ABSTRACT
Young adults experience high coronavirus disease 2019 (COVID-19) incidence yet have the lowest vaccination and booster rates among adults. Understanding the factors influencing their intentions regarding boosters is essential for crafting effective public health strategies. We examined the psychosocial factors (attitudes, norms, perceived behavioral control) associated with their intentions to receive a COVID-19 booster. This cross-sectional study included 292 young adults aged 18–25 residing in Philadelphia who completed an online survey from September 2021 and February 2022 (mean age 21.98, standard deviation 2.25; 51% racial/ethnic minorities). The survey included measures of attitudes, norms, and perceived behavioral control related to COVID-19 vaccination. We employed structural equation modeling analysis to examine the intention of young adults to receive the COVID-19 booster and their vaccine-related attitudes, norms, and perceived behavioral control. Covariates included race/ethnicity and gender. Subjective norms were significantly associated with the intention to receive a COVID-19 booster (standardized β̂ = 0.685, p = .018). Attitudes and perceived behavioral control showed no significant association with intention. Subgroup analyses based on race/ethnicity revealed that attitudes (standardized β̂ = 0.488, p = .004) and subjective norms (standardized β̂ = 0.451, p = .050) were predictors among young adults from racial and ethnic minority backgrounds, while only subjective norms (standardized β̂ = 1.104, p = .002) were significant for non-Hispanic White young adults. Public health efforts should prioritize engaging healthcare providers and peer groups in order to influence subjective norms and promote collective responsibility and acceptance for vaccination. Tailored interventions and diverse communication strategies targeting specific subgroups of young adults may be useful to ensure comprehensive and effective vaccination initiatives.
KEYWORDS: Emerging adult, young adult, theory of planned behavior, vaccine hesitancy, COVID-19, booster vaccine
Introduction
The coronavirus disease 2019 (COVID-19) pandemic that emerged in late 2019 has posed an unprecedented global challenge to public health.1–3 In the United States (U.S.), as in many parts of the world, efforts to combat the spread of the virus have included widespread vaccination campaigns.4 These campaigns have been instrumental in curbing the initial wave of infections, reducing complications from infection, and reducing the burden on healthcare systems. While COVID-19 is no longer classified as a public health emergency of international concern,5 a key strategy for maintaining immunity and controlling the virus’s spread involved administering initial and booster doses of COVID-19 vaccines.6
As of October 2023, young adults in the U.S., particularly those aged 18 to 24, exhibited the lowest vaccination rates, including for booster shots, compared to other adult populations aged older than 24.7 Moreover, young adults aged 18 to 29 had the highest COVID-19 incidence rates among all adult groups, rendering this age group a significant contributor to ongoing community transmission.8,9 This population was also considered a primary contributor to the resurgence of COVID-19 in the U.S. in 2020.10 Many young adults perceive themselves as less likely to experience the negative effects of COVID-19, which resulted in poorer adherence to mitigation strategies.11 Since their symptoms are often mild, they may be less inclined to isolate, thereby increasing the likelihood of unknowingly transmitting the virus.12 As young adults often interact with a wide range of individuals across diverse age groups, including high-risk individuals such as elderly relatives, understanding their intentions regarding COVID-19 boosters is essential for crafting effective public health strategies.
The decision to obtain a COVID-19 vaccination booster is influenced by a complex interplay of factors.13 The Theory of Planned Behavior (TPB) provides a valuable lens through which to understand and predict human behavior, particularly in the context of health-related decisions. According to the TPB, three main factors influence behavioral intentions: (1) an individual’s positive or negative perception and assessment of a specific behavior (attitudes toward behavior), (2) the perceived social pressure to engage or not engage in the behavior (subjective norms), and (3) the perceived ease or difficulty of carrying out the behavior (perceived behavioral control). Together, these elements shape an individual’s intention to perform a particular behavior and are crucial determinants of actual behavior.14
TPB has been successfully applied to numerous health-related behaviors including vaccination decisions and has yielded valuable insights into the factors that drive or hinder people’s intentions to engage in these behaviors.13 Table 1 summarizes findings from previous studies that utilized the TPB to investigate intentions to receive COVID-19 boosters across various countries and populations. Most studies included adults of all ages, highlighting a scarcity of studies specifically addressing intentions to receive boosters tailored for young adults. Two studies focused on young adults and included only college students.22,26 Some studies incorporated all three TPB constructs, while others included only a subset. Of the two studies focusing on young adults, one involving interdisciplinary college students included all three TPB constructs, with attitudes and subjective norms found to be significant predictors.22 The other study, which involved only medical students, included attitudes as the sole construct, and it was also found to be a significant predictor.26
Table 1.
Studies applying the TPB to examine COVID-19 booster intention.
| Authors (Years) | Country (Region) |
Sample | N | Included TPB Constructs | Other Predictors | Key TPB Findings |
|---|---|---|---|---|---|---|
| Almokdad et al. (2023)15 | South Korea | All adults (Mean age: 28.46) | 315 | ATT, SN, PBC | Universalism, benevolence, conformity, tradition, security, herd immunity awareness, ascribed responsibility | ATT, SN and PBC were found to be associated with COVID-19 booster intention. |
| Barattucci et al. (2022)16 | Italy | All adults (Mean age: 40.06 ± 13.8) | 1,095 | SN | Gender, age, education, fear of the vaccine, fear of COVID-19, trust in science, trust in vaccine, COVID-19 knowledge, vulnerability, and severity | SN was found to be associated with COVID-19 booster intention. |
| Catalano et al. (2023)17 | USA (southeastern region) | All adults (Age 18, mean age not reported) | 288 | ATT, SN, PBC | ATT and SN were found to be associated with COVID-19 booster intention. | |
| Geers et al. (2022)18 | USA (national sample) | All adults (Mean age: 31.66 ± 11.05) | 551 | ATT | Trust in development, COVID-19 worry, side effect concern, political affiliation | ATT was found to be associated with COVID-19 booster intention. |
| Folcarelli et al. (2022)19 | Italy | All adults (Mean age: 32.1 ± 15.9) | 615 | ATT | Perceived risk of COVID-19 infection, booster dose hesitancy, gender, age, marital status, cohabitants, education, student status, chronic conditions, COVID-19 history, friends/family diagnosed, self-rated health (global and post-vaccine), received official information, need for more information on the booster | ATT was found to be associated with COVID-19 booster intention. |
| Hagger and Hamilton (2022)20 | USA (region not reported) | All adults (Mean age: 52.14 ± 14.55) | 479 | ATT, SN, PBC | Political orientation, vaccine hesitancy, belief in free will, age, sex, education level, employment status, ethnicity, previous COVID-19 diagnosis, previous influenza vaccine | ATT, SN and PBC were found to be associated with COVID-19 booster intention. |
| Hwang et al. (2024)21 | Malaysia | All adults (Age 18, mean age not reported) | 1,914 | ATT, SN | Age, income, gender, education, employment status, marital status, previous COVID-19 infection, region, satisfaction, perceived usefulness, perceived barriers, perceived benefits, cues to action | ATT and SN were found to be associated with COVID-19 booster intention. |
| Liu et al. (2024)22 | USA (midwestern region) | Young adults (College students with a mean age of 20.27 ± 2.75) | 419 | ATT, SN, PBC | Age, sex, race, ethnicity, chronic conditions, smoking, financial status, parent education, health insurance, vaccination history | ATT and SN were found to be associated with COVID-19 booster intention. |
| Lounis et al. (2022)23 | Algeria | All adults (Age 18, mean age not reported) | 787 | ATT | Sex, age, education, profession, chronic illness, previous COVID-19 infection, post-vaccination relief, regret | ATT was found to be associated with COVID-19 booster intention. |
| Maria et al. (2022)24 | Indonesia | All adults (Age 18, mean age not reported) | 1,684 | ATT, SN, PBC | Education, income, comorbidity, previous COVID-19 infection, perceived barriers, perceived severity, perceived benefits, perceived susceptibility, anticipated regret, self-efficacy | ATT and SN were found to be associated with COVID-19 booster intention. |
| Orellana et al. (2023)25 | Bolivia | All adults (Mean age: 26.61 ± 13.11) | 720 | ATT, SN | Vaccine origin, completed minimum required doses, received third dose, information sources (government authorities, scientific), confidence in COVID-19 vaccines, confidence in previous vaccines, time since last dose, biosafety norms | ATT and SN were found to be associated with COVID-19 booster intention. |
| Sugawara et al. (2021)26 | Japan | Young adults (Medical students with a mean age of 21.1 ± 2.5) | 496 | ATT | Age, sex, grade, allergy history (food, medication, animals, pollen, dust mites, unknown), anaphylaxis, asthma, atopic dermatitis | ATT was found to be associated with COVID-19 booster intention. |
| Wang et al. (2022)27 | China (Hong Kong) | Older adults (Age 65) | 395 | ATT, SN | Education, pneumococcal vaccination history, uncertainty, materials addressing COVID-19 booster concerns, materials helpful for booster decision | Neither ATT nor SN was found to be associated with COVID-19 booster intention. |
| Wang et al. (2023)28 | China (Nanjing) | Older adults (Age 60) | 214 | ATT, SN | Perceived severity, perceived vulnerability, response efficacy, self-efficacy, response cost | SN was found to be associated with COVID-19 booster intention. |
| Wong et al. (2022)29 | Malaysia | All adults (Mean age: 32.1 ± 11.3) |
1,010 | ATT | Age, gender, ethnicity, marital status, occupation, income, living area, chronic condition, COVID-19 history, past COVID-19 vaccination side effects, pandemic fatigue, adherence to recommended COVID-19 measures | ATT was found to be associated with COVID-19 booster intention. |
| Xiang et al. (2023)30 | China (Macao) | All adults (Age 18, mean age not reported) | 469 | ATT | Psychological reactance, perceived threat to freedom, message frame, freedom restoration postscript, other-referencing cue, age, education, income | ATT was found to be associated with COVID-19 booster intention. |
| Zhou et al. (2022)31 | China (Nanjing) | Adult parents (Median age: 32, SD not reported) | 1,602 | ATT, SN, PBC | Belief in problem severity, perceived risk of disease, assessment of protection behavior effectiveness, self-efficacy in implementing behavior, and estimated cost of action | ATT, SN and PBC were found to be associated with COVID-19 booster intention. |
Abbreviations: ATT (attitudes), SN (subjective norms), PBC (perceived behavioral control), COVID-19 (coronavirus disease 2019).
Studies on other respiratory vaccines in young adults present inconsistent findings. For example, a study involving U.S. college students found that subjective norms predicted their intention to receive the COVID-19 primary series, while attitudes and perceived behavioral control did not.32 Moreover, in two U.S. studies applying the TPB to investigate young adults’ intentions regarding influenza vaccines, one study focused on those who had not received a flu shot. It found that attitudes, subjective norms, and perceived behavioral control were all significant predictors.33 Conversely, another study examining influenza vaccination intentions among young adults found that attitudes and subjective norms were significantly associated with intentions, while perceived behavioral control did not play a significant role.34
In this context, we employed the TPB as the foundational framework to investigate the intentions of a diverse sample of young adults in Philadelphia regarding receiving COVID-19 booster shots. Our aim is to uncover the underlying factors influencing these intentions, encompassing an examination of attitudes, perceived behavioral control, and subjective norms. While several instruments based on TPB exist to assess intentions across various populations, the unique context of the COVID-19 pandemic and the introduction of booster vaccinations necessitated the development of a new TPB-based instrument tailored to the young adult population. Existing instruments may not fully capture the specific factors influencing young adults’ intentions to receive a COVID-19 booster, including their unique perceptions, diverse social influences, and beliefs about control. Additionally, the unprecedented nature of the pandemic and the cultural and regional specificities of our target population demanded a contextually relevant tool. Therefore, we developed a new TPB instrument to comprehensively and accurately assess the determinants of young adults’ behavioral intentions in this novel and specific context, seeking insights into how these constructs impact their decision-making process.
Our hypotheses are:
Consistent with the TPB, we hypothesized that there will be a direct and positive association between the intention to receive the COVID-19 booster and the following constructs within the young adult populations: (a) attitudes toward COVID-19 vaccination; (b) subjective norms; and (c) perceived behavioral control.
Given reported differences in vaccine-related attitudes and uptake by race/ethnicity,35–37 we hypothesized that there will be a difference in these associations between non-Hispanic White young adults and young adults from other racial/ethnic groups.
Methods
This cross-sectional study is a component of the larger Philadelphia CEAL (Community Engagement Alliance) initiative,38,39 which aimed to address disparities in COVID-19 testing, vaccine uptake, and participation in clinical trials within communities disproportionately impacted by the pandemic in Philadelphia. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement40 was used to ensure proper reporting of this observational study.
Participants
In the present study, eligibility criteria included participants who had completed the full primary series of the COVID-19 vaccine, consistent with our outcome of intending to receive a booster shot. The series could be either two doses of Moderna/Pfizer-BioNTech or one dose of Johnson & Johnson’s Janssen. Additionally, we restricted the age to 18 years or older to maintain consistency with young adult populations.41
We initially recruited 359 residents of Philadelphia without any dependent children via online and community-based outreach to participate in a self-administered online survey conducted through Qualtrics from September 2021 to February 2022.39 During data collection, Philadelphia’s young adult population exhibited diversity across ethnicity, race, culture, and socioeconomic background.42 COVID-19 booster shots became available starting in September 2021. Among the initial pool, we excluded 34 individuals who did not complete the full primary series of the COVID-19 vaccine. We also excluded an additional 24 participants who were younger than 18. Furthermore, nine participants who did not respond to any of the survey items used in the present study were excluded. As a result, the final dataset included 292 young adult participants. All study procedures received approval from the Institutional Review Board at the University of Pennsylvania (#848650). Written informed consent was obtained from all participants after fully explaining the nature and potential consequences of the study.
Measures
TPB constructs
The questionnaire related to COVID-19 vaccines was designed specifically for this study by researchers based on TPB and adhered to TPB questionnaire construction, measurement, and elicitation guidelines.14,43,44 The items were developed to encompass the core constructs of TPB, which included (1) intention, (2) attitudes, (3) perceived behavioral control, and (4) subjective norms. Adaptation was required for subjective norms questions to specify the relevant individuals important to young adults, with choices informed by existing literature.45,46 The questionnaire featured positively framed items, including nine items for attitudes, eight items for subjective norms, and eight items for perceived behavioral control. Respondents provided their feedback on a five-point Likert scale, ranging from ‘1 = disagree strongly’ to ‘5 = agree strongly.’ Higher scores on the items related to attitudes, subjective norms, and perceived behavioral control indicated more positive cognitive responses from the participants. Given the time-sensitive nature of the pandemic and the need to swiftly collect data, conducting a pilot study was not feasible. However, the questionnaire items were carefully developed based on established constructs from the TPB. Moreover, they were subjected to rigorous review by field experts to ensure content validity.47
Vaccine intentions
The intention to receive a booster vaccine for participants was assessed using a single item: ‘Are you willing to get a COVID-19 booster if one becomes available?’ Given that a COVID-19 booster became available in September 2021,48 some survey participants had already received a booster at the time of the survey. Participants provided responses on a scale, with options ‘1 = yes,’ ‘2 = no,’ ‘3 = I don’t know,’ and ‘4 = I have already received a booster.’ These responses were subsequently dichotomized as follows: ‘2 = no’ and ‘3 = I don’t know’ were grouped as ‘0 = no/I don’t know,’ while ‘1 = yes’ and ‘4 = I have already received a booster’ were combined as ‘1 = yes/already received.’
Statistical analysis
Descriptive statistical analysis, which included generating frequency distributions and calculating means, was carried out using R version 4.2.3. To assess the hypothesized TPB model, Structural Equation Modeling (SEM) was employed via the Lavaan package in R.49,50 SEM is a statistical technique that allows for the simultaneous examination of relationships between observed and latent constructs within the hypothesized model. It helps determine whether the model adequately fits the data and provides estimates of the strength of associations between the modeled constructs.51,52
We adopted a two-stage modeling approach to evaluate the hypothesized TPB model.53 In the initial stage, Confirmatory Factor Analysis (CFA) was conducted to assess the factorial validity of the latent constructs and the adequacy of the measurement model. This stage included the evaluation of three latent constructs: attitudes, perceived behavioral control, and subjective norms. Modification indices were examined to identify potential sources of model misfit, which served as a basis for refining the measurement model as necessary.
Once the measurement model was specified, the subsequent step involved conducting SEM to assess whether the hypothesized TPB model (Figure 1) exhibited a satisfactory fit to the data and to estimate the relationships within the model. The SEM model included four latent variables (attitudes, perceived behavioral control, subjective norms, intention) while gender, race and ethnicity were treated as observed variables (Figure 1). To account for the binary outcome of intention, we employed the diagonally weighted least square estimator with a probit link. Once the SEM was established, we proceeded with a subgroup analysis to compare the SEM model among young adults from racial and ethnic minority backgrounds against a model for non-Hispanic White young adults based upon the definition from the National Institute on Minority Health and Health Disparities.54 This examination was prompted by prior research findings suggesting variations in vaccination intentions associated with race and ethnicity.35–37
Figure 1.
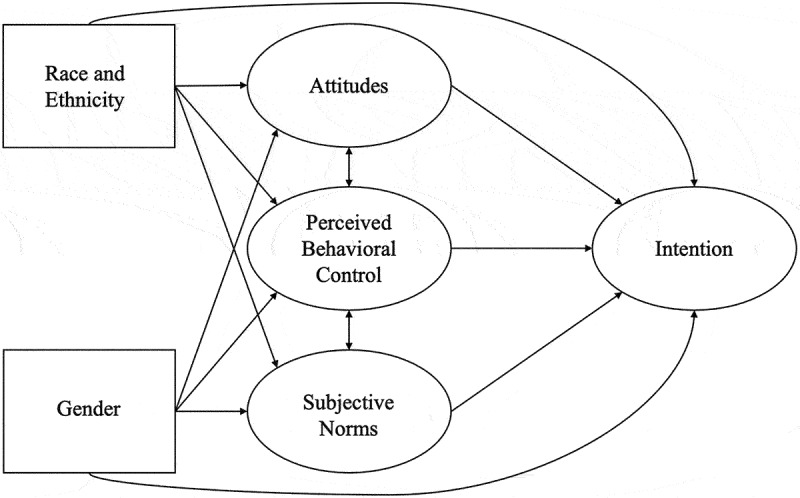
The hypothesized theory of planned behavior (TPB) model.
The hypothesized theory of planned behavior (TPB) model, including four latent variables: (1) intention, (2) attitudes, (3) perceived behavioral control, and (4) subjective norms and two observed variables: race/ethnicity and gender.
To evaluate the model’s fit to the data, we assessed several fit indices, including the chi-square (χ2) test, comparative fit index (CFI), non-normed fit index (NNFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR).55,56 A statistically non-significant result for the chi-square test (p > .05) would suggest a good fit for the model. However, the significance of the chi-square test is greatly influenced by sample size, and large samples can yield significant p-values even with minor model misspecifications.57 Therefore, emphasis was placed on the other fit indices.
To address missing data, participants who did not respond to any of the survey items used in the present study were excluded from the analyses. This decision was made because incomplete surveys may not occur randomly and could be indicative of a lack of interest or engagement, potentially introducing bias into the variability of response variables. For participants with partially missing survey data, we employed multiple imputations using chained equations.58 Prior to conducting multiple imputation, we conducted Little’s MCAR test to evaluate whether the assumptions required for multiple imputation were upheld in our dataset. The test produced a p-value of 0.846, supporting the use of multiple imputation.59 Subsequently, the imputed datasets were combined using Rubin’s rules,60 resulting in a common set of m = 5 imputations. This approach not only helped retain data for use in multivariable models but also enhanced the robustness and reliability of our analysis. Following the completion of the imputation process, we generated a binary indicator variable, denoting ‘0 = not imputed/no missing’ and ‘1 = imputed.’ This variable was then included as a control variable in the SEM analysis. Its incorporation allowed us to assess and potentially adjust for any effects related to imputation, contributing to the overall rigor and validity of the study’s findings. Lastly, to bolster the reliability of our analysis, we introduced bootstrap standard errors with 1,000 replicates to enhance the robustness of the estimates.
Results
Table 2 presents the socio-demographic characteristics of 292 participants. The participants had an average age of 21.98 years (SD = 2.25). The sample was racially diverse, with non-Hispanic White young adult participants comprising 49% of the group. Additionally, 56.7% identified as heterosexual, 23.4% as bisexual, and 8.5% as lesbian or gay Regarding their intention to receive a booster, 88.7% expressed the intention to receive one, while 11.3% reported not intending to do so. The means of TPB constructs among participants were as follows: attitudes (mean 4.5; SD 0.54), subjective norms (mean 4.6; SD 0.55), and perceived behavioral control (mean 4.1; SD 0.57) (Table 3).
Table 2.
Demographic characteristics.
| Young adult participants (n = 292) | |
|---|---|
| Intention (n (%)) | |
| Intended to receive a booster | 259 (88.7) |
| Not intended to receive a booster | 33 (11.3) |
| Age (mean (standard deviation)) | 21.98 (2.25) |
| Race and Ethnicity (n (%)) | |
| Hispanic/Latinx | 25 (8.6) |
| Non-Hispanic Multiracial/Other | 21 (7.2) |
| Non-Hispanic Asian | 69 (23.6) |
| Non-Hispanic Black or African American | 34 (11.6) |
| Non-Hispanic White | 143 (49.0) |
| Gender (n (%)) | |
| Woman | 190 (65.5) |
| Man | 84 (29.0) |
| Transgender or gender diverse | 16 (5.5) |
| Sexual Orientation (n (%)) | |
| Straight (i.e., not gay, lesbian or bisexual) | 160 (56.7) |
| Bisexual | 66 (23.4) |
| Gay | 24 (8.5) |
| Lesbian | 16 (5.7) |
| Other | 16 (5.7) |
Table 3.
The theory of planned behavior measurement model.
| Latent Factors | N | Items | Mean | SD | Standardized Factor Loadings |
|---|---|---|---|---|---|
| Attitude (α = 0.87) |
292 | Receiving a COVID-19 vaccine would protect me from getting COVID-19. | 4.5 | 0.91 | 0.580 |
| 210 | If I get a COVID-19 vaccine, I could go to school in person. | 4.6 | 0.70 | 0.343 | |
| 292 | If I get a COVID-19 vaccine, I could safely participate in school, group, and sports activities. | 4.3 | 0.78 | 0.683 | |
| 292 | If I get a COVID-19 vaccine, I could travel safely. | 4.2 | 0.86 | 0.662 | |
| 292 | If I get a COVID-19 vaccine, I would be less worried about getting COVID-19. | 4.4 | 0.81 | 0.692 | |
| 292 | Receiving a COVID-19 vaccine would help protect our community from COVID-19. | 4.6 | 0.63 | 0.744 | |
| 292 | Receiving a COVID-19 vaccine would make me safe around other people. | 4.4 | 0.80 | 0.781 | |
| 198 | Receiving a COVID-19 vaccine would help protect other students and teachers in my school from COVID-19. | 4.6 | 0.70 | 0.710 | |
| 281 | Receiving a COVID-19 vaccine would protect others in my family from getting COVID-19. | 4.7 | 0.60 | 0.742 | |
| Subjective Norm (α = 0.82) |
292 | Most people who are important to me would approve of me receiving a COVID-19 vaccine. | 4.5 | 0.77 | 0.662 |
| 178 | My boyfriend/girlfriend would approve of me receiving a COVID-19 vaccine. | 4.7 | 0.62 | 0.529 | |
| 292 | My family would approve of me receiving a COVID-19 vaccine. | 4.4 | 0.87 | 0.550 | |
| 291 | My friends would approve of me receiving a COVID-19 vaccine. | 4.6 | 0.61 | 0.648 | |
| 265 | My doctor would approve of me receiving a COVID-19 vaccine. | 4.9 | 0.45 | 0.689 | |
| 81 | My pastor or other religious leader would approve of me receiving a COVID-19 vaccine. | 4.4 | 0.80 | 0.269 | |
| 292 | My mother would approve of me receiving a COVID-19 vaccine. | 4.4 | 1.02 | 0.378 | |
| 292 | My father would approve of me receiving a COVID-19 vaccine. | 4.4 | 0.97 | 0.417 | |
| Perceived Behavioral Control (α = 0.91) |
292 | I am sure I can get a COVID-19 vaccine, even if I have many problems in my life. | 4.3 | 0.82 | 0.478 |
| 292 | I am sure I can get a COVID-19 vaccine, even if I am very busy. | 4.4 | 0.74 | 0.668 | |
| 292 | I am sure I can get a COVID-19 vaccine, even if it is hard to find a place that offers the vaccine. | 4.1 | 0.89 | 0.824 | |
| 292 | I am sure I can get a COVID-19 vaccine, even if it is offered at inconvenient times. | 4.0 | 1.05 | 0.894 | |
| 292 | I am sure I can get a COVID-19 vaccine, even if it is hard to make an appointment. | 3.9 | 1.05 | 0.899 | |
| 257 | I am sure I can get a COVID-19 vaccine, even if I have to take time off from work or school to be vaccinated. | 4.1 | 1.05 | 0.663 | |
| 292 | I am sure I can get a COVID-19 vaccine, even if the place that offers the vaccine is far from my home. | 3.8 | 1.10 | 0.762 | |
| 292 | I am sure I can get a COVID-19 vaccine, even if the waiting time is very long. | 4.0 | 0.93 | 0.753 | |
| Intention | 292 | Are you willing to get a COVID-19 booster if one becomes available? | 1.2 | 0.58 | Not applicable |
Abbreviations: COVID-19 (coronavirus disease 2019), SD (standard deviation).
Measurement model
The complete measurement model is depicted in Table 3. The standardized factor loadings within this model varied from 0.269 to 0.899 and were all statistically significant (p < .001). The standardized correlation coefficients, which represent the relationships between the model’s factors, spanned from 0.208 to 0.657 (Table 4). All factor correlations remained below the established threshold of 0.85.61 These findings collectively affirm the model’s overall satisfactory level of discriminant validity across its latent constructs.61
Table 4.
Standardized factor correlations from the confirmatory factor analysis.
| Constructs | Correlation coefficients |
|---|---|
| Attitude – Subjective norm | 0.657 |
| Attitude – Perceived behavioral control | 0.334 |
| Attitude – Intention | 0.323 |
| Subjective norm – Perceived behavioral control | 0.436 |
| Subjective norm – Intention | 0.461 |
| Perceived behavioral control – Intention | 0.208 |
The initial three-factor measurement model produced the following fit indices: χ2 = 1113.405; degrees of freedom (df) = 272; p < .001; CFI = 0.785; NNFI = 0.763; RMSEA = 0.103 with a 95% confidence interval (CI) of 0.096–0.111; SRMR = 0.118 (Table 5, Model 1). Based on modification indices, the model fit could be improved by allowing a correlation between residuals of three items in the subjective norm construct: (1) “My family would approve of me receiving a COVID-19 vaccine,” (2) “My mother would approve of me receiving a COVID-19 vaccine,” and (3) “My father would approve of me receiving a COVID-19 vaccine.” Given the close interrelation of the concepts of family, mother, and father for young adults,62 these residual correlations made theoretical sense and were thus incorporated into the model. With these adjustments, the final measurement model yielded the following fit indices: χ2 = 956.784; df = 269; p < .001; CFI = 0.824; NNFI = 0.804; RMSEA = 0.094 with a 95% CI of 0.086–0.102; SRMR = 0.082 (Table 5, Model 2).
Table 5.
Fit indices for the TPB measurement and structural models.
| Fit Indices | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| χ2 | 1113.405 | 956.784 | 786.920 | 1011.497 |
| df | 272, p < .001 | 269, p < .001 | 365, p < .001 | 702, p < .001 |
| CFI | 0.785 | 0.824 | 0.946 | 0.954 |
| NNFI | 0.763 | 0.804 | 0.952 | 0.958 |
| RMSEA | 0.103 | 0.094 | 0.063 | 0.057 |
| 95% CI RMSEA | 0.096–0.111 | 0.086–0.102 | 0.056–0.070 | 0.051–0.063 |
| SRMR | 0.118 | 0.082 | 0.077 | 0.097 |
Model 1: Measurement model without modification.
Model 2: Measurement model with modification.
Model 3: Structural model.
Model 4: Multigroup structural model by race.
Abbreviations: TPB (the theory of planned behavior), df (degrees of freedom), CFI (comparative fit index), NNFI (non-normed fit index), RMSEA (root mean square error of approximation), SRMR (standardized root mean square residual), CI (confidence interval).
Structural model
The measurement model fit indices were optimized once we aligned our latent factors with the theoretical pathways proposed by the Theory of Planned Behavior (χ2 = 786.920; df = 365, p < .001; CFI = 0.946; NNFI = 0.952; RMSEA = 0.063 with 95% CI = 0.056–0.070; SRMR = 0.077) (Table 5, Model 3). Among the hypothesized effects, only the subjective norm construct was found to be a statistically significant predictor of intention (standardized β̂ = 0.685, p = .018; 95% CI = 0.235 to 1.136). On the other hand, attitudes (standardized β̂ = 0.131, p = .572; 95% CI = −0.327 to 0.589) and perceived behavioral control (standardized β̂ = 0.171, p = .293; 95% CI = −0.153 to 0.495) were not statistically significant in influencing intention to receive the COVID-19 booster (Table 6). Race and ethnicity (standardized β̂ = 0.151, p = .317; 95% CI = −0.139 to 0.442), and gender (standardized β̂ = 0.289, p = .056; 95% CI = 0.000 to 0.573) did not show statistically significant associations with intention (Figure 2).
Table 6.
Estimated regression coefficients for the structural equation model (Model 3).
| Effects | Unstandardized β̂ | 95% CI | Standardized β̂ | 95% CI |
|---|---|---|---|---|
| Overall (n = 292) | ||||
| Attitude | 0.152 | −0.392 to 0.678 | 0.131 | −0.327 to 0.589 |
| Subjective norm | 0.954* | 0.365 to 1.808 | 0.685* | 0.235 to 1.136 |
| Perceived behavioral control | 0.223 | −0.19 to 0.599 | 0.171 | −0.153 to 0.495 |
| Race and ethnicity | 0.067 | −0.075 to 0.196 | 0.151 | −0.139 to 0.442 |
| Gender | 0.141 | −0.010 to 0.297 | 0.289 | 0.000 to 0.573 |
| Non-Hispanic White (n = 132) | ||||
| Attitude | −0.594 | −1.218 to 0.029 | −0.386 | −0.716 to 0.057 |
| Subjective norm | 2.309* | 0.857 to 3.762 | 1.104* | 0.703 to 1.505 |
| Perceived behavioral control | −0.065 | −0.704 to 0.574 | −0.040 | −0.432 to 0.351 |
| Gender (reference: women) | −0.662* | −1.285 to −0.039 | −0.373* | −0.691 to −0.055 |
| Race and ethnic minority (n = 142) | ||||
| Attitude | 0.490* | 0.154 to 0.827 | 0.488* | 0.153 to 0.823 |
| Subjective norm | 0.537* | 0.000 to 1.074 | 0.451* | 0.022 to 0.879 |
| Perceived behavioral control | 0.207 | −0.189 to 0.603 | 0.153 | −0.143 to 0.449 |
| Gender (reference: women) | −0.256 | −0.795 to 0.284 | −0.190 | −0.579 to 0.198 |
Abbreviation: CI (confidence interval).
*p < .05.
Figure 2.
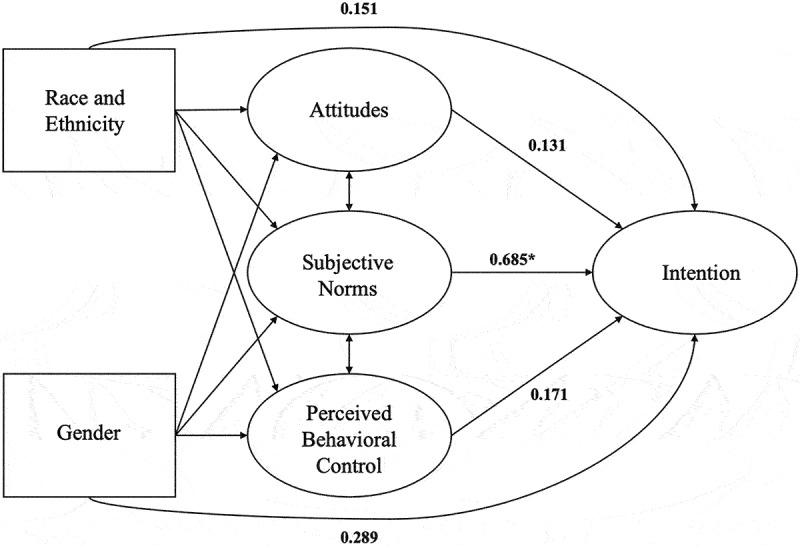
The structural equation model.
*p < 0.05.
Subgroup analyses
Both subgroups had sample sizes exceeding 100, with 142 young adults from racial and ethnic minority backgrounds and 132 non-Hispanic White young adults.63 The structural model for both groups exhibited a good fit (χ2 = 1011.497; df = 702, p < .001, CFI = 0.954, NNFI = 0.958, RMSEA = 0.057 with 95% CI = 0.051–0.063, SRMR = 0.097) (Table 5, Model 4). The hypothesized effects varied across racial and ethnic subgroups (Table 6). Among young adults from racial and ethnic minority backgrounds, attitudes (standardized β̂ = 0.488, p = .004) and subjective norms (standardized β̂ = 0.451, p = .050) were significantly associated with the intention to receive COVID-19 boosters (Figure 3). In contrast, among non-Hispanic White young adults, only subjective norms were significantly associated with intention (standardized β̂ = 1.104, p = .002), while attitudes did not have a statistically significant effect (standardized β̂ = −0.386, p = .062) (Figure 4). Additionally, non-Hispanic White young adult men showed lower intentions compared to non-Hispanic White young adult women (standardized β̂ = −0.373, p = .037).
Figure 3.
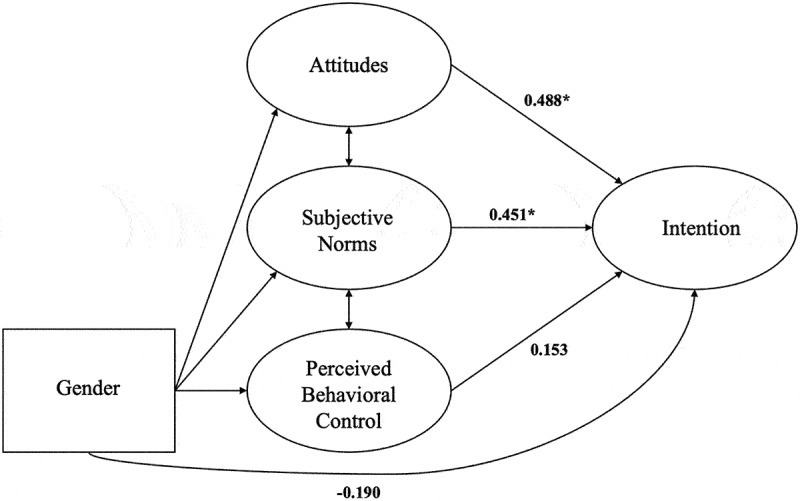
The structural equation model for young adults from racial and ethnic minority backgrounds.
*p < 0.05.
Figure 4.
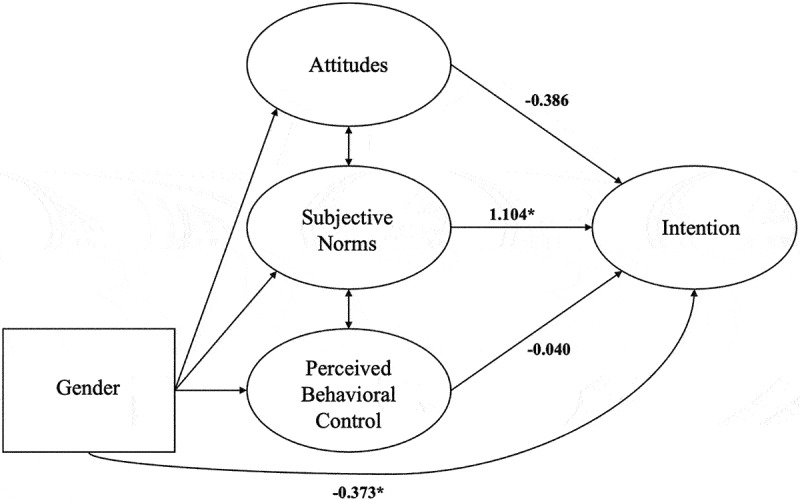
The structural equation model for non-Hispanic White young adults.
*p < 0.05.
Discussion
The results of this SEM analysis provided valuable insights into the factors associated with the intentions of young adults to receive the COVID-19 booster. One of the most significant findings of this study is the dominant role of subjective norms in shaping the intention to receive the COVID-19 booster among young adult participants. Subjective norms, which reflect the influence of family and peer approval,14 emerged as the only statistically significant predictor of intention. This suggests that the perception of approval from one’s immediate social circle is a key driver in motivating young adults to receive a booster.
This finding aligns with prior research underscoring the substantial impact of social factors on health-related behaviors among young adult populations,64,65 especially regarding vaccination decisions.32–34 Of particular note, within the subjective norm items, the desire for acceptance and approval from healthcare providers and peers received the highest mean scores. Moreover, our survey results revealed that participants ranked the Centers for Disease Control and Prevention (CDC), Food and Drug Administration (FDA), and healthcare providers as their top three most trusted sources of information about COVID-19 vaccines. Therefore, public health interventions should strategically leverage these insights by developing approaches that harness the influence of social networks and encourage discussions within healthcare provider and peer groups to emphasize the critical importance of COVID-19 vaccination, in alignment with the continued emphasis from trusted government organizations like the CDC and FDA.
In contrast, attitudes and perceived behavioral control, while integral components of TPB, did not demonstrate statistically significant associations with the intention to receive the COVID-19 vaccine booster. Although this finding is consistent with a recent U.S.-based study that employed the TPB model to examine college students’ intentions to receive COVID-19 primary series,32 it diverges from two previous studies focused on college students’ intentions to receive COVID-19 boosters, which identified attitudes as a significant predictor.22,26 It is important to note that there are only a few studies that specifically focus on young adults’ intentions regarding booster vaccination, and those that do exist are primarily conducted among college students. To address this limitation, our study included young adults from varied educational backgrounds. By doing so, we aimed to capture the diverse experiences and perspectives of young adults more comprehensively. This broader inclusion enhances the applicability and relevance of our findings for public health interventions aimed at promoting booster vaccination uptake among this age group, making our results more generalizable and useful for designing effective vaccination strategies.
Additionally, the previous studies either controlled for race/ethnicity or did not include race in their models. Given ongoing reports of racial and ethnic disparities in COVID-19 vaccine uptake,66,67 our study uniquely investigates factors associated with the intentions of young adults across diverse racial and ethnic backgrounds. Our subgroup analysis revealed that attitudes significantly predicted the intention to receive the booster only among young adults from racial and ethnic groups other than non-Hispanic White young adults. This finding aligns with our study that examined parents’ intentions to vaccinate their children against COVID-19 using the TPB, conducted during the same time period in Philadelphia.47 Among parents from racial and ethnic groups other than non-Hispanic White individuals, both attitudes and subjective norms exhibited significant positive associations with the intention to vaccinate their children. However, for non-Hispanic White parents, only subjective norms played a more prominent role in shaping their intentions.47 This suggests that the influence of attitudes on vaccination intentions may vary significantly across different racial and ethnic groups. These nuances highlight the importance of considering demographic factors, such as race and ethnicity, when examining the determinants of health behaviors. Our study underscores the need for targeted interventions tailored to the specific needs and motivations of diverse populations to enhance vaccine uptake.
The absence of a relationship between COVID-19 booster attitudes and intentions is not consistent with prior studies in the U.S. that examined young adults’ influenza vaccination intentions using the TPB model, where attitudes were identified as a significant predictor.33,34 Several potential reasons might account for this inconsistency. First, it is important to consider the unique context of the COVID-19 pandemic, characterized by rapidly changing information, vaccine hesitancy, and the emergence of new variants. These factors could have differentially influenced young adults’ intentions compared to the more established and familiar context of seasonal influenza. Second, social and peer pressures specific to COVID-19 vaccination, such as vaccine mandates or societal expectations, may have overridden individual attitudes. Last, differences in the implementation of vaccination campaigns, communication strategies, and public health interventions for COVID-19 and influenza could also contribute to varying outcomes within the TPB framework. Moreover, it is important to note that our study was conducted during the initial Omicron wave, characterized by a high number of COVID-19 infections and associated hospitalizations. It is conceivable that attitudes among young adults may have evolved since then, particularly given the dynamic nature of the pandemic. Therefore, it would be valuable for future research to reassess young adults’ attitudes and intentions toward COVID-19 vaccination in light of evolving circumstances and updated public health measures.
Our study also contributes new insights into gender-specific differences in vaccination intentions among non-Hispanic White young adults. Gender did not emerge as a statistically significant predictor of vaccination intention in the overall structural model or in the subgroup model for young adults from racial and ethnic minority backgrounds. However, among non-Hispanic White young adults, gender differences were observed. Specifically, men from these backgrounds showed a lower intention to receive the COVID-19 vaccine booster compared to women. A study that examined gender differences in the intention to receive the COVID-19 primary series using the TPB reported that attitudes were associated exclusively with the intentions of men, whereas subjective norms were associated exclusively with the intentions of women.68 Although we were unable to conduct multigroup analyses by gender due to a limited sample size for male participants, these findings underscore the importance of considering gender as a potential variable in understanding vaccination behaviors, particularly within specific demographic groups. The lower intention among non-Hispanic White young adult men could be attributed to several factors, such as differing levels of trust in the healthcare system, varying degrees of perceived risk, and different sources of information and influence. Future research should examine these factors within more diverse and larger populations to gain a comprehensive understanding of their impact on vaccination intentions. Additionally, these gender-based differences suggest that public health campaigns may need to adopt tailored strategies that address the unique concerns and motivations of men and women within these communities to enhance vaccine uptake effectively. Addressing such nuances is crucial for developing interventions that are both equitable and effective in reaching all segments of the population.
In the assessment of this study, several crucial considerations come to light. First, one of the study’s strengths lies in its foundation on a theory-based approach, particularly focusing on the intentions of young adults related to COVID-19 booster shots. However, it is essential to recognize the study’s limitations. First, the findings may not be universally applicable to all young adults due to the convenience sampling method used and the study’s limited geographic scope, limited to a single city in the United States. Additionally, a notable aspect of our study is the overrepresentation of certain populations, particularly individuals identifying as bisexual, compared to other national surveys. This may be attributed to our specific focus on young adults from Generation Z, a demographic characterized by a higher representation of LGBTQ+ individuals.69 Second, our model did not account for broader socio-cultural influences, such as school or workplace vaccine policies, including vaccine mandate policies. Future research should consider integrating multi-level theoretical frameworks to better comprehend and address these broader influences on vaccination behavior. Third, we also did not include the construct of “actual behavior” in our model. This decision was primarily due to the constraints of our study design and data collection methodology. Our data collection was conducted during a period when COVID-19 vaccination boosters were newly available, making it challenging to measure “actual behavior” reliably. Many participants had not yet had the opportunity to act on their intentions due to various external factors, such as vaccine availability and appointment scheduling issues. Therefore, we concentrated on “behavioral intention” as a proximal outcome, which is a strong predictor of “actual behavior” according to TPB. Despite this limitation, our study contributes valuable insights into the early stages of the decision-making process, which are essential for designing effective public health interventions. Fourth, although we employed Little’s MCAR test to examine whether multiple imputation was an adequate technique to handle missing data, we acknowledge that unmeasured constructs or the value of the variables with missing data could be associated with missingness in this data. Next, in the use of cross-sectional data to test a SEM model, it is crucial to clarify that the models are not designed to depict a causal pathway. This cross-sectional design, while valuable for providing a snapshot of young adults’ intentions, may not fully account for the dynamic nature of the situation, characterized by evolving vaccine availability and shifting recommendations. To gain a more comprehensive understanding of how young adults’ intentions change over time in response to these developments, longitudinal studies could provide further insight. Finally, our CFA results produced suboptimal fit indices initially and required modification. However, it is noteworthy that the fit improved once the theoretical pathways of the TPB were modeled onto our data, both in the overall sample and in racial/ethnic subgroup analyses, suggesting that the inclusion of theoretically-driven pathways enhanced the model’s explanatory power and alignment with the observed data.
Conclusion
This study underscores the importance of subjective norms and the influence of social networks in motivating young adults to receive the COVID-19 vaccine booster. Public health interventions should prioritize leveraging social influences and trusted sources to promote COVID-19 booster uptake among young adults. Strategies should harness the power of social networks and encourage discussions within peer groups and healthcare provider interactions, emphasizing endorsements from respected health authorities. Integrating digital platforms and social media influencers could be a novel approach to reaching young adults. Collaborations with influencers who resonate with this demographic can amplify messages about the importance of COVID-19 boosters. Additionally, creating interactive online forums or virtual events where young adults can engage with healthcare professionals and peers in real-time discussions about vaccination could foster a more informed and supportive community. These digital engagement strategies, combined with culturally sensitive messaging and the leveraging of social networks, can create a more robust and effective campaign to increase COVID-19 booster uptake among young adults.
As the COVID-19 vaccination effort continues, understanding the dynamics of young adults’ vaccine intentions is crucial. These findings can inform targeted and effective public health interventions that take into account the unique perspectives and influences that shape young adults’ decisions about vaccination.
Acknowledgments
This research was supported by an award from the National Institutes of Health to Drs. Bauermeister & Villarruel as part of the NIH Community Engagement Alliance (CEAL) program (Philadelphia Community Engagement Alliance to Address COVID-19 Inequities). We thank our participants and community partners for their participation in this initiative.
Biographies
Hyunmin Yu is a postdoctoral fellow at the University of Pennsylvania School of Nursing.
Stephen Bonett is an assistant professor of nursing at the University of Pennsylvania School of Nursing.
Ufuoma Oyiborhoro is a project manager at the University of Pennsylvania School of Nursing.
Subhash Aryal is a professor and director of the Biostatistics and Methods Core at the Johns Hopkins School of Nursing.
Melanie Kornides is an associate professor of nursing at the University of Pennsylvania School of Nursing.
Karen Glanz is the George A. Weiss University Professor, with appointments in the Perelman School of Medicine and the School of Nursing at the University of Pennsylvania.
Antonia Villarruel is a professor and the Margaret Bond Simon Dean of Nursing at the University of Pennsylvania School of Nursing.
José Bauermeister is the Albert M. Greenfield Professor of Human Relations and a professor at the University of Pennsylvania School of Nursing.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Funding Statement
This research was, in part, funded by the National Institutes of Health (NIH) Agreement OT2HL158287. The views and conclusions contained in this document are those of the authors and should not be interpreted as representing the official policies, either expressed or implied, of the NIH.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Authors’ contributions
Conceptualization and methodology, H.Y., S.B., U.O., S.A. and J.B.; data curation H.Y.; statistical analysis, H.Y., S.B., S.A., A.V. and J.B.; original draft preparation and writing, H.Y.; review and editing, S.B., U.O., S.A., M.K., K.G., A.V. and J.B.; supervision and funding, A.V. and J.B. All authors have read and agreed to the published version of the manuscript.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Human rights
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the University of Pennsylvania Institutional Review Board (IRB protocol#: 848650).
References
- 1.Nicola M, Alsafi Z, Sohrabi C, Kerwan A, Al-Jabir A, Iosifidis C, Agha M, Agha R.. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–11. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mishra NP, Das SS, Yadav S, Khan W, Afzal M, Alarifi A, Ansari MT, Hasnain MS, Nayak AK.. Global impacts of pre-and post-COVID-19 pandemic: focus on socio-economic consequences. Sens Int. 2020;1:100042. doi: 10.1016/j.sintl.2020.100042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buheji M, da Costa Cunha K, Beka G, Mavric B, De Souza Y, da Costa Silva SS, Hanafi M, Yein TC. The extent of COVID-19 pandemic socio-economic impact on global poverty. A global integrative multidisciplinary review. Am J Econ. 2020;10(4):213–224. doi: 10.5923/j.economics.20201004.02. [DOI] [Google Scholar]
- 4.Tewarson H, Greene K, Fraser MR. State strategies for addressing barriers during the early US COVID-19 vaccination campaign. Am J Public Health. 2021;111(6):1073–1077. doi: 10.2105/AJPH.2021.306241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . Statement on the fifteenth meeting of the IHR (2005) emergency committee on the COVID-19 pandemic. [accessed 2023 Dec 21]. https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic.
- 6.Mbaeyi S, Oliver SE, Collins JP, Godfrey M, Goswami ND, Hadler SC, Jones J, Moline H, Moulia D, Reddy S, et al. The advisory committee on immunization practices’ interim recommendations for additional primary and booster doses of COVID-19 vaccines—United States, 2021. Morb Mortal Wkly Rep. 2021;70(44):1545. doi: 10.15585/mmwr.mm7044e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention . Map of COVID-19 vaccinations by age and sex. [accessed 2023 Dec 21]. https://covid.cdc.gov/covid-data-tracker/#vaccination-states-jurisdictions.
- 8.Boehmer TK, DeVies J, Caruso E, van Santen KL, Tang S, Black CL, Hartnett KP, Kite-Powell A, Dietz S, Lozier M, et al. Changing age distribution of the COVID-19 pandemic—United States, May–August 2020. Morb Mortal Wkly Rep. 2020;69(39):1404. doi: 10.15585/mmwr.mm6939e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. COVID Data Tracker; [accessed 2023 Dec 21]. https://covid.cdc.gov/covid-data-tracker/#demographics. [Google Scholar]
- 10.Monod M, Blenkinsop A, Xi X, Hebert D, Bershan S, Tietze S, Baguelin M, Bradley VC, Chen Y, Coupland H. Age groups that sustain resurging COVID-19 epidemics in the United States. Science. 2021;371(6536):eabe8372. doi: 10.1126/science.abe8372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jørgensen F, Bor A, Petersen MB. Compliance without fear: Individual‐level protective behaviour during the first wave of the COVID‐19 pandemic. Br J Health Psychol. 2021;26(2):679–696. doi: 10.1111/bjhp.12519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Furuse Y, Sando E, Tsuchiya N, Miyahara R, Yasuda I, Ko YK, Saito M, Morimoto K, Imamura T, Shobugawa Y. Clusters of coronavirus disease in communities, Japan, January–April 2020. Emerg Infect Dis. 2020;26(9):2176. doi: 10.3201/eid2609.202272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Limbu YB, Gautam RK, Zhou W. Predicting vaccination intention against COVID-19 using theory of planned behavior: a systematic review and meta-analysis. Vaccines. 2022;10(12):2026. doi: 10.3390/vaccines10122026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 15.Almokdad E, Kiatkawsin K, Lee CH. Antecedents of booster vaccine intention for domestic and international travel. Sustainability. 2023;15(8):6399. doi: 10.3390/su15086399. [DOI] [Google Scholar]
- 16.Barattucci M, Pagliaro S, Ballone C, Teresi M, Consoli C, Garofalo A, De Giorgio A, Ramaci T. Trust in science as a possible mediator between different antecedents and COVID-19 booster vaccination intention: an integration of health belief model (HBM) and theory of planned behavior (TPB). Vaccines. 2022;10(7):1099. doi: 10.3390/vaccines10071099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Catalano HP, Richards K, Shaw KHH, Catalano M. Applying the theory of planned behavior to predict COVID-19 booster vaccination intentions of college students. J Am Coll Health. 2023;1–0. doi: 10.1080/07448481.2023.2228425. [DOI] [PubMed] [Google Scholar]
- 18.Geers AL, Clemens KS, Colagiuri B, Jason E, Colloca L, Webster R, Vase L, Seig M, Faasse K. Do side effects to the primary COVID-19 vaccine reduce intentions for a COVID-19 vaccine booster? Ann Behav Med. 2022;56(8):761–768. doi: 10.1093/abm/kaac027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folcarelli L, Miraglia Del Giudice G, Corea F, Angelillo IF. Intention to receive the COVID-19 vaccine booster dose in a university community in Italy. Vaccines. 2022;10(2):146. doi: 10.3390/vaccines10020146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hagger MS, Hamilton K. Predicting COVID‐19 booster vaccine intentions. Appl Psychol Health Well‐Being. 2022;14(3):819–841. doi: 10.1111/aphw.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hwang L-A, Vaithilingam S, Ng JWJ, Nair M, Ahmed P, Musa KI, Mahmoud AB. The continuance intention to vaccinate against COVID-19: an empirical study from Malaysia. PLoS One. 2024;19(4):e0301383. doi: 10.1371/journal.pone.0301383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu CC, Ling J, Zahry NR, Liu C, Ammigan R, Kaur L, Mehmood K. Using the theory of planned behavior to determine COVID-19 vaccination intentions and behavior among international and domestic college students in the United States. PLoS One. 2024;19(2):e0293130. doi: 10.1371/journal.pone.0293130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lounis M, Bencherit D, Rais MA, Riad A. COVID-19 vaccine booster hesitancy (VBH) and its drivers in Algeria: national cross-sectional survey-based study. Vaccines. 2022;10(4):621. doi: 10.3390/vaccines10040621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maria S, Pelupessy DC, Koesnoe S, Yunihastuti E, Handayani DOT, Siddiq TH, Mulyantini A, Halim ARV, Wahyuningsih ES, Widhani A, et al. COVID-19 booster vaccine intention by health care workers in Jakarta, Indonesia: using the extended model of health behavior theories. Trop Med Infect Dis. 2022;7(10):323. doi: 10.3390/tropicalmed7100323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orellana D, Mercado A, Roth E. Psychosocial factors associated with the intention to get a COVID-19 booster vaccine: evidence from a low-income country. J Public Health (Berl). 2023;2023:1–9. doi: 10.1007/s10389-023-01937-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sugawara N, Yasui-Furukori N, Fukushima A, Shimoda K. Attitudes of medical students toward COVID-19 vaccination: who is willing to receive a third dose of the vaccine? Vaccines. 2021;9(11):1295. doi: 10.3390/vaccines9111295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang Z, Fang Y, Yu F-Y, Chan P-F, Chen S, Sun F. Facilitators and barriers to take up a COVID-19 vaccine booster dose among community-dwelling older adults in Hong Kong: a population-based random telephone survey. Vaccines. 2022;10(6):966. doi: 10.3390/vaccines10060966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang J, Li T, Ge J, Zhou M, Walker AN, Chen J, Zhang T, Zhang K, Gu S, You H, et al. Applying two behavioral theories to predict the willingness to receive COVID-19 vaccine booster in the elderly: a cross-sectional study. Res Soc Adm Pharm. 2023;19(3):495–501. doi: 10.1016/j.sapharm.2022.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wong LP, Alias H, Siaw Y-L, Muslimin M, Lai LL, Lin Y, Hu Z. Intention to receive a COVID-19 vaccine booster dose and associated factors in Malaysia. Hum Vaccin Immunother. 2022;18(5):2078634. doi: 10.1080/21645515.2022.2078634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiang H, Li Y, Guo Y. Promoting COVID-19 booster vaccines in Macao: a psychological reactance perspective. Soc Sci Med. 2023;332:116128. doi: 10.1016/j.socscimed.2023.116128. [DOI] [PubMed] [Google Scholar]
- 31.Zhou M, Liu L, Gu S-Y, Peng X-Q, Zhang C, Wu Q-F, Xu X-P, You H. Behavioral intention and its predictors toward COVID-19 booster vaccination among Chinese parents: applying two behavioral theories. Int J Environ Res Public Health. 2022;19(12):7520. doi: 10.3390/ijerph19127520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reyes CT, Cao W, Astorini AG, Drohan MM, Schulz CT, Shuster CL, Robbins ML, Yang M, Stamates AL. Using the theory of planned behavior to assess willingness and attitudes towards COVID-19 vaccination among a predominantly white US college sample. Health Psychol Behav Med. 2023;11(1):2248236. doi: 10.1080/21642850.2023.2248236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agarwal V. A/H1N1 vaccine intentions in college students: an application of the theory of planned behavior. J Am Coll Health. 2014;62(6):416–424. doi: 10.1080/07448481.2014.917650. [DOI] [PubMed] [Google Scholar]
- 34.Yang ZJ. Predicting young adults’ intentions to get the H1N1 vaccine: an integrated model. J Health Commun. 2015;20(1):69–79. doi: 10.1080/10810730.2014.904023. [DOI] [PubMed] [Google Scholar]
- 35.Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, Curran GM, McElfish PA. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin Transl Sci. 2021;14(6):2200–2207. doi: 10.1111/cts.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nápoles AM, Stewart AL, Strassle PD, Quintero S, Bonilla J, Alhomsi A, Santana-Ufret V, Maldonado AI, Pérez-Stable EJ. Racial/ethnic disparities in intent to obtain a COVID-19 vaccine: a nationally representative United States survey. Prev Med Rep. 2021;24:101653. doi: 10.1016/j.pmedr.2021.101653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nguyen LH, Joshi AD, Drew DA, Merino J, Ma W, Lo CH, Kwon S, Wang K, Graham, MS, Polidori L, et al. Racial and ethnic differences in COVID-19 vaccine hesitancy and uptake. medRxiv. 2021; doi: 10.1101/2021.02.25.21252402. [DOI] [Google Scholar]
- 38.Mensah GA, Johnson LE, Zhang X, Stinson N, Carrington K, Malla G, Land SR, Huff E, Freeman N, Stoney C, et al. Community Engagement Alliance (CEAL): a national institutes of health program to advance health equity. Am J Public Health. 2023;114(S1):e1–e6. doi: 10.2105/ajph.2023.307476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bonett S, Lin W, Sexton Topper P, Wolfe J, Golinkoff J, Deshpande A, Villarruel A, Bauermeister J. Assessing and improving data integrity in web-based surveys: comparison of fraud detection systems in a COVID-19 study. JMIR Form Res. 2024;8:e47091. doi: 10.2196/47091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 41.National Research Council . Investing in the health and well-being of young adults. Washington, DC, USA: National Academies Press; 2015. [PubMed] [Google Scholar]
- 42.City of Philadelphia . Health of the city: Philadelphia’s community health assessment 2021. 2021. [accessed 2024 June 12]. https://www.phila.gov/media/20220718132807/HealthOfTheCity-2021.pdf.
- 43.Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. New York: Taylor & Francis; 2011. [Google Scholar]
- 44.Montano DE, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. Health Behav: Theory, Res Pract. 2015;70(4):231. [Google Scholar]
- 45.Guassi Moreira JF, Tashjian SM, Galván A, Silvers JA. Parents versus peers: assessing the impact of social agents on decision making in young adults. Psychol Sci. 2018;29(9):1526–1539. doi: 10.1177/0956797618778497. [DOI] [PubMed] [Google Scholar]
- 46.Halpern-Felsher B, Baker M, Stitzel S. Decision-making in adolescents and young adults. Handb Health Decis Sci. 2016;157–167. doi: 10.1007/978-1-4939-3486-7_12. [DOI] [Google Scholar]
- 47.Yu H, Bonett S, Oyiborhoro U, Aryal S, Kim A, Kornides ML, Jemmott JB, Glanz K, Villarruel AM, Bauermeister JA, et al. Psychosocial correlates of parents’ willingness to vaccinate their children against COVID-19. PLOS ONE. 2024;19(6):e0305877. doi: 10.1371/journal.pone.0305877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Center for Disease Control and Prevention . CDC statement on ACIP booster recommendations. [accessed 2023 Dec 21]. https://www.cdc.gov/media/releases/2021/p0924-booster-recommendations-.html.
- 49.Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Soft. 2012;48(2):1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- 50.Beaujean AA. Latent variable modeling using R: a step-by-step guide. New York: Routledge; 2014. [Google Scholar]
- 51.Nachtigall C, Kroehne U, Funke F, Steyer R, Schiller F. v. Pros and cons of structural equation modeling. Methods Psychol Res Online. 2003;8(2):1–22. [Google Scholar]
- 52.Ullman JB, Bentler PM. Structural equation modeling. Handb Phychol, Second Ed. 2012;2. doi: 10.1002/9781118133880.hop202023. [DOI] [Google Scholar]
- 53.Cheung MW-L, Chan W. Meta-analytic structural equation modeling: a two-stage approach. Psychol Methods. 2005;10(1):40. doi: 10.1037/1082-989X.10.1.40. [DOI] [PubMed] [Google Scholar]
- 54.National Institute of Minority Health and Health Disparities . Minority health and health disparities: definitions and parameters 2024. [accessed 2024 June 12]. https://www.nimhd.nih.gov/about/strategic-plan/nih-strategic-plan-definitions-and-parameters.html.
- 55.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model: Multidiscip J. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 56.Schumacker RE, Lomax RG. A beginner’s guide to structural equation modeling. New York: Psychology Press; 2004. [Google Scholar]
- 57.Shi D, Lee T, Maydeu-Olivares A. Understanding the model size effect on SEM fit indices. Educ Psychol Meas. 2019;79(2):310–334. doi: 10.1177/0013164418783530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Van Buuren S, Brand JP, Groothuis-Oudshoorn CG, Rubin DB. Fully conditional specification in multivariate imputation. J Stat Comput Simul. 2006;76(12):1049–64. doi: 10.1080/10629360600810434. [DOI] [Google Scholar]
- 59.Little RJ. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–1202. doi: 10.1080/01621459.1988.10478722. [DOI] [Google Scholar]
- 60.Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley & Sons Inc; 1987. doi: 10.1002/9780470316696. [DOI] [Google Scholar]
- 61.Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Market Sci. 2015;43(1):115–135. doi: 10.1007/s11747-014-0403-8. [DOI] [Google Scholar]
- 62.Garfat T. A child and youth care approach to working with families. Child & Youth Serv. 2004;25(1–2):7–37. doi: 10.1300/J024v25n01_02. [DOI] [Google Scholar]
- 63.Kyriazos TA. Applied psychometrics: sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology. 2018;9(8):2207. doi: 10.4236/psych.2018.98126. [DOI] [Google Scholar]
- 64.Valente TW. Network interventions. Science. 2012;337(6090):49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- 65.Park S, Oh S. The relationships of perceived susceptibility, perceived severity, and subjective norms with COVID-19 preventive behaviors: a secondary data analysis comparing adolescents and emerging adults in South Korea. Child Health Nurs Res. 2023;29(2):149. doi: 10.4094/chnr.2023.29.2.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Na L, Banks S, Wang PP. Racial and ethnic disparities in COVID-19 vaccine uptake: a mediation framework. Vaccine. 2023;41(14):2404–11. doi: 10.1016/j.vaccine.2023.02.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Medcalfe SK, Slade CP. Racial residential segregation and COVID-19 vaccine uptake: an analysis of Georgia USA county-level data. BMC Public Health. 2023;23(1):1392. doi: 10.1186/s12889-023-16235-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dou K, Yang J, Wang LX, Li JB. Theory of planned behavior explains males’ and females’ intention to receive COVID-19 vaccines differently. Hum Vaccin Immunother. 2022;18(5):2086393. doi: 10.1080/21645515.2022.2086393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gallup . U.S. LGBT identification steady at 7.2% 2023. [accessed 2024 June 12]. https://news.gallup.com/poll/470708/lgbt-identification-steady.aspx.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.


