Abstract
We have studied the mechanisms by which the CC-chemokine RANTES can enhance the infectivities of human immunodeficiency virus type 1 (HIV-1) and other enveloped viruses, when present at concentrations in excess of 500 ng/ml in vitro. Understanding the underlying mechanisms might throw light on fundamental processes of viral infection, in particular for HIV-1. Our principal findings are twofold: firstly, that oligomers of RANTES can cross-link enveloped viruses, including HIV-1, to cells via glycosaminoglycans (GAGs) present on the membranes of both virions and cells; secondly, that oligomers of RANTES interact with cell-surface GAGs to transduce a herbimycin A-sensitive signal which, over a period of several hours, renders the cells more permissive to infection by several viruses, including HIV-1. The enhancement mechanisms require that RANTES oligomerize either in solution or following binding to GAGs, since no viral infectivity enhancement is observed with a mutant form of the RANTES molecule that contains a single-amino-acid change (glutamic acid to serine at position 66) which abrogates oligomerization.
Infection of target cells by human immunodeficiency virus type 1 (HIV-1) is mediated by interactions of the viral envelope glycoproteins with CD4 and a coreceptor (32). Among the latter, the CC-chemokine receptor CCR5 and the CXC-chemokine receptor CXCR4 are the most physiologically important (8, 27, 56). The cognate chemokines can influence HIV-1 infection in several ways in vitro, the most commonly observed being inhibition of virus entry because of competition between the virus and the chemokine for binding sites on the same receptor (5, 17, 22, 29, 64, 66, 80, 84, 85, 94). Receptor down-regulation in response to chemokine binding and signaling can also interfere with virus entry by reducing the density of available coreceptors on the cell surface (2, 4, 51). However, CC-chemokines have also been reported to enhance HIV-1 infection of various cells in vitro (26, 36, 45, 58, 78).
Previously, we showed that the CC-chemokine RANTES could enhance HIV-1 infection of target cells in a manner that was independent of CD4 and any known coreceptor and even independent of the route of virus entry (36). Other CC-chemokines, such as macrophage-inhibitory protein (MIP)-1α and MIP-1β, did not have this effect (36). The extent of infectivity enhancement caused by RANTES was significant: in excess of 100-fold under some conditions. Two components of the enhancement mechanism were noted: one was apparent when the target cells were preincubated for several hours with RANTES prior to the addition of virus, and the other was evident when RANTES was added simultaneously with the virus (36). Here, we further analyze how RANTES can increase viral infectivity. We conclude that a major mechanism of infectivity enhancement is caused by the cross-linking of virions to the cell surface by oligomers of RANTES. These oligomers form after binding to glycosaminoglycans (GAGs), such as heparan sulfate, on both the virion and cell membranes. Of note is the fact that RANTES variants that do not oligomerize do not enhance viral infectivity (24). A second mechanism of viral infectivity enhancement arises from the prolonged interaction of RANTES oligomers with cell surface GAGs, which activates a herbimycin A-sensitive, tyrosine-kinase-dependent signal transduction pathway.
MATERIALS AND METHODS
Cells.
HeLa-CD4 cells were provided by David Kabat (47). They were maintained in Dulbecco’s minimal essential medium containing 10% fetal calf serum (FCS), glutamine, and antibiotics and split twice a week. Chinese hamster ovary (CHO)-K1 cells, heparan sulfate-mutant CHO cells (psgD-677 cells), and chondroitin sulfate-mutant CHO cells (psgA-745 cells) were all obtained from the American Type Culture Collection (Rockville, Md.) (30, 31, 49). These lines were maintained in F12K nutrient mixture (Kaighn’s modification) supplemented with 10% FCS.
Chemokines.
Human MIP-1α was purchased from R&D Systems Inc. (Minneapolis, Minn.). Recombinant human RANTES was produced in the bacterial host Escherichia coli as previously described (75). AOP-RANTES was derived from RANTES, as reported elsewhere (80). Rat RANTES was purchased from Peprotech Inc., Rockville, N.J. RANTES(3-68) was made by total peptide synthesis and provided by RMF DICTAGENE, Epalinges, Switzerland. The RANTES(3-68) molecule has the wild-type RANTES sequence but lacks the two N-terminal amino acids, serine and proline (65, 74). Its N-terminal sequence is therefore YSSDTPP… . The mutated, nonaggregating RANTES molecule, BB-10520 RANTES, was made at British Biotechnology Ltd. (Oxford, United Kingdom) (24). It has the wild-type RANTES sequence except for a single-amino-acid change: glutamic acid to serine at residue 66 (E66>S). The RANTES E66>S gene was expressed and secreted from the yeast Pichia pastoris at high yield. The purified protein, designated BB-10520 RANTES, had undergone truncation of the two N-terminal amino acids so that its N-terminal sequence was YSSDTPP… (24). This molecule and RANTES(3-68) are therefore identical except for the E66>S substitution.
Viruses.
Env-pseudotyped, luciferase-expressing reporter viruses were produced by the calcium phosphate technique (15, 23, 29). Thus, 293T cells were cotransfected with the envelope-deficient HIV-1 NL4-3 construct, pNL-Luc, and with a pSV vector expressing viral envelope glycoproteins (15, 23, 29). The pNL-Luc virus carries the luciferase reporter gene; the pSV vectors express envelope glycoproteins derived from HIV-1, amphotropic murine leukemia virus (MuLV), or vesicular stomatitis virus (VSV). The Env-pseudotyped viruses are designated HIV-1MuLV, HIV-1VSV, HIV-1HXB2, etc., with the subscript representing the pseudotyped env gene.
Viral infection assay with luciferase readout.
The extent of HIV-1 entry was determined by using a single-cycle infection assay (15, 23, 29). One day before infection, cells were seeded at a density of 104 per well of a 96-well tissue culture plate (HeLa-CD4) or at 5 × 104 per well of a 24-well tissue culture plate (CHO-K1, psgD-677, and psgA-745). After 24 h, the cells were infected with Env-pseudotyped HIV-1 (e.g., HIV-1MuLV) for 2 h at 37°C in the presence or absence of chemokines in a total infection volume of 100 (HeLa-CD4) or 500 (CHO-K1, psgD-677, and psgA-745) μl. The amount of input virus was determined by measuring its HIV-1 p24 antigen content. Unbound virus was removed by washing, and fresh medium lacking chemokines was added to the cells. Seventy-two hours postinfection, the cells were washed once with phosphate-buffered saline (PBS) and lysed in 50 μl of Reporter Lysis Buffer (Promega Inc.). The luciferase activity in a mixture of 100 μl of luciferase substrate (Promega) and 30 μl of cell lysate was measured in relative light units (RLU) with a DYNEX MLX microplate luminometer. Statistical analyses were performed by an unpaired Student t test (95% confidence interval; two tailed) to estimate significance.
Cell-cell fusion assay.
In the cell-cell fusion assay, a luciferase reporter gene is transactivated when cell-cell fusion occurs (28, 61). The T7-luciferase system and the recombinant vaccinia viruses were provided by Bernard Moss and Robert Doms. Two days before a fusion experiment, the target HeLa-CD4 cells were transfected with the T7-luciferase construct by using Lipofectin (Gibco BRL-Life Technologies), according to the manufacturer’s instructions. The next day, 4 × 104 lipofected target cells were seeded into each well of a 96-well plate in the presence or absence of chemokines and then incubated for 24 h at 37°C. One day before the experiment, the T7 RNA polymerase and Env proteins were introduced into the effector HeLa cells by infection for 2.5 h with recombinant vaccinia viruses at a multiplicity of infection of 10 in Dulbecco’s minimal essential medium supplemented with 2.5% FCS. The cells were then trypsinized, washed in PBS, and incubated overnight in medium containing rifampin (Sigma Chemicals; 100 μg/ml) at room temperature. For the fusion experiment, the effector cells were washed in PBS and resuspended in medium containing rifampin and cytosine β-d-arabinofuranoside (10 μM; Sigma Chemicals). The effector cells (8 × 104), with or without chemokine, were added to each well. Fusion took place for 2.5 h at 37°C, and then the luciferase activity in cell lysates was determined with the Promega system described above.
RANTES oligomerization assay.
The ability of RANTES and RANTES derivatives to oligomerize was assayed on heparin beads as described previously (37). Heparin-Sepharose CL-6B beads (Pharmacia; 0.5 μg/ml) were shaken with 0.23 nM 125I-labeled RANTES or RANTES derivative (each custom labeled by Amersham International, Little Chalfont, United Kingdom) in the presence of increasing concentrations of unlabeled protein in 100 μl of binding buffer (50 mM HEPES, pH 7.4, containing 5 mM MgCl2, 1 mM CaCl2, 150 mM NaCl, and 0.5% bovine serum albumin [BSA]) for 4 h at room temperature. The beads were then washed three times with 200 μl of binding buffer adjusted to contain 500 mM NaCl. The bound radioactivity was measured in a MicroWallac beta counter, and the data were plotted as described elsewhere (37).
Virus-cell adsorption assay.
The virus-cell adsorption assay was performed as described previously (54, 88). Briefly, sucrose gradient-purified HIV-1IIIB particles grown on H9 cells and sucrose gradient-purified control microvesicles from uninfected H9 cells were provided by Larry Arthur (Frederick Cancer Research and Development Center, Frederick, Md.) (9). The two preparations were standardized for total protein content. For the binding reactions, 1 μg of protein was added to 2 × 105 target cells. These were either from the CD4-positive, T-lymphoid cell line A3.01 or the related CD4-negative A2.01 line (54, 88).
For experiments in which RANTES was added to target cells simultaneously with virions, 2 × 105 cells were incubated for 2 h on ice with virions (or control microvesicles) and the anti-HLA-DR antibody G46-6 (0.5 μg/ml; Pharmingen) in the presence or absence of various concentrations of RANTES or BB-10520 RANTES. The cells were washed three times with ice-cold binding buffer (Dulbecco’s PBS containing 1% BSA and 0.1% sodium azide [D-PBS–BSA]), and then bound particles were detected with goat-anti-mouse-phycoerythrin secondary antibody (DAKO Diagnostics) and quantitated by fluorescence-activated cell sorter (FACS).
For experiments in which target cells were pretreated with RANTES, the cells (106/ml in culture medium) were incubated for 24 h at 37°C in the presence or absence of various concentrations of RANTES or BB-10520 RANTES. After being washed in ice-cold binding buffer, 2 × 105 cells were incubated for 2 h on ice with virions or microvesicles and the G46-6 antibody (0.5 μg/ml). The cells were then washed three times with binding buffer before detection and quantitation of bound particles as described above.
Virion binding to immobilized RANTES.
Two methods were used for virion binding. In the first, 4 × 107 magnetic beads coated with anti-murine immunoglobulin G (Dynal Inc.) were reacted with 5 μg of monoclonal anti-RANTES antibody (MAB-278; R&D Systems Inc.)/ml for 30 min at 37°C. Unbound antibody was removed by washing with D-PBS–BSA, and then the beads were incubated with 10 μg of RANTES or BB-10520 RANTES/ml for 30 min at 37°C in the presence or absence of chondroitin sulfate. Unbound chemokine was washed away, and the beads were incubated with HIV-1MuLV (250 ng of HIV-1 p24 antigen per sample) for 2 h at 37°C. Unbound virus was washed away and the beads were pelleted, resuspended, and analyzed for their p24 antigen content.
In the second assay, 6.7 × 107 streptavidin-coated magnetic beads (Dynal Inc.) were reacted with 5 μg of biotinylated polyclonal anti-RANTES or anti-MIP-1β antibodies (BAF 278 and BAF 271; R&D Systems Inc.)/ml for 30 min at 37°C. The rest of the procedure was as described above, except that the HIV-1MuLV input was 500 ng of HIV-1 p24 antigen per sample.
RESULTS
Enhancement of viral infectivity by RANTES is dependent upon the RANTES sequence.
We have demonstrated previously that RANTES, but not other CC-chemokines such as MIP-1α and MIP-1β, is able to enhance viral infectivity independently of the envelope glycoproteins and the route used by the test viruses to enter target cells (36). To gain further insight into the underlying mechanisms, we tested several different sequence variants of the RANTES molecule. The origins and properties of these RANTES variants are described in Materials and Methods. To eliminate any direct influences of RANTES on the receptor used for virus entry, we used as a test virus MuLV envelope glycoprotein pseudotypes of HIV-1 (HIV-1MuLV); the entry of HIV-1MuLV occurs via a plasma membrane phosphate transporter which is not known to be a RANTES receptor (53). As target cells, we used the HeLa-CD4 cell line, since RANTES enhances HIV-1MuLV infection of HeLa cells just as it does HIV-1 infection via CD4 and the CCR5 or CXCR4 coreceptors (36).
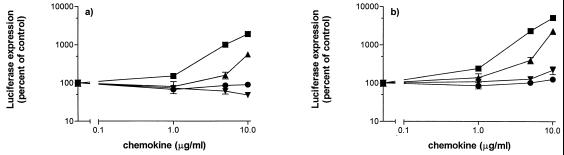
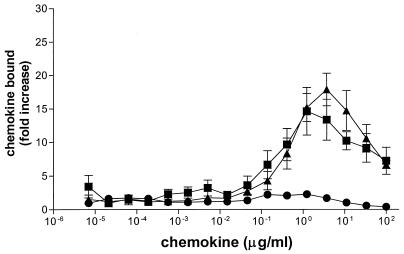
Based on our previous observations, RANTES enhancement of HIV-1MuLV infectivity was studied in two ways (36). The target cells were pretreated with CC-chemokines for 24 h and then washed before the addition of virus for 2 h in the absence of CC-chemokine (Fig. 1a); alternatively, CC-chemokines were added to the cells for a 2-h period, simultaneously with the viral inoculum, and then washed away (Fig. 1b).
FIG. 1.
Effect of RANTES and RANTES variants on infection with MuLV pseudotypes. (a) CC-chemokines at the indicated concentrations were added to HeLa-CD4 cells for 24 h and then washed from the cells immediately before infection was initiated by the addition of HIV-1MuLV (3.2 ng of HIV-1 p24 antigen) for 2 h. No CC-chemokines were present during the infection period or subsequently. (b) CC-chemokines were added during the 2-h viral infection period but were not present before or after that time. In all experiments, unbound virus and CC-chemokines (if present) were washed away after the infection period and the cultures were replenished with fresh medium without CC-chemokine. The extent of viral infection was measured by determination of luciferase expression in quadruplicate cultures on day 3 postinfection; the data (mean ± standard deviation) are presented as percentages of control (no chemokine = 100%). The chemokines used were RANTES (■), RANTES(3-68) (▴), BB-10520 RANTES (▾), and MIP-1α (●). The untreated control values were 5,063 ± 948 RLU for both panels a and b. To test for statistical significance, we compared the data sets obtained in the presence and absence of CC-chemokine by the unpaired Student t test (95% confidence interval; two-tailed P values). Treatment of the cells for 24 h with 10, 5, and 1 μg of RANTES/ml (a) caused a significant increase in HIV-1MuLV infection compared to the untreated control (P < 0.0001). A significant increase in HIV-1MuLV infection was also caused by 10 μg of RANTES(3-68)/ml (P = 0.001) but not by MIP-1α (P = 0.299). Treatment with BB-10520 RANTES significantly decreased HIV-1MuLV infection (P < 0.001). In the experiment shown in panel b, all four compounds significantly increased HIV-1MuLV infection; even the moderate increases observed with BB-10520 RANTES and MIP-1α at 10 μg/ml achieved statistical significance (P < 0.001 and P = 0.011, respectively).
As was found previously, RANTES but not MIP-1α substantially enhanced HIV-1MuLV infectivity in a dose-dependent manner, whether it was added to the target cells 24 h prior to the virus (Fig. 1a) or simultaneously with the virus (Fig. 1b) (36). Significant, but somewhat reduced, infectivity enhancements were also observed with RANTES(3-68), a variant of RANTES that is N-terminally truncated by two residues (Fig. 1). In contrast, BB-10520 RANTES, which differs from the conventional RANTES molecule at only a single position (E66>S) and by a two-residue truncation at the N terminus (24), caused a modest decrease in HIV-1MuLV infectivity when added to the cells 24 h prior to the virus (Fig. 1a). Furthermore, BB-10520 RANTES stimulated only a very slight increase in infectivity when added at the highest concentration tested (10 μg/ml) simultaneously with HIV-1MuLV (Fig. 1b). Clearly, whether viral infectivity enhancement occurs is a function of the RANTES sequence, which presumably affects an important structural feature of this molecule. Of note is the fact that AOP-RANTES and rat RANTES both behave like the wild-type human RANTES molecule in that they also enhance viral infectivity (references 24 and 36 and data not shown). Each of these molecules, and also RANTES(3-68), is identical to wild-type human RANTES at residue 66, but each differs from BB-10520 RANTES at this position. The two-residue N-terminal truncation of BB-10520 RANTES is not responsible for its inability to enhance viral infectivity, since RANTES(3-68) has the same truncation yet still causes infectivity enhancement (Fig. 1).
RANTES promotes virion adsorption to target cells.
The experiments described above (Fig. 1a), taken together with our previous findings (36), show that RANTES causes a significant increase in the infectivity of cell-free virus when it is present during the virus-cell adsorption phase of the viral life cycle. One explanation of this would be that RANTES promotes virion binding to the cells. To test this directly, we measured the attachment of HIV-1IIIB to target cells (Fig. 2), using an assay developed by Mandor, Ugolini, and colleagues (54, 88). Virions grown in cells expressing HLA-DR (e.g., H9 cells) incorporate this protein into their membranes on budding from the cell membrane. The virions are then added to cells that do not express HLA-DR (e.g., A2.01 or A3.01 cells), and bound HLA-DR (i.e., virion membrane derived) is detected by FACS, using an anti-HLA-DR antibody. Cells that grow in suspension were used for this assay, to avoid damage to the membrane composition of adherent cells when they are detached for FACS analysis. By using CEM.NKR cells that are closely related to A3.01 cells, we have confirmed that RANTES causes viral infectivity enhancement in T cells which grow in suspension (data not shown).
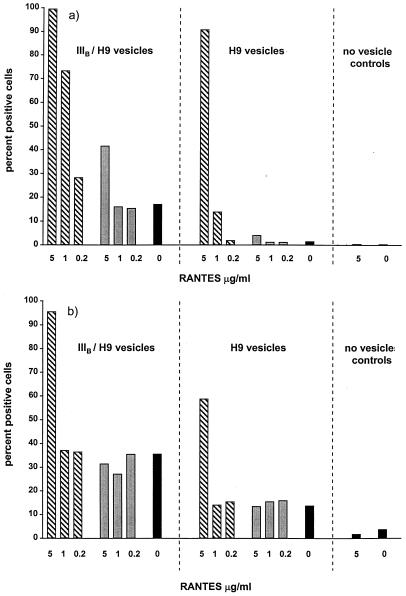
FIG. 2.
RANTES promotes virion adsorption to target cells. (a) A3.01 cells were incubated for 2 h on ice with preparations containing HIV-1IIIB virions (IIIB/H9 vesicles) or control microvesicles (H9 vesicles) in the presence of the indicated concentrations of RANTES (hatched bars) or BB-10520 RANTES (shaded bars) or with no CC-chemokine (solid bars). (b) A3.01 cells were treated for 24 h at 37°C with RANTES, BB-10520 RANTES, or no CC-chemokine, as described above. IIIB/H9 vesicles or control H9 vesicles were subsequently added for 2 h on ice in the absence of CC-chemokine. In both panels, cell-bound particles were detected by FACS after HLA-DR monoclonal antibody staining. The values shown are the percentages of positive cells that were gated.
Because cells produce small vesicles derived from cell membranes that are of a size similar to that of virions, it is necessary to control for the binding of these vesicles to target cells (9, 35). Consequently, we used sucrose gradient-purified preparations from both HIV-1IIIB-infected and uninfected H9 cells, designated IIIB/H9 vesicles and H9 vesicles, respectively. The former contain virions and microvesicles; the latter contain only microvesicles.
The binding of virions and microvesicles to CD4-positive A3.01 cells was measured in the presence and absence of RANTES and BB-10520 RANTES (Fig. 2). In one set of experiments, we mimicked what happens when RANTES and virions are added simultaneously to target cells in infectivity assays (Fig. 1b and 2a); in a second set, we treated the cells for 24 h with the RANTES molecules before adding virions in the absence of chemokine, again mimicking what happens in some infectivity assays (Fig. 1a and 2b).
We could detect the binding to A3.01 cells of HIV-1IIIB virions (IIIB/H9 vesicles) and, to a lesser extent, of the control microvesicles (H9 vesicles) (Fig. 2). The simultaneous addition of RANTES (5 μg/ml) caused a substantial increase in the number of A3.01 cells to which virions or microvesicles were attached. The effect of RANTES was greater with the virion-containing preparation than with the microvesicles, especially at a RANTES concentration of 1 μg/ml (Fig. 2a). In contrast, BB-10520 RANTES only slightly increased the number of cells that had virions attached and only at the highest concentration tested (5 μg/ml). BB-10520 RANTES had no effect on microvesicle attachment (Fig. 2a). Furthermore, when virion attachment was quantified by measuring the median fluorescence intensity levels, as opposed to the percentage of fluorescence-positive cells, BB-10520 RANTES caused no increase whereas the same concentration of RANTES raised the median fluorescence intensity by 20-fold (data not shown). A similar pattern of results was found when A3.01 cells were treated with the CC-chemokines for 24 h before the addition of virions or microvesicles (Fig. 2b). RANTES, but not BB-10520 RANTES, pretreatment caused an increase in the attachment of IIIB/H9 vesicles and, to a lesser extent, of H9 vesicles, although only at the highest concentration tested (5 μg/ml).
Analogous experiments were performed with CD4-negative A2.01 cells. In the absence of RANTES, no binding of either the IIIB/H9 virions or the control H9 vesicles was detectable (data not shown). This is consistent with previous observations that CD4 is required on the target cells for specific, stable virus attachment in this assay (54, 88). However, RANTES, either added simultaneously with the virions or used to pretreat the cells, caused a large increase in the binding of both virions and microvesicles to the A2.01 cells (data not shown). These effects of RANTES were not mimicked by BB-10520 RANTES (data not shown). Thus, RANTES can promote the attachment of virions and cell membrane-derived vesicles to target cells in a CD4-independent manner.
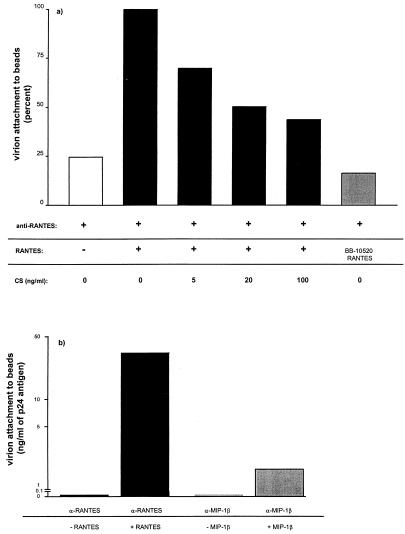
RANTES binds to virions.
One mechanism by which RANTES could promote virus-cell attachment would be for it to bind simultaneously to both virions and cells, cross-linking the former to the latter. It is well established that RANTES binds to cell surfaces via multiple receptors, including both classical chemokine receptors (73, 92) and GAGs (10, 37, 66, 89). To test whether RANTES can also bind to virions, we used two assays. In the first, we attached RANTES to magnetic beads via indirectly adsorbed anti-RANTES antibodies and then added HIV-1MuLV and determined the extent of virion binding by measuring how much HIV-1 p24 antigen was associated with the beads. There was significantly greater binding of virions to RANTES-coated beads than to control beads lacking RANTES (Fig. 3a). Virion attachment to the RANTES-coated beads was inhibited by the soluble GAG chondroitin sulfate, suggesting that the process was GAG mediated (see Fig. 6). The BB-10520 RANTES molecule did not promote significant virion attachment to beads (Fig. 3a), despite being able to recognize the anti-RANTES monoclonal antibody coating the beads (data not shown). In a similar assay, RANTES and MIP-1β were immobilized on streptavidin-coated beads via biotinylated polyclonal antibodies. The amount of virus captured on the beads was 20-fold greater in the presence of RANTES than when MIP-1β was used (Fig. 3b), which is consistent with the ability of RANTES, but neither MIP-1α nor MIP-1β, to enhance viral infectivity (36) (Fig. 1).
FIG. 3.
RANTES binds to virions. (a) RANTES was captured on magnetic beads via an anti-murine immunoglobulin G antibody and a murine anti-RANTES antibody (solid bars). HIV-1MuLV virions were then reacted with the beads for 2 h in the presence or absence of the indicated concentrations of soluble chondroitin sulfate (CS). The use of BB-10520 RANTES is indicated by the shaded bar, and the background binding in the absence of RANTES is represented by an open bar. The extent of virion capture was measured by p24 antigen determination and is expressed as the percentage of that achieved in the presence of RANTES but absence of CS (6.5 ng/sample, defined as 100%). The data shown are from one of two to three independent experiments. (b) Biotin-labeled antibodies to CC-chemokines were immobilized on streptavidin-coated magnetic beads and incubated with the appropriate CC-chemokines (solid bars, RANTES; shaded bars, MIP-1β) before the addition of HIV-1MuLV virions for 2 h. The extent of virion capture was measured by p24 antigen determination. The data shown are from one of three independent experiments.
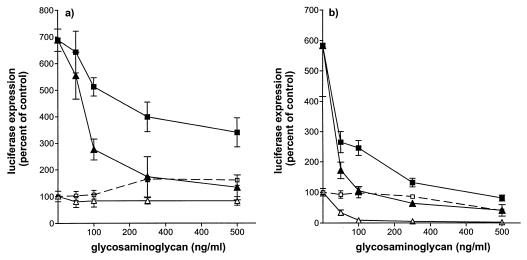
FIG. 6.
RANTES-mediated infectivity enhancement is inhibited by soluble GAGs. HeLa-CD4 cells were infected with HIV-1MuLV as described in Materials and Methods. (a) The cells were pretreated for 24 h with RANTES (5 μg/ml) in the presence or absence of soluble GAGs, and then infection was initiated in the absence of both RANTES and GAGs. (b) RANTES and GAGs were both added simultaneously with the virus at the initiation of infection. The GAG used was heparan sulfate (■ and □) or chondroitin sulfate (▴ and ▵). Open symbols, no RANTES; closed symbols, plus RANTES. The extent of viral infection was measured by determination of luciferase expression in quadruplicate cultures on day 3 postinfection; the data (mean ± standard deviation) are presented as percentages of control (no RANTES = 100%). The untreated control values were (a) 27,290 ± 2,450 RLU and (b) 27,151 ± 5,468 RLU.
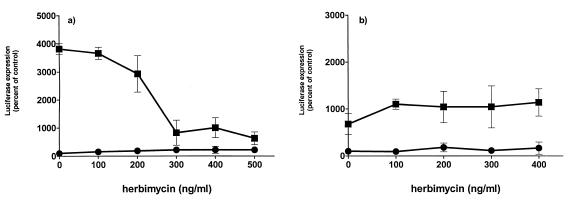
RANTES forms oligomers induced by binding to GAGs.
The results discussed above demonstrate that RANTES molecules which enhance viral infectivity promote virion attachment to cells and also bind to virions. In contrast, a RANTES variant (BB-10520 RANTES) that does not enhance virus-cell attachment also does not cause virus-cell binding and is not virion reactive. This correlation suggests that RANTES cross-links viruses to cells by binding simultaneously to receptors present on both the virion and cell membranes. But does a single RANTES molecule cause cross-linking or must RANTES oligomerize? To test this, we measured the extent to which RANTES and its variants can oligomerize, using an assay in which the RANTES molecules that bind to immobilized heparin, a typical GAG, are quantitated (Fig. 4).
FIG. 4.
RANTES and AOP-RANTES, but not BB-10520 RANTES, multimerize upon binding to heparin. Radiolabeled RANTES (■), AOP-RANTES (▴), or BB-10520 RANTES (●) was incubated with heparin-Sepharose beads in the presence of increasing amounts of the same, unlabeled chemokine, and the amount of radiolabeled chemokine bound to the beads was determined. The values shown are the means (± standard deviations) from five independent experiments.
RANTES and AOP-RANTES clearly form oligomers in this assay at concentrations above 100 ng/ml, whereas BB-10520 RANTES only dimerizes at similar concentrations (Fig. 4). The single-amino-acid change (E66>S) introduced into the RANTES molecule to make BB-10520 RANTES therefore prevents oligomerization, an observation also made by others (24). The extent of the RANTES multimerization shown here is greater than that previously described (37). This may be due to a variation in bivalent cation concentration in the assay buffers used in the present and earlier sets of experiments. We have noticed that EDTA completely abolishes the oligomerization of RANTES, indicating that the process is cation dependent (data not shown).
Qualitatively, there is a correlation between the abilities of RANTES-based molecules to oligomerize and to enhance viral infectivity (Fig. 1 and 4). Quantitatively, the concentration range at which RANTES binding to immobilized heparin occurs should not be precisely compared with what happens when RANTES binds to the cell surface, because the efficiency of the latter varies with the cell surface GAG composition and concentration. Overall, the results shown in Fig. 4 are consistent with the hypothesis that RANTES oligomers attach simultaneously to both virions and cells, cross-linking one to the other and promoting viral infectivity by increasing the amount of cell-bound virus.
GAGs are involved in the attachment of virions to cells via RANTES.
To what receptor(s) on virions and cells do oligomers of RANTES bind? We reported previously that we could not identify a seven-transmembrane-spanning receptor common to all the human and nonhuman cell lines in which RANTES enhanced viral infectivity (36). These negative findings, together with knowledge of the RANTES concentration range over which enhancement occurred, focused our attention on cell surface GAGs. These molecules, typified by heparan sulfate and chondroitin sulfate, are known to be low-affinity cell surface RANTES receptors (10, 37, 66). Indeed, RANTES is secreted from CD8+ cells as GAG complexes (89).
To address the involvement of GAGs, we first used two cell lines defective in GAG synthesis, derived by treating wild-type CHO-K1 cells with a chemical mutagen (31, 49). These CD4-negative lines have been used to demonstrate that GAGs are required for adhesion of the malarial circumsporozoite protein to target cells (34). The pgsA-745 line contains a mutation resulting in a defect in xylosyltransferase, an enzyme that attaches xylose to a serine residue of the core protein in the first sugar transfer reaction of GAG synthesis (31). This cell line does not, therefore, produce any GAGs. The psgD-677 line expresses altered forms of N-acetylglucosaminyltransferase and glucuronosyltransferase, enzymes required for heparan sulfate polymerization. These cells specifically lack heparan sulfate and accumulate three- to fourfold more chondroitin sulfate than wild-type cells (49).
Because HIV-1 and HIV-1MuLV pseudotypes do not efficiently infect CHO-K1 cells (41) (or mutants thereof), we used HIV-1 pseudotyped with the VSV envelope glycoproteins (HIV-1VSV); RANTES enhances the infectivity of this virus just as it does HIV-1 and HIV-1MuLV (36). The enhancement of HIV-1VSV infectivity by RANTES was significantly reduced in simultaneous-addition experiments with both CHO-K1 cell mutants, especially with the pgsA-745 GAG-deficient cell line (Fig. 5b). Similar, but more pronounced, reductions in the extent of infectivity enhancement were observed when both mutant CHO-K1 cell lines were pretreated with RANTES for 24 h before the addition of HIV-1VSV in the absence of RANTES compared to what was observed with the wild-type CHO-K1 cells. Indeed, there was no significant enhancement of infectivity with the pgsA-745, GAG-deficient cells under these conditions (Fig. 5a).
FIG. 5.
RANTES-mediated infectivity enhancement is dependent upon GAG expression on target cells. CHO-K1 cells (■), heparan sulfate-deficient psgD-677 cells (●), or GAG-deficient psgA-745 cells (▴) were infected with HIV-1VSV (1.5 ng of HIV-1 p24 antigen) in the presence or absence of the indicated concentrations of RANTES. Unbound virus was removed after a 2-h incubation, and the cultures were replenished with fresh medium without RANTES. (a) RANTES was added to the cells for 24 h, and then the chemokine-containing medium was washed away immediately before the addition of virus. RANTES was absent during the 2-h infection period and subsequently. (b) RANTES was added during the 2-h infection period but was not present prior to or after that time. The extent of viral infection was measured by determination of luciferase expression in quadruplicate cultures on day 3 postinfection; the data (mean ± standard deviation) are presented as percentages of control (no RANTES = 100%). The untreated control values (in RLU) were as follows: (a) CHO-K1 cells, 71.4 ± 16.3; pgsD 677 cells, 19.9 ± 4.4; pgsA 745 cells, 71.8 ± 8.4; (b) CHO-K1, cells 47.4 ± 11.5; pgsD 677 cells, 22.9 ± 6.9; pgsA 745 cells, 37.8 ± 4.0.
These results implicate cell surface GAGs as mediators of RANTES-induced viral infectivity enhancement. The most likely explanation of the effect is that oligomers of RANTES bind to GAGs on both the virus and cell membranes, cross-linking the two. We investigated whether this was, in fact, the case by adding soluble GAGs as competitors for RANTES binding to virion- or cell-associated GAGs. When HeLa-CD4 cells were treated with RANTES (5 μg/ml) in the presence or absence of soluble GAGs for 24 h prior to the addition of HIV-1MuLV, both heparan sulfate and chondroitin sulfate caused a dose-dependent inhibition of the RANTES-mediated infectivity enhancement (Fig. 6a). In the absence of RANTES, neither soluble GAG affected viral infectivity (Fig. 6a). Similar results were obtained when HIV-1HXB2 (Env pseudotype) was substituted for HIV-1MuLV (data not shown). When RANTES and soluble GAGs were both present during the period of virus-cell attachment and infection, the GAGs again reversed the enhancing effect of RANTES in a dose-dependent manner (Fig. 6b). However, the interpretation of this result is complicated by the inhibition of viral infectivity caused by GAGs in the absence of RANTES, a phenomenon that has been described previously (39, 63). Of note is the fact that soluble chondroitin sulfate inhibits the attachment of HIV-1MuLV virions to RANTES-coated magnetic beads (Fig. 3a).
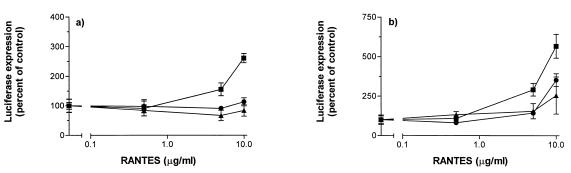
Effect of signal transduction inhibitors on RANTES-mediated infectivity enhancement.
We have noted previously the correlation between the concentrations of RANTES that enhance viral infectivity and those that were reported by Bacon et al. to cause a large, sustained increase in cytosolic Ca2+ concentrations in CD4+ T cells (6, 7, 25). This increase in intracellular Ca2+ was sensitive to the protein tyrosine kinase inhibitor herbimycin A, whereas smaller, more transient Ca2+ increases induced by lower concentrations of RANTES were blocked by pertussis toxin, an inhibitor of signaling via G-protein-coupled receptors (6, 7, 25). We therefore tested whether the RANTES-induced enhancements of viral infectivity were affected by herbimycin A (Fig. 7).
FIG. 7.
Effect of the tyrosine kinase inhibitor herbimycin A on RANTES-induced infectivity enhancement. HeLa-CD4 cells were incubated for 25 h with the indicated concentrations of herbimycin A. The cells were then infected with HIV-1MuLV (2.5 ng of HIV-1 p24 antigen) in the presence (■) or absence (●) of 10 μg of RANTES/ml. Unbound virus was removed after a 2-h incubation period, and the cultures were replenished with fresh medium without RANTES. (a) RANTES was added to the cells 24 h before the initiation of infection (i.e., 1 h after herbimycin A was added) and then washed away immediately before the addition of virus. Neither RANTES nor herbimycin A was present during the 2-h infection period or thereafter. (b) RANTES was added to the cells simultaneously with the viral inoculum so that both RANTES and herbimycin A were present during the 2-h infection period but neither agent was present after that period. In both experiments, the extent of viral infection was determined by measuring luciferase expression in quadruplicate cultures on day 3 postinfection; the data are presented as percentages of control (no chemokine = 100%). The untreated control values were (a) 183 ± 63 RLU and (b) 262 ± 53 RLU.
The enhancement of HIV-1MuLV infectivity caused by RANTES pretreatment of HeLa-CD4 cells was inhibited by herbimycin A in a dose-dependent manner (Fig. 7a). In the absence of RANTES, herbimycin A had no significant effect on HIV-1MuLV infectivity (Fig. 7a). Similar results were obtained when herbimycin A was added to the target cells 48 instead of 25 h prior to infection (data not shown). In contrast, herbimycin A pretreatment for 25 h had no effect on the infectivity enhancement which occurred when RANTES was added to the HeLa-CD4 cells simultaneously with HIV-1MuLV (Fig. 7b). To exclude the possibility that herbimycin A was no longer active after it had been in contact with the cells for 25 h, we repeated this experiment but with only a 1-h interval between the addition of herbimycin A and HIV-1MuLV; the results were identical (data not shown). Under the conditions used in both Fig. 7a and b, the same pattern of data was obtained when HIV-1HxB2 (Env pseudotype) was substituted for HIV-1MuLV (data not shown). Thus, the identity of the viral envelope glycoproteins which mediate entry into the target cells does not influence the RANTES-induced infectivity enhancement mechanisms or their sensitivity to herbimycin A.
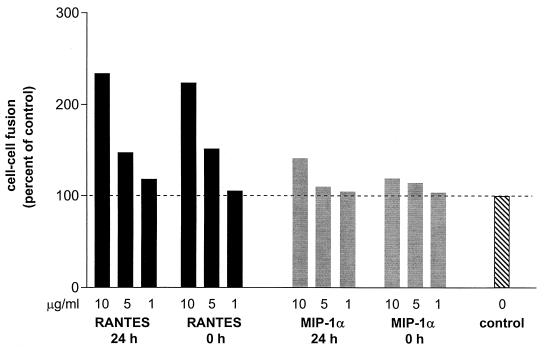
RANTES increases the efficiency of cell-cell fusion.
To gain more insight into the effects of treating target cells with RANTES for prolonged periods, we tested whether such cells were more permissive to cell-cell fusion and not just virus-cell fusion. To do this, we used an assay in which a luciferase reporter gene is transactivated when cell-cell fusion occurs (28, 61). HeLa cells expressing the envelope glycoproteins of HIV-1IIIB (HeLa-EnvIIIB cells) are the effector cells, and luciferase-containing HeLa-CD4 cells are the targets.
RANTES, at 5 to 10 μg/ml, caused an increase in the extent of cell-cell fusion, both when it was added to the mixed effector and target cell population only during the fusion reaction and when it was added to the effector cells for 24 h prior to the initiation of cell-cell fusion (Fig. 8). In contrast, the same concentrations of MIP-1α had little or no effect on cell-cell fusion under these conditions (Fig. 8). Thus, whatever changes are caused to HeLa cells by prolonged exposure to RANTES, their effect is to increase the extent of both virus-cell fusion and Env-mediated cell-cell fusion.
FIG. 8.
Effect of RANTES on HIV-1 Env-mediated cell-cell fusion. HeLa target cells expressing the HIV-1IIIB envelope glycoproteins were allowed to fuse with HeLa-CD4 effector cells in the presence of the indicated concentrations of RANTES (solid bars), MIP-1α (shaded bars), or medium (hatched bars). The designation 0 h means that the chemokine was only added to the mixed effector-target cell population during the fusion process; the designation 24 h indicates that the effector cells were pretreated with the chemokine for 24 h. The values shown are representative of those from four independent experiments.
DISCUSSION
The purpose of this study was to understand the mechanisms by which the CC-chemokine RANTES enhances the infectivities of HIV-1 and other enveloped viruses when present at concentrations in excess of 500 ng/ml in vitro (36). We do not argue that what we have observed is necessarily physiologically relevant—plasma concentrations of RANTES rarely exceed 200 ng/ml in HIV-1-infected or uninfected people (42, 48, 52, 60)—although we note that local concentrations of RANTES in tissues are unknown but could be rather higher than in plasma, especially at the sites of inflammation, where RANTES performs its normal physiological functions. Neither do we expect that plasma concentrations of exogenously administered RANTES or its derivatives would approach the range at which viral infectivity enhancement occurs, if and when these compounds are used therapeutically. It should not be overlooked that concentrations of RANTES lower than those we have studied here can inhibit the replication of R5 HIV-1 isolates in vitro by preventing the use of the CCR5 coreceptor by these viruses (5, 10, 22, 29, 51, 64, 80, 85).
We believe, however, that understanding how RANTES enhances viral infectivity in vitro might throw light on the fundamental processes of viral infection, in particular for HIV-1. The complexity of the phenomena described here could also help explain the various, seemingly contradictory reports that RANTES can either inhibit or enhance HIV-1 replication in primary monocytes/macrophages (1, 3, 12, 29, 44, 59, 78, 96). We have not yet studied these cells in detail, but we and others have noted that RANTES can either inhibit or enhance the replication of X4 and R5X4 HIV-1 isolates in primary CD4+ T cells in a donor-dependent manner (26, 45, 58, 83, 85). We are presently investigating this phenomenon, to see whether it is mechanistically related to what we have observed here and previously (36).
In the present study, our principal findings are twofold: firstly, that oligomers of RANTES can cross-link enveloped viruses, including HIV-1, to cells via GAGs that are present on the membranes of both virions and cells; secondly, that oligomers of RANTES form on cell surface GAGs and transduce a herbimycin A-sensitive signal which, over a period of several hours, renders the cells more permissive to infection by HIV-1 or envelope pseudotypes of HIV-1. These phenomena may be relevant to studies of several viruses, because we have observed the first process with HIV-1, HIV-1MuLV, and HIV-1VSV and the second with HIV-1, HIV-1MuLV, HIV-1VSV, and influenza and vaccinia viruses (36, 83) (see above).
The observation that RANTES oligomers can cross-link virions to cells via GAGs is consistent with previous studies emphasizing the importance of GAGs in virus-cell binding. Mondor et al. reported that the attachment of the TCLA strain of HIV-1Hx10 to HeLa-CD4 cells was strongly dependent on the binding of the virus to cell surface GAGs (heparans); attachment could be efficiently inhibited by soluble heparin, dextran sulfate, or pentosan polysulfate but not by chondroitin sulfate (54). The importance of virus-GAG interactions, mediated by envelope glycoproteins or other virion components, for HIV-1 infection of various cell lines is well characterized (62, 71, 77); indeed, the rate-limiting step in HIV-1 penetration of its target cells is attachment to the cell surface, not the subsequent fusion reaction (68). This is also true of many other viruses (18, 57, 72, 90), and as with HIV-1, interactions with cell surface GAGs can be used to increase virion infectivity. For example, GAGs play an important role in facilitating interactions of herpes simplex virus with its fusion receptors (55, 95) and of the following viruses with the target cell surface: Dengue virus (16), vaccinia virus (19), foot-and-mouth disease virus (40), Sindbis virus (46), human herpesvirus 7 (79), and pseudorabies virus (86).
Virus-cell attachment can also be mediated by virion-associated adhesion factors binding to cell surface counterreceptors (11, 33, 67, 76) or, as we show here, by oligomers of RANTES. The mechanism and route by which virus-cell fusion subsequently occurs are irrelevant. We have found that RANTES oligomers can enhance the infectivity of VSV and MuLV Env pseudotypes of HIV-1, which enter target cells independently of CD4 and coreceptors (36). Similarly, the infectivities of murine influenza virus and vaccinia virus are also enhanced by oligomerized RANTES (83). The subsequent association of viruses with specific fusion receptors (e.g., of HIV-1 with CD4 and coreceptors) is still necessary for fusion and infection to occur. But an elevated concentration of virions attached to the cell surface increases the rate of virus-cell fusion, however fusion is achieved and also however attachment occurs.
In addition to virus-cell attachment, GAGs play an important role in the binding of other proteins to the cell surface. Thus, the major surface protein of the malaria sporozoites, the circumsporozoite protein, contains a highly conserved sequence responsible for the specific homing of malaria sporozoites to hepatocytes, the target cells for the first stage of infection (14, 81). The conserved sequence includes a series of positively charged amino acids whose interaction with cell surface GAGs is required for target cell adhesion of the sporozoite (34).
The GAG-binding region of RANTES is also positively charged and is located close to its C terminus. Thus, Burns et al. found that lysine and arginine residues within the C-terminal α-helical region of RANTES are critical for the interaction of this chemokine with GAGs (10). Of note is the fact that a monoclonal antibody (4A12) whose epitope is heavily dependent on residues in this region interferes with the binding of RANTES to cell surface GAGs; this process is necessary for the transduction of Ca2+ signals and the antiviral action of low concentrations of RANTES (10). The single-residue change (glutamic acid to serine) in BB-10520 RANTES that abolishes its ability to oligomerize and cause infectivity enhancement lies at position 66, only two amino acids away from the C terminus and within the 4A12 epitope (10, 24).
The three-dimensional structures of chemokines clearly show that these molecules can dimerize in a manner that is not GAG dependent. The dimeric topology of CC-chemokines, as illustrated by RANTES (20), differs considerably from that of CXC-chemokines, for example, interleukin-8 (21). Furthermore, the crystal structure of MCP-1 reveals that this CC-chemokine can also form tetramers (50), yet MCP-1 binds to its seven-transmembrane receptor as a monomer (70). Whether it is monomeric or higher-order forms of RANTES that bind, at low nanomolar concentrations, to high-affinity receptors such as CCR1 and CCR5 (6, 75, 80) remains to be determined. It should be noted that while the E66>S mutation abrogates the ability of RANTES to form multimers, the protein is still able to dimerize (Fig. 4) (24). Dimerization is clearly not sufficient for a CC-chemokine to cause viral infectivity enhancement; MIP-1α is another molecule which dimerizes yet does not enhance infectivity (36, 37). One difference between RANTES and MIP-1α is that, at physiological pH, the former is cationic and the latter is anionic (20). Yet charge cannot be the sole determinant of whether a CC-chemokine can increase viral infectivity; MCP-1 is also cationic and oligomerizes upon binding to heparin (50), but it does not increase HIV-1 infectivity (36, 37). Clearly, aspects of the chemistry and structure of RANTES that influence its ability to cause viral infectivity enhancement remain to be identified.
We do not yet understand how the prolonged interactions of RANTES oligomers with cell surface GAGs render target cells more permissive for infection by HIV-1 and other enveloped viruses. We did, however, note the correlation between the concentrations of RANTES that enhance viral infectivity (36) and those found by Bacon et al. to cause a large, sustained increase in cytosolic Ca2+ concentrations in CD4+ T cells (6, 7, 25). Since this increase in intracellular Ca2+ was sensitive to the protein tyrosine kinase inhibitor herbimycin A (6, 7, 25), we tested the effect of this compound on the RANTES-induced viral infectivity enhancement and found that the enhancement was also herbimycin A sensitive. Dairaghi et al. suggested that intracellular Ca2+ increases stimulated by high concentrations of RANTES were associated with CD3 expression (25). Our experiments, however, were all performed on CD3-negative cells, so the expression of CD3 is not necessary for infectivity enhancement to occur.
We suggest, therefore, that the binding of RANTES oligomers to cell-surface GAGs activates a signal transduction pathway(s) which involves herbimycin A-sensitive tyrosine kinases. Several signaling pathways activated by RANTES in T cells have been described (6, 7, 25, 43, 82, 87, 91, 93). At present, those involved in viral infectivity enhancement remain to be identified, as does the stage(s) in the life cycles of HIV-1 and other viruses that is affected by this signal(s). Syndecans are one group of prototypic proteoglycans that have been extensively studied; their expression changes dramatically during cell development and differentiation and is influenced by cell activation (13). Syndecans and another proteoglycan, CD44, have been shown to associate with protein tyrosine kinases from the Src family (38, 69). Useful information might accrue from studies in these general areas.
ACKNOWLEDGMENTS
We are very grateful to David Kabat, Dan Littman, and Tanya Dragic for providing cell lines, to Bernard Moss and Robert Doms for the recombinant vaccinia viruses used in cell-cell fusion assays, to Larry Arthur for gradient-purified HIV-1IIIB and control microvesicles, and to Fréderic Borlat, Jazza Segal, and Simon Monard for technical assistance.
This work was supported by RO1 AI41420 and by the Pediatric AIDS Foundation. A.T. is a Fellow of the Austrian Program for Advanced Research and Technology; J.P.M. is an Elizabeth Glaser Scientist of the Pediatric AIDS Foundation.
REFERENCES
- 1.Alkhatib G, Combadiere C, Broder C C, Feng Y, Kennedy P E, Murphy P M, Berger E A. CC CKR5: a RANTES, MIP-1α, MIP-1β receptor as a fusion cofactor for macrophage-tropic HIV-1. Science. 1996;272:1955–1958. doi: 10.1126/science.272.5270.1955. [DOI] [PubMed] [Google Scholar]
- 2.Amara A, Le Gall S, Schwartz O, Salamero J, Montes M, Loetscher P, Baggiolini M, Virelizier J-L, Arenzana-Seisdedos F. HIV coreceptor downregulation as antiviral principle: SDF-1α-dependent internalization of the chemokine receptor CXCR4 contributes to inhibition of HIV replication. J Exp Med. 1997;186:139–146. doi: 10.1084/jem.186.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amzazi S, Ylisastigul Y L, Bakri Y, Rabehi L, Gattegno L, Parmentier M, Gluckman J C, Benjouad A. The inhibitory effect of RANTES on the infection of primary macrophages by R5 human immunodeficiency virus type-1 depends on the macrophage activation state. Virology. 1998;252:96–105. doi: 10.1006/viro.1998.9452. [DOI] [PubMed] [Google Scholar]
- 4.Aramori I, Ferguson S S G, Bieniasz P D, Cullen B R, Caron M G. Molecular mechanism of desensitization of the chemokine receptor CCR-5: receptor signalling and internalization are dissociable from its role as an HIV-1 co-receptor. EMBO J. 1997;16:4606–4616. doi: 10.1093/emboj/16.15.4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arenzana-Seisedos F, Virelizier J-L, Rousset D, Clark-Lewis I, Loetscher P, Moser B, Baggiolini M. HIV blocked by chemokine antagonist. Nature. 1996;383:400. doi: 10.1038/383400a0. [DOI] [PubMed] [Google Scholar]
- 6.Bacon K B, Premack B A, Gardner P, Schall T J. Activation of dual T cell signaling pathways by the chemokine RANTES. Science. 1995;269:1727–1730. doi: 10.1126/science.7569902. [DOI] [PubMed] [Google Scholar]
- 7.Bacon K B, Schall T J, Dairaghi D J. RANTES activation of phospholipase D in Jurkat T cells: Requirement of GTP-binding proteins ARF and RhoA. J Immunol. 1998;160:1894–1900. [PubMed] [Google Scholar]
- 8.Berger E A. HIV entry and tropism: the chemokine receptor connection. AIDS. 1997;11(Suppl. A):S3–S16. [PubMed] [Google Scholar]
- 9.Bess J W, Gorelick R J, Henderson L E, Arthur L O. Microvesicles are a source of contaminating cellular proteins found in purified HIV-1 preparations. Virology. 1997;230:134–144. doi: 10.1006/viro.1997.8499. [DOI] [PubMed] [Google Scholar]
- 10.Burns J M, Gallo R C, DeVico A L, Lewis G K. A new monoclonal antibody, mAb 4A12, identifies a role for the glycosoaminoglycan (GAG) binding domain of RANTES in the antiviral effect against HIV-1 and intracellular Ca2+ signaling. J Exp Med. 1998;188:1917–1927. doi: 10.1084/jem.188.10.1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cantin R, Fortin J-F, Lamontagne G, Tremblay M. The presence of host-derived HLA-DR1 on human immunodeficiency virus type 1 increases viral infectivity. J Virol. 1997;17:1922–1930. doi: 10.1128/jvi.71.3.1922-1930.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Capobianchi M R, Abbate I, Antonelli G, Turriziani O, Dolei A, Dianzani F. Inhibition of HIV type 1 BaL replication by MIP-1α, MIP-1β, and RANTES in macrophages. AIDS Res Hum Retroviruses. 1998;14:233–240. doi: 10.1089/aid.1998.14.233. [DOI] [PubMed] [Google Scholar]
- 13.Carey D. Syndecans: multifunctional cell-surface co-receptors. Biochem J. 1997;327:1–16. doi: 10.1042/bj3270001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cerami C, Frevert U, Sinnis P, Takacs B, Nussenzweig V. Rapid clearance of malaria circumsporozoite protein (CS) by hepatocytes. J Exp Med. 1994;179:695–701. doi: 10.1084/jem.179.2.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen B K, Saksela K, Andino R, Baltimore D. Distinct modes of human immunodeficiency virus type 1 proviral latency revealed by superinfection of nonproductively infected cell lines with recombinant luciferase-encoding viruses. J Virol. 1994;68:654–660. doi: 10.1128/jvi.68.2.654-660.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Y, Maguire T, Hileman R, Fromm J, Esko J, Linhardt R, Marks R. Dengue virus infectivity depends on envelope protein binding to target cell heparan sulfate. Nat Med. 1997;3:866–871. doi: 10.1038/nm0897-866. [DOI] [PubMed] [Google Scholar]
- 17.Choe H, Farzan M, Sun Y, Sullivan N, Rollins B, Ponath P D, Wu L, Mackay C R, LaRosa G, Newman W, Gerard N, Gerard G, Sodroski J. The β-chemokine receptors CCR3 and CCR5 facilitate infection by primary HIV-1 isolates. Cell. 1996;85:1135–1148. doi: 10.1016/s0092-8674(00)81313-6. [DOI] [PubMed] [Google Scholar]
- 18.Chuck A S, Palsson B O. Consistent and high rates of gene transfer can be obtained using flow-through transduction over a wide range of retroviral titers. Hum Gene Ther. 1996;7:743–750. doi: 10.1089/hum.1996.7.6-743. [DOI] [PubMed] [Google Scholar]
- 19.Chung C-S, Hsiao J-C, Chang Y-S, Chang W. A27L protein mediates vaccinia virus interaction with cell surface heparan sulfate. J Virol. 1998;72:1577–1585. doi: 10.1128/jvi.72.2.1577-1585.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chung C W, Cooke R M, Proudfoot A E, Wells T N C. The three-dimensional solution structure of RANTES. Biochemistry. 1995;34:9307–9314. doi: 10.1021/bi00029a005. [DOI] [PubMed] [Google Scholar]
- 21.Clore G M, Appella E, Yamada M, Matsushima K, Gronenborn A M. Three-dimensional structure of interleukin 8 in solution. Biochemistry. 1990;29:1689–1696. doi: 10.1021/bi00459a004. [DOI] [PubMed] [Google Scholar]
- 22.Cocchi F, DeVico A L, Garzino-Demo A, Arya S K, Gallo R C, Lusso P. Identification of RANTES, MIP-1 alpha and MIP-1 beta as the major HIV suppressive factors produced by CD8+ T cells. Science. 1995;270:1811–1815. doi: 10.1126/science.270.5243.1811. [DOI] [PubMed] [Google Scholar]
- 23.Connor R I, Sheridan K E, Ceradini D, Choe S, Landau N R. Change in coreceptor use correlates with disease progression in HIV-1 infected individuals. J Exp Med. 1997;185:621–628. doi: 10.1084/jem.185.4.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Czaplewski, L. G., J. McKeating, C. J. Craven, L. D. Higgins, V. Appay, A. Brown, T. Dudgeon, L. A. Howard, T. Meyers, J. Owen, S. R. Palan, P. Tan, G. Wilson, N. R. Woods, C. M. Heyworth, B. I. Lord, D. Brotherton, R. Christison, S. Craig, S. Cribbes, R. M. Edwards, S. J. Evans, R. Gilbert, P. Morgan, E. Randle, N. Schofield, P. G. Varley, J. P. Waltho, and M. G. Hunter. Identification of amino acid residues critical for aggregation of human CC chemokines MIP-1α, MIP-1β and RANTES: characteristics of active disaggregated chemokine variants. J. Biol. Chem., in press. [DOI] [PubMed]
- 25.Dairaghi D J, Soo K S, Oldham E R, Premack B A, Kitamura T, Bacon K B, Schall T J. RANTES-induced T cell activation correlates with CD3 expression. J Immunol. 1998;160:426–433. [PubMed] [Google Scholar]
- 26.Dolei A, Biolchini A, Serra C, Currali S, Gomes E, Dianzani F. Increased replication of a T-cell-tropic HIV strain and CXC chemokine receptor-4 induction in T cells treated with macrophage inflammatory protein (MIP)-1α, MIP-1β and RANTES β-chemokines. AIDS. 1998;12:183–190. doi: 10.1097/00002030-199802000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Doms R W, Peiper S C. Unwelcome guests with master keys: how HIV uses chemokine receptors for cellular entry. Virology. 1997;235:179–190. doi: 10.1006/viro.1997.8703. [DOI] [PubMed] [Google Scholar]
- 28.Doranz B J, Rucker J, Yi Y, Smyth R J, Samson M, Peiper S, Parmentier M, Collman R G, Doms R W. A dual-tropic, primary HIV-1 isolate that uses fusin and the β-chemokine receptors CKR-5, CKR-2b as fusion cofactors. Cell. 1996;85:1149–1159. doi: 10.1016/s0092-8674(00)81314-8. [DOI] [PubMed] [Google Scholar]
- 29.Dragic T, Litwin V, Allaway G P, Martin S R, Huang Y, Nagashima K A, Cayanan C, Maddon P J, Koup R A, Moore J P, Paxton W A. HIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5. Nature. 1996;381:667–673. doi: 10.1038/381667a0. [DOI] [PubMed] [Google Scholar]
- 30.Esko J D. Replica plating of animal cells. Methods Cell Biol. 1989;32:387–422. doi: 10.1016/s0091-679x(08)61183-8. [DOI] [PubMed] [Google Scholar]
- 31.Esko J D, Stewart T E, Taylor W H. Animal cell mutants defective in glycosaminoglycan biosynthesis. Proc Natl Acad Sci USA. 1985;82:3197–3201. doi: 10.1073/pnas.82.10.3197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feng Y, Broder C C, Kennedy P E, Berger E A. HIV-1 entry cofactor: functional cDNA cloning of a seven-transmembrane G protein-coupled receptor. Science. 1996;272:872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- 33.Fortin J-F, Cantin R, Lamontagne G, Tremblay M. Host-derived ICAM-1 glycoproteins incorporated on human immunodeficiency virus type 1 are biologically active and enhance viral infectivity. J Virol. 1997;71:3588–3596. doi: 10.1128/jvi.71.5.3588-3596.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gantt S M, Clavijo P, Bai X, Esko J D, Sinnis P. Cell adhesion to a motif shared by the malaria circumsporozoite protein and thrombospondin is mediated by its glycosaminoglycan-binding region and not by CSVTCG. J Biol Chem. 1997;272:19205–19213. doi: 10.1074/jbc.272.31.19205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gluschankof P, Mondor I, Gelderblom H R, Sattentau Q J. Cell membrane vesicles are a major contaminant of gradient-enriched human immunodeficiency virus type 1 (HIV-1) preparations. Virology. 1997;230:125–133. doi: 10.1006/viro.1997.8453. [DOI] [PubMed] [Google Scholar]
- 36.Gordon C J, Muesing M A, Proudfoot A E I, Power C A, Moore J P, Trkola A. Enhancement of human immunodeficiency virus type 1 infection by the CC-chemokine RANTES is independent of the mechanism of virus-cell fusion. J Virol. 1999;73:684–694. doi: 10.1128/jvi.73.1.684-694.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoogewerf A J, Kuschert G S, Proudfoot A E, Borlat F, Clark-Lewis I, Power C A, Wells T N. Glycosaminoglycans mediate cell surface oligomerization of chemokines. Biochemistry. 1997;36:13570–13578. doi: 10.1021/bi971125s. [DOI] [PubMed] [Google Scholar]
- 38.Ilangumaran S, Briol A, Hoessli D. CD44 selectively associates with active src family tyrosine kinases lck and fyn in glycosphongollipid rich plasma membrane domains of human peripheral blood lymphocytes. Blood. 1998;91:3901–3908. [PubMed] [Google Scholar]
- 39.Ito M, Baba M, Sato A, Pauwels R, De Clerq E, Shigeta S. Inhibitory effect of dextran sulfate and heparin on the replication of human immunodeficiency virus (HIV) in vitro. Antiviral Res. 1987;7:361–367. doi: 10.1016/0166-3542(87)90018-0. [DOI] [PubMed] [Google Scholar]
- 40.Jackson T, Ellard F, Ghazaleh R, Brookes S, Blakemore W, Corteyn A, Stuart D, Newman J, King A. Efficient infection of cells in culture by type O foot-and-mouth disease virus requires binding to cell surface heparan sulfate. J Virol. 1996;70:5282–5287. doi: 10.1128/jvi.70.8.5282-5287.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kadan M J, Sturm S, Anderson W F, Eglitis M A. Detection of receptor-specific murine leukemia virus binding to cells by immunofluorescence analysis. J Virol. 1992;66:2281–2287. doi: 10.1128/jvi.66.4.2281-2287.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kakkanaiah V N, Ojo-Amaize E A, Peter J B. Concentrations of circulating beta-chemokines do not correlate with viral load in human immunodeficiency virus-infected individuals. Clin Diagn Lab Immunol. 1998;5:499–502. doi: 10.1128/cdli.5.4.499-502.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Karpus W J, Lukacs N W, Kennedy K J, Smith W S, Hurst S D, Barrett T A. Differential CC chemokine-induced enhancement of T helper cell cytokine production. J Immunol. 1997;158:4129–4136. [PubMed] [Google Scholar]
- 44.Kelly M D, Naif H M, Adams S L, Cunningham A L, Lloyd A R. Dichotomous effects of β-chemokines on HIV replication in monocytes and monocyte-derived macrophages. J Immunol. 1998;160:3091–3095. [PubMed] [Google Scholar]
- 45.Kinter A, Catanzaro A, Monaco J A, Ruiz M, Justement J, Moir S, Arthos J, Oliva A, Ehler L, Mizell S, Jackson R, Ostrowski M, Hoxie J, Offord R, Fauci A S. CC-chemokines enhance the replication of T tropic strains of HIV-1 in CD4+ T cells: role of signal transduction. Proc Natl Acad Sci USA. 1998;95:11880–11885. doi: 10.1073/pnas.95.20.11880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Klimstra W, Ryman K, Johnston R. Adaptation of Sindbis virus to BHK cells selects for use of heparan sulfate as an attachment receptor. J Virol. 1998;72:7357–7366. doi: 10.1128/jvi.72.9.7357-7366.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kozak S L, Platt E J, Madani N, Ferro F E, Jr, Peden K, Kabat D. CD4, CXCR-4, and CCR-5 dependencies for infection by primary patient and laboratory-adapted isolates of human immunodeficiency virus type 1. J Virol. 1997;71:873–882. doi: 10.1128/jvi.71.2.873-882.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Krowka J F, Gesner M L, Ascher M S, Sheppard H W. Lack of associations of chemotactic cytokines with viral burden, disease progression, or lymphocyte subsets in HIV-infected individuals. Clin Immunol Immunopathol. 1997;85:21–27. doi: 10.1006/clin.1997.4411. [DOI] [PubMed] [Google Scholar]
- 49.Lidholt K, Weinke J L, Kiser C S, Lugemwa F N, Bame K J, Cheifetz S, Massague J, Lindahl U, Esko J D. A single mutation affects both N-acetylglucosaminyltransferase and glucuronosyltransferase activities in a Chinese hamster ovary cell mutant defective in heparan sulfate biosynthesis. Proc Natl Acad Sci USA. 1992;89:2267–2271. doi: 10.1073/pnas.89.6.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lubkowski J, Bujacz G, Boque L, Domaille P J, Handel T M, Wlodawer A. The structure of MCP-1 in two crystal forms provides a rare example of variable quaternary interactions. Nat Struct Biol. 1997;4:64–69. doi: 10.1038/nsb0197-64. [DOI] [PubMed] [Google Scholar]
- 51.Mack M, Luckow B, Nelson P J, Lihak J, Simmons G, Clapham P R, Signoret N, Marsh M, Stangassinger M, Borlat F, Wells T N C, Schlöndorff D, Proudfoot A E I. Aminooxypentane-RANTES induces CCR5 internalization but inhibits recycling: a novel inhibitory mechanism of HIV infectivity. J Exp Med. 1998;187:1215–1224. doi: 10.1084/jem.187.8.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McKenzie S W, Dallalio G, North M, Frame P, Means R T. Serum chemokine levels in patients with non-progressing HIV infection. AIDS. 1996;10:F29–F33. doi: 10.1097/00002030-199610090-00001. [DOI] [PubMed] [Google Scholar]
- 53.Miller D G, Miller A D. A family of retroviruses that utilize related phosphate transporters for cell entry. J Virol. 1994;68:8270–8276. doi: 10.1128/jvi.68.12.8270-8276.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mondor I, Ugolini S, Sattentau Q J. Human immunodeficiency virus type 1 attachment to HeLa CD4 cells is CD4 independent and gp120 dependent and requires cell surface heparans. J Virol. 1998;72:3623–3634. doi: 10.1128/jvi.72.5.3623-3634.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Montgomery R I, Warner M S, Lum R J, Spear P G. Herpes simplex virus-1 entry into cells mediated by a novel member of the TNF/NGF receptor family. Cell. 1996;87:427–436. doi: 10.1016/s0092-8674(00)81363-x. [DOI] [PubMed] [Google Scholar]
- 56.Moore J P, Trkola A, Dragic T. Co-receptors for HIV-1 entry. Curr Opin Immunol. 1997;9:551–562. doi: 10.1016/s0952-7915(97)80110-0. [DOI] [PubMed] [Google Scholar]
- 57.Morgan J R, LeDoux J M, Snow R G, Tompkins R G, Yarmush M L. Retrovirus infection: effect of time and target cell number. J Virol. 1995;69:6994–7000. doi: 10.1128/jvi.69.11.6994-7000.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Moriuchi H, Moriuchi M, Fauci A S. Factors secreted by human T lymphotropic virus type I (HTLV-I)-infected cells can enhance or inhibit replication of HIV-1 in HTLV-I-uninfected cells: implications for in vivo coinfection with HTLV-I and HIV-1. J Exp Med. 1998;187:1689–1697. doi: 10.1084/jem.187.10.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Moriuchi M, Moriuchi H, Combadiere C, Murphy P M, Fauci A S. CD8+ T cell-derived factor(s), but not β-chemokines RANTES, MIP-1α, and MIP-1β, suppress HIV-1 replication in monocyte/macrophages. Proc Natl Acad Sci USA. 1996;93:15341–15345. doi: 10.1073/pnas.93.26.15341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Muller P, Engelstadter M, Werner A, Braner J, Staszewski S, Miller V, Doerr H W, Kurth R, Cichutek K. Increased serum and mRNA levels of RANTES associated with elevated levels of activated CD8+CD38+ T cells in HIV-1 infected individuals. Intervirology. 1997;40:263–270. doi: 10.1159/000150556. [DOI] [PubMed] [Google Scholar]
- 61.Nussbaum O, Broder C C, Berger E A. Fusogenic mechanisms of enveloped-virus glycoproteins analyzed by a novel recombinant vaccinia virus-based assay quantitating cell fusion-dependent reporter gene activation. J Virol. 1994;68:5411–5422. doi: 10.1128/jvi.68.9.5411-5422.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ohshiro Y, Murakami T, Matsuda K, Nishioka K, Yoshida K, Yamamoto N. Role of cell surface glycosaminoglycans of human T cells in human immunodeficiency virus type-1 (HIV-1) infection. J Virol. 1996;40:827–835. doi: 10.1111/j.1348-0421.1996.tb01148.x. [DOI] [PubMed] [Google Scholar]
- 63.Okada T, Gurney M. Single basic amino acid substitutions at position 302 or 320 in the V3 domain of HIV type 1 are not sufficient to alter the antiviral activity of dextran sulfate and heparin. AIDS Res Hum Retroviruses. 1995;11:571–575. doi: 10.1089/aid.1995.11.571. [DOI] [PubMed] [Google Scholar]
- 64.Oravecz T, Pall M, Norcross M A. β-Chemokine inhibition of monocytotropic HIV-1 infection. Interference with a postbinding fusion step. J Immunol. 1996;157:1329–1332. [PubMed] [Google Scholar]
- 65.Oravecz T, Pall M, Roderiquez G, Gorrell M D, Ditto M, Nguyen N Y, Boykins R, Unsworth E, Norcross M A. Regulation of the receptor specificity and function of the chemokine RANTES (Regulated on Activation, Normal T cell Expressed and Secreted) by dipeptidyl peptidase IV (CD26)-mediated cleavage. J Exp Med. 1997;186:1865–1872. doi: 10.1084/jem.186.11.1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Oravecz T, Pall M, Wang J, Roderiquez G, Ditto M, Norcross M A. Regulation of anti-HIV-1 activity of RANTES by heparan sulfate proteoglycans. J Immunol. 1997;159:4587–4592. [PubMed] [Google Scholar]
- 67.Orentas R J, Hildreth J E K. Association of host cell surface adhesion receptors and other membrane proteins with HIV and SIV. AIDS Res Hum Retroviruses. 1993;9:1157–1165. doi: 10.1089/aid.1993.9.1157. [DOI] [PubMed] [Google Scholar]
- 68.Orloff G M, Orloff S L, Kennedy M S, Maddon P J, McDougal J S. Penetration of CD4 T cells by HIV-1. The CD4 receptor does not internalize with HIV, and CD4-related signal transduction events are not required for entry. J Immunol. 1991;146:2578–2587. [PubMed] [Google Scholar]
- 69.Ott V, Rapraeger A. Tyrosine phosphorylation of syndecan-1 and -4 cytoplasmic domains in adherent B82 fibroblasts. J Biol Chem. 1998;273:35291–35298. doi: 10.1074/jbc.273.52.35291. [DOI] [PubMed] [Google Scholar]
- 70.Paavola C D, Hemmerich S, Grunberger D, Polsky I, Bloom A, Freedman R, Mulkins M, Bhakta S, McCarley D, Wiesent L, Wong B, Jarnagin K, Handel T M. Monomeric monocyte chemoattractant protein-1 (MCP-1) binds and activates the MCP-1 receptor CCR2B. J Biol Chem. 1998;273:33157–33165. doi: 10.1074/jbc.273.50.33157. [DOI] [PubMed] [Google Scholar]
- 71.Patel M, Yanagishita M, Rodriquez G, Bou-Habib D C, Oravecz T, Hascall V C, Norcross M A. Cell surface heparan sulfate proteoglycan mediates HIV-1 infection of T cell lines. AIDS Res Hum Retroviruses. 1993;9:167–174. doi: 10.1089/aid.1993.9.167. [DOI] [PubMed] [Google Scholar]
- 72.Poret C D, Lukacs K V, Box G, Takeuchi Y, Collins M K L. Cationic liposomes enhance the rate of transduction by a recombinant retroviral vector in vitro and in vivo. J Virol. 1998;72:4832–4840. doi: 10.1128/jvi.72.6.4832-4840.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Premack B A, Schall T J. Chemokine receptors: gateways to inflammation and infection. Nat Med. 1996;2:1174–1178. doi: 10.1038/nm1196-1174. [DOI] [PubMed] [Google Scholar]
- 74.Proost P, De Meester I, Schols D, Struyf S, Lambeir A-M, Wuyts A, Oppendakker G, De Clercq E, Scharpe S, van Damme J. Amino-terminal truncation of chemokines by CD26/dipeptidyl-peptidase IV. Conversion of RANTES into a potent inhibitor of monocyte chemotaxis and HIV-1-infection. J Biol Chem. 1998;273:7222–7227. doi: 10.1074/jbc.273.13.7222. [DOI] [PubMed] [Google Scholar]
- 75.Proudfoot A E, Power C A, Hoogewerf A, Montjovent M O, Borlat F, Wells T N C. Characterisation of the RANTES/MIP-1 alpha receptor (CC CKR-1) stably transfected in HEK 293 cells and the recombinant ligands. FEBS Lett. 1995;376:19–23. doi: 10.1016/0014-5793(95)01235-x. [DOI] [PubMed] [Google Scholar]
- 76.Rizzuto C D, Sodroski J G. Contribution of virion ICAM-1 to human immunodeficiency virus infectivity and sensitivity to neutralization. J Virol. 1997;71:4847–4851. doi: 10.1128/jvi.71.6.4847-4851.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Roderiquez G, Oravecz T, Yanagishita M, Bou-Habib D C, Mostowski H, Norcross M A. Mediation of human immunodeficiency virus type 1 binding by interaction of cell surface heparan sulfate proteoglycans with the V3 region of envelope gp120-gp41. J Virol. 1995;69:2233–2239. doi: 10.1128/jvi.69.4.2233-2239.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schmidtmayerova H, Sherry B, Bukrinsky M. Chemokines and HIV replication. Nature. 1996;382:767. doi: 10.1038/382767a0. [DOI] [PubMed] [Google Scholar]
- 79.Secchiero P, Sun D, DeVico A, Crowley R, Reitz M, Jr, Zauli G, Lusso P, Gallo R. Role of the extracellular domain of human herpesvirus 7 glycoprotein B in virus binding to cell surface heparan sulfate proteoglycans. J Virol. 1997;71:4571–4580. doi: 10.1128/jvi.71.6.4571-4580.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Simmons G, Clapham P R, Picard C, Offord R E, Rosenkilde M M, Schwartz T W, Buser R, Wells T N C, Proudfoot A E I. Potent inhibition of HIV-1 infectivity in macrophages and lymphocytes by a novel CCR5 antagonist. Science. 1997;276:276–279. doi: 10.1126/science.276.5310.276. [DOI] [PubMed] [Google Scholar]
- 81.Sinnis P, Willnow T E, Briones M R, Herz J, Nussenzweig V. Remnant lipoproteins inhibit malaria sporozoite invasion of hepatocytes. J Exp Med. 1996;184:945–954. doi: 10.1084/jem.184.3.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Taub D D, Turcovski-Corrales S M, Key M L, Longo D L, Murphy W J. Chemokines and T lymphocyte activation. J Immunol. 1996;156:2095–2103. [PubMed] [Google Scholar]
- 83.Trkola, A., and A. Garcia-Sastre. Unpublished results.
- 84.Trkola A, Dragic T, Arthos J, Binley J M, Olson W C, Allaway G P, Cheng-Mayer C, Robinson J, Maddon P J, Moore J P. CD4 dependent, antibody sensitive interactions between HIV-1 and its co-receptor CCR5. Nature. 1996;384:184–186. doi: 10.1038/384184a0. [DOI] [PubMed] [Google Scholar]
- 85.Trkola A, Paxton W A, Monard S P, Hoxie J A, Siani M A, Thompson D A, Wu L, Mackay C R, Horuk R, Moore J P. Genetic subtype independent inhibition of human immunodeficiency virus type 1 replication by CC and CXC chemokines. J Virol. 1998;72:396–404. doi: 10.1128/jvi.72.1.396-404.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Trybala E, Bergstrom T, Spillman D, Svennerholm B, Olofsson S, Flynn S, Ryan P. Mode of interaction between pseudorabies virus and heparan sulfate/heparin. Virology. 1996;218:35–42. doi: 10.1006/viro.1996.0163. [DOI] [PubMed] [Google Scholar]
- 87.Turner L, Ward S G, Westwick J. RANTES-activated human T lymphocytes. J Immunol. 1995;155:2437–2444. [PubMed] [Google Scholar]
- 88.Ugolini S, Mondor I, Parren P W H I, Burton D R, Tilley S, Klasse P J, Sattentau Q J. Inhibition of virus attachment to CD4+ target cells is a major mechanism of T cell line-adapted HIV-1 neutralization. J Exp Med. 1997;186:1287–1298. doi: 10.1084/jem.186.8.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wagner L, Yang O O, Garcia-Zepeda E A, Ge Y, Kalams S A, Walker B D, Pasternak M S, Luster A D. β-Chemokines are released from HIV-1 specific cytotoxic T-cell granules complexed to proteoglycans. Nature. 1998;391:908–911. doi: 10.1038/36129. [DOI] [PubMed] [Google Scholar]
- 90.Wang H, Paul R, Burgeson R E, Keene D R, Kabat D. Plasma membrane receptors for ecotropic murine retroviruses require a limiting accessory factor. J Virol. 1991;65:6468–6477. doi: 10.1128/jvi.65.12.6468-6477.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ward S G, Bacon K, Westwick J. Chemokines and T lymphocytes: more than an attraction. Immunity. 1998;9:1–11. doi: 10.1016/s1074-7613(00)80583-x. [DOI] [PubMed] [Google Scholar]
- 92.Wells T N C, Power C A, Lusti-Narasimhan M, Hoogewerf A J, Cooke R M, Chung C-W, Peitsch M C, Proudfoot A E I. Selectivity and antagonism of chemokine receptors. J Leukoc Biol. 1996;59:53–60. doi: 10.1002/jlb.59.1.53. [DOI] [PubMed] [Google Scholar]
- 93.Wong M, Fish E N. RANTES and MIP-1α activate STATS in T cells. J Biol Chem. 1998;273:309–314. doi: 10.1074/jbc.273.1.309. [DOI] [PubMed] [Google Scholar]
- 94.Wu L, Gerard N P, Wyatt R, Choe H, Parolin C, Ruffing N, Borsetti A, Cardoso A A, Desjardin E, Newman W, Gerard C, Sodroski J. CD4-induced interaction of primary HIV-1 gp120 glycoproteins with the chemokine receptor CCR-5. Nature. 1996;384:179–183. doi: 10.1038/384179a0. [DOI] [PubMed] [Google Scholar]
- 95.WuDunn D, Spear P G. Initial interaction of herpes simplex virus with cells is binding to heparan sulfate. J Virol. 1989;63:52–58. doi: 10.1128/jvi.63.1.52-58.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ylisastigui L, Vizzavona J, Drakopoulou E, Paindavoine P, Calvo C-F, Parmentier M, Gluckman J C, Vita C, Benjouad A. Synthetic full-length and truncated RANTES inhibit HIV-1 infection of primary macrophages. AIDS. 1998;12:977–984. [PubMed] [Google Scholar]