Abstract
Background
With survival rates of critical illness increasing, quality of life measures are becoming an important outcome of ICU treatment. Therefore, to study the impact of critical illness on quality of life, we explored quality of life before and 1 year after ICU admission in different subgroups of ICU survivors.
Methods
Data from an ongoing prospective multicenter cohort study, the MONITOR-IC, were used. Patients admitted to the ICU in one of eleven participating hospitals between July 2016 and June 2021 were included. Outcome was defined as change in quality of life, measured using the EuroQol five-dimensional (EQ-5D-5L) questionnaire, and calculated by subtracting the EQ-5D-5L score 1 day before hospital admission from the EQ-5D-5L score 1 year post-ICU. Based on the minimal clinically important difference, a change in quality of life was defined as a change in EQ-5D-5L score of ≥ 0.08. Subgroups of patients were based on admission diagnosis.
Results
A total of 3913 (50.6%) included patients completed both baseline and follow-up questionnaires. 1 year post-ICU, patients admitted after a cerebrovascular accident, intracerebral hemorrhage, or (neuro)trauma, on average experienced a significant decrease in quality of life. Conversely, 11 other subgroups of ICU survivors reported improvements in quality of life. The largest average increase in quality of life was seen in patients admitted due to respiratory disease (mean 0.17, SD 0.38), whereas the largest average decrease was observed in trauma patients (mean -0.13, SD 0.28). However, in each of the studied 22 subgroups there were survivors who reported a significant increase in QoL and survivors who reported a significant decrease in QoL.
Conclusions
This large prospective multicenter cohort study demonstrated the diversity in long-term quality of life between, and even within, subgroups of ICU survivors. These findings emphasize the need for personalized information and post-ICU care.
Trial registration: The MONITOR-IC study was registered at ClinicalTrials.gov: NCT03246334 on August 2nd 2017.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-024-05036-5.
Keywords: Quality of life, Critical care outcomes, Prognosis, Patient-reported outcome measures
Background
ICU survivors’ quality of life (QoL) is generally lower than that of the general population [1]. Additionally, with survival rates of critical illness increasing, patient reported outcomes, such as QoL, are becoming an important factor in decisions regarding ICU treatment [2–4]. However, as most studies do not take pre-ICU QoL into account, it is unknown to what extent this reduced QoL is attributable to critical illness [5].
To study the long-term impact of critical illness and ICU treatment on patient outcomes, the MONITOR-IC study was initiated in the Netherlands. This multicenter prospective cohort study provides both a baseline measurement and follow-up data up to 5 years after ICU admission. This study has shown that physical, mental, and cognitive symptoms after ICU discharge can negatively affect patients’ QoL [6].
However, due to the heterogeneity of the ICU population, general data alone may not be sufficient. By gaining insight into the long-term outcomes of subgroups of ICU survivors, we can better inform patients with different characteristics about their expected long-term outcomes after an ICU admission. This may also facilitate the incorporation of long-term outcomes, such as QoL, in ICU treatment.
Therefore, the aim of this study was to explore QoL before and 1 year after ICU admission in different subgroups of ICU survivors.
Methods
Study design
The MONITOR-IC study, an ongoing multicenter prospective cohort study (ClinicalTrials.gov: NCT03246334, registered on August 2nd 2017), was approved on August 23rd 2016 by the research ethics committee of the Radboud university medical center, the Netherlands (2016–2724) and conducted in accordance with the declaration of Helsinki. Each participant, or their legal representative, provided written informed consent [7] . This study was reported in line with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline for cohort studies (E-Appendix 1) [8].
Study population
Patients were included if they were 16 years of age or older and admitted for ≥ 12 h to the ICU of one of the eleven participating hospitals between July 2016 and June 2021. Patients were excluded if they had a short life expectancy (≤ 48 h), or did not speak the Dutch language.
Data collection
Patients were asked to complete self-administered paper-based or online questionnaires regarding their health status before hospital admission. If patients were unable to fill in the questionnaires themselves, proxies were asked to perform this task. When possible, elective surgical patients received the questionnaires preoperatively. Other patients, or their proxies, received the questionnaires during admission and were asked to fill in the questionnaires as soon as possible, recalling their QoL on the day before hospital admission.
1 year after ICU admission, patients received a paper-based or online follow-up questionnaire regarding, among others, QoL. In case of non-response, study participants received two reminders.
Data on admission type, admission diagnosis, and co-morbidities were retrieved from the Dutch National Intensive Care Evaluation registry [9, 10].
Outcome
Outcome was defined as change in QoL, measured using the EuroQol five-dimensional (EQ-5D-5L) questionnaire, and calculated by subtracting the pre-admission EQ-5D-5L index score from the EQ-5D-5L index score 1 year after ICU admission [11]. The EQ-5D-5L questionnaire is a validated questionnaire and is commonly used for measuring health-related QoL after critical illness [12–14]. Each of its five questions represents a dimension of health-related QoL: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has five levels, ranging from no problems (1) to severe problems (5). The Dutch EQ-5D-5L index ranges from -0.446 to 1, with a higher score indicating a better health-related QoL [15]. The reference value of the Dutch general population aged ≥ 40 years is 0.85 [15].
Considering that previous studies have identified a minimal clinically important difference (MCID) of 0.08, an improvement in QoL was defined as an increase in EQ-5D-5L index score of ≥ 0.08, a deterioration in QoL was defined as a decrease of ≥ 0.08, and an unchanged QoL was defined as a delta EQ-5D-5L index score < 0.08 [16, 17].
Subgroups
Patients were grouped by their primary admission diagnosis, using the Acute Physiology and Chronic Health Evaluation (APACHE) IV diagnosis system, resulting in 6 main groups and 22 subgroups, based on previous studies and expert opinion [1, 18–22]. The list of diagnoses can be found in Table E1.
Statistical analysis
Only ICU survivors who completed both baseline and 1-year EQ-5D-5L questionnaires were included in the analyses. Descriptive statistics were performed to assess differences between responders and non-responders, using the chi-square test, independent-sample t-test, or Wilcoxon rank sum test, whenever appropriate. Continuous data were presented as means with standard deviation (SD) or medians with first and third quartile expressed as interquartile range (IQR), depending on their distribution. Categorical data were presented as numbers and percentages.
Since not all data were normally distributed, statistical differences between EQ-5D-5L index scores before hospital admission and 1 year after ICU admission were assessed using the Wilcoxon signed ranks test.
A p-value of < 0.05 was considered statistically significant for all analyses. Analyses were performed with R software, version 3.6.2 (R Foundation for Statistical Computing).
Results
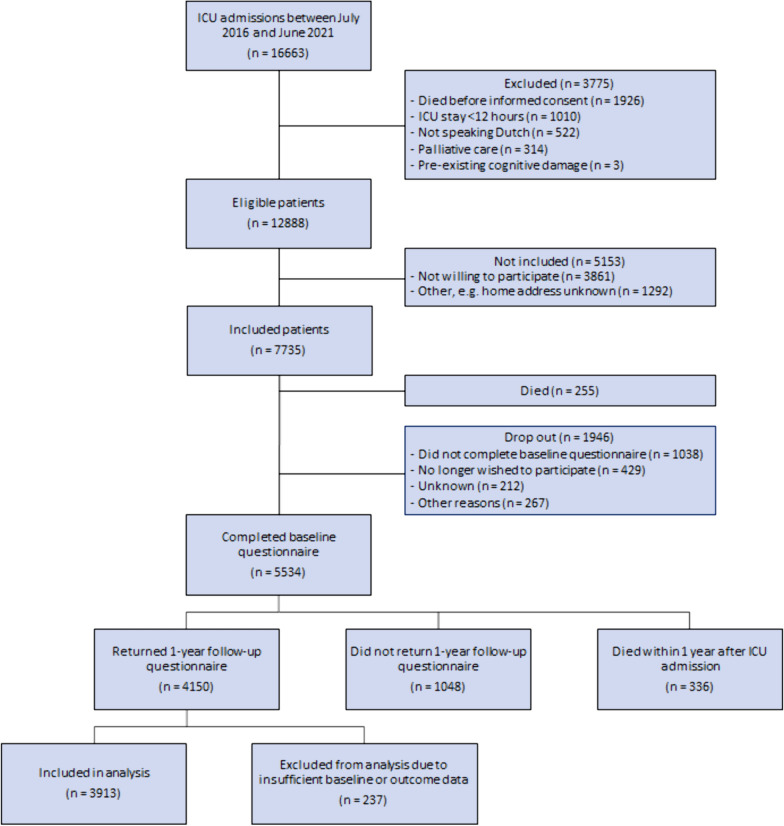
Of 12888 eligible patients, 7735 (60.0%) patients were included, of whom 5534 (71.5%) responded to the baseline questionnaire. 5198 (93.9%) patients survived until 1 year after ICU, of whom 3913 (75.3%) completed both baseline and follow-up questionnaires, and were therefore included in analysis (Fig. 1).
Fig. 1.
Flowchart inclusion procedure
The non-responders to the 1-year follow-up questionnaire (n = 1048) differed significantly from the responders. Among others, non-responders were younger, had more comorbidities and reported a lower pre-admission QoL (Table E2).
The age of included patients varied between groups with the youngest group being patients admitted after trauma (mean 53.9, SD 18.3) and the oldest group consisting of patients admitted after cardiovascular surgery (mean 66.2, SD 9.3) (Table 1). This variability was also seen in the number of patients with comorbidities, with the prevalence of chronic obstructive pulmonary disease ranging from 2.7% in patients admitted due to trauma, to 17.8% in patients admitted due to respiratory disease. Patients admitted due to cardiovascular surgery had a short ICU length of stay (median 1.0 day, IQR 0.8–1.7) and hospital length of stay (median 8.4 days, IQR 6.4–11.6). In contrast, patients admitted due to a respiratory disease had a median ICU length of stay of 7.6 days (IQR 3.0–16.3) and median hospital length of stay of 16.5 days (IQR 9.0–28.5).
Table 1.
Patient characteristics
| Variable | Cardiovascular (n = 587) |
Cardiovascular surgery (n = 1464) |
Respiratory (n = 675) |
Neurological (n = 186) |
Trauma (n = 184) |
Other (n = 817) |
|---|---|---|---|---|---|---|
| Baseline questionnaire completed by proxy, n (%) | 67 (12.3) | 69 (5.1) | 46 (11.9) | 63 (34.2) | 55 (30.9) | 80 (10.5) |
| Sex: Female, n (%) | 197 (33.5) | 319 (21.8) | 217 (32.2) | 92 (49.5) | 54 (29.4) | 339 (41.5) |
| Age (yrs), mean (SD) | 62.6 (13.0) | 66.2 (9.3) | 61.3 (11.2) | 57.3 (14.9) | 53.9 (18.3) | 61.6 (13.9) |
|
Comorbidities, n (%) Chronic obstructive pulmonary disease Diabetes Chronic renal insufficiency Immunological insufficiency Cardiovascular insufficiency Metastasized neoplasm |
44 (7.5) 67 (11.4) 26 (4.4) 60 (10.2) 18 (3.1) 12 (2.0) |
103 (7.0) 214 (14.6) 27 (1.8) 42 (2.9) 58 (4.0) 2 (0.1) |
120 (17.8) 97 (14.4) 22 (3.3) 92 (13.6) 7 (1.0) 7 (1.0) |
8 (4.3) 21 (11.3) 2 (1.1) 19 (10.2) 3 (1.6) 2 (1.1) |
5 (2.7) 14 (7.6) 1 (0.5) 6 (3.3) 0 (0.0) 1 (0.5) |
36 (4.4) 76 (9.3) 36 (4.4) 111 (13.6) 12 (1.5) 103 (12.6) |
| Mechanical ventilation within 24 h of ICU admission, n (%) | 313 (53.3) | 1405 (96.0) | 473 (70.0) | 90 (48.4) | 118 (64.1) | 382 (46.8) |
| Vasoactive medication in first 24 h of ICU admission, n (%) | 334 (56.9) | 1165 (79.6) | 354 (52.4) | 72 (38.7) | 72 (39.1) | 394 (48.2) |
| APACHE IV score, mean (SD) | 67.9 (29.8) | 53.2 (15.1) | 61.3 (18.2) | 47.5 (21.8) | 50.6 (20.7) | 49.4 (18.5) |
| ICU length of stay (days), median (IQR) | 2.1 (1.1–4.6) | 1.0 (0.8–1.7) | 7.6 (3.0–16.3) | 1.6 (0.9–3.4) | 1.9 (0.9–4.7) | 1.0 (0.9–2.1) |
| Hospital length of stay (days), median (IQR) | 11.6 (6.0–19.6) | 8.4 (6.4–11.6) | 16.5 (9.0–28.5) | 11.1 (5.7–21.8) | 11.2 (6.0–19.6) | 8.9 (6.1–13.7) |
The distribution of the EQ-5D-5L index scores before hospital admission and 1 year after ICU admission, and the distribution of the delta EQ-5D-5L index scores, are shown in Fig. E1.
Table 2 shows the changes in QoL 1 year after ICU for the different admission diagnoses. Of the 22 subgroups, 11 on average reported a clinically relevant improvement in QoL 1 year after ICU. In contrast, patients admitted to the ICU due to a cerebrovascular accident, intracerebral hemorrhage, trauma or neurotrauma, on average reported a decrease in QoL score. The largest average decrease in EQ-5D-5L index score was seen in trauma and neurotrauma patients (mean -0.13, SD 0.28), whereas the largest average increase was observed in patients admitted to the ICU due to COVID-19 (mean 0.18, SD 0.39).
Table 2.
Changes in quality of life 1 year after ICU for different subgroups of ICU patients
| Admission diagnosis | EQ-5D-5L index score before hospital admission Median (IQR) |
EQ-5D-5L index score 1 year after ICU admission Median (IQR) |
P value* | Delta EQ-5D-5L index score** Mean (SD) |
|---|---|---|---|---|
| Cardiovascular (n = 587, 15.0%) | 0.82 (0.59–0.96) | 0.82 (0.70–0.91) | < 0.01 | 0.07 (0.30) |
| - Sepsis/septic shock (n = 230) | 0.72 (0.45–0.88) | 0.78 (0.64–0.88) | < 0.001 | 0.11 (0.34) |
| - Hemodynamic instability (n = 168) | 0.85 (0.70–1.00) | 0.85 (0.76–1.00) | < 0.01 | 0.09 (0.31) |
| - Cardiac arrest (n = 117) | 1.00 (0.84–1.00) | 0.87 (0.74–1.00) | < 0.001 | -0.05 (0.19) |
| - Cardiac (n = 72) | 0.78 (0.60–0.85) | 0.81 (0.69–0.89) | 0.02 | 0.08 (0.24) |
| Cardiovascular surgery (n = 1464, 37.4%) | 0.83 (0.70–0.91) | 0.86 (0.78–1.00) | < 0.001 | 0.07 (0.22) |
| - Thoracic aortic aneurysm (n = 172) | 0.85 (0.74–0.91) | 0.81 (0.74–0.89) | 0.03 | -0.02 (0.21) |
| - Coronary artery bypass grafting (n = 650) | 0.85 (0.72–0.92) | 0.89 (0.79–1.00) | < 0.001 | 0.08 (0.22) |
| - Cardiac valve surgery (n = 506) | 0.81 (0.66–0.89) | 0.88 (0.78–1.00) | < 0.001 | 0.09 (0.23) |
| - Vascular surgery (n = 136) | 0.81 (0.66–0.89) | 0.84 (0.74–0.90) | < 0.01 | 0.07 (0.22) |
| Respiratory (n = 675, 17.2%) | 0.68 (0.31–0.88) | 0.81 (0.67–0.89) | < 0.001 | 0.17 (0.38) |
| - Obstructive pulmonary disease (n = 39) | 0.46 (0.17–0.70) | 0.64 (0.37–0.76) | < 0.01 | 0.16 (0.34) |
| - Pneumonia (n = 140) | 0.63 (0.30–0.81) | 0.73 (0.60–0.85) | < 0.001 | 0.15 (0.32) |
| - COVID-19 (n = 440) | 0.74 (0.33–0.89) | 0.84 (0.72–0.91) | < 0.001 | 0.18 (0.39) |
| - Other respiratory (n = 56) | 0.74 (0.30–0.88) | 0.79 (0.63–1.00) | 0.01 | 0.13 (0.43) |
| Neurological (n = 186, 4.7%) | 0.82 (0.55–0.91) | 0.80 (0.62–0.89) | 0.55 | 0.01 (0.36) |
| - Intracerebral hemorrhage (n = 67) | 0.89 (0.76–1.00) | 0.81 (0.63–0.88) | 0.05 | -0.08 (0.29) |
| - Cerebrovascular accident (n = 20) | 0.75 (0.62–0.86) | 0.75 (0.54–0.83) | 0.43 | -0.09 (0.42) |
| - Neurosurgery (n = 45) | 0.78 (0.42–0.88) | 0.73 (0.36–0.85) | 0.53 | 0.02 (0.38) |
| - Other neurological (n = 54) | 0.71 (0.45–0.91) | 0.84 (0.66–0.91) | < 0.01 | 0.15 (0.36) |
| Trauma (n = 184, 4.7%) | 1.00 (0.82–1.00) | 0.82 (0.61–0.89) | < 0.001 | -0.13 (0.28) |
| - Neurotrauma (n = 87) | 1.00 (0.85–1.00) | 0.84 (0.65–0.92) | < 0.001 | -0.13 (0.26) |
| - Other trauma (n = 97) | 1.00 (0.79–1.00) | 0.81 (0.57–0.89) | < 0.001 | -0.13 (0.29) |
| Other (n = 817, 20.9%) | 0.81 (0.60–0.89) | 0.82 (0.74–0.91) | < 0.001 | 0.08 (0.26) |
| - Metabolic or endocrine (n = 41) | 0.81 (0.63–0.89) | 0.80 (0.67–0.89) | 0.52 | 0.07 (0.32) |
| - Chest surgery (n = 110) | 0.82 (0.66–0.91) | 0.85 (0.78–0.98) | < 0.01 | 0.06 (0.21) |
| - Oncologic surgery (n = 385) | 0.81 (0.66–0.89) | 0.84 (0.74–0.92) | < 0.001 | 0.05 (0.23) |
| - Other (n = 281) | 0.74 (0.51–0.86) | 0.81 (0.70–0.89) | < 0.001 | 0.12 (0.29) |
*Comparison of EQ-5D-5L index score before hospital admission and EQ-5D-5L index score 1 year after ICU admission, using Wilcoxon signed rank test
**Clinically relevant changes in quality of life (≥ 0.08, based on MCID) are shown in bold
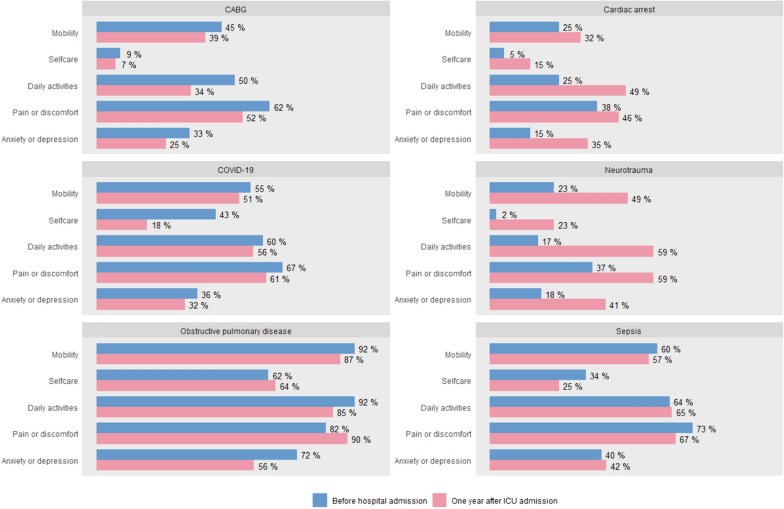
The lowest QoL 1 year after ICU admission was observed in the group admitted to the ICU due to obstructive pulmonary disease (EQ-5D-5L index score 0.64, IQR 0.37–0.76). This group also reported the lowest pre-admission QoL (EQ-5D-5L index score 0.46, IQR 0.17–0.70). Notably, before hospital admission 92.3% (n = 36) of these patients experienced limitations in their daily activities, while 82.1% (n = 32) experienced pain or discomfort. 1 year after ICU, this was true for 84.6% (n = 33) and 89.7% (n = 35), respectively. In contrast, before hospital admission, 2.3% (n = 2) of patients admitted due to neurotrauma experienced limitations in selfcare, while 17.2% (n = 15) experienced limitations in daily activities. 1 year after ICU admission, this increased to 23.0% (n = 20) and 58.6% (n = 51) respectively. The percentage of patients experiencing limitations in each dimension of the EQ-5D-5L, before and after ICU, is shown in Fig. 2 (for 6 subgroups) and Figure E2 (for the remaining subgroups).
Fig. 2.
Percentage of patients reporting limitations in each dimension of the EQ-5D-5L, before hospital admission and 1 year after ICU admission
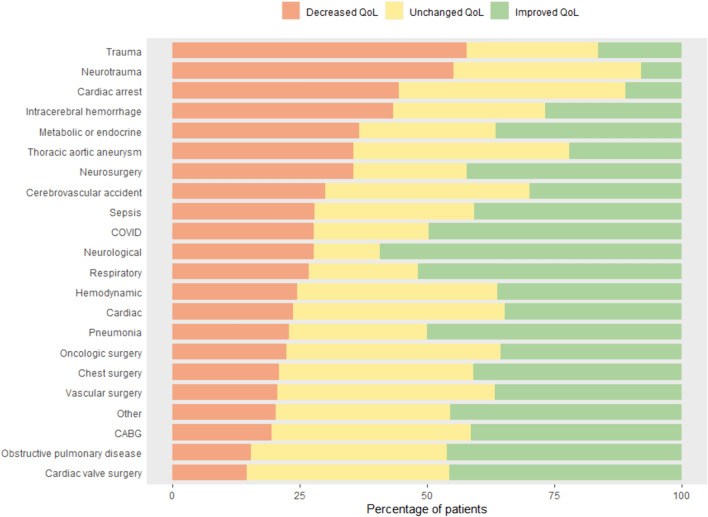
The highest QoL 1 year after ICU admission was seen in patients admitted after coronary artery bypass grafting (CABG) (EQ-5D-5L index score 0.89, IQR 0.79–1.00). In this group, 41.4% (n = 269) of patients reported an improvement in QoL 1 year after ICU, while after cardiac arrest this was true for 11.1% (n = 13) (Fig. 3). Moreover, after ICU admission due to a neurological trauma, more than half of patients (55.2%, n = 48) experienced a deterioration in QoL. However, in each of the studied 22 subgroups there were patients who reported a significant increase in QoL and patients who reported a significant decrease in QoL.
Fig. 3.
Percentage of patients experiencing an improved, unchanged or decreased quality of life 1 year after ICU admission, based on the MCID of 0.08
In general, 19.7% (n = 388) of patients admitted to the ICU after a planned surgery experienced a decrease in QoL, while 40.9% (n = 807) experienced an improvement in QoL. In contrast, after an acute ICU admission 31.0% (n = 601) reported a decrease in QoL, with a median EQ-5D-5L index score of 0.81 (IQR 0.67–0.89) 1 year post-ICU. For planned ICU admissions the median EQ-5D-5L index score 1 year post-ICU was 0.85 (IQR 0.75–1.00).
Discussion
This large prospective multicenter cohort study including 3913 ICU survivors, showed that there is substantial variability in long-term QoL following ICU admission, even within subgroups. 1 year after ICU, patients admitted after a cerebrovascular accident, intracerebral hemorrhage and trauma, including neurotrauma, on average experienced a significant decrease in QoL. Conversely, 11 other subgroups, such as patients admitted after cardiac valve surgery, reported improvements in QoL 1 year after ICU.
Subgroups with the largest average improvements in QoL were patients admitted due to COVID-19, obstructive pulmonary disease, pneumonia and neurological disease. This improvement may be explained by the subacute nature of these diseases, as patients are asked to recall their QoL on the day before hospital admission, at which time they might already have been experiencing symptoms.
Another possible explanation is the phenomenon called “response shift”, which has previously been described in, among others, patients suffering from stroke and spinal cord injury [23–25]. This response shift is caused by psychological adaptation, altering the relationship between functional disabilities and subjective wellbeing. This could explain the discrepancy between the high incidence of physical, mental and cognitive symptoms after ICU, collectively called post-intensive care syndrome (PICS), and the relatively small number of patients reporting a decrease in QoL 1 year after ICU admission [6]. A previous study, showing that only the mental component of PICS is associated with a self-reported unacceptable outcome of ICU treatment, affirms this discrepancy between functional outcomes and subjective wellbeing [26]. This exhibits the importance of incorporating subjective outcomes, such as QoL, in decision-making.
However, up to now, only a few studies have assessed long-term outcomes in subgroups of ICU patients [1, 22, 27]. Importantly, very few of these studies have taken pre-admission QoL into account, while pre-admission QoL has been identified as the most important predictor of long-term outcomes after ICU [13, 14, 28]. Moreover, pre-admission QoL helps us put the impaired QoL of ICU survivors into perspective, as shown by this study. Compared to the general Dutch population, many patients reported lower EQ-5D-5L index scores, both before hospital admission and 1 year after ICU admission [15]. This finding suggests that this reduced QoL is not attributable to critical illness, as their pre-ICU QoL was already impaired.
To the best of our knowledge, this is the first study that explored changes in QoL in multiple subgroups of ICU survivors. This can give ICU clinicians insight into the long-term outcomes of critical illness in specific patient groups and help them to better inform patients and their family members about the long-term outcomes of critical illness.
However, this study does have some limitations. First, in case of an unplanned ICU admission, patients were asked to recall their QoL on the day before hospital admission, possibly leading to recall bias. Moreover, patients may already have been ill at the time, in which case the pre-admission QoL is potentially not representative of the pre-morbid QoL. Future studies should consider different reference points when measuring pre-admission QoL. Additionally, up to 35% of baseline questionnaires, depending on the admission diagnosis, were completed by proxies. However, studies have demonstrated that proxies are able to reliably assess patients’ quality of life [29–31]. Second, there were significant differences between responders and non-responders, with non-responders reporting a lower pre-ICU QoL and having more comorbidities. Furthermore, certain subgroups of ICU patients were more often lost to follow-up, due to either death (e.g., patients admitted to the ICU after oncologic surgery) or non-response (e.g., patients admitted to the ICU after trauma). This response bias may have resulted in an overestimation of the QoL of survivors. The same may be true for patients who did not wish to participate or were not included for other reasons, possibly resulting in selection bias. However, a recent study shows that the MONITOR-IC study participants have similar characteristics to the general Dutch ICU population [32]. Third, the EQ-5D-5L measures a patient’s limitations in five areas, possibly not capturing all components of QoL. Nonetheless, the EQ-5D-5L is a validated instrument, frequently used for measuring health-related QoL, both in the general population and after critical illness [12, 23]. Moreover, the EQ-5D-5L is practical due to its concise nature, and its importance is illustrated by its presence in core outcome sets [33–35]. Fourth, subgroups were based on admission diagnosis, which resulted in intuitive and clinically relevant subgroups. However, future studies could consider using artificial intelligence to create subgroups, as this might result in more homogenous patient groups.
Conclusions
This large prospective multicenter cohort study demonstrated the diversity in long-term QoL between, and even within, subgroups of ICU survivors. These findings emphasize the need for personalized information and post-ICU care.
Supplementary Information
Acknowledgements
The authors thank the study participants and ICU staff of the participating hospitals (Canisius Wilhelmina Hospital, Bernhoven Hospital, Rijnstate Hospital, Amphia Hospital, Maas Hospital Pantein, Jeroen Bosch Hospital, Elkerliek Hospital, Maastricht University Medical Center, University Medical Center Utrecht, Zuyderland Medical Center, and Radboud university medical center) for their contribution to this study.
Abbreviations
- APACHE
Acute physiology and chronic health evaluation
- CABG
Coronary artery bypass grafting
- EQ-5D-5L
EuroQol five-dimensional
- ICU
Intensive care unit
- IQR
Interquartile range
- MCID
Minimal clinically important difference
- QoL
Quality of life
Author contributions
MZ, MvdB, KS, LP and JvdH designed the study. MZ, MvdB, JvdH, KS, SC, BW, TR, EE, IJ, CJ, SvS, AS and MvdW contributed substantially to the acquisition of data. LP performed the statistical analyses and drafted the manuscript. All other authors provided critical revisions of the article and approved the final version of the manuscript submitted for publication.
Funding
This work was funded by Radboud University Medical Center and Jeroen Bosch Hospital.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request. The data are not publicly available due to them containing information that could compromise research participant privacy.
Declarations
Ethics approval and consent to participate
The MONITOR-IC study (ClinicalTrials.gov: NCT03246334, registered on August 2nd 2017) was approved by the local ethics committee of the Radboud University Medical Center, CMO region Arnhem-Nijmegen, the Netherlands (2016–2724) and conducted in accordance with the declaration of Helsinki. Informed consent was obtained from all individual participants included in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Soliman IW, de Lange DW, Peelen LM, Cremer OL, Slooter AJ, Pasma W, Kesecioglu J, van Dijk D. Single-center large-cohort study into quality of life in Dutch intensive care unit subgroups, 1 year after admission, using EuroQoL EQ-6D-3L. J Crit Care. 2015;30(1):181–6. 10.1016/j.jcrc.2014.09.009 [DOI] [PubMed] [Google Scholar]
- 2.Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, Zawistowski C, Bemis-Dougherty A, Berney SC, Bienvenu OJ, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders’ conference. Crit Care Med. 2012;40(2):502–9. 10.1097/CCM.0b013e318232da75 [DOI] [PubMed] [Google Scholar]
- 3.Rowan KM, Jenkinson C, Black N. Health-related quality of life. In: Surviving intensive care: 2003// 2003. Springer, Berlin; 2003: 35–50
- 4.Akkermans A, Prins S, Spijkers AS, Wagemans J, Labrie NHM, Willems DL, Schultz MJ, Cherpanath TGV, van Woensel JBM, van Heerde M, et al. Argumentation in end-of-life conversations with families in Dutch intensive care units: a qualitative observational study. Intensive Care Med. 2023;49:421–33. 10.1007/s00134-023-07027-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azoulay E, Vincent JL, Angus DC, Arabi YM, Brochard L, Brett SJ, Citerio G, Cook DJ, Curtis JR, Dos Santos CC, et al. Recovery after critical illness: putting the puzzle together-a consensus of 29. Crit Care. 2017;21(1):296. 10.1186/s13054-017-1887-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geense WW, Zegers M, Peters MAA, Ewalds E, Simons KS, Vermeulen H, van der Hoeven JG, van den Boogaard M. New physical, mental, and cognitive problems 1 year after ICU admission: a prospective multicenter study. Am J Respir Crit Care Med. 2021;203(12):1512–21. 10.1164/rccm.202009-3381OC [DOI] [PubMed] [Google Scholar]
- 7.Geense W, Zegers M, Vermeulen H, van den Boogaard M, van der Hoeven J. MONITOR-IC study, a mixed methods prospective multicentre controlled cohort study assessing 5-year outcomes of ICU survivors and related healthcare costs: a study protocol. BMJ Open. 2017;7(11):e018006. 10.1136/bmjopen-2017-018006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van de Klundert N, Holman R, Dongelmans DA, de Keizer NF. Data resource profile: the dutch national intensive care evaluation (NICE) registry of admissions to adult intensive care units. Int J Epidemiol. 2015;44(6):1850–1850h. 10.1093/ije/dyv291 [DOI] [PubMed] [Google Scholar]
- 10.Dutch National Intensive Care Evaluation registry (https://stichting-nice.nl)
- 11.Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36. 10.1007/s11136-011-9903-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turnbull AE, Rabiee A, Davis WE, Nasser MF, Venna VR, Lolitha R, Hopkins RO, Bienvenu OJ, Robinson KA, Needham DM. Outcome measurement in ICU survivorship research from 1970 to 2013: a scoping review of 425 publications. Crit Care Med. 2016;44(7):1267–77. 10.1097/CCM.0000000000001651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wubben N, van den Boogaard M, Ramjith J, Bisschops LLA, Frenzel T, van der Hoeven JG, Zegers M. Development of a practically usable prediction model for quality of life of ICU survivors: a sub-analysis of the MONITOR-IC prospective cohort study. J Crit Care. 2021;65:76–83. 10.1016/j.jcrc.2021.04.019 [DOI] [PubMed] [Google Scholar]
- 14.Oeyen S, Vermeulen K, Benoit D, Annemans L, Decruyenaere J. Development of a prediction model for long-term quality of life in critically ill patients. J Crit Care. 2018;43:133–8. 10.1016/j.jcrc.2017.09.006 [DOI] [PubMed] [Google Scholar]
- 15.Versteegh MM, Vermeulen KM, Evers SMAA, de Wit GA, Prenger R, Stolk EA. Dutch tariff for the five-level version of EQ-5D. Value Health. 2016;19(4):343–52. 10.1016/j.jval.2016.01.003 [DOI] [PubMed] [Google Scholar]
- 16.Pickard AS, Neary MP, Cella D. Estimation of minimally important differences in EQ-5D utility and VAS scores in cancer. Health Qual Life Outcomes. 2007;5:70. 10.1186/1477-7525-5-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vainiola T, Pettila V, Roine RP, Rasanen P, Rissanen AM, Sintonen H. Comparison of two utility instruments, the EQ-5D and the 15D, in the critical care setting. Intensive Care Med. 2010;36(12):2090–3. 10.1007/s00134-010-1979-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute physiology and chronic health evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006;34(5):1297–310. 10.1097/01.CCM.0000215112.84523.F0 [DOI] [PubMed] [Google Scholar]
- 19.Oeyen SG, Vandijck DM, Benoit DD, Annemans L, Decruyenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386–400. 10.1097/CCM.0b013e3181f3dec5 [DOI] [PubMed] [Google Scholar]
- 20.Blokzijl F, et al. The impact of surgical aortic valve replacement on quality of life-a multicenter study. J Thorac Cardiovasc Surg. 2021;161(4):1204-1210.e1207. 10.1016/j.jtcvs.2019.09.184 [DOI] [PubMed] [Google Scholar]
- 21.Blokzijl F, et al. Quality of life after coronary bypass: a multicentre study of routinely collected health data in the Netherlandsdagger. Eur J Cardiothorac Surg. 2019;56(3):526–33. 10.1093/ejcts/ezz051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cuthbertson BH, Elders A, Hall S, Taylor J, MacLennan G, Mackirdy F, Mackenzie SJ. Scottish critical care trials g, scottish intensive care society audit G: mortality and quality of life in the five years after severe sepsis. Crit Care. 2013;17(2):R70. 10.1186/cc12616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turnbull AE, Hurley M, Oppenheim IM, Hosey MM, Parker AM. Curb your enthusiasm: definitions, adaptation, and expectations for quality of life in ICU survivorship. Ann Am Thorac Soc. 2020;17:406–11. 10.1513/AnnalsATS.201910-772IP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barclay R, Tate RB. Response shift recalibration and reprioritization in health-related quality of life was identified prospectively in older men with and without stroke. J Clin Epidemiol. 2014;67(5):500–7. 10.1016/j.jclinepi.2013.12.003 [DOI] [PubMed] [Google Scholar]
- 25.van Leeuwen CM, Post MW, van der Woude LH, de Groot S, Smit C, van Kuppevelt D, Lindeman E. Changes in life satisfaction in persons with spinal cord injury during and after inpatient rehabilitation: adaptation or measurement bias? Qual Life Res. 2012;21(9):1499–508. 10.1007/s11136-011-0073-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kerckhoffs MC, Kosasi FFL, Soliman IW, van Delden JJM, Cremer OL, de Lange DW, Slooter AJC, Kesecioglu J, van Dijk D. Determinants of self-reported unacceptable outcome of intensive care treatment 1 year after discharge. Intensive Care Med. 2019;45(6):806–14. 10.1007/s00134-019-05583-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turnbull AE, Ji H, Dinglas VD, Wu AW, Mendez-Tellez PA, Himmelfarb CD, Shanholtz CB, Hosey MM, Hopkins RO, Needham DM. Understanding patients’ perceived health after critical illness: analysis of two prospective, longitudinal studies of ARDS survivors. Chest. 2022;161(2):407–17. 10.1016/j.chest.2021.07.2177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porter LL, Simons KS, Ramjith J, Corsten S, Westerhof B, Rettig TCD, Ewalds E, Janssen I, van der Hoeven JG, van den Boogaard M, Zegers M. Development and external validation of a prediction model for quality of life of ICU survivors: a subanalysis of the MONITOR-IC prospective cohort study. Crit Care Med. 2023;51(5):632–41. 10.1097/CCM.0000000000005800 [DOI] [PubMed] [Google Scholar]
- 29.Hofhuis J, Hautvast JLA, Schrijvers AJP, Bakker J. Quality of life on admission to the intensive care: can we query the relatives? Intensive Care Med. 2003;29(6):974–9. 10.1007/s00134-003-1763-6 [DOI] [PubMed] [Google Scholar]
- 30.Gifford JM, Husain N, Dinglas VD, Colantuoni E, Needham DM. Baseline quality of life before intensive care: a comparison of patient versus proxy responses. Crit Care Med. 2010;38(3):855–60. 10.1097/CCM.0b013e3181cd10c7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dinglas VD, Gifford JM, Husain N, Colantuoni E, Needham DM. Quality of life before intensive care using EQ-5D: patient versus proxy responses. Crit Care Med. 2013;41(1):9–14. 10.1097/CCM.0b013e318265f340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Gemert J, Zegers M, Adang E, Bakhshi-Raiez F, Simons KS, Corsten S, Westerhof B, Ewalds E, de Vries M, Dongelmans DA et al. Evaluating the representativeness of ICU survivors in a large patient-reported outcome measures cohort (MONITOR-IC): a comparative cohort analysis. Submitted 2024.
- 33.Rose L, Burry L, Agar M, Campbell NL, Clarke M, Lee J, Marshall JC, Devlin JW, Blackwood B, Needham DM, et al. A core outcome set for research evaluating interventions to prevent and/or treat delirium in critically ill adults: an international consensus study (Del-COrS). Crit Care Med. 2021;49(9):1535–46. 10.1097/CCM.0000000000005028 [DOI] [PubMed] [Google Scholar]
- 34.Needham DM, et al. Core outcome measures for clinical research in acute respiratory failure survivors. An international modified Delphi consensus study. Am J Respir Crit Care Med. 2017;196(9):1122–30. 10.1164/rccm.201702-0372OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Auriemma CL, Butt MI, Bahti M, Silvestri JA, Solomon E, Harhay MO, Klaiman T, Schapira MM, Barg FK, Halpern SD. Measuring quality-weighted hospital-free-days in acute respiratory failure: a modified Delphi study. Ann Am Thorac Soc. 2024;21:928–39. 10.1513/AnnalsATS.202311-962OC [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author on reasonable request. The data are not publicly available due to them containing information that could compromise research participant privacy.