloted data extraction form. The following data were extracted from each included study: number of participants, age and sex distribution, comparability of groups at baseline, inclusion and exclusion criteria, type, frequency and duration of treatment of acupuncture therapy, type of control treatment, number of adverse events, duration of follow‐up and number and reasons for dropouts.
Extracted data were entered into RevMan by one review author (Cui) and then checked by another review author (Wang). Missing data were obtained from trialists whenever possible.
Data analysis
We carried out the statistical analyses using RevMan 4.2. Data were to be combined for meta‐analysis if individual trials were clinically homogeneous, otherwise a descriptive analysis was performed. We used relative risks (RR) with 95% confidence intervals (CI) for binary outcomes and weighted mean difference (WMD) with 95% CI for continuous variables. We used the chi‐square test for heterogeneity to assess statistical heterogeneity among trials. We pooled results using a fixed‐effect model in the absence of heterogeneity. We used a random‐effects model if heterogeneity was detected.
Subgroup analysis
We had pre‐specified the following subgroup analyses:
(1) different types of acupuncture therapies;
(2) different control interventions.
Sensitivity analysis
We planned to carry out sensitivity analyses to examine the effects of including only those studies with adequate allocation concealment or blinding of the outcome assessor.
Publication bias
We planned to investigate potential biases of publication using the funnel plot or other analytical methods, if sufficient trials were identified (Egger 1997).
Results
Description of studies
Fourteen potentially relevant trials were identified from the initial searches. All of them were from the published literature. Of these, two studies (Shi 2003; Zhou 2002) involving 170 patients in total met our inclusion criteria. Although there were no language restrictions, both included studies were published in Chinese.
Twelve trials were excluded for the following reasons:
(1) different forms of acupuncture were compared (Huang 1996; Tang 2003; Yang 1993);
(2) different acupoints were compared (Zhao 2005b);
(3) patients suffered from other psychiatric or organic disorders (Dai 2006; Gong 2004; Ma 2001);
(4) the four essential diagnostic criteria defined by IRLSSG were only partly met (Meng 2003; Zhang 2001);
(5) the non‐acupuncture treatment used in the experimental group was not used in the control group (Tan 2005; Wang 1999; Zhang 2006).
The included studies used different acupuncture therapies as well as different comparators. The rationale for the style of acupuncture used was stated in both trials. Participants in the first trial (Shi 2003) were diagnosed according to the criteria established by IRLSSG (Walters 1995). Participants in the second trial (Zhou 2002) were diagnosed according to a similar set of criteria stated in The Dictionary of Medical Syndromes (Lin 1994), which described all four clinical diagnostic criteria mandatory for RLS. The participants of both studies were outpatients with primary RLS. Both trials excluded participants with other disorders. A fixed protocol of acupuncture prescription was used for the participants in both trials.
In the first trial (Shi 2003), 120 patients were assigned, according to the entry sequence, into three groups to receive: (1) acupuncture plus fuming and washing with herbs, or (2) Western medications, or (3) acupuncture. However, the non‐acupuncture treatment (i.e. fuming and washing with herbs) used in Group 1 was not used in the other two groups, therefore, only Group 2 and Group 3 were eligible for comparison. Patients in Group 2 were treated with Western medications for 30 days consecutively. Patients in Group 3 were treated with a combination of body and scalp acupuncture. For body acupuncture, needles were inserted perpendicularly into acupoints ST36, GB34, SP10, BL56 and BL57. For scalp acupuncture, treatment zones consisted of MS5, the upper one fifth of MS7, and MS8. The needle was first inserted obliquely at an angle of 15 to 30 degrees with the scalp until its tip reached subgaleal level, and then inserted transversely. Manipulation techniques called 'even supplementation and drainage' were applied for both scalp and body acupuncture until the arrival of Qi had been achieved. The needles were retained for 30 minutes, during which the same manipulation techniques were applied twice. Acupuncture was administered daily over three treatment courses, each of which comprised of eight days in addition to a two‐day interval.
In the second trial (Zhou 2002), 90 patients were randomized to receive: (1) dermal needle therapy plus Western medications and self massage of legs, or (2) Western medications and self massage of legs. The dermal needle is made of seven short needles mounted onto the end of a plastic handle. The practitioner held the handle and tapped vertically with an interval of 1cm. The leg portions of four meridians, including the Stomach Meridian of Foot‐Yangming, the Spleen Meridian of Foot‐Taiyin, the Bladder Meridian of Foot‐Taiyang and the Kidney Meridian of Foot‐Shaoyin, were tapped three times. Both groups received treatment for 30 days consecutively.
The first trial (Shi 2003) described a follow‐up period of six months, however, only the outcome immediately after treatment was reported. The second trial (Zhou 2002) followed participants for one month, but the outcome measures used immediately after treatment were different from the outcome measures used in the follow‐up.
Ordinal outcomes immediately following treatment were reported by both studies. The first study (Shi 2003) used categories including 'cured', 'marked effective', 'improved', and 'no effect' to measure changes in overall symptoms. The second study (Zhou 2002) used 'cured', 'effective', and 'no effect' to measure changes in unpleasant sensations in the legs. Both ordinal scales were made into binary data by combining adjacent categories together. For the first study (Shi 2003), we combined 'cured', 'marked effective' and 'improved' into 'remission', and for the second study (Zhou 2002), we combined 'cured' and 'effective' into 'remission'.
The second study (Zhou 2002) also reported the means and standard deviations for four continuous outcomes: (1) unpleasant sensations of RLS measured by VAS (baseline and immediately after treatment); (2) the longest duration of RLS symptoms before and after the treatment (baseline and after one month); (3) the shortest duration of RLS symptoms before and after the treatment (baseline and after one month) ; (4) the frequency of RLS symptoms before and after the treatment (baseline and after one month).
Neither trial reported PLMS index, sleep disturbance, quality of life or adverse effects.
Risk of bias in included studies
Included trials were either inadequately reported or had methodological flaws. Neither of the trials mentioned a sample size calculation or any training of acupuncture practitioners. Neither trial stated the specific data collection period. Both trials claimed that baseline differences between groups were not significant. In the first trial (Shi 2003), patients were allocated according to their entry sequence, therefore, quasi‐randomized, and its approach to allocation concealment was apparently inadequate. The second trial (Zhou 2002) did not describe how the randomization was conducted, or report any concealment approach. Neither trial explicitly described the use of blinding. There was no statement on dropouts or withdrawals in either trial, and both trials analyzed outcome data from the same number of patients allocated. Therefore, both included studies were classified as category B for their methodological quality.
Effects of interventions
The included trials were extremely heterogeneous regarding acupuncture and control interventions. Therefore, pooling of data was not performed. Scalp and body acupuncture versus medications
In the first trial (Shi 2003), we only compared the outcome between Group 2 and Group 3, because Group 1 was not eligible for comparison. Interestingly, acupuncture alone was not significantly more effective than medications in remission of overall symptoms at the end of treatment (RR 0.97, 95% CI 0.76 to 1.24).
Dermal needle plus medications and massage versus medications and massage
In the second trial (Zhou 2002), acupuncture plus medications and massage was slightly more effective for relief of unpleasant sensations in the legs than medications and massage administrated alone. When remission of unpleasant sensations was analyzed as a dichotomous variable, the RR was 1.36 (95% CI 1.06 to 1.75) in favor of the dermal needle group. For the reduction in VAS score of unpleasant sensations, the WMD was ‐0.61 (95% CI ‐0.96 to ‐0.26), also in favor of the dermal needle group. There was no significant difference between the two groups for the reduction in either the longest or the shortest duration of RLS (WMD ‐2.58, 95% CI ‐5.92 to 0.76; WMD ‐0.38, 95% CI ‐1.08 to 0.32). However, there was a significant difference in favor of dermal needle therapy for the reduction in RLS frequency (WMD ‐3.44, 95% CI ‐5.15 to ‐1.73).
Neither trial reported the presence of harmful side effects.
We were unable to perform subgroup analysis, sensitivity analyses, or investigate potential biases of publication due to the lack of available studies.
Discussion
Despite the growing popularity of acupuncture around the world, there is still insufficient evidence to support the hypotheses that acupuncture is more effective in the treatment of RLS than no treatment or other therapies. Neither included trial reported data on side effects, but we still cannot guarantee the safety of acupuncture in treating RLS since the small sample sizes could have limited the power of detecting rare events.
This review is limited by the lack of well‐designed randomized controlled trials. Only two trials with 170 patients were included. The quality of reporting was rather disappointing and did not meet the standards in the CONSORT statement (Begg 1996) and STRICTA recommendations (MacPherson 2001). Although both studies mentioned the use of randomization, it was apparent that patients were quasi‐randomized in the first trial (Shi 2003), and it was uncertain whether or not the patients in the second trial (Zhou 2002) were genuinely randomized. The inadequacy of allocation concealment in the first trial (Shi 2003) and the possible lack of allocation concealment in the second trial (Zhou 2002) may have led to selection bias. The possible lack of blinding of the outcome assessors may have introduced detection bias in both trials.
Due to the clinical heterogeneity in terms of the type of acupuncture administered and the intervention of the control groups, no pooling of data was possible and it was difficult to draw conclusions for different types of acupuncture treatments.
In the first trial (Shi 2003), no significant difference was detected in remission of overall symptoms between acupuncture and medications. In the second trial (Zhou 2002), dermal needle therapy used in combination with medications and massage was demonstrated to be more effective than medications and massage alone, in terms of remission of unpleasant sensations in the legs and reduction of RLS frequency. This might suggest that some patients with RLS are more likely to benefit from dermal needle treatment for symptom management.
The results above should be interpreted with extreme caution because these comparisons involved only single studies. Additionally, both included trials enrolled small numbers of patients, which might have limited statistical power. The small sample sizes together with the wide confidence intervals also make it difficult to show a significant difference between acupuncture and control interventions should one exist. At the same time, it is necessary to point out that the ordinal outcomes of both included trials were poorly defined and based on subjective evaluations, thus it is likely that the results might have been overestimated as well.
Authors' conclusions
Implications for practice.
The belief that acupuncture is an effective treatment for RLS is not based on rigorous and comprehensive evidence. The hypotheses need to be validated by further high quality research before the routine use of acupuncture can be recommended for patients suffering from RLS.
Implications for research.
Further high quality research is warranted to evaluate the efficacy and safety of acupuncture in the treatment of RLS. Here are some suggestions for future studies:
(1) statistical method of sample size calculations with at least 80% power of detecting a difference of clinical importance on a chosen outcome measure should be conducted to determine the minimum number of patients required;
(2) the method of randomization and allocation concealment should be rigorous and fully described to encourage confidence in the control of selection bias;
(3) although blinding of acupuncture practitioners is very unlikely, blinding of participants and outcome assessors should be attempted in order to minimize performance and detection biases;
(4) more sensitive and valid clinical outcomes such as PLMS index and quality of life should be used;
(5) a longer follow‐up period is recommended to determine the long‐term effects of acupuncture in the treatment of RLS;
(6) adverse effects of acupuncture should be critically assessed and reported; and
(7) it might also be worthwhile to examine the effectiveness of non‐invasive acupressure therapy for RLS.
What's new
| Date | Event | Description |
|---|---|---|
| 30 May 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 2, 2007 Review first published: Issue 4, 2008
| Date | Event | Description |
|---|---|---|
| 30 May 2008 | Amended | Substantive amendment |
Acknowledgements
We would like to acknowledge the helpful comments of the panel of experts who refereed the review. We are grateful to Ema Roque, Movement Disorders Review Group Coordinator. We would also like to thank Liu Jie and Dr. Zhang Wei for their assistance in the preparation of the review.
Data and analyses
Comparison 1. Acupuncture versus no acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reduction in VAS score of unpleasant sensations | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Symptom remission | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Scalp and body acupuncture versus medications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Dermal needle plus medications and massage versus medications and massage | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Reduction in RLS duration | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Longest duration | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Shortest duration | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Reduction in RLS frequency | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
1.1. Analysis.
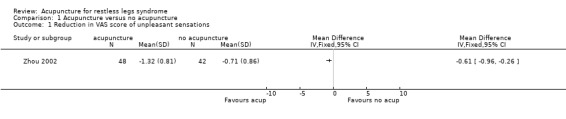
Comparison 1 Acupuncture versus no acupuncture, Outcome 1 Reduction in VAS score of unpleasant sensations.
1.2. Analysis.

Comparison 1 Acupuncture versus no acupuncture, Outcome 2 Symptom remission.
1.3. Analysis.
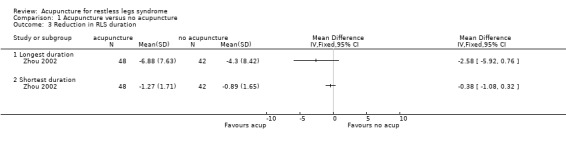
Comparison 1 Acupuncture versus no acupuncture, Outcome 3 Reduction in RLS duration.
1.4. Analysis.
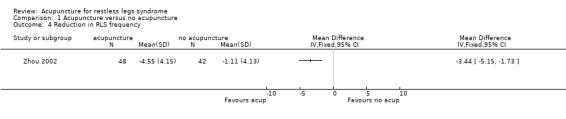
Comparison 1 Acupuncture versus no acupuncture, Outcome 4 Reduction in RLS frequency.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Shi 2003.
| Methods | Quasi‐randomized trial. Patients were allocated according to the entry sequence. Blinding: The patients and acupuncture practitioners could not be blinded and it was unclear if the outcome assessors were blinded. Dropout/withdrawals: no statement. |
|
| Participants | Setting: Hospital outpatient, China. Demographics: aged 30 to 69 yrs; 64 male, 56 female. Baseline comparability: Yes. Diagnosis: Patients with primary RLS diagnosed according to the criteria established by IRLSSG. Number of patients: 120 (40/40/40). |
|
| Interventions | 3 arms: Group 1: scalp and body acupuncture plus fuming and washing with herbs. Group 2: oryzanol 20mg three times a day plus diazepam 5mg before bedtime. Group 3: scalp and body acupuncture. Comparison eligible: scalp and body acupuncture versus oryzanol and diazepam. Acupuncture treatment: (1) Acupuncture rationale: traditional Chinese medical theories and modern theories of cerebral cortical function. (2) Needle type: sterilised stainless steel, body acupuncture: 50 mm in length and 0.30 mm in diameter, 75 mm in length and 0.30 mm in diameter; scalp acupuncture: 50 mm in length and 0.35 mm in diameter. (3) Acupuncture prescriptions: body acupoints: ST36, GB34, SP10, BL56 and BL57; scalp treatment zones: MS5 (from GV20 to GV21), the upper 1/5th of MS7 (from GV20 to GB7) and MS8 (extending for 1.5 Cun from BL7 along the Bladder Meridian of Foot‐Taiyang). (4) Depth of needle insertion: body acupuncture: 40 mm to 62.5 mm; scalp acupuncture: 40 mm. |
|
| Outcomes | Only one outcome reported: Ordinal outcome (immediately following treatment): (a) Cured: disappearance of all symptoms; Group 1: 27/40, Group 2: 18/40, Group 3: 19/40. (b) Marked effective: most of the symptoms disappeared and sleep was occasionally disturbed by unpleasant sensations and the urge to move the legs; Group 1: 8/40, Group 2: 6/40, Group 3: 6/40. (c) Improved: symptoms were partially relieved, but sleep was often disturbed by unpleasant sensations and the urge to move the legs; Group 1: 4/40, Group 2: 7/40, Group 3: 5/40. (d) No effect: symptoms were unchanged after treatment. Group 1: 1/40, Group 2: 9/40, Group 3: 10/40. |
|
| Notes | Author's conclusion: Acupuncture plus fuming was significantly better than Western medications or acupuncture. No significant difference was detected between Western medications and acupuncture alone. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Zhou 2002.
| Methods | Randomized controlled trial. No details could be obtained from the author on how the allocation sequence was generated. Blinding: The patients and acupuncture practitioners could not be blinded and it was unclear if the outcome assessors were blinded. Dropout/withdrawals: no statement. |
|
| Participants | Setting: Hospital outpatient, China. Demographics: aged 27 to 52 yrs; 47 male, 43 female. Baseline comparability: Yes. Diagnosis: Patients with primary RLS diagnosed according to the criteria stated in The Dictionary of Medical Syndromes, which described all four clinical diagnostic criteria mandatory for RLS. Number of patients: 90 (48/42). |
|
| Interventions | Group 1: dermal needle therapy. Group 2: no acupuncture. Both groups: dipyridamole 50mg three times a day + nicotinic acid 50mg three times a day + inositol 1g before bedtime + self massage of legs before bedtime. Acupuncture treatment: (1) Acupuncture rationale: traditional Chinese medical theories and modern theories of neurology. (2) Needle type: Dermal needle is made of seven short stainless needles mounted onto the end of a plastic handle. (3) Acupuncture prescriptions: The leg portions of four meridians (the Stomach Meridian of Foot‐Yangming, the Spleen Meridian of Foot‐Taiyin, the Bladder Meridian of Foot‐Taiyang and the Kidney Meridian of Foot‐Shaoyin) were tapped vertically with an interval of 1cm. (4) Depth of needle insertion: the dermal needle was tapped superficially on the skin until slight bleeding appeared. |
|
| Outcomes | Five outcomes reported: 1. Ordinal outcome (immediately following treatment): (a) Cured: disappearance of unpleasant sensations in the legs; Group 1: 26/48, Group 2: 15/42. (b) Effective: the unpleasant sensations were considerably relieved; Group 1: 16/48, Group 2: 12/42. (c) No effect: the unpleasant sensations were unchanged after treatment. Group 1: 6/48, Group 2: 15/42. 2. Unpleasant sensations of RLS measured by VAS. Baseline: Group 1: 8.86 ± 0.93, Group 2: 8.79 ± 0.95; Immediately following treatment: Group 1: 7.54 ± 0.56, Group 2: 8.08 ± 0.73. 3. The longest duration of RLS symptoms in one month before and after the treatment. Baseline: Group 1: 30.59 ± 8.74, Group 2: 31.15 ± 9.30; After one month: Group 1: 23.71 ± 5.30, Group 2: 26.85 ± 7.12. 4. The shortest duration of RLS symptoms in one month before and after the treatment. Baseline: Group 1: 6.84 ± 1.95, Group 2: 6.72 ± 1.88; After one month: Group 1: 5.57 ± 1.26, Group 2: 5.83 ± 1.20. 5. The frequency of RLS symptoms in one month before and after the treatment. Baseline: Group 1: 15.24 ± 4.79, Group 2: 14.65 ± 4.24; After one month: Group 1: 10.69 ± 2.57, Group 2: 13.54 ± 4.02. |
|
| Notes | Author's conclusion: Acupuncture was significantly better. We calculated the changes from baseline for the four continuous outcomes. The mean changes were obtained by subtracting the final means from the baseline means. We imputed the standard deviations for the change scores of both the experimental and control group by using an imputed correlation coefficient of 0.5. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Explanations for the two terms used in the description of the first trial (Shi 2003):
Manipulation techniques called 'even supplementation and drainage' include lifting and thrusting of the needle performed with even lifts and thrusts and/or rotation performed with even strength in both directions with a medium arc.
The arrival of Qi (De Qi in Chinese) means a sensation of soreness, numbness, distention or heaviness around the point.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Dai 2006 | All subjects had experienced cerebrovascular diseases. |
| Gong 2004 | Subjects suffered from various psychiatric and organic disorders. |
| Huang 1996 | Different forms of acupuncture were compared. |
| Ma 2001 | All subjects suffered from type 2 diabetes mellitus (DM). |
| Meng 2003 | The four essential diagnostic criteria defined by IRLSSG were only partly met. |
| Tan 2005 | Electro‐acupuncture plus massage were compared with Western medications. |
| Tang 2003 | Different forms of acupuncture were compared. |
| Wang 1999 | Acupressure plus massage and herbs fumigation were compared with Western medications. |
| Yang 1993 | Different forms of acupuncture were compared. |
| Zhang 2001 | The four essential diagnostic criteria defined by IRLSSG were only partly met. |
| Zhang 2006 | Herbs plus acupoint injection of Vitamin B12 were compared with estazolam plus intramuscular injection of Vitamin B1 and Vitamin B12. |
| Zhao 2005b | Effects of different acupoints were compared. |
Contributions of authors
Ye Cui wrote the protocol and was responsible for study identification, methodological quality assessment, data extraction and data analysis.
Yin Wang contributed to protocol development, study identification, quality assessment and data extraction.
Zhishun Liu contributed to protocol development and worked as the arbitrator in the process of study selection and quality assessment.
Sources of support
Internal sources
Department of Acupuncture and Moxibustion, Guang An Men Hospital, The China Academy of Chinese Medicine Science, China.
Beijing University of Chinese Medicine, China.
External sources
No sources of support supplied
Declarations of interest
None known.
Edited (no change to conclusions)
References
References to studies included in this review
Shi 2003 {published data only}
- Shi YL, Wang YM. Observation on therapeutic effects of acupuncture plus steaming washing with Chinese herbs for treatment of 40 cases of restless legs syndrome. Chinese Acupuncture & Moxibustion 2003;23(11):651‐2. [Google Scholar]
Zhou 2002 {published data only}
- Zhou GY. Treatment of 48 cases of restless legs syndrome with dermal needle therapy. Chinese Journal of Information on TCM 2002;9(10):63‐4. [Google Scholar]
References to studies excluded from this review
Dai 2006 {published data only}
- Dai XY, Li Y, Song QZ, Han BJ. Observation on the efficacy of Biguan warming acupuncture for treating post‐apoplectic restless legs syndrome. Shanghai Journal of Acupuncture and Moxibustion 2006;25(1):23‐4. [Google Scholar]
Gong 2004 {published data only}
- Gong CL, Zhang AQ. Treatment of 20 cases of restless legs syndrome with acupoint injection. Modern Journal of Integrated Traditional Chinese and Western Medicine 2004;13(8):1036. [Google Scholar]
Huang 1996 {published data only}
- Huang W, Liu XQ. Treatment of restless legs syndrome with scalp acupuncture and warming acupuncture. Journal of Guiyang College of Traditional Chinese Medicine 1996;18(4):34‐5. [Google Scholar]
Ma 2001 {published data only}
- Ma HX. Treatment of restless legs syndrome with acupuncture and herbs in patients with diabetes mellitus. Journal of Shanxi College of Traditional Chinese Medicine 2001;2(2):42‐3. [Google Scholar]
Meng 2003 {published data only}
- Meng XH. Treatment of 24 cases of restless legs syndrome with compound salvia acupoint injection. Guangxi Journal of Traditional Chinese Medicine 2003;26(1):24‐5. [Google Scholar]
Tan 2005 {published data only}
- Tan JY. Treatment of 38 cases of restless legs syndrome with electroacupuncture and massage. Journal of Practical Traditional Chinese Medicine 2005;21(10):617. [Google Scholar]
Tang 2003 {published data only}
- Tang SX, Xu ZH, Tang P. Clinical study on treating restless legs syndrome by acupuncture. Chinese Journal of the Practical Chinese with Modern Medicine 2003;3(16):1430. [Google Scholar]
Wang 1999 {published data only}
- Wang DJ, Wu ZY. Treatment of 40 cases of restless legs syndrome with massage and herbs fumigation. Journal of Practical Traditional Chinese Medicine 1999;15(8):8‐9. [Google Scholar]
Yang 1993 {published data only}
- Yang YD. Treatment of 108 cases of restless legs syndrome with body and ear acupuncture. Chinese Acupuncture & Moxibustion 1993, (3):13‐4. [Google Scholar]
Zhang 2001 {published data only}
- Zhang ZY. Treatment of 32 cases of restless legs syndrome with acupuncture. Journal of Fujian College of TCM 2001;11(2):32. [Google Scholar]
Zhang 2006 {published data only}
- Zhang H. Treatment of restless legs syndrome with acupoint injection and herbs. Hubei Journal of Traditional Chinese Medicine 2006;28(8):47‐8. [Google Scholar]
Zhao 2005b {published data only}
- Zhao W, Wang DH, Yang RK, Zhou H. Comparison of therapeutic effects of acupoints selected along different meridians on restless legs syndrome. Chinese Acupuncture & Moxibustion 2005;25(9):616‐8. [PubMed] [Google Scholar]
Additional references
Allen 1998
- Allen RP, Earley CJ, Hening WA, Walters AS, Yaffee J, Wagner ML. Pergolide treatment of the restless legs syndrome: A double‐blind placebo‐controlled study with objective assessment of leg movements. Neurology 1998;50(4) (Suppl 4):A68‐9. [Google Scholar]
Allen 2001
- Allen RP, Barker PB, Wehrl F, Song HK, Earley CJ. MRI measurement of brain iron in patients with restless legs syndrome. Neurology 2001;56:263‐5. [DOI] [PubMed] [Google Scholar]
Allen 2003
- Allen RP, Picchietti D, Hening W, Trenkwalder C, Walters AS, Montplaisir J, et al. Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology: a report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Medicine 2003;4:101‐19. [DOI] [PubMed] [Google Scholar]
Allen 2005
- Allen RP, Walters AS, Montplaisir J, Hening W, Myers A, Bell TJ, et al. Restless legs syndrome prevalence and impact: REST general population study. Archives of Internal Medicine 2005;165(11):1286‐92. [DOI] [PubMed] [Google Scholar]
Begg 1996
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials: The CONSORT statement. JAMA 1996;276(8):637‐9. [DOI] [PubMed] [Google Scholar]
Bogan 2006
- Bogan RK, Fry JM, Schmidt MH, Carson SW, Ritchie SY, for the TREAT RLS US (Therapy with Ropinirole Efficacy And Tolerability in RLS US) Study Group. Ropinirole in the treatment of patients with restless legs syndrome: A US‐based randomized, double‐blind, placebo‐controlled clinical trial. Mayo Clinic Proceedings 2006;81(1):17‐27. [DOI] [PubMed] [Google Scholar]
Brodeur 1988
- Brodeur C, Montplaisir J, Godbout R, Marinier R. Treatment of restless legs syndrome and periodic movements during sleep with L‐dopa: a double‐blind, controlled study. Neurology 1988;38:1845‐8. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekbom 1945
- Ekbom KA. Restless legs. Acta medica Scandinavica 1945;158:5‐122. [DOI] [PubMed] [Google Scholar]
Green 2006
- Green S, Buchbinder R, Barnsley L, Hall S, White M, Smidt N, et al. Acupuncture for lateral elbow pain. The Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrison's 2001
- Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's Principles of Internal Medicine. 15th Edition. The McGraw‐Hill Companies, Inc, 2001. [Google Scholar]
Higgins 2005
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. In: The Cochrane Library [database on CDROM]. The Cochrane Collaboration, Chichester, UK: John Wiley & Sons Ltd; 2005, Issue 3.
Hogl 2005a
- Hogl B, Kiechl S, Willeit J, Saletu M, Frauscher B, Seppi KM, et al. Restless legs syndrome: A community‐based study of prevalence, severity, and risk factors. Neurology 2005;64(11):1920‐4. [DOI] [PubMed] [Google Scholar]
Hogl 2005b
- Hogl B, Poewe W. Restless legs syndrome. Current Opinion in Neurology 2005;18(4):405‐10. [DOI] [PubMed] [Google Scholar]
Hornyak 2006
- Hornyak M, Berner MM, Kriston L, Riemann D. Dopamine agonists for restless legs syndrome. The Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Controlled Clinical Trials 1996;17:1‐12. [DOI] [PubMed] [Google Scholar]
Kjaergard 2001
- Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta‐analyses. Annals of Internal Medicine 2001;135(11):982‐9. [DOI] [PubMed] [Google Scholar]
Lin 1994
- Lin LR, Lin WT, Yu MS, editors. The Dictionary of Medical Syndromes. 1st Edition. China Science and Technology Publishing House, 1994. [Google Scholar]
Lin 1998
- Lin SC, Kaplan J, Burger CD, Fredrickson PA. Effect of pramipexole in treatment of resistant restless legs syndrome. Mayo Clinic Proceedings 1998;73(6):497‐500. [DOI] [PubMed] [Google Scholar]
MacPherson 2001
- MacPherson H, White A, Cummings M, Jobst K, Rose K, Niemtzow R. Standards for reporting interventions in controlled trials of acupuncture: the STRICTA recommendations. Complementary Therapies in Medicine 2001;9(4):246‐9. [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad A, Moher M, et al. Does quality of reports of randomized trials affect estimates of intervention efficacy reported in meta‐analysis. Lancet 1998;352:609‐13. [DOI] [PubMed] [Google Scholar]
Montplaisir 1999
- Montplaisir J, Nicolas A, Denesle R, Gomez‐Mancilla B. Restless legs syndrome improved by pramipexole: A double‐blind randomized trial. Neurology 1999;52(5):938‐43. [DOI] [PubMed] [Google Scholar]
NINDS 2006
- National Institute of Neurological Disorders and Stroke. Restless Legs Syndrome Fact Sheet. http://www.ninds.nih.gov/disorders/restless_legs/detail_restless_legs.htm (accessed 3 September 2006).
Qiao 1997
- Qiao HJ, Zhang LC. Treatment of restless legs syndrome with herbs and plum‐blossom needle. Henan Traditional Chinese Medicine 1997;17(1):57. [Google Scholar]
Schapira 2004
- Schapira AHV. Restless legs syndrome: An update on treatment options. Drugs 2004;64(2):149‐58. [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Silber 2004
- Silber MH, Ehrenberg BL, Allen RP, Buchfuhrer MJ, Earley CJ, Hening WA, et al. for the Medical Advisory Board of the Restless Legs Syndrome Foundation. An algorithm for the management of restless legs syndrome. Mayo Clinic Proceedings 2004;79(7):916‐22. [DOI] [PubMed] [Google Scholar]
Smith 2006
- Smith CA, Hay PPJ. Acupuncture for depression. The Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI] [PubMed] [Google Scholar]
Song 2004
- Song BL, Pang XZ. Treatment of 37 cases of restless legs syndrome by puncturing BL57 exclusively. Hebei Journal of Traditional Chinese Medicine 2004;26(8):618. [Google Scholar]
Sun 2002
- Sun ZT, Chen M. Treatment of 68 cases of restless legs syndrome by acupoint injection therapy. Henan Traditional Chinese Medicine 2002;22(6):43‐4. [Google Scholar]
Tan 2001
- Tan EK, Seah A, See SJ, Lim E, Wong MC. Restless legs syndrome in an Asian population: a study in Singapore. Movement Disorders 2001;16:577‐8. [DOI] [PubMed] [Google Scholar]
Tison 2005
- Tison F, Crochard A, Leger D, Bousee S, Lainey E, Hasnaoui A. Epidemiology of restless legs syndrome in French adults: A national survey: The INSTANT Study. Neurology 2005;65(2):239‐46. [DOI] [PubMed] [Google Scholar]
Trenkwalder 2005
- Trenkwalder C, Paulus W, Walters AS. The restless legs syndrome. The Lancet Neurology 2005;4:465‐75. [DOI] [PubMed] [Google Scholar]
Walters 1988
- Walters AS, Hening WA, Kavey N, Chokroverty S, Gidro‐Frank S. A double‐blind randomized crossover trial of bromocriptine and placebo in restless legs syndrome. Annals of Neurology 1988;24(3):455‐8. [DOI] [PubMed] [Google Scholar]
Walters 1995
- Walters AS. The International Restless Legs Syndrome Study Group. Toward a better definition of restless legs syndrome. Movement Disorders 1995;10:634‐42. [DOI] [PubMed] [Google Scholar]
Wang 1994
- Wang DY. Treatment of 30 cases of restless legs syndrome with electro‐acupuncture. Journal of Gansu College of Traditional Chinese Medicine 1994;11(1):46. [Google Scholar]
Wang 2001
- Wang CX. Recent developments in TCM treatment of restless legs syndrome. Shandong Journal of Traditional Chinese Medicine 2001;20(7):443‐4. [Google Scholar]
Wang 2005
- Wang JZ, Zhou JD. Treatment of restless legs syndrome with manipulation and acupoint injection therapy. Chinese Manipulation & Qi Gong therapy 2005;21(5):40. [Google Scholar]
Wen 2000
- Wen XL. Treatment of 75 cases of restless legs syndrome with body acupuncture and auricular acupuncture. Chinese Journal of Traditional Medical Science and Technology 2000;7(4):264. [Google Scholar]
Wong 2006
- Wong KK, Dobbin CJ, Joffe D, March L. Interventions for dialysis‐associated restless legs syndrome. The Cochrane Database of Systematic Reviews 2006, Issue 2. [Google Scholar]
Yang 1997
- Yang JS, Zhang J, Chen ZF, He SH, editors. Acupuncture and Moxibustion. People's Medical Publishing House, 1997. [Google Scholar]
Zhao 2005a
- Zhao W. Treatment of restless legs syndrome with manipulation and acupuncture. China Journal of Orthopaedics and Traumatology 2005;18(8):506. [Google Scholar]


