Abstract
Pulsed field ablation (PFA) is an emerging technology for the treatment of atrial fibrillation (AF), for which pre-clinical and early-stage clinical data are suggestive of some degree of preferentiality to myocardial tissue ablation without damage to adjacent structures. Here in the MANIFEST-17K study we assessed the safety of PFA by studying the post-approval use of this treatment modality. Of the 116 centers performing post-approval PFA with a pentaspline catheter, data were received from 106 centers (91.4% participation) regarding 17,642 patients undergoing PFA (mean age 64, 34.7% female, 57.8% paroxysmal AF and 35.2% persistent AF). No esophageal complications, pulmonary vein stenosis or persistent phrenic palsy was reported (transient palsy was reported in 0.06% of patients; 11 of 17,642). Major complications, reported for ~1% of patients (173 of 17,642), were pericardial tamponade (0.36%; 63 of 17,642) and vascular events (0.30%; 53 of 17,642). Stroke was rare (0.12%; 22 of 17,642) and death was even rarer (0.03%; 5 of 17,642). Unexpected complications of PFA were coronary arterial spasm in 0.14% of patients (25 of 17,642) and hemolysis-related acute renal failure necessitating hemodialysis in 0.03% of patients (5 of 17,642). Taken together, these data indicate that PFA demonstrates a favorable safety profile by avoiding much of the collateral damage seen with conventional thermal ablation. PFA has the potential to be transformative for the management of patients with AF.
Subject terms: Outcomes research, Atrial fibrillation
In a post-approval study including more than 17,000 patients on the safety of pulsed field ablation, a new method for treatment of atrial fibrillation, the procedure was found to have a low rate of adverse events but was associated with some unexpected rare complications that will need further study.
Main
Atrial fibrillation (AF) is the most common sustained heart rhythm disorder, with notable impact on quality of life, morbidity and mortality1–4. Catheter ablation using thermal energy is an effective means to treat AF, even as a first-line therapy to improve quality of life and morbidity and even to prevent mortality in heart failure patients5–7. Technological evolution in catheter design, mapping and optimization across the spectrum of thermal ablation modalities (radiofrequency/laser/heat or cryothermy/cold) have made positive strides in improving its safety and efficacy.
However, inherent to thermal ablation is the indiscriminate nature of tissue destruction, which can have deleterious consequences on the myocardium and pericardiac structures. While the overall complication rates during thermal ablation have improved over time, there remain residual safety considerations including the risk for pulmonary vein (PV) stenosis, stroke, phrenic nerve palsy and the deadliest complication, atrio-esophageal fistula, which even today has a mortality of ~50% (refs. 8–10).
Pulsed field ablation (PFA) is an emerging AF ablation modality with an important degree of preferentiality to myocardial tissue damage. By delivering ultrarapid (microsecond to nanosecond) electrical pulses to generate strong electrical fields, PFA can produce irreversible nanoscale pore formation culminating in cellular death11,12. Pre-clinical studies demonstrated no (or little) damage to peri-atrial tissue such as the esophagus and phrenic nerve, and no PV stenosis13–16. The first and most extensively investigated PFA catheter is a multi-electrode pentaspline catheter, studied in first-in-human trials for treating either paroxysmal or persistent AF patients in IMPULSE/PEFCAT/PEFCAT2 and PersAFOne, respectively17–19. These trials demonstrated the feasibility and safety of PFA for AF ablation in a relatively small cohort of patients (<150) and few operators. Though promising, concerns remained around the safety of this novel ablation modality, particularly in a ‘real-world’ setting with a large volume of patients and operators.
After European regulatory approval (CE mark certification) of the pentaspline PFA catheter in March 2021, the MANIFEST-PF Survey of all AF patients receiving PFA in year 2021 (n = 1,758 patients at 24 centers) revealed no esophageal damage or PV stenosis and rare phrenic palsy (<1 in 1,000) with good clinical effectiveness20–22. These findings were consistent with the safety observed in the EU-PORIA registry (n = 1,233 patients at 7 centers). Additionally, the recently published ADVENT randomized clinical trial demonstrated noninferiority of PFA to conventional thermal ablation (cryothermal or radiofrequency) for efficacy and safety in a cohort of 707 paroxysmal AF patients23.
While encouraging, it is important to recognize that: (1) when cryoballoon ablation was first introduced approximately two decades ago, atrio-esophageal fistula formation was observed only after a few thousand patients were treated, and (2) unforeseen PFA-related adverse events (AEs) may only manifest after several thousands of procedures are performed24–26. Accordingly, the retrospective MANIFEST-17K study assessed the safety of PFA in the very large cohort of >17,000 patients.
Results
MANIFEST-17K is a retrospective observational study of centers performing PFA after regulatory approval of the pentaspline PFA catheter (Farawave, Farapulse-Boston Scientific Inc.) with the goal of collecting comprehensive data on the methods and safety of the post-approval clinical use of PFA. An invitation to participate in MANIFEST-17K was sent to all 116 centers performing post-approval clinical cases with this PFA catheter. Institution-level data were obtained on center characteristics, limited patient baseline characteristics, limited procedure parameters, and all AEs. We excluded from this analysis the initial 1,758 patients treated in 2021 by the initial 24 centers (herein referred to as the ‘initial MANIFEST-PF sites’) and previously reported in the MANIFEST-PF survey (the ‘MANIFEST-PF cohort’)20,21.
Baseline characteristics
Clinical site characteristics
Out of 116 centers contacted for participation, a total of 106 centers agreed (91.4% response), including the 24 initial MANIFEST-PF sites, plus 82 of the expanded MANIFEST-17K sites (Fig. 1). Clinical centers were located in 20 countries, 19 in Europe and 1 in Israel. All data forms were considered complete. Of the ten nonparticipating centers, five were not reachable, three declined participation owing to the time required for either local ethics approval or insufficient research staff, and two could not provide the data within the specified time frame.
Fig. 1. Study center, operator and patient numbers.
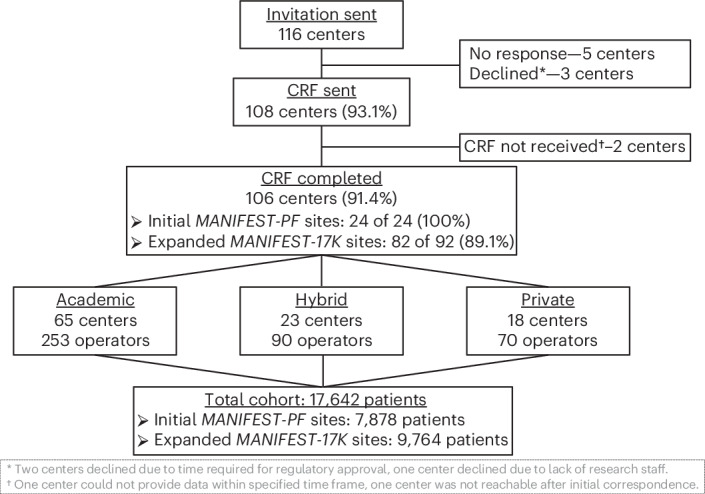
Shown are the invited and participating centers, along with the number of operators and the number of patients included in the study. CRF, case report form.
As shown in Extended Data Table 1, most centers (61.3%) self-classified as academic, 21.7% were hybrid and 17% were private practice. The mean number of operators per center was 3.9 (range 1–11), with an average of 13.6 years in practice (range 3–25 years). The average number of AF ablations performed annually was 590 (range 80–2,000). The date of the first PFA case performed ranged from March 2021 to March 2023, with each site performing an average of 166 PFA cases (range 17–1,277). The average follow-up time was 15 months (range 3–25 months).
Extended Data Table 1.
Clinical Site Characteristics
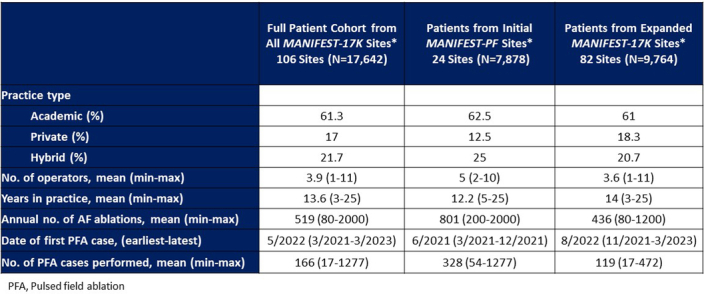
As compared to the initial MANIFEST-PF sites (n = 24), the expanded MANIFEST-17K sites (n = 82) similarly classified themselves as private (18.3% versus 12.5%, respectively, P = 0.506) or hybrid (20.7% versus 25%, respectively, P = 0.655). The initial MANIFEST-PF sites were higher volume centers for total AF ablation (801 (200–2,000) versus 436 (80–1,200), P < 0.001), and for PFA cases (328 (54–1,277) versus 119 (17–472), P < 0.001) and, as expected, had earlier exposure to PFA (average first case—June 2021 versus June 2022; Extended Data Table 1).
Patient characteristics
The study population included a total of 17,642 patients who underwent PFA between early 2022 to, for most centers, June 2023. The mean age was 64 years (range 11–96 years), of which 34.7% were female (Table 1). The type of AF treated was paroxysmal (57.8%), persistent (35.2%), long-standing persistent AF (5.6%) or, infrequently, atrial flutter/atrial tachycardia (1.4%). The procedures were performed under deep sedation without intubation in 53.1% of the patients.
Table 1.
Baseline patient characteristics
| Full MANIFEST-17K cohort (N = 17,642) | |
|---|---|
| Demographic | |
| Age (years), mean (minimum–maximum) | 64 (11–96) |
| Female (%) | 34.7 |
| Indication for ablation | |
| Paroxysmal atrial fibrillation (%) | 57.8 |
| Persistent atrial fibrillation (%) | 35.2 |
| Long-standing persistent atrial fibrillation (%) | 5.6 |
| Atrial flutter/atrial tachycardia (%) | 1.4 |
| Sedation | |
| General anesthesia (%) | 46.9 |
| Deep sedation/no intubation (%) | 53.1 |
AEs overview
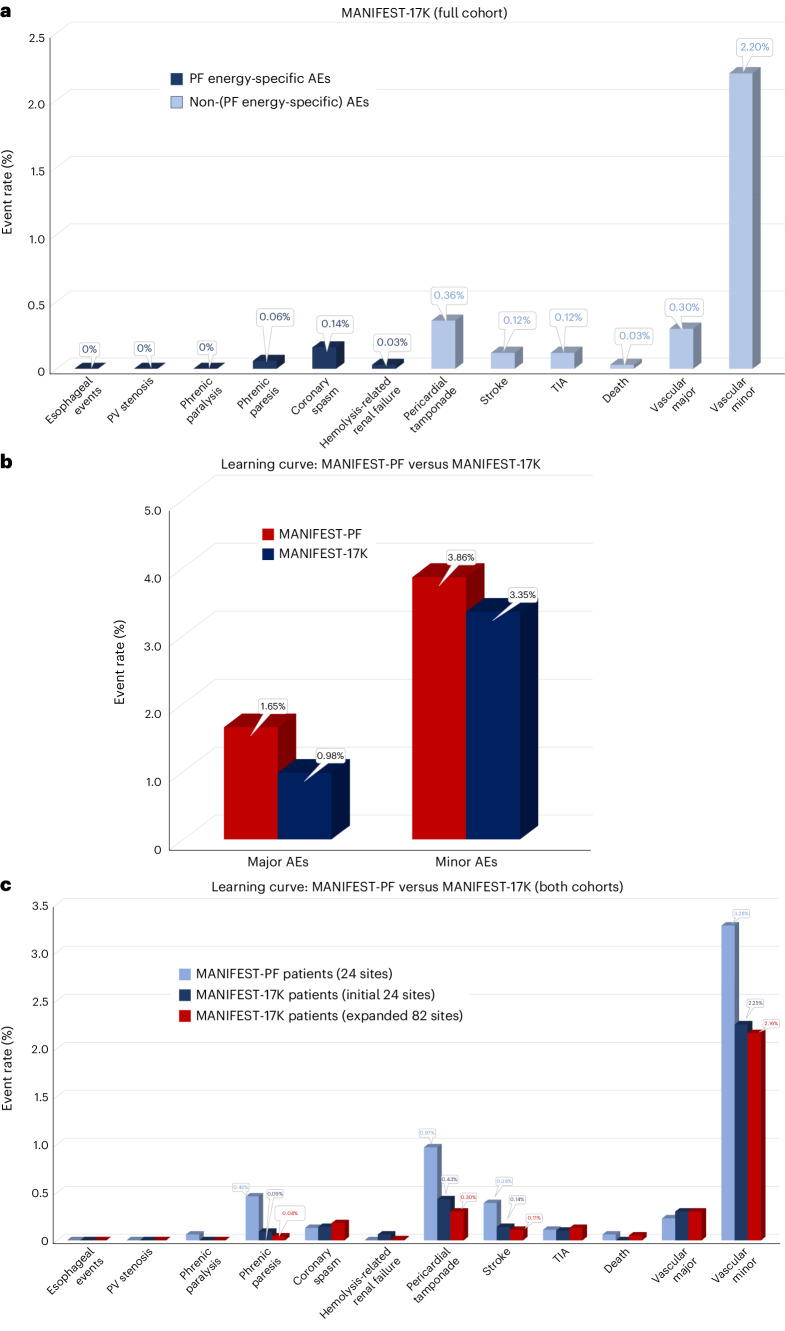
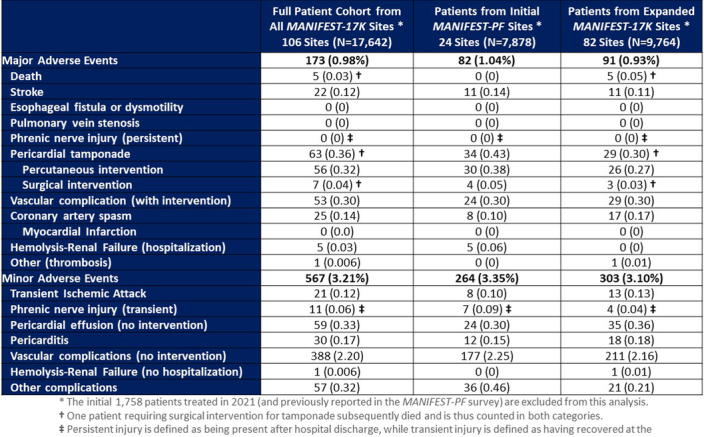
As shown in Table 2 and Fig. 2a, in the 17,642 patient cohort, the major complication rate was 0.98%. The most common of these major complications were of vascular origin (0.30%) and pericardial tamponade (0.36%), with the majority of the latter being treated percutaneously (56 of 63, 88.9%) instead of surgically (7 of 63, 11.1%). The remaining major complications included stroke (0.12%) and coronary spasm (0.14%), with mortality being rare at 0.03% (n = 5).
Table 2.
Major and minor complications
| Full patient cohort from all 106 MANIFEST-17K sitesa (N = 17,642) | |
|---|---|
| Major AEs | 173 (0.98%) |
| Deathb | 5 (0.03%) |
| Stroke | 22 (0.12%) |
| Esophageal fistula or dysmotility | 0 (0%) |
| Pulmonary vein stenosis | 0 (0%) |
| Phrenic nerve injury (persistent)c | 0 (0%) |
| Pericardial tamponadeb | 63 (0.36%) |
| Percutaneous intervention | 56 (0.32%) |
| Surgical interventionb | 7 (0.04%) |
| Vascular complication (with intervention) | 53 (0.30%) |
| Coronary artery spasm | 25 (0.14%) |
| Myocardial infarction | 0 (0.0%) |
| Hemolysis renal failure (hospitalization) | 5 (0.03%) |
| Other (thrombosis) | 1 (0.006%) |
| Minor AEs | 567 (3.21%) |
| Transient ischemic attack | 21 (0.12%) |
| Phrenic nerve injury (transient)c | 11 (0.06%) |
| Pericardial effusion (no intervention) | 59 (0.33%) |
| Pericarditis | 30 (0.17%) |
| Vascular complications (no intervention) | 388 (2.20%) |
| Hemolysis renal failure (no hospitalization) | 1 (0.006%) |
| Other complications | 57 (0.32%) |
aThe initial 1,758 patients treated in 2021 (and previously reported in the MANIFEST-PF survey) are excluded from this analysis.
bOne patient requiring surgical intervention for tamponade subsequently died and is thus counted in both categories.
cPersistent injury is defined as being present after hospital discharge, while transient injury is defined as having recovered by the time of discharge.
Overall major and minor event rates have been highlighted in bold.
Fig. 2. Complication rates.
a, Shown are the rates of complications, partitioned by relationship to pulsed field energy. Dark blue, complications with some degree of specificity to the energy source; light blue, complications that are more general to catheter ablation procedures. b, Shown are aggregated major and minor AE rates as initially reported in the MANIFEST-PF cohort (n = 1,758 patients; red bars) and observed in the currently studied MANIFEST-17K cohort (n = 17,642 patients; blue bars). c, Shown is a comparison of complication rates between those observed in the MANIFEST-PF cohort (light blue) as compared to both subcohorts of MANIFEST-17K. TIA, transient ischemic attack.
The minor complication rate was 3.21%, composed primarily of vascular complications (2.2%) and, to a lesser extent, pericardial effusion not requiring intervention (0.33%). Other minor complications included transient ischemic attack (0.12%), pericarditis (0.17%) and transient phrenic injury (0.06%)—the last defined as phrenic palsy that recovered before hospital discharge.
PFA energy-specific AEs
There were no post-PFA esophageal complications, including no reported instances of atrio-esophageal fistula formation or dysmotility disorders (Table 2). There were also no instances of pulmonary vein stenosis.
Phrenic nerve
Persistent phrenic nerve injury was not reported. However, transient phrenic paresis was reported in 11 patients (0.06%), with patients recovering diaphragmatic function by the next day.
Coronary spasm
There was evidence of coronary arterial spasm in 25 patients (0.14%). The majority of these cases were proximity-related spasm (22 of 25, 88%), and the remaining were instances of generalized/remote spasm (Table 3). Electrocardiogram (EKG) changes were observed in most patients (23 of 25; 92%), hypotension was observed in 5 cases (20%) and intravenous or intracoronary nitroglycerin was administered in 21 cases (84%). Clinical sequelae were reported in four cases (16%): (1) one patient developed atrioventricular block and ventricular fibrillation during PFA of the cavotricuspid isthmus (CTI), prompting resuscitation and defibrillation27, (2) two patients developed chest pain in the post-procedure recovery area, with both promptly resolved with nitroglycerin, and (3) one patient developed anterior ST elevation, polymorphic premature ventricular contractions and subsequent ventricular fibrillation after PFA at the right inferior PV—prompting resuscitation, defibrillation and intravenous nitroglycerin administration.
Table 3.
Coronary artery spasm
| Coronary spasm (N = 25) | |
|---|---|
| Type of spasm: | |
| Proximity-related spasma | 22 (88%) |
| Generalized spasmb | 3 (12%) |
| EKG changes | 23 (92%) |
| Hypotension | 5 (20%) |
| Clinical sequelae | 4 (16%) |
| Chest pain | 2 (8%) |
| Ventricular fibrillation | 2 (8%) |
| Intravenous nitroglycerin administered | 21 (84%) |
aSpasm occurring during PFA adjacent to a coronary artery, either during mitral isthmus or CTI ablation.
bSpasm occurring during conventional PV application remote from the location of a coronary artery.
Hemolysis-related renal failure
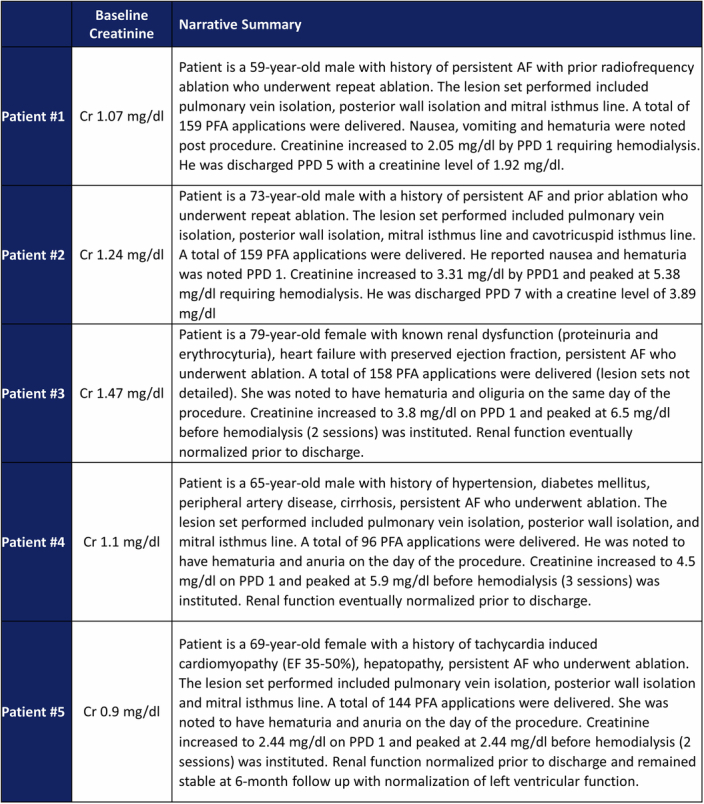
Hemolysis with resultant acute renal failure occurred in five patients (0.03%). The creatinine level increased by 100% by the next post-procedure day in all patients, with a peak creatinine of 6.5 mg dl−1 in one patient (Extended Data Fig. 1). Symptomatology included hemoglobinuria, nausea and oliguria, beginning either immediately post-procedure or the next day. Three patients had normal creatinine levels at baseline, while two patients had baseline elevation (1.2 and 1.5 mg dl−1). For all patients, transient hemodialysis significantly improved renal function by the time of hospital discharge.
Extended Data Fig. 1. Hemolysis-Renal Failure.
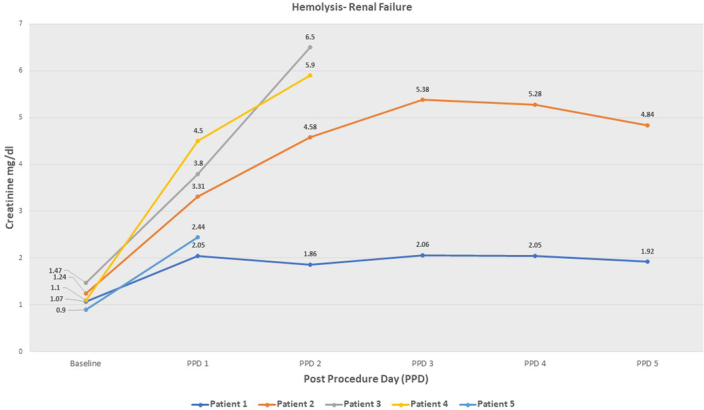
Shown are the creatinine trends for the five patients with hemolysis related renal failure.
All five patients had received PFA for persistent AF, with a complex lesion set including pulmonary vein isolation (PVI), posterior wall ablation, mitral isthmus and CTI lines. Importantly, an extensive number of PF applications (143 ± 27 per procedure) had been placed (patient details in Extended Data Table 2).
Extended Data Table 2.
Hemolysis-Related Acute Renal Failure: Patient Details
Hemolysis
One other patient was reported as having hemolysis, but without kidney injury (Table 2). In addition, there were several patients at one other center reported to have ‘dark urine or hemoglobinuria’ in either the immediate post-procedure setting or the next day. However, there was no reported kidney injury or drop in the red cell count.
Non-PFA energy-specific AEs
Pericardial tamponade
Pericardial tamponade occurred in 63 patients (0.36%), with the majority (n = 56, 0.32%; or 56 of 63, 88.9%) managed with percutaneous pericardiocentesis. Surgery was required in the remaining seven patients (0.04%), of which details were available for four: (1) right atrial appendage injury related to the guidewire for transeptal puncture, (2) laceration of the left atrium (LA) and right inferior pulmonary vein, (3) left ventricular perforation with the PFA catheter while trying to probe the left inferior pulmonary vein, and (4) perforation/tamponade with emergent sternotomy and repair but irreversible brain damage culminating in death (see below).
Stroke
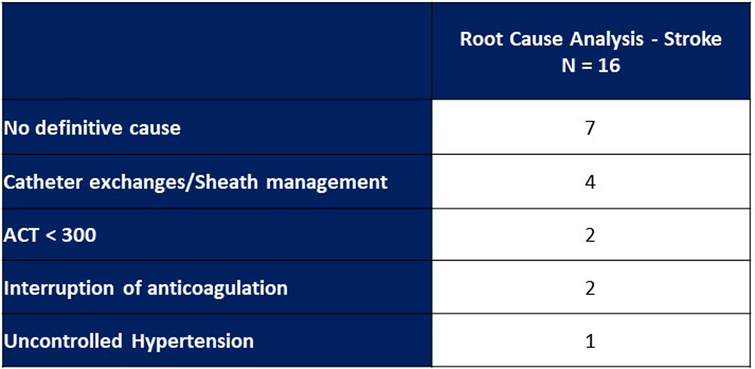
Stroke occurred in 22 patients (0.12%). In a root cause analysis including 16 of these patients, the most common putative cause was catheter exchanges/sheath management in 4 cases (Extended Data Table 3). Other putative contributory causes were an activated clotting time (ACT) <300 and interruption of anticoagulation in each of two patients, and uncontrolled hypertension in one patient. No definitive cause was identified in seven cases. None of these strokes culminated in death.
Extended Data Table 3.
Root Cause Analysis of Stroke Events
In a subset of the MANIFEST-17K cohort, 96 patients at eight clinical sites underwent routine post-procedural brain magnetic resonance imaging (MRI) to assess for asymptomatic lesions. Such asymptomatic MRI abnormalities were observed in nine patients (9.4%).
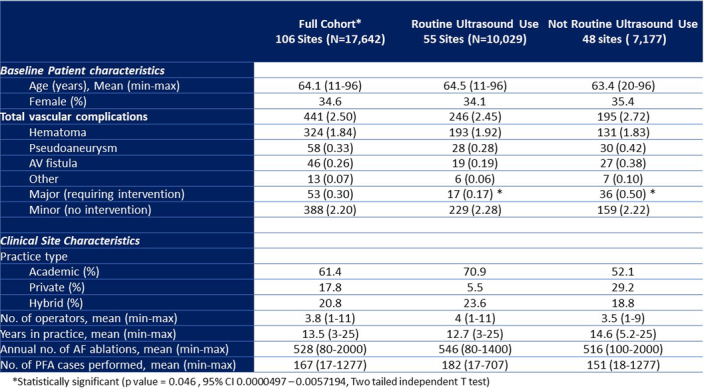
Vascular complications
Vascular complications occurred in 2.5% of patients, with most being minor complications (2.2%) not requiring intervention (Table 2). As shown in Extended Data Table 4, the most commonly observed vascular complications were hematomas (1.84%). The cohort was stratified by centers that did versus did not routinely use ultrasound guidance for vascular access: 55 sites versus 48 sites, respectively (data on ultrasound usage were not reported by 3 sites). The sites routinely using ultrasound were more likely to be classified as academic (70.9% versus 52.1%, P = 0.037) and less likely to be private (5.5% versus 29.2%, P = 0.0014). The clinical site characteristics and baseline patient characteristics were similar between both groups, including the number of PFA cases per site (182 (range 17–707) versus 151 (18–1,277), P = 0.393). However, the rate of major vascular complications was significantly higher in the group not routinely using ultrasound guidance (0.50% versus 0.17%, P = 0.046; Extended Data Table 4).
Extended Data Table 4.
Vascular Complications as a Function of Routine Vascular Ultrasound Usage
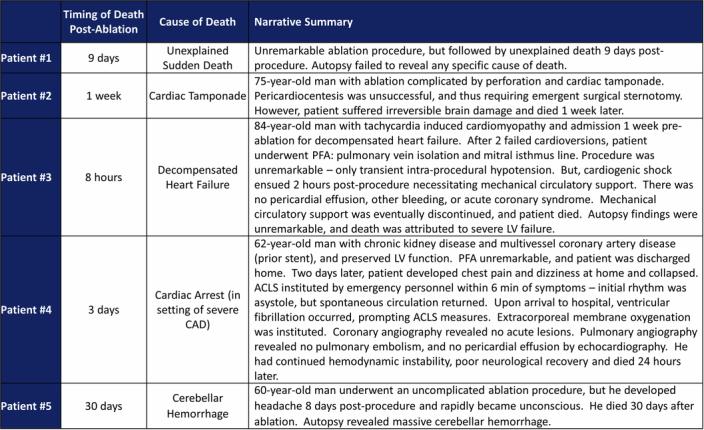
Mortality
The mortality rate was 0.03% (n = 5) in the MANIFEST-17K cohort. The available relevant details for each patient are listed in Extended Data Table 5. Briefly, two deaths were clearly procedure-related—a cardiac tamponade prompting emergent surgical repair but resulting in irreversible neurological damage and post-procedure cardiogenic shock in a patient with cardiomyopathy and decompensated heart failure. The remaining three deaths occurred at 3, 9 and 30 days post-ablation—two were sudden deaths that were unexplained or in the setting of severe coronary artery disease, respectively, and the last was a noncardiovascular death secondary to a brain hemorrhage.
Extended Data Table 5.
Details of Patient Deaths
Other complications
Complications categorized as ‘other’ occurred in 57 patients—0.32% of the full cohort. As shown in Table 4, the most common of these was the need for pacemaker implantation, occurring in 0.07% (n = 12), with lead dislocation or malfunction in another 0.02% (n = 3). Air emboli without clinical sequelae occurred in 0.06% (n = 10). Hemoptysis was noted in 0.02% (n = 3). Other notable unusual complications included individual cases of Takotsubo, Bell’s palsy and electrical isolation of the left atrial appendage (Extended Data Table 6).
Table 4.
Other complications
| Other complications N = 57 (0.32%) | |
|---|---|
| Pacemaker implant | 12 (0.07%) |
| Air emboli | 10 (0.06%) |
| Lead malfunction/dislocation | 3 (0.02%) |
| Atrioventricular block | 3 (0.02%) |
| Migraine | 3 (0.02%) |
| Hemoptysis | 3 (0.02%) |
| Anesthesia-related hypotension | 2 (0.01%) |
| Heart failure | 2 (0.01%) |
| Pneumonia | 2 (0.01%) |
| Gastritis | 2 (0.01%) |
| Miscellaneous | 15 (0.09%) |
Extended Data Table 6.
Complications in Both Cohorts – Initial MANIFEST-PF Sites vs Expanded MANIFEST-17K Sites
Learning curve
The initial 24 sites included in the previously published MANIFEST-PF study were the first sites/operators to utilize PFA for AF ablation after regulatory approval in Europe. There was an overall decrease in the rate of AEs when comparing outcomes from the 1,758 patients from MANIFEST-PF versus these same sites’ experience with the subset of 7,878 patients treated by these sites in MANIFEST-17K. There were trends for reduced rates of both major (1.65% versus 0.98%, P = 0.193) and minor (3.86% versus 3.35%, P = 0.266) AEs (Fig. 2b). As shown in Fig. 2c and Extended Data Table 6, there were numerical reductions in the rates of cardiac tamponade (0.97% versus 0.43%, P = 0.093) and minor vascular complications (3.28% versus 2.25%, P = 0.326). There were also numerical reductions in the rates of stroke (0.39% versus 0.14%, P = 0.387), transient phrenic nerve paresis (0.46% versus 0.09%, P = 0.344) and mortality (0.06% versus 0%, P = 0.323), although these did not reach statistical significance. The rate of major vascular complications was not different (0.23% versus 0.30%, P = 0.592).
In addition to the site-level learning observed at these 24 sites, there was also evidence of community-level global learning: when the AE rates of the initial MANIFEST-PF sites were compared to the expanded MANIFEST-17K sites, there was no significant difference in complication rates (Extended Data Fig. 2). Interestingly, all five deaths in this study occurred in the expanded MANIFEST-17K cohort, while all five cases of hemolysis with renal failure occurred in the initial MANIFEST-PF cohort.
Extended Data Fig. 2.
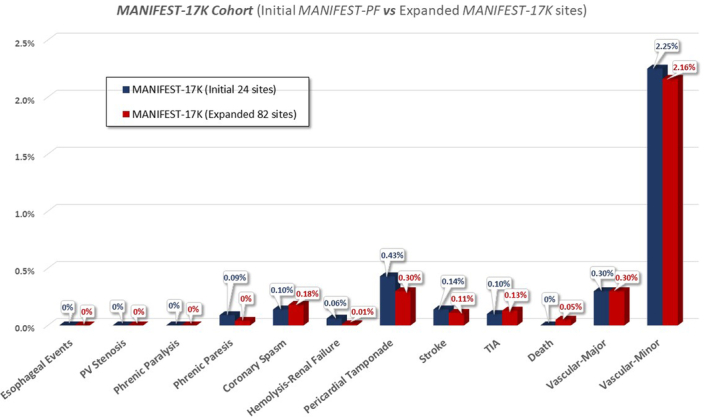
MANIFEST-17K Cohort (Initial MANIFEST-PF vs Expanded MANIFEST-17K sites.
Discussion
The MANIFEST-17K registry is a multicenter multinational study including 17,642 consecutive unselected AF patients undergoing post-approval PFA with a pentaspline catheter in routine clinical practice. Patients were treated at 106 clinical sites—representing >90% of all centers employing this PFA catheter. The major findings are: (1) there were no esophageal complications, symptomatic PV stenoses or persistent phrenic nerve injury, demonstrating the tissue preferentiality of PFA; (2) the overall rate of non-PFA energy-specific AEs was low, including a major complication rate of 0.98%—primarily pericardial tamponade and vascular complications—and a minor complication rate of 3.21%—primarily of vascular etiology; (3) coronary spasm occurred in 0.14%, primarily proximity-related vasospasm (0.12%), and to a lesser extent, generalized vasospasm (0.02%) during PVI; (4) there was an unexpected finding of hemolysis with associated acute renal failure requiring temporary hemodialysis in five patients (0.03%), although all patients recovered without sequalae; (5) the overall mortality rate was low at 0.03%; and (6) there was evidence of both center-level and global community-level learning with reduced rates of key AEs in the MANIFEST-17K cohort as compared to the previously published MANIFEST-PF cohort.
PFA is being utilized across the spectrum of AF, mostly paroxysmal AF (57.8%), but also persistent AF (35.2%). This is unsurprising given the success of PVI alone in many patients with persistent AF, and especially since posterior wall ablation is relatively easy to perform with PFA. PFA utilization spanned all practice settings, mostly academic centers (61.3%). Patient demographics, average age of 64 (11–96) and 34% female were consistent with routine clinical practice.
For procedural workflow, it is interesting that the use of deep sedation without endotracheal intubation and general anesthesia with intubation was relatively evenly split, slightly in favor of the former: 56.1% versus 43.9%, respectively. In the initial MANIFEST-PF survey, the majority of cases (82.1%) were performed without endotracheal intubation. The reason for this variance is unclear, but perhaps related to better access to anesthesia services, or a desire to minimize diaphragmatic stimulation and cough.
The cohort enrolled in this study, namely 17,642 patients, represents the largest PFA study so far. In this real-world cohort, preferentiality to tissue ablation was demonstrated for PFA, including no esophageal complications, PV stenosis or persistent phrenic nerve injury. This is consistent with prior pre-clinical, observational and randomized clinical studies.
Pre-clinical studies demonstrated the esophageal sparing properties of PFA. In an open chest porcine model, PFA application (200 J) directly atop the esophagus resulted in only intraepithelial vesicles being noted in the esophageal adventitia on day 2, with complete normalization by day 7 (ref. 13). In another porcine model, which better approximated the clinical situation, the esophagus was mechanically apposed against the inferior vena cava, from which either radiofrequency ablation (RFA) or PFA was performed. PFA revealed no chronic histopathological esophageal changes, while RFA demonstrated the full spectrum of esophageal injury including deep ulcers, abscesses and fistula formation15.
The initial clinical experience, including the initial MANIFEST-PF survey of >1,700 patients, also revealed no esophageal complications. Although promising, cryoballoon ablation was also initially thought to not result in esophageal complications; however, this was proven untrue after a few thousand patients were treated24–26. In the POTTER-AF worldwide survey including 553,729 procedures, the incidence of esophageal fistula was 0.025% (RFA, 0.038% (1 in 2,600) and cryoablation, 0.0015% (1 in 66,000)), with an associated mortality rate of 65.8% (ref. 8). In this context, it is striking that in the present MANIFEST-17K cohort of >17,000 patients, with no esophageal management strategy employed during procedures, no esophageal complications were observed. These data are entirely consistent with a post-ablation chest MRI study of patients undergoing either PFA (n = 18) or thermal ablation (n = 23; radiofrequency or cryoballoon) for AF; acute esophageal lesions were observed in 43% of thermal cases, but none with PFA16.
Interestingly, at one center, routine post-procedural esophagogastroduodenoscopy was performed in all patients (n = 29) undergoing PFA ablation. Imaging identified four cases of esophageal wall edema. However, there was no evidence of ulceration or gastric dysmotility, and no clinical symptoms were reported.
In pre-clinical studies of phrenic nerve injury, only transient (recovering in 30 min) phrenic nerve palsy was observed14,28,29. There were no histological changes suggestive of nerve injury. In the MANIFEST-PF registry of 1,568 patients, only 1 patient (0.06%) sustained phrenic nerve injury persisting beyond 1 year21. In the randomized ADVENT trial, persistent phrenic nerve injury was observed in 2 of 302 thermal ablation patients (0.7%), as opposed to 0 of 305 PFA patients.
In the present MANIFEST-17K cohort of >17,000 patients, there were no instances of persistent phrenic nerve injury and only 11 cases (0.06%) of transient phrenic nerve injury recovering within a few minutes or by the next day, with the latter nominally less frequently observed than in the initial MANIFEST-PF study (0.46%; P = 0.29). It has been postulated that transient phrenic nerve paresis may represent electrical hyperpolarization due to its rapid recovery. Nonetheless, care should be taken to limit excessive PFA in proximity to the phrenic nerve, and routine monitoring of post-PFA diaphragmatic function should be considered.
There were no reported cases of PV stenosis in this MANIFEST-17K cohort. Importantly, this is in the context of a large number of operators (n = 413) with varying experience (average 13.6 years, range 3–25 years). Notably, this potential complication was not prospectively defined and routine post-ablation PV imaging was not performed. However, these findings are in line with prior pre-clinical and clinical studies, including a nonrandomized comparison of RFA to PFA: neither PV stenosis nor even PV narrowing was present with PFA, whereas PV stenosis/narrowing was present in 32.5% of patients with RFA30. In the randomized ADVENT trial, there was a significant average decrease in the change in PV cross-sectional area 3 months post-ablation with thermal ablation (12.0%) versus no significant decrease with PFA (0.9%; posterior probability of superiority of PFA >99.9%)23.
There were 25 cases (0.14%) of coronary spasm: (1) most were proximity-related (n = 23, 88%), that is, occurring during PFA adjacent to a coronary artery during mitral isthmus or CTI ablation, and (2) the remaining (n = 3, 12%) were generalized spasm. The latter represent the Prinzmetal’s type of spasm occurring after ablation anywhere within the LA. Three cases of proximity-related spasm occurred while intending to perform PFA of the left inferior PV, but fluoroscopy review revealed inadvertent anterior positioning of the pentaspline catheter in flower pose toward the mitral isthmus. Of the 25 cases of spasm, 2 (8%) culminated in ventricular fibrillation; both patients required resuscitation and nitroglycerin administration; however, both patients recovered.
Coronary spasm during AF ablation, although rare, has even been reported with RFA in proximity to the coronary arteries31,32. The increased depth of the electric field generated during PFA may increase this likelihood. Indeed, upon routine post-PFA coronary angiography, PFA at the CTI or mitral isthmus results in frequent subclinical coronary vasospasm33,34. And there have been case reports of patients manifesting clinical spasm35,36. Importantly, spasm is attenuated by pre-administration of intracoronary or intravenous nitroglycerin33,34. The possibility of ventricular fibrillation, although infrequent, suggests that nitroglycerin should be considered before PFA in proximity to coronary arteries.
Most intriguing are the cases of generalized spasm following PFA at locations remote from the coronary arteries. This appears to be a sympathetic/autonomic response to energy delivery, and is not unique to PFA. Indeed, in a meta-analysis of >22,000 Japanese patients, generalized coronary vasospasm during PVI occurred with both cryoablation (0.27%) and RFA (0.04%) at rates similar to that presently observed with PFA (0.017%; 3 of 17,640)37. Proceduralists must be aware of this rare complication as timely intervention is crucial in this circumstance.
An unexpected finding was hemolysis-related renal failure, which occurred in five patients (0.03%). Symptoms were reported either immediately post-procedure or by the next day, with rapid progression of oliguria or anuria, requiring dialysis for normalization in renal function. One or more factors additional to the higher number of PFA applications may have contributed, including dehydration, relative hypotension due to general anesthesia, contrast computed tomography on the day of procedure and some degree of pre-existing kidney disease. With thermal ablation, hemolysis-related renal failure is an extremely rare finding. In the surgical literature, an increased risk of acute kidney injury with concomitant surgical AF ablation has been reported, but the pathophysiology may not be the same27.
The mechanism of hemolysis is probably related to the electroporative effects on erythrocytes. Foundational experiments had demonstrated voltage-induced pore formation in human erythrocytes during therapeutic PFA applications38. Using clinical defibrillators, when a homogeneous electrical field (field strength of 1,700 V cm−1 as single or double monopolar or bipolar pulses) was applied to a human erythrocyte suspension, hemolysis occurred in a dose-dependent fashion39, and of course, the renal toxic effect of sudden high concentrations of globular hemeproteins is well appreciated (for example, myoglobinuria from rhabdomyolysis after traumatic crush injury to an extremity). In fact, there are probably more instances of under-recognized hemolysis not resulting in renal failure.
Given this putative mechanism, it is not surprising that all five patients received more complex lesion sets than simple PVI, with a mean of 143 PFA applications per patient; indeed two patients received 159 PFA applications. For context, in the PFA for persistent AF ablation (PersAFOne) trial, wherein patients underwent PVI, posterior wall isolation and CTI, an average of 46 PF lesions were applied per patient19. In a real-world retrospective analysis of 45 patients undergoing PVI, posterior wall ablation and mitral isthmus ablation, a total of 85 ± 23 PFA applications/patient were employed40. It seems likely that the risk of hemolysis is dose-dependent. Accordingly, it is prudent to moderate the number of PFA applications, and when a large number of PFA applications is necessary, one should consider applying simple mitigation strategies such as saline hydration.
The major complication rate was low at ~1% and primarily consisted of pericardial tamponade (0.36%), stroke (0.12%), and vascular complications (0.30%), with a procedural mortality rate of only 0.03%. Considering the novelty of the technology, diversity of operators, and the first utilization by most operators, these rates are consistent with an excellent safety profile. For comparison, in a large US registry of AF ablation between 2000 and 2010 including >90,000 patients, the rate of pericardial complications was 1.52%, stroke was 1.02% and mortality was 0.42% (refs. 10,41). Furthermore, all 24 sites who treated the initial 1,758 patients in the MANIFEST-PF safety study were also in MANIFEST-17K, and there was a striking learning curve observed with >50% reductions in arguably the two most important complications, namely pericardial tamponade (0.97% reduced to 0.43%) and stroke (0.39% reduced to 0.14%). Interestingly, these low complication rates were also observed in the remaining 82 expanded MANIFEST-17K sites, namely pericardial tamponade (0.30%) and stroke (0.11%); this is indicative that the learnings from the initial MANIFEST-PF experience (in other words, careful catheter manipulation with utilization of a J-tip guidewire and careful sheath management with diligent saline flushing) were successfully elaborated to the full community. This bodes well for future sites commencing utilization of PFA.
Finally, it is notable that, in a small subset of the MANIFEST-17K cohort who underwent routine post-procedural brain MRI, asymptomatic abnormalities were observed in only 9 of 96 patients (9.4%). Their clinical significance remains unclear, as asymptomatic MRI-detected brain lesions are commonly seen after conventional AF ablation and other interventional cardiac procedures and more recently with another PFA ablation catheter42–44. Indeed, this incidence compares favorably with the 26.1% rate of silent cerebral ischemic events observed during routine brain MRI in 321 patients undergoing RF or cryoballoon ablation in the prospective multicenter AXAFA-AFNET5 trial (anticoagulation using the direct factor Xa inhibitor apixaban during atrial fibrillation catheter ablation: comparison to vitamin K antagonist therapy)45
MANIFEST-17K is limited by being a retrospective observational study of center-level data without prospectively defined safety outcomes. However, most centers maintained a PFA registry from which the data were extracted, and the near-universal engagement of the centers for data acquisition (91.4% overall participation), the breadth of AEs reported and the sheer scale of PFA cases included (representing almost all post approval PFA cases for AF) extends credibility to the study. Second, it is possible that additional patients may have sustained subclinical events; examples include esophageal lesions that healed without symptomatology, asymptomatic PV stenosis, asymptomatic cerebral lesions, subclinical coronary spasm, hemolysis causing mild reversible renal dysfunction, and so on. Third, in the cases of suspected vasospasm, actual spasm was not always observed, probably because of both prompt nitroglycerin administration and the time delay to angiography; thus, clinical determination of spasm was based on a number of factors (for example, proximity of PFA location to a coronary artery, distribution of ST elevation, temporal response to nitroglycerin and so on). Fourth, while MANIFEST-17K included >400 operators at 106 sites, of which 38.7% were private practice and hybrid institutions, it is possible that this cohort of operators is enriched for greater expertize; accordingly, the favorable safety profile may not directly translate to all other centers. Finally, this study is focused on the pentaspline PFA catheter; because of potential variability between PFA technologies, the safety observed in this study should not be assumed for other PFA catheters.
In conclusion, this is the largest registry of the safety of the post-approval use of a PFA catheter for the treatment of AF. In a ‘real-world’ setting of an unselected AF patient population, PFA demonstrated a safety profile consistent with an important degree of preferentiality to myocardial tissue ablation, with no evidence of esophageal complications, and with a low rate of major complications. Hemolysis-related renal failure requiring hemodialysis did occur, albeit rarely. Finally, the low incidence of coronary arterial spasm belies its potentially serious implications and warrants further study and guidance.
Methods
Survey overview
The MANIFEST-17K study is a retrospective observational study of centers performing PFA after regulatory approval of the pentaspline PFA catheter (Farawave, Farapulse-Boston Scientific Inc). The data form was developed by two of the authors (E.E. and V.R.) with the goal of collecting comprehensive data on the methods and safety of the post-approval clinical use of PFA (Online Supplement, case report form pages 7–9). MANIFEST-17K was approved by the Homolka hospital ethical committee (6.4.2022/18). The requirement of informed consent was waived by the ethical committee given the restrospective nature of the study.
An invitation to participate in the MANIFEST-17K study was sent to all 116 centers performing clinical cases with this PFA catheter since commercialization. All centers who accepted the invitation were sent the comprehensive data form. Institution-level data were obtained on center characteristics, limited patient baseline characteristics, limited procedure parameters and all AEs. Additional root cause analysis data were obtained for specific AEs. Data were typically collected from each center’s institution-level ablation database when available. All data forms were provided with the condition of anonymity of the identity of the physicians and institutions. Of note, we excluded from this analysis the initial 1,758 patients treated in 2021 by the initial 24 centers (herein referred to as the ‘initial MANIFEST-PF sites’) and previously reported in the MANIFEST-PF survey (the ‘MANIFEST-PF cohort’). Thus, the patients included in this study include those patients treated after 2021 from the initial MANIFEST-PF sites plus all patients treated by newer sites not initially participating in MANIFEST-PF (the ‘expanded MANIFEST-17K sites’).
The PFA procedure
The PFA system has been previously described; per manufacturer protocol, physicians were trained to employ a standard protocol17–19. Briefly, the 12F over-the-wire pentaspline PFA catheter (Farawave) is advanced through a 13F steerable sheath (Faradrive; Farapulse-Boston Scientific) into the LA. After positioning either a straight- or J-tip 0.035 guidewire into each target PV, the PFA catheter is positioned at the ostium of each PV and a total of eight PF lesions are applied per vein: four each in ‘basket’ and ‘flower’ configurations, with rotation between each pair of lesions. For posterior LA wall ablation, the catheter was placed into a flower configuration and positioned along the posterior LA to deliver overlapping sets of pulses at each location. The PF voltage amplitude could range between 1.8 and 2.0 kV, but 2.0 kV was typically employed. Unlike thermal ablation where one typically employs esophageal mitigation strategies (such as reduced ablation energy application along the posterior LA, esophageal temperature monitoring, esophageal cooling or mechanical esophageal deviation), no esophageal management strategy was employed during the PFA procedures.
Study data specifics
The data form was composed of questions covering the following areas: geographic region, clinical site characteristics, baseline patient characteristics, procedural parameters and AEs (Online Supplement, case report form pages 7–9). Major complications were defined as death, stroke, esophageal fistula or dysmotility, PV stenosis, phrenic nerve injury (persistent), pericardial tamponade, vascular complications requiring intervention, coronary spasm, myocardial infarction, hemolysis with resultant renal failure requiring hospitalization/dialysis, and thrombosis. If a major AE was identified (specifically stroke and coronary spasm) a root cause analysis form or AE detail form, respectively, was sent to the clinical site. The root cause analysis collected information on the event details, the physician’s hypothesis as to the most likely etiology and recommendations to prevent future complications. Minor complications were defined as transient ischemic attack, phrenic nerve injury (transient), pericardial effusion (no intervention), vascular complications (no intervention), hemolysis not requiring hospitalization and others.
Data analysis
The survey data form was considered complete if at least 80% of the questions were answered. In actuality, >95% of the forms were 100% completed. Importantly, the missing data were limited to the baseline patient demographics; there was no missingness in the reported safety outcomes.
Descriptive statistics were employed to analyze outcomes. Continuous variables were presented as means with minimum and maximum values provided. Continuous variables were compared using either the unpaired Student’s t-test (normal distribution) or Mann–Whitney U test (skewed distribution). Categorical variables were presented as counts or percentages and comparative analysis performed using the chi-squared or Fisher exact test. A two-tailed P value <0.05 was considered statistically significant. All analyses were performed using SPSS software (IBM Corp) version 29.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Online content
Any methods, additional references, Nature Portfolio reporting summaries, source data, extended data, supplementary information, acknowledgements, peer review information; details of author contributions and competing interests; and statements of data and code availability are available at 10.1038/s41591-024-03114-3.
Supplementary information
Participating sites and MANIFEST-17K case report form.
Extended data
Author contributions
E.E. and V.Y.R. designed, conducted and analyzed the study, and prepared the manuscript. All authors were study investigators and contributed to data acquisition and interpretation, review, revisions and final approval of the manuscript.
Peer review
Peer review information
Nature Medicine thanks Jason Andrade, Isabel Deisenhofer, Lars Eckardt and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Michael Basson, in collaboration with the Nature Medicine team.
Data availability
Data can be made available upon reasonable request as part of a scientific collaboration with adherence to standards of good scientific practice. Restrictions may apply due to privacy reasons, scale of contributors and ongoing research projects. Requests should be sent to the corresponding author, and a period of 90 days should be expected for a response.
Competing interests
E.E. received speaker honorarium from Boston Scientific and travel grants from Abbott and Biotronik. V.Y.R. has served as a consultant to Boston Scientific and formerly owned stock options in Farapulse (now divested); unrelated to this manuscript, he serves as a consultant for and has equity in Ablacon, Acutus Medical, Affera-Medtronic, Apama Medical-Boston Scientific, Anumana, APN Health, Aquaheart, Atacor, Autonomix, Axon Therapies, Backbeat, BioSig, CardiaCare, CardioNXT/AFTx, Circa Scientific, CoRISMA, Corvia Medical, Dinova-Hangzhou DiNovA EP Technology, East End Medical, EPD-Philips, EP Frontiers, Epix Therapeutics-Medtronic, EpiEP, Eximo, Field Medical, Focused Therapeutics, HRT, Intershunt, Javelin, Kardium, Keystone Heart, LuxMed, Medlumics, Middlepeak, Neutrace, Nuvera-Biosense Webster, Oracle Health, Restore Medical, Sirona Medical, SoundCath, Valcare; unrelated to this work, has served as a consultant for Abbott, AtriAN, Biosense Webster, BioTel Heart, Biotronik, Cairdac, Cardiofocus, Cardionomic, CoreMap, Fire1, Gore and Associates, Impulse Dynamics, Medtronic, Novartis, Philips, Pulse Biosciences; and has equity in DRS Vascular, Manual Surgical Sciences, Newpace, Nyra Medical, Surecor and Vizaramed. T.R. has received research grants from the Swiss National Science Foundation, the Swiss Heart Foundation, the sitem insel support funds, Boston-Scientific, Medtronic and Biotronik. He has received speaker/consulting honoraria or travel support from Abbott/SJM, Biosense Webster, Biotronik, Boston-Scientific and Medtronic, and support for the institution’s fellowship program from Abbott/SJM, Biosense Webster, Biotronik, Boston-Scientific and Medtronic. J.K. reports personal fees from Abbott, Biosense Webster, Biotronik, Boehringer Ingelheim, GE Healthcare, Medtronic, Pfizer, ProMed CS, and Viatris for lectures, advisory boards, and consultancy. P.J. has received grants by BSC and ANR grant IHU LIRYC ANR-10-IAHU-04. G.-B.C. received compensation for teaching purposes and proctoring from Medtronic, Abbott, Biotronik, Boston Scientific and Acutus Medical. A. Bulava received consultant and/or grant support from Abbott, Biotronik and Boston Scientific. Y.B. received research grants from Medtronic and Atricure and consulting fees from Abbott, Biosense Webster and Boston Scientific. G.S. received personal fees from Abbott, Bayer, Boston Scientific, Biosense Webster Inc. and LumaVision outside the submitted work. G.J. received personal fees from Boston Scientific. B.S. received consulting fees from Boston Scientific, Biosense Webster and Medtronic. J.C. has received funding from Boston Scientific, Medtronic and Biosense Webster (Education). K.N. has received funding from Biosense Webster, Boston Scientific and Field Medical. A.F. has received funding from Boston Scientific. J.V. has received research grants from Medtronic, Boston Scientific, Abbott, Biotronik, Daiichi Sankyo, BMS and Pfizer. He received honoraria from Abbott and Daiichi Sankyo, and support for meeting attendance from Biosense and Boston Scientific. He serves on the advisory board for Boston Scientific and is the Chairman of the Belgian Heart Rhythm Association. E.G. reports consulting fees from Medtronic, Boston, Microport, Abbott and Biotronik. P.K. has received research grants from Medtronic, Boston Scientific, Abbott, Biotronik, Daiichi Sankyo, BMS and Pfizer. He received honoraria from Abbott and Daiichi Sankyo, and support for meeting attendance from Biosense and Boston Scientific. He serves on the advisory board for Boston Scientific and is the Chairman of the Belgian Heart Rhythm Association. D. Scherr reports speaker and consulting fees from Boston Scientific. M.M. reports receiving speaker fees from Bayer, Biosense Webster, Biotronik, Amomed, AOP Orphan, Boston Scientific, Daiichi Sankyo and BMS/Pfizer and research grants from Biosense Webster and Abbott. J.H. reports receiving speaker fees and grant support from Biosense Webster and Medtronic. S.B. serves as a consultant for Medtronic, Boston Scientific, Microport and Zoll. I.G.-B. received speaker honoraria from Boston Scientific and proctorship fees from Abbott. A.A. has served as a consultant to Boston Scientific Inc., Farapulse Inc., Galaxy Medical Inc., Biosense and Webster and Arga Medtech, and has contracted research with Boston Scientific Inc., Farapulse Inc., Galaxy Medical Inc., Biosense and Webster, Arga Medtech, Future Cardia Inc. and Atacor Medical Inc. Z.J. served as consultant to Boston Scientific Inc and has contracted research with Atacor Medical Inc. D.G. has received research grants from Boston Scientific. P.D. has received research grants and honoraria from Boston Scientific. C.S. is a member of Medtronic Advisory Board Europe and Boston Scientitic Advisory Board Europe. He has received educational grants from Biosense Webster and Biotronik and a research grant from the European Union’s FP7 program and Biosense Webster. He reports lecture and consulting fees from Abbott, Medtronic, Biosense Webster, Boston Scientific, Microport and Biotronik, all outside the submitted work. P.S. is a member of the advisory board for Abbott, Biosense Webster, Boston Scientific and Medtronic. J.O. received speaking honoraria from Boston Scientific, Abbot, Biotronik and Medtronic. M. Gramlich received speaker honoraria and travel grants from Boston Scientific. C.T. served on the advisory board of and has received lecture/tutoring fees from Boston Scientific, Medtronic and Atricure. He has received lecture/tutoring fees from Abbott Medical. A.D.R. received speaker honoraria from Boston Scientific and Abbott. J.S. received speaker’s honoraria and travel grants from Boston Scientific, Biosense Webster, Medtronic, Bayer HealthCare and Bristol-Myers Squibb. A.L. received consulting fees from Boston Scientific, Biosense Webster, Pfizer, Bristol-Myers Squibb and Medtronic. G.F. received lecture honoraria and travel grants from Boston Scientific. F.A. received honoraria and served as a consultant for Boston Scientific, Medtronic and Microport CRM. A.M. received lecture honoraria and travel fees from Medtronic, Boston Scientific, Biosense Webster, Lifetech, BMS and Bayer. He also served as a consultant for Medtronic, Boston-Scientific and Biosense Webster. L.G. served as a consultant for Abbott, Medtronic, Boston, Biotronik and Johnson and Johnson. S.W. reports receiving grants and personal fees from Abbott, Boston Scientific and Medtronic, and personal fees from Boehringer Ingelheim, Brystol Myers Squibb, Bayer Vital, Accutus, Daiichi and Farapulse Inc. M. Gunawardene reports grants from Farapulse Inc. and Abbott. A. Goette was supported by EU Grant Horizon 2020 MAESTRIA Consortium grant number 965286 and has received speaker fees from Abbott, AstraZeneca, Bayer Health Care, Berlin Chemie, Biotronik, Boehringer Ingelheim, BMS/Pfizer, Boston Scientific, Daiichi Sankyo, Medtronic, Viofor, Novartis and Sanofi. C.M. reports honoraria and speaker’s fees from Boston Scientific, Medtronic, Biosense Webster, Acutus and Adagio. She served as a consultant and on the advisory board for Boston Scientific and Medtronic. She received research grant from Boston Scientific. R.T. reports receiving consulting fees from Boston Scientific, Abbot Medical, Biotronik and speaker’s honoraria from Boston Scientific, Abbot Medical, Biotronik and Biosense Webster. A. George has served as a consultant to Boston Scientific and has received fees for lectures from Boston Scientific. He has also received fees for consultation and/or lecturing from Abbot, AstraZeneca, Bard, Bayer Healthcare, Boehringer Ingelheim, Bristol-Myers Squibb, ELPEN, Galenica, Lilly, Medtronic, Menarini, MSD, Pfizer, Sanofi, Servier, Unifarma and Vianex. S.S. received speaker’s honoraria from Medtronic and Abbott, and participation in clinical trials with Abbott, Ablacon, Boston and Medtronic. R.B. received honoraria from Boston Scientific. T.D. received consulting fees from Farapulse (<2,000 US$), speaker fees with Galaxy Medical (<1,000 US$) and speaker fees with Abbott (<3,000 US$). A. Glowniak received compensation for proctoring and speaking duties from Medtronic and for speaking duties from Abbott and Boston. A.R. served as a consultant for Boston Scientific. H.P. served as a consultant/advisory board for Abbott, Biosense Webster, Boston Scientific and Medtronic. D.D. received modest lecture honoraria, travel grants and/or a fellowship grant from Abbott, Astra Zeneca, Biotronik, Boehringer Ingelheim, Boston Scientific, Bristol-Myers Squibb, CVRx, Medtronic, Microport, Pfizer and Zoll. D. Steven received research grant <50,000 € and speaker fees <10,000 € from Biosense Webster and Boston Scientific. A.S. reports receiving lecture and consulting honoraria from Medtronic, Abbott and Bayer. J.S.S.G.d.J. was a consultant for Medtronic. R.W. reports receiving honoraria for lectures from Adagio medical, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Boston Scientific, Biotronik, Daiichi Sankyo, Abiomed, Bayer, Novartis, Zoll. Honoraria for advisory board activities from Adagio medical, Boehringer Ingelheim, Bristol-Myers Squibb,Pfizer, Bayer. He reports participating in clinical trials with Daiichi Sankyo, Boehringer Ingelheim, Boston Scientific. He reports research funding from boston Scientific, BMS/Pfizer, Abiomed (all investigator-initiated trials). C.L.-G. received honoraria from Abbott and Biosense Webster. A. Breitenstein received consulting fees from Abbott, Bayer Health Care, Biosense Webster, Biotronik, BMS/Pfizer, Boston Scientific, Cook Medical, Daiichi Sankyo, Spectranetics/Philips and Medtronic. He received educational grants from Biosense Webster, Biotronik and Actelion. He received presenter fees from Abbott, Bayer Health Care, Biotronik, Cook Medical, BMS/Pfizer, Boston Scientific, Daiichi Sankyo, Medtronic and Spectranetics/Philips. J.I. received fees from Boston Scientific and an educational grant from Boston Scientific. D.L. has served as a consultant to Boston Scientific (now divested); and unrelated to this manuscript, he serves as a consultant for Ablacon, ATriAN, Bayer, Biosense Webster, Medtronic and Philips. J.R.-M. has received research funding and speaker/proctorship fees from Boston Scientific. D.R.M. has received speaker honoraria and research grants from Boston Scientific. All of the remaining authors have declared no conflicts of interest. There was no external funding support for this study.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
is available for this paper at 10.1038/s41591-024-03114-3.
Supplementary information
The online version contains supplementary material available at 10.1038/s41591-024-03114-3.
References
- 1.Mark, D. B. et al. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation. J. Am. Med. Assoc.321, 1275–1285 (2019). 10.1001/jama.2019.0692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turagam, M. K. et al. Catheter ablation of atrial fibrillation in patients with heart failure. Ann. Intern. Med.170, 41–50 (2018). 10.7326/M18-0992 [DOI] [PubMed] [Google Scholar]
- 3.Marrouche, N. F. et al. Catheter ablation for atrial fibrillation with heart failure. N. Engl. J. Med.378, 417–427 (2018). 10.1056/NEJMoa1707855 [DOI] [PubMed] [Google Scholar]
- 4.Packer, D. L. et al. Ablation versus drug therapy for atrial fibrillation in heart failure: results from the CABANA trial. Circulation143, 1377–1390 (2021). 10.1161/CIRCULATIONAHA.120.050991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuck, K.-H. et al. Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur. Heart J.37, 2858–2865 (2016). 10.1093/eurheartj/ehw285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turagam, M. K. et al. Assessment of catheter ablation or antiarrhythmic drugs for first-line therapy of atrial fibrillation. JAMA Cardiol.6, 697–705 (2021). 10.1001/jamacardio.2021.0852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirchhof, P. et al. Early rhythm-control therapy in patients with atrial fibrillation. N. Engl. J. Med.383, 1305–1316 (2020). 10.1056/NEJMoa2019422 [DOI] [PubMed] [Google Scholar]
- 8.Tilz, R. R. et al. A worldwide survey on incidence, management, and prognosis of oesophageal fistula formation following atrial fibrillation catheter ablation: the POTTER-AF study. Eur. Heart J.44, 2458–2469 (2023). 10.1093/eurheartj/ehad250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Calkins, H. et al. HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace9, 335–379 (2007). 10.1093/europace/eum120 [DOI] [PubMed] [Google Scholar]
- 10.Deshmukh, A. et al. In-hospital complications associated with catheter ablation of atrial fibrillation in the United States between 2000 and 2010. Circulation128, 2104–2112 (2013). 10.1161/CIRCULATIONAHA.113.003862 [DOI] [PubMed] [Google Scholar]
- 11.Kotnik, T., Rems, L., Tarek, M. & Miklavčič, D. Membrane electroporation and electropermeabilization: mechanisms and models. Annu. Rev. Biophys.48, 63–91 (2019). 10.1146/annurev-biophys-052118-115451 [DOI] [PubMed] [Google Scholar]
- 12.Reddy, V. Y. et al. Ablation of atrial fibrillation with pulsed electric fields. JACC Clin. Electrophysiol.4, 987–995 (2018). 10.1016/j.jacep.2018.04.005 [DOI] [PubMed] [Google Scholar]
- 13.Neven, K. et al. Acute and long-term effects of full-power electroporation ablation directly on the porcine esophagus. Circ. Arrhythm. Electrophysiol.10, e004672 (2017). 10.1161/CIRCEP.116.004672 [DOI] [PubMed] [Google Scholar]
- 14.Koruth, J. et al. Preclinical evaluation of pulsed field ablation: electrophysiological and histological assessment of thoracic vein isolation. Circ. Arrhythm. Electrophysiol.12, e007781 (2019). 10.1161/CIRCEP.119.007781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koruth, J. S. et al. Pulsed field ablation versus radiofrequency ablation: esophageal injury in a novel porcine model. Circ. Arrhythm. Electrophysiol.13, e008303 (2020). 10.1161/CIRCEP.119.008303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cochet, H. et al. Pulsed field ablation selectively spares the oesophagus during pulmonary vein isolation for atrial fibrillation. Europace23, 1391–1399 (2021). 10.1093/europace/euab090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reddy, V. Y. et al. Pulsed field ablation for pulmonary vein isolation in atrial fibrillation. J. Am. Coll. Cardiol.74, 315–326 (2019). 10.1016/j.jacc.2019.04.021 [DOI] [PubMed] [Google Scholar]
- 18.Reddy, V. Y. et al. Pulsed field ablation of paroxysmal atrial fibrillation: 1-year outcomes of IMPULSE, PEFCAT, and PEFCAT II. JACC Clin. Electrophysiol.7, 614–627 (2021). 10.1016/j.jacep.2021.02.014 [DOI] [PubMed] [Google Scholar]
- 19.Reddy, V. Y. et al. Pulsed field ablation in patients with persistent atrial fibrillation. J. Am. Coll. Cardiol.76, 1068–1080 (2020). 10.1016/j.jacc.2020.07.007 [DOI] [PubMed] [Google Scholar]
- 20.Ekanem, E. et al. Multi-national survey on the methods, efficacy, and safety on the post-approval clinical use of pulsed field ablation (MANIFEST-PF). Europace24, 1256–1266 (2022). 10.1093/europace/euac050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turagam, M. K. et al. Safety and effectiveness of pulsed field ablation to treat atrial fibrillation: one-year outcomes from the MANIFEST-PF registry. Circulation148, 35–46 (2023). 10.1161/CIRCULATIONAHA.123.064959 [DOI] [PubMed] [Google Scholar]
- 22.Schmidt, B. et al. European real-world outcomes with pulsed field ablation in patients with symptomatic atrial fibrillation: lessons from the multi-centre EU-PORIA registry. Europace25, euad185 (2023). 10.1093/europace/euad185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reddy, V. Y. et al. Pulsed field or conventional thermal ablation for paroxysmal atrial fibrillation. N. Engl. J. Med.389, 1660–1671 (2023). 10.1056/NEJMoa2307291 [DOI] [PubMed] [Google Scholar]
- 24.Kawasaki, R., Gauri, A., Elmouchi, D., Duggal, M. & Bhan, A. Atrioesophageal fistula complicating cryoballoon pulmonary vein isolation for paroxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol.25, 787–792 (2014). 10.1111/jce.12426 [DOI] [PubMed] [Google Scholar]
- 25.Metzner, A. et al. Increased incidence of esophageal thermal lesions using the second-generation 28-mm cryoballoon. Circ. Arrhythm. Electrophysiol.6, 769–775 (2013). 10.1161/CIRCEP.113.000228 [DOI] [PubMed] [Google Scholar]
- 26.Straube, F. et al. Comparison of the first and second cryoballoon: high-volume single-center safety and efficacy analysis. Circ. Arrhythm. Electrophysiol.7, 293–299 (2014). 10.1161/CIRCEP.113.000899 [DOI] [PubMed] [Google Scholar]
- 27.Bakir, N. H. et al. Concomitant surgical ablation for atrial fibrillation is associated with increased risk of acute kidney injury but improved late survival. J. Thorac. Cardiovasc. Surg.164, 1847–1857.e3 (2022). 10.1016/j.jtcvs.2021.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Driel, V. J. H. M. et al. Low vulnerability of the right phrenic nerve to electroporation ablation. Heart Rhythm12, 1838–1844 (2015). 10.1016/j.hrthm.2015.05.012 [DOI] [PubMed] [Google Scholar]
- 29.Yavin, H. et al. Pulsed field ablation using a lattice electrode for focal energy delivery: biophysical characterization, lesion durability, and safety evaluation. Circ. Arrhythm. Electrophysiol.13, e008580 (2020). 10.1161/CIRCEP.120.008580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kuroki, K. et al. Ostial dimensional changes after pulmonary vein isolation: pulsed field ablation vs radiofrequency ablation. Heart Rhythm17, 1528–1535 (2020). 10.1016/j.hrthm.2020.04.040 [DOI] [PubMed] [Google Scholar]
- 31.Meissner, A. et al. Impact of irrigated energy application on the right coronary artery hemodynamics: FFR measurement in patients who underwent ablation of common type atrial flutter. J. Interv. Card. Electrophysiol.21, 35–42 (2008). 10.1007/s10840-007-9188-8 [DOI] [PubMed] [Google Scholar]
- 32.Wong, K. C. K. et al. High incidence of acute sub-clinical circumflex artery ‘injury’ following mitral isthmus ablation. Eur. Heart J.32, 1881–1890 (2011). 10.1093/eurheartj/ehr117 [DOI] [PubMed] [Google Scholar]
- 33.Reddy, V. Y. et al. Coronary arterial spasm during pulsed field ablation to treat atrial fibrillation. Circulation146, 1808–1819 (2022). 10.1161/CIRCULATIONAHA.122.061497 [DOI] [PubMed] [Google Scholar]
- 34.Zhang, C. et al. Coronary artery spasm during pulsed field vs radiofrequency catheter ablation of the mitral isthmus. JAMA Cardiol.10.1001/jamacardio.2023.4405 (2023). 10.1001/jamacardio.2023.4405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gunawardene, M. A. et al. Coronary spasm during pulsed field ablation of the mitral isthmus line. JACC Clin. Electrophysiol.7, 1618–1620 (2021). 10.1016/j.jacep.2021.08.016 [DOI] [PubMed] [Google Scholar]
- 36.Della Rocca, D. G. et al. Transient inferior ST-segment elevation and ventricular fibrillation after cavotricuspid isthmus pulsed-field ablation. JACC Clin. Electrophysiol.9, 704–706 (2023). 10.1016/j.jacep.2022.11.027 [DOI] [PubMed] [Google Scholar]
- 37.Nakamura, T. et al. Incidence and characteristics of coronary artery spasms related to atrial fibrillation ablation procedures – large-scale multicenter analysis. Circ. J.85, 264–271 (2021). 10.1253/circj.CJ-20-1096 [DOI] [PubMed] [Google Scholar]
- 38.Kinosita, K. Jr. & Tsong, T. Y. Voltage-induced pore formation and hemolysis of human erythrocytes. Biochim. Biophys. Acta471, 227–242 (1977). 10.1016/0005-2736(77)90252-8 [DOI] [PubMed] [Google Scholar]
- 39.Moroz, V. V., Bogushevich, M. S., Chernysh, A. M., Kozlova, E. K. & Sharakshane, A. S. Effect of defibrillation pulses of different shapes on biomembranes: experimental study. Bull. Exp. Biol. Med.137, 120–123 (2004). 10.1023/B:BEBM.0000028118.86481.f6 [DOI] [PubMed] [Google Scholar]
- 40.Davong, B. et al. Pulsed-field ablation on mitral isthmus in persistent atrial fibrillation: preliminary data on efficacy and safety. JACC Clin. Electrophysiol.9, 1070–1081 (2023). 10.1016/j.jacep.2023.03.021 [DOI] [PubMed] [Google Scholar]
- 41.Cheng, E. P. et al. Risk of mortality following catheter ablation of atrial fibrillation. J. Am. Coll. Cardiol.74, 2254–2264 (2019). 10.1016/j.jacc.2019.08.1036 [DOI] [PubMed] [Google Scholar]
- 42.Kim, I.-C. et al. Incidence and predictors of silent embolic cerebral infarction following diagnostic coronary angiography. Int. J. Cardiol.148, 179–182 (2011). 10.1016/j.ijcard.2009.10.053 [DOI] [PubMed] [Google Scholar]
- 43.Kahlert, P. et al. Silent and apparent cerebral ischemia after percutaneous transfemoral aortic valve implantation. Circulation121, 870–878 (2010). 10.1161/CIRCULATIONAHA.109.855866 [DOI] [PubMed] [Google Scholar]
- 44.Verma, A. et al. Pulsed field ablation for the treatment of atrial fibrillation: Pulsed af pivotal trial. Circulation147, 1422–1432 (2023). 10.1161/CIRCULATIONAHA.123.063988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haeusler, K. G. et al. MRI-detected brain lesions and cognitive function in patients with atrial fibrillation undergoing left atrial catheter ablation in the randomized AXAFA-AFNET 5 trial. Circulation145, 906–915 (2022). 10.1161/CIRCULATIONAHA.121.056320 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Participating sites and MANIFEST-17K case report form.
Data Availability Statement
Data can be made available upon reasonable request as part of a scientific collaboration with adherence to standards of good scientific practice. Restrictions may apply due to privacy reasons, scale of contributors and ongoing research projects. Requests should be sent to the corresponding author, and a period of 90 days should be expected for a response.