Abstract
This study highlights the complexities and challenges in managing obstetric emergencies, detailing critical interventions and outcomes in various high-risk cases. A retrospective analysis was conducted on four high-risk obstetric cases, each characterized by distinct complications necessitating immediate medical interventions. The study specifically examined cases involving: Fetal Distress cases where fetal health was compromised, necessitating interventions such as emergency cesarean sections. Complex Labor Dynamics detailed examinations of labor complications such as obstructed labor, precipitate labor, or labor complicated by malpresentation. Early pregnancy complications analysis focused on emergencies arising in the first trimester or early second trimester, including ectopic pregnancies and complications in pregnancies with a history of multiple cesarean sections. Severe postpartum hemorrhage investigations into cases of significant blood loss post-delivery, which required interventions ranging from pharmacological management to surgical procedures like hysterectomy. The first case concerned a 28-year-old primigravida with fetal bradycardia and thick meconium, requiring an emergency cesarean section. Postoperative complications included gestational thrombocytopenia and anemia, necessitating a total abdominal hysterectomy for severe sepsis. The newborn showed good recovery, indicated by Apgar scores. In Case 2, the need for a hysterectomy following complications during the third stage of labor was likely due to the presence of Placenta Accreta Spectrum, specifically placenta accreta or increta. While a retained placenta typically can be managed with less invasive methods, the situation escalates when the placenta is abnormally adherent to, or deeply invasive into, the uterine muscle. This can lead to uncontrollable bleeding, making a hysterectomy necessary and justified as a life-saving measure to control the severe hemorrhage while the histology confirms the diagnosis for the placenta accreta. In the third case, the decision to perform a dilation and curettage over manual vacuum aspiration was influenced by several factors. Given the severity of the patient’s hemorrhage and the presence of a suspicious echogenic structure, a dilation and curettage provided a more controlled environment for thorough evacuation and immediate bleeding control. This approach was also supported by the combination technique using both Karman aspiration and a curette, allowing for effective management of complicated cases, particularly in patients with a history of multiple cesareans and potential scar tissue. The fourth case involved a 37-year-old multipara with severe postpartum hemorrhage from uterine atony, treated with surgery and managed for diabetic ketoacidosis, leading to discharge on the fourth day. This underscores the urgency and complexity of managing obstetric emergencies effectively.
Keywords: Obstetric emergencies, high-risk pregnancy, fetal bradycardia, cesarean section, gestational thrombocytopenia, anemia in pregnancy
Introduction
Obstetrics, as a field of medicine, is uniquely characterized by its dual focus on both mother and child, often under circumstances of rapid change and potential emergency. The complexity inherent in obstetric care is further amplified by the diverse range of complications that can arise during pregnancy, labor, and the postpartum period, such as severe postpartum hemorrhage (PPH), which may necessitate life-saving interventions like peripartum hysterectomies.
This series of case reports illustrates the multifaceted nature of obstetric emergencies, encompassing a spectrum of scenarios that challenge even the most seasoned practitioners. Recent studies have shown varying rates of peripartum hysterectomies, with figures ranging from 0.26 per 1000 deliveries in Denmark to 1.07 per 1000 in Italy, highlighting a significant disparity in maternal health outcomes across high-income countries. The increasing trend in PPH and subsequent surgical interventions in these regions underscores an urgent need for a deeper understanding of these emergencies. 1
Each case in this series presents a unique set of circumstances and complications, requiring timely decision-making and often urgent intervention to ensure the safety and well-being of both the mother and the neonate. From emergency cesarean sections due to fetal distress to the aggressive management of PPH following spontaneous delivery, these reports underscore the critical importance of a well-coordinated, multidisciplinary approach in obstetric care.
The first case details a life-saving cesarean section in the face of fetal bradycardia, highlighting the nuances of managing fetal distress alongside maternal well-being. The second report delves into the complexities encountered during the third stage of labor, illustrating the challenges in managing retained placenta and Placenta Accreta Spectrum (PAS). In the third scenario, we explore the emergency management of a pregnant patient with a history of multiple cesarean sections, presenting a unique challenge due to her complicated obstetric history. Finally, the fourth case provides insights into the aggressive management of PPH following spontaneous delivery, a scenario that is as common as it is potentially life-threatening.
Together, these cases offer valuable insights into the realities of obstetric emergencies. They serve as a testament to the unpredictable nature of childbirth and the imperative for readiness and adaptability in the face of evolving clinical situations. This series aims not only to shed light on specific medical and surgical interventions but also to underscore the importance of comprehensive obstetric care that prioritizes the health and safety of both mother and child.
Case presentation
Case 1: Emergency cesarean section in response to fetal bradycardia
The case narrative begins with a 28-year-old primiparous woman experiencing her first pregnancy. Her pregnancy journey had been uneventful, with no significant medical or surgical history, until a sudden and alarming complication arose, necessitating swift medical intervention. As her pregnancy neared full term, she experienced spontaneous rupture of membranes (SROM), a common precursor to labor. However, this event took a concerning turn with the presence of thick, meconium-stained amniotic fluid, indicative of potential fetal distress and escalating the need for medical attention.
Upon arriving at the hospital, a Doppler ultrasound examination revealed a critical sign: fetal heart rate (FHR) was alarmingly low at around 60 beats per minute, a condition known as fetal bradycardia, suggesting significant fetal distress or compromise and necessitating immediate action. In the scenario you described, the presence of fetal bradycardia with a heart rate of around 60 beats per minute indeed suggests significant fetal distress, typically warranting urgent medical intervention. However, to fully assess the situation and justify the course of action taken, several other factors should be considered:
The presence of labor, especially active labor, can influence the urgency and type of intervention. The state of labor can be assessed by evaluating contractions and checking the cervical dilatation.
Cervical Dilatation: The degree of cervical opening (dilatation) is critical in labor management decisions. If the cervix is significantly dilated and the patient is in active labor, this might support a decision for an emergency delivery method, such as a cesarean section if vaginal delivery is not immediately feasible.
Cause of Fetal Bradycardia: Identifying the cause is crucial. Fetal bradycardia can result from several conditions including umbilical cord problems (e.g., prolapse, compression), maternal hypotension, uterine rupture, or placental abruption. Determining the cause would guide appropriate interventions.
Possibility of Maternal Pulse Confusion: It’s important to ensure that the low heart rate detected was indeed the fetus’s and not the mother’s. Misinterpretation could lead to unnecessary interventions. This can usually be clarified by confirming the rate through multiple methods or different monitoring equipment.
Diagnosis of Fetal Demise: A sustained low FHR below 80 bpm can be indicative of impending fetal demise. Confirmation of such a condition necessitates immediate action to either attempt to salvage the fetus or manage the situation depending on the gestational age and viability.
Justification for immediate action
Risk of Hypoxia: Fetal bradycardia, especially if confirmed to be sustained and associated with other signs of distress (like meconium-stained amniotic fluid), typically indicates that the fetus is not receiving enough oxygen. Immediate delivery might be necessary to prevent further hypoxia and potential neurological damage or fetal death.
Monitoring and Diagnostic Tools: Utilizing continuous fetal monitoring and possibly an ultrasound to assess for any acute changes (like placental abruption or cord issues) can provide more data to justify the course of action.
Given the critical nature of fetal bradycardia, especially at such a low rate, the justification for immediate action generally revolves around the potential for severe fetal compromise or demise. The decision for an emergency cesarean section or other interventions would be based on a combination of the ultrasound findings, the clinical presentation of the mother and fetus, and the immediate availability of further diagnostic information. Each case would need to be evaluated on its specifics, with a rapid yet thorough assessment to determine the safest course of action for both mother and child.
A decision was made for an urgent primary cesarean section. However, the procedure was delayed due to technical issues with spinal anesthesia administration, heightening concern for the mother and fetus.
The decision to perform an urgent cesarean section was based on critical signs of fetal distress, notably an FHR of approximately 60 beats per minute. While fetal pH values would have offered additional insights into the fetal metabolic condition, such testing was not available due to resource limitations faced by healthcare institutions in Lebanon amid ongoing crises. Consequently, the clinical assessment was primarily guided by Doppler ultrasound findings and Apgar scores post-delivery. 2 The infant’s initial Apgar score 2 of 7 at 1 min, improving to 8 at 5 min, was relied upon as key indicators of her condition at birth and her subsequent recovery.
Blood test results of each day
Day 1:
WBC (White Blood Cells): 0.81 × 109/L—Extremely low, indicates leukopenia, which could suggest an underlying infection or bone marrow suppression.
HGB (Hemoglobin): 8.6 g/dL—Indicates anemia.
PLT (Platelets): 21 × 109/L—Very low, indicates thrombocytopenia.
K+ (Potassium): 3.33 mmol/L—Slightly low.
Bicarb (Bicarbonate): 17 mmol/L—Low, suggests metabolic acidosis.
CRP (C-Reactive Protein): 271 mg/L—Extremely high, indicating significant inflammation or infection.
Day 2:
WBC: 1.91 × 109/L—Increase from Day 1 but still low.
HGB: 9.7 g/dL—Improvement, but still anemic.
HTC (Hematocrit): 28%—Indicates anemia.
PLT: 24 × 109/L—Slight improvement but still critically low.
Day 3:
WBC: 4.5 × 109/L—Improved, nearing normal.
HGB: 8.9 g/dL—Slight decrease from Day 2.
HTC: 26%—Decrease from Day 2, still anemic.
PLT: 18 × 109/L—Decreased, worsening thrombocytopenia.
INR (International Normalized Ratio): 1.29—Slightly elevated.
PT (Prothrombin Time): 16 s—Prolonged.
PTT (Partial Thromboplastin Time): 38 s—Prolonged.
CREA (Creatinine): 0.34 mg/dL—Low, may suggest malnutrition or decreased muscle mass.
Day 4:
WBC: 9.29 × 109/L—Further improved, within normal limits.
HGB: 9.7 g/dL—Stable from Day 2.
HTC: 29%—Improvement.
PLT: 25 × 109/L—Slight improvement, still low.
CRP: 210 mg/L—High, decreased from Day 1 but still indicates active inflammation.
Culture results:
Urine, Surgical, Peritoneal Fluid: Sterile.
Interpretation
The data indicates a severe and progressing inflammatory response, likely due to infection, despite initial sterile cultures. The leukopenia initially noted might have been due to a severe acute response or marrow suppression, improving with medical intervention but complicated by severe and persistent thrombocytopenia and anemia. The elevated inflammatory markers (CRP), prolonged clotting times (INR, PT, PTT), and metabolic acidosis suggest a severe systemic inflammatory response, possibly septic in nature, which aligns with the clinical findings and the decision for surgical intervention.
Ongoing monitoring and management would focus on addressing the infection, supporting marrow function, managing metabolic imbalances, and stabilizing hemodynamic status, all critical given the severe clinical picture.
Postoperatively, the mother’s condition required close monitoring, as she faced anemia and gestational thrombocytopenia. On the third day, she developed fever, tachypnea, tachycardia, dyspnea, worsening diarrhea, and abdominal pain. An urgent computed tomography (CT) scan of the abdomen and pelvis revealed extensive subcutaneous fat stranding and edema in the pelvis and lower anterolateral abdominal wall near the surgical scar, with numerous soft tissue air pockets suggestive of necrotizing fasciitis and abdominopelvic free air pockets indicative of septic peritonitis. The uterus showed intraluminal and endometrial air pockets, potentially indicating early endometritis, while the small bowels were mildly distended with diffuse wall thickening and edema.
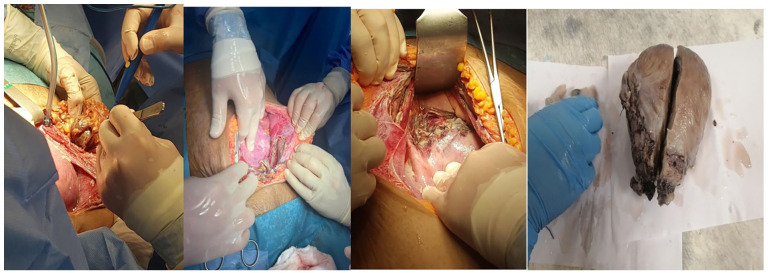
The patient was prepared for surgery and received transfusions during anesthesia induction. A midline vertical incision was made, revealing a large amount of ascitic fluid with foul-smelling discharge upon entering the peritoneal cavity. Peritoneal fluid was sent for culture. Surprisingly, inspection of the abdomen and pelvis revealed necrotizing fasciitis at the rectus fascia near the surgical site, with complete necrosis of the lower uterine incision (Figure 1).
Figure 1.
Complications of postoperative necrosis: fasciitis of the rectus fascia and uterine necrosis with pathological features.
Surgery team checked for bowel integrity twice, bowels were intact and in good condition
Decision for total abdominal hysterectomy taken and done after getting the approval from the family to remove the nidus of infection (uterus) Debridement of the fascia with insertion of penrose.
Total abdominal hysterectomy (TAH) was uneventful but upon removing the uterus the cervix was completely necrotic, and re-debridement was done, sent for culture insertion of hemo-vac in abdominal cavity Closure of the abdomen.
Her postoperative course involved close observation and repeated blood tests to ensure her safety. Histopathology confirmed gravid uterus diffusely ischemic cervical wall and acute nonspecific inflammation involving the cervix and the endometrial cavity no residual placental tissue was seen.
When fluid from the abdomen is sent for microbiological analysis during an operation, the goal is to determine if there is any infection present within the abdominal cavity. This fluid could be ascitic fluid, peritoneal fluid, or blood, depending on the context of the surgery and the concerns of the surgical team (culture negative).
Learning points
Interpretation of FHR: The importance of accurate interpretation of FHR patterns, particularly recognizing signs that indicate urgent fetal distress such as severe bradycardia.
Decision-Making Under Pressure: The case underscores the need for swift decision-making in emergency scenarios, especially when presented with critical signs like meconium-stained amniotic fluid and low FHR.
Resource Adaptation: It illustrates how to manage obstetric emergencies within the constraints of available resources, emphasizing the adaptation to context-specific limitations.
Case 2: Complex third stage of labor in a primigravida
Clinical background and presentation
A 20-year-old primiparous woman presented at full term for delivery. Her prenatal course was unremarkable with no significant medical or surgical history. Labor commenced naturally and progressed without complications. She delivered a healthy male infant with appearance, pulse, grimace, activity respiration (APGAR) scores 2 of 9 and 10 at 1 and 5 min, respectively.
Complication and initial management
During the third stage of labor, the placenta did not follow the delivery of the infant, leading to a diagnosis of retained placenta. This condition risks significant PPH and was initially managed with controlled cord traction and uterine massage. Despite these efforts, the placenta remained adherent.
Progression and surgical intervention
Subsequent moderate vaginal bleeding indicated escalating risk, prompting further diagnostic assessment. Imaging studies suggested the presence of PAS, specifically placenta increta, where the placenta invades deeply into the myometrium of the uterus.
Given the failure of conservative management and the high risk of severe hemorrhage, the decision was made to proceed with surgical intervention. The patient was transferred to the operating room, where a total abdominal hysterectomy was performed under general anesthesia. During the procedure, the placenta was manually removed, which was complicated by its deep attachment within the uterine wall.
Surgical outcomes and postoperative care
The surgery involved meticulous dissection and management of the uterine tissue to minimize blood loss and ensure complete removal of the placenta. The operation was successful, with controlled hemostasis and no immediate postoperative complications. The patient’s recovery was monitored intensively in the postoperative period, focusing on pain management, prevention of infection, and monitoring for signs of any post-surgical complications. Her recovery was uneventful, and she was discharged on the second day of post-delivery in stable condition.
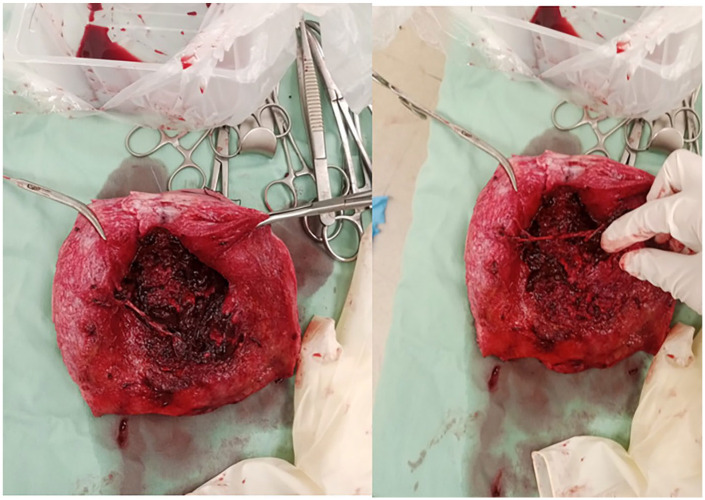
Histopathological confirmation
The removed placenta underwent histopathological examination, which confirmed the diagnosis of placenta increta. This finding was significant as it provided a clear explanation for the placenta’s abnormal adherence and the challenges encountered during manual removal (Figure 2).
Figure 2.
Intrauterine presentation of placenta increta: detailed pathological examination.
This case underscores the importance of prompt recognition and management of retained placenta and PAS. Effective management requires a coordinated approach involving obstetric maneuvers, surgical intervention, and vigilant postoperative care to mitigate associated risks and promote favorable maternal outcomes
Learning points
Importance of Pelvic Ultrasound in the Delivery Room: This case underscores the crucial role of pelvic ultrasound in identifying abnormal placental insertion, such as PAS disorders, particularly when the patient has not been followed prenatally at the institution. The use of ultrasound in the operating room provided essential diagnostic insights that were not available preoperatively.
Management of Unexpected Placental Disorders: The case highlights the necessity of being prepared for unforeseen complications. The intraoperative discovery of placenta increta necessitated immediate and effective surgical intervention under challenging circumstances.
Adapting Surgical Strategy Based on Intraoperative Findings: The need for flexibility in surgical planning and the ability to adapt quickly when unexpected findings, such as deeply adherent placenta, are encountered. This was critical in preventing severe complications like massive hemorrhage.
Cross-disciplinary Collaboration: The case illustrates the benefit of having a cross-disciplinary team readily available, especially in scenarios where the patient’s complete prenatal history and follow-up are lacking. Collaboration among obstetricians, radiologists, and surgical teams is essential to manage such complex cases effectively.
Documentation and Communication: Emphasizes the importance of thorough documentation and clear communication during the transition of care, particularly when dealing with patients who have not been previously assessed at the facility. This ensures all team members are informed and prepared to handle the complexities of the case.
Case 3: Early pregnancy emergency in a high-risk multiparous woman
The third case involves a 31-year-old woman, gravida 5, para 4, with a complex obstetric history due to four previous cesarean sections. Her current pregnancy, initially without complications, changed dramatically when she presented with acute lower abdominal pain.
The patient’s ordeal began the night before her emergency room (ER) visit, when she sought medical advice for her symptoms. At that time, she was mistakenly told she had a missed abortion and subsequently took an unidentified medication. She firmly denied using cytotec, a medication known for inducing labor. Despite this, her condition did not improve, prompting her to seek further medical help.
In the ER, she was in noticeable distress, suffering from continuous pelvic pain that did not respond to antispasmodic treatment. Her initial physical examination revealed a soft abdomen with mild suprapubic tenderness, but no active vaginal bleeding was observed. Her vital signs were stable: a pulse rate of 80 beats per minute, blood pressure at 120/80 mmHg, temperature at 36.8°C, and respiratory rate of 20 breaths per minute. A speculum examination showed a closed cervix.
A bedside ultrasound was conducted immediately, revealing a single intrauterine pregnancy. Alarmingly, no FHR was detectable, a concerning finding. Despite this, her hemoglobin level was 10.1, and her blood group O was positive, which was somewhat reassuring in terms of her immediate physical health.
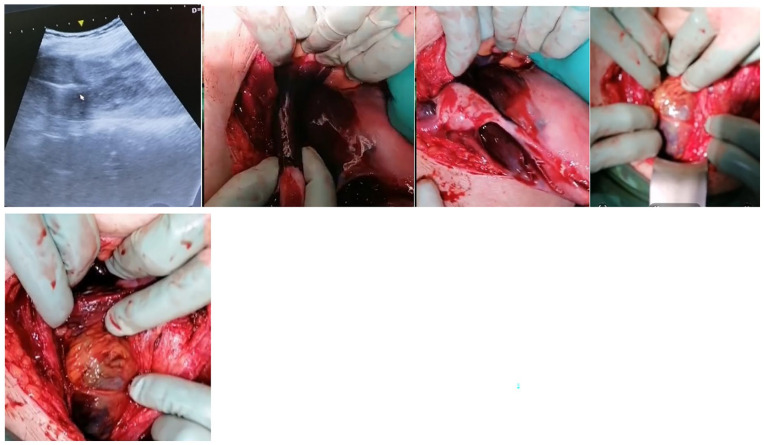
While waiting for further tests, including a complete blood count and blood grouping, her condition evolved. She began to experience minimal vaginal bleeding along with persistent pelvic pain. A repeat bedside ultrasound reaffirmed the initial findings, showing no improvement in the fetal status and a persistently soft abdomen (Figure 3).
Figure 3.
Intrauterine pregnancy with non-viable fetus near previous scar accompanied by hematoma and intra-abdominal hemorrhage.
Given her stable vital signs and the minimal nature of her vaginal bleeding, the initial plan was to monitor her in the ER for a brief period before considering discharge. This decision, made after a careful reassessment by the OB resident in charge and consultation with the attending physician on call, included scheduling an official follow-up ultrasound in the outpatient department for the following day.
However, the situation rapidly and severely deteriorated. As preparations for her discharge were underway, the patient developed intense vaginal bleeding, hypotension, and a rapid heart rate, marking a drastic shift from her previously stable condition. This change necessitated an immediate and urgent reassessment. She now exhibited moderate vaginal bleeding, as indicated by a fully soaked blue pad, a heart rate accelerated to 130 beats per minute, and a blood pressure dropped to a concerning 80/50 mmHg.
In response to this acute decline, the medical team acted swiftly. Two intravenous lines were inserted, and she received 2 l of normal saline solution and 1 g of tranexamic acid (Exacyl) to control the bleeding. Essential laboratory tests were conducted, and the blood bank was urgently contacted to prepare two units of packed red blood cells (PRBCs).
A subsequent physical examination revealed a distressing state. The patient appeared pale and drowsy, in stark contrast to her earlier alertness, and displayed guarding behavior over her abdomen, which now showed signs of severe generalized tenderness—a concerning indication of potential intra-abdominal pathology.
A repeat bedside ultrasound in view of her rapidly changing clinical picture revealed the gestational sac still within the uterus but confirmed the absence of fetal heart activity. A new, alarming finding was also noted—a heterogeneous, echogenic, encapsulated structure above the anterior uterine wall, extending from the isthmus to the uterine fundus and laterally toward the right side (Figure 3).
The encapsulated structure observed above the anterior uterine wall, extending from the isthmus to the uterine fundus and laterally toward the right side, raised concerns about possible complications related to her previous cesarean sections, such as a uterine rupture or abnormal placental attachment.
Recognizing the seriousness of the situation, a multidisciplinary consultation was sought, involving both high-risk pregnancy and placenta accreta specialists. Following in-depth discussions, the team decided to proceed with a life-saving dilation and curettage (D&C). The patient’s condition was increasingly precarious. In an attempt to control the bleeding, a uterine Foley catheter was inserted and inflated with 50cc. This provided only temporary relief, as the Foley catheter spontaneously ruptured after 20 min. It was then reinserted and inflated with 90cc. Despite these efforts, the patient’s bleeding persisted, and she became pulseless. In response to her rapidly worsening condition, a repeat bedside ultrasound was conducted (Figure 4).
Figure 4.
Severe intra-abdominal hemorrhage, adhesions, and uterine rupture: comprehensive surgical findings.
Consent for the procedure and a potential hysterectomy were obtained from both the patient and her family, highlighting the critical nature of her condition. In the preoperative phase, her vital signs indicated some improvement following initial resuscitation efforts: her blood pressure was 100/80 mmHg, and her heart rate was 102 beats per minute. However, these signs still reflected a critical state.
During the operation, the team encountered severe bleeding within the abdomen and significant adhesions between the abdomen and uterus, complicating the hysterectomy (Figure 4). The retracted gravid uterus exhibited hemorrhagic areas and a partially ruptured isthmus, thankfully free of residual placental tissue. Additionally, the cervix displayed focal intraparietal hemorrhage.
Learning points
Routine Ultrasound Screening Post-Cesarean: This case highlights the critical importance of routine ultrasound assessments for women with previous cesarean sections to monitor the integrity of the cesarean scar in subsequent pregnancies. Such screenings are essential for early identification of potential complications, like scar pregnancies, which can have severe outcomes if not promptly managed.
Continuity of Care: The case illustrates the significant advantages of having a patient follow-up and deliver at the same institution where her prenatal history and previous surgical details are well-documented and readily available. This continuity allows for more personalized and informed care, potentially reducing the risk of complications.
Risk Assessment in High-Risk Pregnancies: Emphasizes the need for heightened vigilance and proactive management strategies in high-risk patients, particularly those with a history of multiple cesareans. Early and frequent assessments can help in making timely decisions to ensure the safety of both the mother and fetus.
Cross-disciplinary Expertise: This scenario underscores the importance of a multidisciplinary approach involving obstetricians, radiologists, and emergency care specialists to handle complex cases effectively. Collaboration is crucial, especially in emergency settings where rapid decision-making is needed.
Patient Education and Precautionary Measures: Educating patients about the potential risks associated with multiple cesarean sections and the importance of regular check-ups can empower them to seek timely medical advice. This is particularly crucial for recognizing unusual symptoms that might indicate underlying complications.
Case 4: PPH and uterine rupture in a multiparous woman
In an unexpected turn of events, a 37-year-old woman, Gravida 7 Para 6, with a history of straightforward, uncomplicated deliveries, found herself facing a life-threatening complication following the birth of her seventh child. This case unfolded at 38 weeks of gestation when she arrived at the hospital with SROM. Her pregnancy had been complicated by gestational diabetes, managed with metformin, but otherwise uneventful. Upon admission, her vital signs were stable, and her non-stress test was reassuring—category I, reactive, and showing no contractions.
Labor was induced with cytotec, and after enduring contractions for 6 h, she delivered a healthy baby girl. The delivery was soon overshadowed by a critical complication. Despite the absence of lacerations on her vagina, cervix, and paraurethral areas, she began experiencing PPH. The bleeding was significant, estimated at about 1000cc, indicative of uterine atony—a condition where the uterus fails to contract effectively after delivery, leading to hemorrhage.
The medical team responded swiftly, administering a combination of PITOCIN, CYTOTEC, and EXACYL, along with bilateral uterine massage in an effort to manage the hemorrhage and stabilize her condition. Initially, this intervention seemed effective; the patient’s vital signs stabilized, and she began to recover, showing signs of normal post-delivery activities like ambulating, breastfeeding, and tolerating oral intake.
However, 3 h post-delivery, the situation deteriorated. She reported heavy vaginal bleeding; her blood pressure plummeted to 80/60 mmHg, and her hemoglobin dropped to 8.9. An examination revealed the uterus was still atonic, not contracting as it should. The team escalated their response: two intravenous lines were placed, and methergine was administered, along with preparations for a possible blood transfusion. The blood bank was notified, and two units of pRBCs and fresh frozen plasma (FFPs) were cross-matched.
Despite these efforts, another episode of heavy vaginal bleeding occurred 2.5 h later, accompanied by hypotension and tachycardia. The situation was becoming increasingly dire. A uterine Foley was inserted and inflated with 80cc in an attempt to tamponade the bleeding. This measure, however, provided only temporary relief, as the Foley ruptured spontaneously after 50 min, necessitating its reinsertion with inflation of 90cc. Unfortunately, the bleeding continued, and the patient’s pulse became undetectable.
At this critical juncture, the medical team initiated a blood transfusion with 2 units of red blood cells (RBCs) and 2 units of FFPs, alongside the administration of Levophed, a vasopressor to maintain blood pressure. An urgent decision for a cesarean hysterectomy was made, given the severity of her condition and the continued uncontrolled bleeding.
In the operating room, the surgical team discovered a hematoma in the left lower segment of the uterus at the level of the uterine artery, extending to the retroperitoneal area. This was likely the source of the bleeding. While exploring the hematoma, they identified a 3 × 4 cm uterine perforation (Figure 5).
Figure 5.
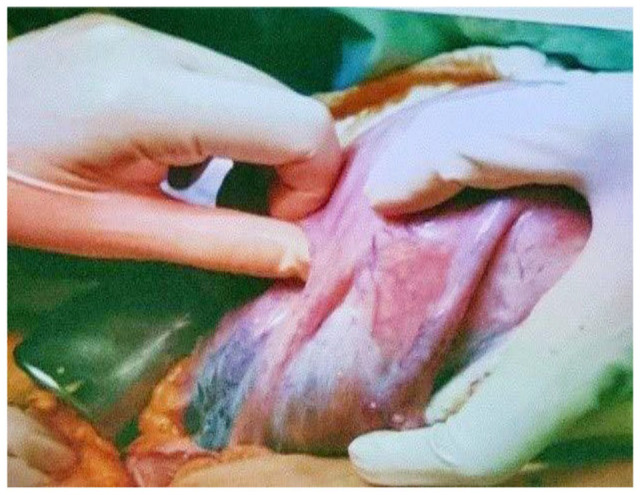
Retroperitoneal hematoma linked to uterine perforation: A 3 × 4 cm pathological presentation.
The patient received an additional 4 units of RBCs and 3 FFPs intraoperatively, and the estimated blood loss was 1.2 l.
Following surgery, she was transferred to the ICU for recovery. The pathology report of the specimen described a gravid uterus with a hemorrhagic wall and noted vascular thrombosis but no residual placental tissue or other abnormalities. Her postoperative period in the ICU was challenging. Her hemoglobin levels initially increased, but her platelet count decreased, necessitating the continuation of FFP transfusions. She developed suspected diabetic ketoacidosis, indicated by a high blood sugar level and a low bicarbonate level, which was managed with intravenous insulin until her blood sugar levels normalized.
The patient remained intubated and on Levophed for some time due to her tachycardia and hypertension. Her abdomen was soft but mildly distended, and her vaginal pad was soaked in blood, with some oozing noted around the drain insertion site, though no active bleeding was observed. A chest X-ray showed some congestion, and her creatinine levels were slightly elevated, indicating some strain on her kidneys. Her troponin levels were also elevated postoperatively but later decreased.
The patient’s condition gradually improved. She was extubated, and her nasogastric tube was removed. She began a soft diet two days post-operation and was discharged on the fourth postoperative day.
Learning points
Prompt Recognition and Management of PPH: This case exemplifies the importance of early recognition and immediate management of PPH. Recognizing the signs of PPH quickly and initiating treatment protocols promptly are crucial to prevent severe outcomes.
Diagnostic Assessment to Identify the Cause of Hemorrhage: Effective management of PPH hinges on accurately diagnosing its cause. In this case, the rapid identification of uterine atony as a contributing factor enabled targeted interventions that are specific to this condition, such as the use of uterotonic agents.
Use of Multimodal Interventions: The case highlights the necessity for employing a multimodal approach to manage severe PPH. This includes the use of pharmacologic agents (Pitocin, Cytotec), mechanical methods (uterine massage, Foley balloon tamponade), and preparedness for surgical interventions if needed.
Preparedness for Rapid Escalation: Stressing the importance of being prepared to escalate care swiftly if initial interventions fail. This involves having blood products ready for transfusion, access to emergency surgical intervention, and the ability to perform a hysterectomy if necessary.
Interdisciplinary Teamwork in Emergency: Demonstrates the effectiveness of an interdisciplinary team, including obstetricians, anesthesiologists, and surgical staff, working together under pressure. Quick and coordinated actions are essential to manage complex cases of PPH efficiently.
Continuous Monitoring and Post-Treatment Care: Emphasizing the need for vigilant post-treatment monitoring in PPH cases to observe for signs of recurrence or complications. Continuous assessment helps ensure that the patient stabilizes and recovers without additional adverse events.
Discussion
The four cases presented provide a compelling insight into the spectrum of complexities and emergencies encountered in obstetrics, highlighting critical decision-making, timely interventions, and multidisciplinary approaches. This discussion will juxtapose these cases with existing literature to illuminate the broader context of obstetric care.
The gravity of fetal bradycardia and the imperative of timely cesarean sections
The first case, involving fetal bradycardia necessitating an emergency cesarean section, represents a critical intersection of fetal distress and maternal care. Fetal bradycardia, particularly in the context of thick meconium, is a well-documented emergency that demands immediate intervention. 3 In addition to fetal bradycardia and the presence of meconium, another critical factor complicating the delivery in your first case is that the cervix was not adequately prepared or “ready” for vaginal delivery. This situation, often referred to as cervical ripening failure or an “unfavorable cervix,” can significantly delay labor progression and necessitates consideration for a cesarean section.
In clinical practice, the interpretation of meconium-stained amniotic fluid as a sign of fetal distress is usually considered alongside other clinical findings. Additional supporting tests and monitoring techniques are used to assess the condition of the fetus more accurately:
FHR Monitoring: Continuous electronic fetal monitoring is crucial. Patterns such as bradycardia (as in your case), tachycardia, or other abnormalities like variable or late decelerations can provide more direct evidence of fetal compromise or distress.
The literature consistently underscores the need for rapid cesarean delivery in such instances to mitigate risks of neonatal hypoxia and its potential long-term neurological impacts. 4 The delay experienced in this case, due to anesthesia issues, highlights the challenges faced in emergency settings. Such delays, though critical, are sometimes unavoidable and require swift adaptation by the medical team. This aligns with studies. 5 who discuss the impact of perioperative factors on maternal and neonatal outcomes in emergency cesarean sections. The risk of post-cesarean hysterectomy may be increased by certain anatomical distortion conditions. 6
Complications in third stage of labor
The second case’s focus on complications in the third stage of labor, particularly retained placenta and PAS, resonates with the growing body of research on this subject. The prevalence and risk factors for PAS have been increasingly recognized in recent literature, especially in the context of rising cesarean section rates. 6 The need for hysterectomy, as seen in this case, underscores the potential severity of PAS and aligns with the current understanding that early and aggressive intervention can be lifesaving and fertility-preserving. 7
Early pregnancy emergency in a high-risk multiparous woman
The third case illustrates the complexities inherent in managing early pregnancy complications in patients with histories of multiple cesarean deliveries. The literature recognizes that such patients face elevated risks, including abnormal placentation, uterine rupture, and increased complications in subsequent pregnancies. 8 These risks necessitate vigilant monitoring and readiness for emergency intervention, as underscored by recent studies. 9
Among the causes of severe hemorrhage in these patients, while common issues like placenta previa and accreta are frequently noted, it is also crucial to consider less frequent but equally challenging conditions that may require urgent hysterectomy. For instance, conditions such as vasa previa and uterine artery rupture, although rare, can lead to life-threatening bleeding and necessitate immediate surgical response to mitigate maternal risk. A detailed examination of these less frequent causes is provided in a comprehensive review 10 which highlights the importance of considering a broad spectrum of potential complications in such high-risk scenarios. This perspective is essential for developing a proactive approach to management, ensuring that treatment strategies are as inclusive and effective as possible.
PPH following spontaneous delivery
The fourth case highlights the critical challenges associated with PPH due to uterine atony, a prevalent issue that continues to be a leading cause of maternal morbidity and mortality worldwide. 11 In managing this severe PPH, the use of uterotonic agents and surgical interventions such as cesarean hysterectomy were implemented, aligning with recommended strategies found in current obstetric research. 12 The complexities of treating uterine atony and the necessity for intensive surgical responses underscore the persistent difficulties faced in obstetric care and are consistent with the known challenges in managing severe PPH.13,14
To further comprehend the evolving landscape of PPH management, it is beneficial to consult recent studies that delve into the efficacy of various interventions. One such study, 15 offers valuable insights into newer approaches and outcomes related to the management of PPH following spontaneous deliveries. This work not only expands on traditional methods but also explores the implications of emerging techniques and their roles in enhancing patient safety and outcomes. By incorporating these findings, practitioners can better understand the full spectrum of strategies available for addressing this life-threatening condition, thereby improving the standards of care and potentially reducing global maternal mortality rates.
In all four cases, a common thread is the necessity for rapid, decisive action in the face of obstetric emergencies. These narratives demonstrate the critical importance of aligning clinical practice with evolving evidence and guidelines to improve maternal and neonatal outcomes. The discussion of these cases in the context of existing literature also emphasizes the ongoing need for research and education in obstetrics, particularly in the management of high-risk pregnancies and emergency situations.
Patient follow-up limitations
A significant limitation of our study is the lack of comprehensive long-term follow-up data for the patients. While immediate postoperative outcomes, such as the management of diabetic ketoacidosis and early recovery indicators like Apgar scores, 1 are well-documented, there is scant information on the longer-term health of the mothers and the developmental progress of the newborns.
The short-term focus restricts our understanding of the long-term effects of critical interventions, such as total abdominal hysterectomy and emergency cesarean sections, on the mothers’ future reproductive and mental health, as well as the infants’ neurodevelopmental outcomes.
Incorporating structured long-term follow-up into future studies would provide deeper insights into the full impact of obstetric emergencies on maternal and neonatal health, enhancing treatment strategies and overall care.
Conclusions
In conclusion, these cases highlight the diverse array of emergencies and complications that can arise in obstetrics, emphasizing the need for a multidisciplinary approach, rapid decision-making, and readiness for intervention. These narratives underscore the importance of aligning clinical practice with current research and guidelines, continually adapting to emerging evidence to improve maternal and neonatal outcomes. This approach is crucial in ensuring holistic care that addresses both the immediate clinical needs and the long-term implications for the patient’s health and quality of life.
Acknowledgments
We express our deepest gratitude to Hamza Nakib for his significant contributions to the design and methodology of this study. His dedication and meticulous attention to detail have been invaluable, and his collaborative spirit has greatly enhanced our work. We sincerely thank him for his hard work and commitment throughout the research process.
Footnotes
Author contributions: G.Y. Approved the final version of the manuscript and provided overall supervision of the project; N.M. Hassan Barakat: Both Dr. Madi and Dr. Barakat supervised the project, ensuring adherence to ethical and research standards; C.E.H. Provided supervision and critical revisions of the manuscript, contributing to the theoretical framework of the study; H.B. Gathered data essential for the study and provided supervision throughout the project. His efforts ensured the integrity and accuracy of the data collection process and contributed significantly to the overall management and oversight of the research activities; J.A.H. Offered supervision and was instrumental in the design and implementation phases of the research; H.N. Collaborated closely with other team members on the design and methodology of the study; K.G. Was primarily responsible for the design, implementation, writing, and presentation of the research, contributing to 90% of the work.
Data availability statement: The data supporting the findings of this study are available upon request from the corresponding author.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval statement: Ethical approval to report this case series was obtained from approved by the local institutional review board RAFIC HARIRI UNIVERSITY HOSPITAL and by chief DR. GEORGES YARED
Informed consent statement: Written informed consent was obtained from all the subjects for publication of this case report.
ORCID iD: Kariman Ghazal  https://orcid.org/0000-0002-3199-631X
https://orcid.org/0000-0002-3199-631X
References
- 1. Pettersen S, Falk RS, Vangen S, et al. Peripartum hysterectomy due to severe postpartum hemorrhage: a hospital-based study. Acta Obstet Gynecol Scand 2022; 101(7): 819–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Apgar V. A proposal for a new method of evaluation of the newborn infant. Anesth Analg 1953; 32(4): 260–267. [PubMed] [Google Scholar]
- 3. Batra AS, Balaji S. Fetal arrhythmias: Diagnosis and management. Indian Pacing Electrophysiol J 2019; 19(3): 104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang L, Liu C, Wang X, et al. The impact of general anesthesia on the outcomes of preterm infants with gestational age less than 32 weeks delivered via cesarean section. Front Pharmacol 2024; 15: 1360691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hruban L, Janků P, Jordanova K, et al. The effect of transient fetal bradycardia and other heart rate changes during and after external cephalic version on perinatal outcomes. Eur J Obstet Gynecol Reprod Biol 2020; 245: 39–44. [DOI] [PubMed] [Google Scholar]
- 6. Silver RM, Branch DW. Placenta Accreta Spectrum. N Engl J Med 2018; 378(16): 1529–1536. [DOI] [PubMed] [Google Scholar]
- 7. Escobar MF, Gallego JC, Nasner D, et al. Management of abnormal invasive placenta in a low- and medium-resource setting, Best Practice & Research Clinical Obstetrics & Gynaecology, 2021; 72: 117–128. [DOI] [PubMed] [Google Scholar]
- 8. Çintesun E, Al RA. The effect of increased number of cesarean on maternal and fetal outcomes. Ginekol Pol 2017; 88(11): 613–619. [DOI] [PubMed] [Google Scholar]
- 9. Blondon M, Martinez de Tejada B, Glauser F, Righini M, et al. Management of high-risk pulmonary embolism in pregnancy. Thromb Res 2021; 204: 57–65. [DOI] [PubMed] [Google Scholar]
- 10. Passerini I, Marasciulo F, Prefumo F, et al. Treatment of early cesarean scar pregnancy with double balloon catheter: a systematic review of the literature. Clin Exp Obstet Gynecol 2023; 50(10): 222. [Google Scholar]
- 11. Thawal V, Kolate DS, Patvekar MM, et al. Study of management of postpartum hemorrhage and its complications. Int J Reprod Contracept Obstet Gynecol 2019; 8(5): 1790–1794 [Google Scholar]
- 12. Gallos ID, Williams HM, Price MJ, et al. Uterotonic agents for preventing postpartum haemorrhage: a network meta-analysis. Cochrane Database Syst Rev 2018; 4(4): CD011689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Butwick A, Lyell D, Goodnough L. How do I manage severe postpartum hemorrhage? Transfusion 2020; 60(5): 897–907. [DOI] [PubMed] [Google Scholar]
- 14. Ferrari F, Ferrari FA, Negri B, et al. Uterine torsion and intrauterine growth restriction: case report and systematic literature review. J Obstet Gynaecol Res 2021; 47(12): 4224–4231. [DOI] [PubMed] [Google Scholar]
- 15. Ferrari FA, Garzon S, Raffaelli R, et al. Tranexamic acid for the prevention and the treatment of primary postpartum haemorrhage: a systematic review. J Obstet Gynaecol 2022; 42(5): 734–746. [DOI] [PubMed] [Google Scholar]