Abstract
BACKGROUND
Radical laparoscopic gastrectomy is an important treatment modality for gastric cancer. Surgery requires general anesthesia, and patients are susceptible to the effects of anesthetic drugs and carbon dioxide insufflation during the procedure, leading to inflammation or severe pain, which can affect patient outcome.
AIM
To explore the efficacy of combining dexmedetomidine (DEX) with nalbuphine in patients underwent laparoscopic radical gastrectomy for gastric cancer.
METHODS
Patients scheduled to undergo laparoscopic radical gastrectomy were selected and randomly assigned to A or B group. In A group, patients received an intravenous injection of nalbuphine 0.2 mg/kg + DEX 0.4 μg/kg 10 min before the end of surgery; in B group, patients received only an intravenous injection of nalbuphine. The trends in hemodynamic parameter fluctuations, awakening quality during the recovery period, serum inflammatory markers, agitation scores, cough severity, incidence, and duration of postoperative delirium (POD) were compared.
RESULTS
The mean arterial pressure and heart rate in the A group were more stable (P < 0.05). The A group had a lower average awakening time, extubation time, and agitation scores during recovery than the B group. Agitation control in the A group was more effective at different time points (P < 0.05). Patients in the A group had lower serum interleukin (IL)-6, tumour necrosis factor alpha, and IL-10 levels at 1 h after surgery than the B group. The incidence of coughing and duration of POD were lower and shorter in the A group than in the B group. Adverse reactions caused by the two anesthesia methods were less frequent in the A group than in the B group (P < 0.05).
CONCLUSION
The use of DEX and nalbuphine in patients undergoing laparoscopic radical gastrectomy for gastric cancer help reducing the inflammatory response, cough severity, and agitation and helps maintain hemodynamic stability.
Keywords: Laparoscopic radical gastrectomy, Gastric cancer, Dexmedetomidine, Nalbuphine, Anesthetic quality, Anesthetic effect, Restlessness, Delirium
Core Tip: This study analyzed the effects of dexmedetomidine combined with nalbuphine on the quality and effect of anesthesia in patients undergoing laparoscopic radical gastrectomy for gastric cancer, in order to provide clinical reference.
INTRODUCTION
Radical laparoscopic gastrectomy is an important treatment modality for gastric cancer. Surgery requires general anesthesia, and patients are susceptible to the effects of anesthetic drugs and carbon dioxide (CO2) insufflation during the procedure, leading to inflammation or severe pain, which can affect patient outcomes[1,2]. During the postoperative recovery phase, the anesthetic and analgesic effects of anesthetic drugs gradually diminish[3,4]. At the same time, patients have a reduced tolerance to tracheal intubation and pain, making them prone to restlessness, coughing, and postoperative delirium (POD), which are unfavorable for postoperative recovery[5,6]. Therefore, anesthesiologists must manage the anesthesia process during the perioperative period. Nalbuphine is widely used for analgesia and anesthesia; however, clinical observations have shown that general anesthesia’s anti-inflammatory and analgesic effects in combination with nalbuphine require improvement. Therefore, combining it with other drugs is necessary to enhance anesthetic effectiveness[7,8]. Dexmedetomidine (DEX) has a dual action of sedation and analgesia and contributes to hemodynamic stability[9]. Studies have shown[5,10] that intravenous administration of DEX during general anesthesia can reduce the incidence of coughing and restlessness to some extent. This study analyzed the effect of the combination of DEX and nalbuphine on anesthetic quality and effectiveness in patients undergoing laparoscopic radical gastrectomy for gastric cancer to provide a clinical reference.
MATERIALS AND METHODS
General data
This study included patients scheduled to undergo laparoscopic radical gastrectomy for gastric cancer under general anesthesia at our institution between January 2021 and January 2023. Using a random number table, they were divided into a A group and B group, each consisting of 80 patients. The baseline data of the patients in the combination and B groups were compared (P > 0.05; Table 1).
Table 1.
Comparison of baseline data between the two groups of subjects
| Group | n | Age (yr) | BMI (kg/m2) |
Sex, n (%)
|
ASA grade, n (%)
|
Smoking | Operation time (min) | Blood loss (mL) | Hypertension, n (%) | Diabetes, n (%) | TNM stage, n (%) | ||||
|
Male
|
Female
|
Grade I
|
Grade II
|
||||||||||||
| A group | 80 | 65.30 ± 7.30 | 22.88 ± 2.06 | 43 (53.75) | 37 (46.25) | 30 (37.50) | 50 (62.50) | 29 (36.25) | 164.80 ± 22.00 | 87.90 ± 12.40 | 22 (27.50) | 16 (20.00) | 18 (22.50) | 27 (33.75) | 35 (43.75) |
| B group | 80 | 63.80 ± 8.00 | 22.59 ± 1.88 | 35 (43.75) | 45 (56.25) | 37 (46.25) | 43 (53.75) | 21 (26.25) | 160.50 ± 24.10 | 91.00 ± 14.20 | 26 (32.50) | 23 (28.75) | 24 (30.00) | 30 (37.50) | 26 (32.50) |
| t/χ2 | 1.239 | 0.930 | 1.601 | 1.258 | 1.862 | 1.179 | -1.471 | 0.476 | 1.661 | 2.343 | |||||
| P value | 0.217 | 0.354 | 0.206 | 0.262 | 0.172 | 0.240 | 0.143 | 0.490 | 0.197 | 0.310 | |||||
BMI: Body mass index; ASA: American Society of Anesthesiologists; TNM: Tumour, node, metastasis.
Inclusion criteria: (1) The diagnostic criteria of gastric cancer patients (refer to the criteria in the Clinical Diagnosis and Treatment Guidelines for Gastric Cancer[11]) confirmed by pathological biopsy of the tissue taken by gastroscope; (2) patients with American Society of Anesthesiologists classification criteria[12] levels I-II; (3) patients aged 45-75 years; and (4) patients with tumour, node, metastasis (TNM) stage ≤ IIIA who can tolerate laparoscopic radical surgery. The same group of medical staff performed all operations. The Medical Ethics Committee approved the study protocol.
Exclusion criteria: (1) Gastrointestinal obstruction or perforation; (2) liver and kidney dysfunctions; (3) blood diseases; (4) alcoholism; (5) drug abuse or long-term use of analgesics; and (6) distant tumor metastases that cannot be treated with radical surgery.
Anesthesia methods
The patients were required to fast for 8 h before surgery. Standard intravenous access was established upon entering the operating room, and a multifunctional monitor was used to monitor patients’ vital signs. Both groups received general intravenous anesthesia induction with the following medications: 0.30 mg/kg etomidate, 0.15 mg/kg cisatracurium besylate, 0.03 mg/kg midazolam, and 0.40 μg/kg sufentanil. Tracheal intubation was performed following muscle relaxation. Anesthesia maintenance during surgery involved continuous infusion through a microinfusion pump with 4-6 mg/(kg/h) propofol and 0.1-0.3 μg/(kg/min) remifentanil, with intermittent injections of cisatracurium besylate. The tidal volume was set at 8.0 mL/kg, and the anesthesia ventilator frequency was set at 12 breaths/min. After successful induction of anesthesia, laparoscopic radical gastrectomy for gastric cancer was performed. In the B group, patients received an intravenous injection of 0.2 mg/kg nalbuphine 10 min before the end of surgery; in contrast, in the A group, patients received an intravenous injection of 0.2 mg/kg nalbuphine + 0.4 μg/kg DEX 10 min before the end of surgery. The administration of propofol and remifentanil was discontinued 10 min before the conclusion of the surgery, and tracheal extubation was performed after the patient regained consciousness. Postoperatively, continuous intravenous PCIA was administered, consisting of 1.5 μg/kg sufentanil citrate injection combined with 0.2 mg/kg dezocine injection (Yangtze River Pharmaceutical Group Co., Ltd., specification: 1 mL: 5 mg, China Food and Drug Administration Approval Number H20080329), diluted in 100 mL of normal saline.
Surgical methods
The patient was positioned in the supine position, and standard disinfection and draping procedures were carried out, including placing a urinary catheter. A 10 mm curved incision was made at the lower border of the umbilicus, and a Veress needle was used for abdominal puncture. CO2 gas was introduced to create a pneumoperitoneum, and the pressure was maintained at 12 mmHg. A 10 mm trocar was inserted through the puncture site, and a laparoscope was introduced into the abdominal cavity. A 12 mm incision was made below the left costal margin along the anterior axillary line for the main operative port. As the secondary operative port, a 5 mm incision was made 5 cm above and to the left of the umbilicus. On the right side, a 5 mm incision was made below the right costal margin along the anterior axillary line, and a 10 mm incision was made slightly above the umbilicus along the midline. The abdominal cavity was explored to determine the appropriate surgical approach and resection range. A midline incision of approximately 6 cm was made in the upper abdomen, and various abdominal wall layers were sequentially incised. A wound protector was then placed on the incision. Roux-en-Y esophagojejunostomy was performed between the esophagus and the jejunum. After completion of the surgery, the abdominal cavity was irrigated, and a drainage tube was left in place. The abdominal layers were closed step-by-step, and the surgery was concluded.
Observation indicators and check methods
The hemodynamic indexes [mean arterial pressure (MAP) and heart rate (HR)] fluctuation trend, recovery period quality (recovery time and extubation time), serum inflammatory factors [interleukin (IL)-6, tumour necrosis factor alpha (TNF-α), IL-10], agitation score, cough degree, and incidence and duration of POD were compared between the two groups.
Venous blood samples were collected from patients’ outer elbow veins before and 1 h after surgery. The serum was separated after centrifugation at 2000 revolutions/min for 15 min. Enzyme-linked immunosorbent assay (ELISA) was used to measure IL-6, TNF-α, and IL-10 levels. The ELISA kits were purchased from Nanjing Jiancheng Bioengineering Institute.
The Riker Sedation-Agitation Scale was used to assess the level of agitation during the awakening period. This scale has a seven-point score, with lower scores indicating better sedation. A total score of ≥ 4 points is considered agitation; in contrast, < 4 points indicate sedation[13].
The modified Minogue Scale assessed cough severity during extubation[14]. The scale categorizes patients as grade 1, no coughing and no coughing during extubation. Grade 2: Mild coughing, with 1-2 coughing episodes during extubation. Grade 3: Moderate coughing, with 3-7 coughing episodes during extubation. Grade 4: Severe coughing with > seven episodes of coughing during extubation. Grade 5: Extremely severe coughing and agitation during extubation.
Statistical analysis
Data were analyzed using SPSS21.0. The statistical description of the measurement data of serum IL-6, TNF-α, IL-10, and other measurement data collected in this study adopts the (mean ± SD) method. The measured MAP and HR values were repeated measurement data. The variance analysis method of repeated measurements was adopted for statistical comparison, and the t-test was used to compare the two groups of non-non-repetitive measurement data. Count data, such as the degree of cough and adverse reactions during extubation, were presented as rates (%). The data were compared by χ2 test or rank sum test.
RESULTS
Comparison of fluctuation of hemodynamic indexes between the combination and B groups
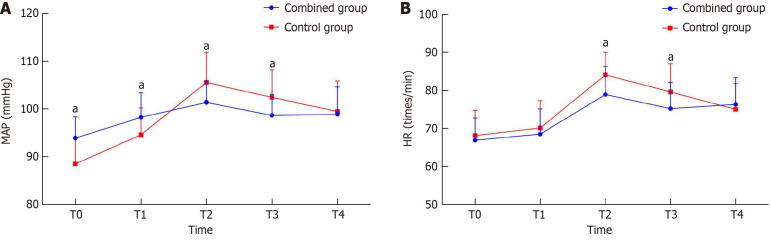
The comparison between the combination and B groups revealed the following trends in MAP and HR fluctuations at different time points. At the end of surgery and before extubation, the MAP in the A group was higher than that in the B group. Immediately and 5 min after extubation, both MAP and HR in the A group were lower than those in the B group, and MAP and HR in the A group were closer to the levels observed 10 min after extubation, indicating a smoother overall trend (P < 0.05) (Table 2 and Figure 1).
Table 2.
Comparison of fluctuation of hemodynamic indexes between combined group and B group, mean ± SD
|
Index
|
Group
|
At the end of surgery
|
Before extubation
|
Immediately after extubation
|
5 min after extubation
|
10 min after extubation
|
| MAP (mmHg) | A group (n = 80) | 93.91 ± 4.40 | 98.25 ± 5.14 | 101.41 ± 4.47 | 98.65 ± 4.40 | 98.91 ± 5.74 |
| B group (n = 80) | 88.50 ± 5.51 | 94.59 ± 5.66 | 105.58 ± 6.28 | 102.41 ± 5.75 | 99.50 ± 6.38 | |
| t value | 6.862 | 4.282 | -4.839 | -4.645 | -0.615 | |
| P value | 0 | 0 | 0 | 0 | 0.540 | |
| HR (times/min) | A group (n = 80) | 66.91 ± 5.88 | 68.50 ± 6.60 | 78.94 ± 7.40 | 75.19 ± 6.94 | 76.33 ± 7.00 |
| B group (n = 80) | 68.13 ± 6.60 | 70.13 ± 7.17 | 84.10 ± 5.91 | 79.58 ± 7.47 | 75.00 ± 6.81 | |
| t value | -1.234 | -1.496 | -4.873 | -3.851 | 1.218 | |
| P value | 0.219 | 0.137 | 0 | 0 | 0.225 |
MAP: Mean arterial pressure; HR: Heart rate.
Figure 1.
Comparative analysis. A: Comparative analysis of mean arterial pressure fluctuation trend between the two groups of patients; B: Comparative analysis of heart rate fluctuation change trend between the two groups of patients. MAP: Mean arterial pressure; HR: Heart rate. aP < 0.05.
Comparison of the quality of the recovery period between the combination and B groups
The patients in the A group had shorter average awakening times, shorter extubation times, and lower agitation scores during the awakening period than those in the B group. The A group had better control of agitation at different times during the awakening period, leading to a smoother and more comfortable recovery (P < 0.05; Table 3).
Table 3.
Comparison of the quality of recovery period between the combined group and the B group, mean ± SD
|
Group
|
n
|
Recovery time (min)
|
Extubation time (min)
|
Agitation score (score)
|
| A group | 80 | 20.81 ± 1.77 | 22.07 ± 2.48 | 3.87 ± 0.68 |
| B group | 80 | 22.08 ± 2.51 | 24.18 ± 2.53 | 4.42 ± 0.81 |
| t value | -3.698 | -5.327 | -4.651 | |
| P value | 0 | 0 | 0 |
Comparison of serum inflammatory factors levels between the combination and B groups
The baseline serum IL-6, TNF-α, and IL-10 levels were compared before surgery in both groups (P > 0.05). However, 1 h after surgery, serum IL-6, TNF-α, and IL-10 Levels in the A group were lower than those in the B group. This suggests that the anesthesia method used in the A group was more effective in reducing the degree of inflammatory response induced by surgery (P < 0.05; Table 4).
Table 4.
Comparison of serum inflammatory factors levels between the combined group and the B group, mean ± SD
| Group | n |
IL-6 (pg/mL)
|
TNF-α (pg/mL)
|
IL-10 (ng/mL)
|
|||
|
Before operation
|
1 h after operation
|
Before operation
|
1 h after operation
|
Before operation
|
1 h after operation
|
||
| A group | 80 | 44.81 ± 6.50 | 113.92 ± 13.74 | 32.04 ± 5.94 | 84.39 ± 11.73 | 29.83 ± 4.47 | 75.40 ± 9.37 |
| B group | 80 | 42.94 ± 7.17 | 128.59 ± 15.50 | 33.78 ± 7.20 | 89.46 ± 13.18 | 31.11 ± 6.00 | 83.49 ± 12.30 |
| t value | 1.728 | -6.335 | -1.667 | -2.570 | -1.530 | -4.680 | |
| P value | 0.086 | 0 | 0.097 | 0.011 | 0.128 | 0 | |
IL: Interleukin; TNF-α: Tumour necrosis factor alpha.
Comparison of the degree of cough during extubation between the combination and B groups
When comparing the severity of coughing during extubation between the combination and B groups, patients in the B group experienced a more severe degree of coughing than those in the A group (P < 0.05; Table 5).
Table 5.
Comparison of the degree of cough during extubation between the combined group and the B group, n (%)
|
Group
|
n
|
Grade 1
|
Grade 2
|
Grade 3
|
Grade 4
|
Grade 5
|
| A group | 80 | 22 (27.50) | 51 (63.75) | 7 (8.75) | 0 (0) | 0 (0) |
| B group | 80 | 11 (13.75) | 41 (51.25) | 27 (33.75) | 1 (1.25) | 0 (0) |
| Z value | -3.889 | |||||
| P value | 0 |
Comparison of the incidence and duration of POD in the A group and B groups
The patients in the A group had a lower incidence and shorter POD duration than those in the B group. This indicated that the anesthesia method used in the A group was generally more favorable for reducing surgery-induced coughing (P < 0.05; Table 6).
Table 6.
Comparison of the incidence and duration of postoperative delirium in the combined group and the B group
|
Group
|
n
|
Incidence of POD (%)
|
Duration of POD (h)
|
| A group | 80 | 11 (13.75) | 38.9 ± 7.1 |
| B group | 80 | 21 (26.25) | 46.4 ± 8.3 |
| t/χ2 | 3.906 | -6.142 | |
| P value | 0.048 | 0 |
POD: Postoperative delirium.
Comparison of the incidence of adverse reactions between the combination and B groups
The incidence of adverse reactions was lower in the A group than in the B group (P < 0.05; Table 7).
Table 7.
Comparison of the incidence of adverse reactions between the combined group and the B group
|
Group
|
n
|
Nausea
|
Vomiting
|
Pruritus
|
Hypotension
|
Bradycardia
|
Adverse reactions (%)
|
| A group | 80 | 9 | 2 | 1 | 1 | 0 | 13 (16.25) |
| B group | 80 | 16 | 4 | 2 | 2 | 2 | 26 (32.50) |
| χ2 | 5.730 | ||||||
| P value | 0.017 |
DISCUSSION
Laparoscopic radical gastrectomy is the main surgical method for treating gastric cancer, aiming to completely remove the tumor and its potentially affected surrounding tissues, including some or all of the gastric tissue and surrounding lymph nodes. Lymph node dissection is an important component of surgery, and its type depends on the stage and location of the tumor, including different levels of dissection such as D1 and D2. The surgical time varies depending on the patient’s specific situation, the complexity of the surgery, and the surgeon’s experience. Laparoscopic radical gastrectomy for gastric cancer can induce significant stress responses in patients, leading to drastic fluctuations in blood pressure and HR. Mitigating the extent of this stress response is important for patient prognosis[15,16]. The results of this study indicated that the A group exhibited more stable MAP and HR than the B group, suggesting that using DEX in combination with nalbuphine during laparoscopic radical gastrectomy is beneficial for maintaining hemodynamic stability. The sedative and analgesic mechanisms of nalbuphine are similar to those of opioids, and their impact on hemodynamics should be closely monitored in clinical practice[17,18]. Furthermore, DEX can significantly reduce the release of norepinephrine, inhibit excitation of the sympathetic nervous system, and promote the release of vasodilatory substances to inhibit vasoconstriction. This effect helps reduce the degree of fluctuation in HR and MAP during extubation. In the context of this study, the combination of DEX with nalbuphine on the foundation of nalbuphine alone can play a significant role in maintaining hemodynamic stability.
The results of this study indicated that the patients in the A group had shorter average awakening times, shorter extubation times, and lower agitation scores during the awakening period than those in the B group. This suggests that using DEX combined with nalbuphine during laparoscopic radical gastrectomy is advantageous in reducing the degree of agitation and improving the quality of patient awakening. DEX can maintain a certain level of sedation, has the advantage of not causing respiratory depression, and is easy to awaken from[19,20]. DEX, which belongs to the imidazole derivative class, exerts its sedative effect by stimulating the alpha-2C receptor subtype, which synergizes with opioid drugs and reduces the required dose of opioid medications[21,22]. This drug has a relatively short duration of action, improves cardiovascular stability during surgery, and reduces the incidence of agitation. DEX can promote patient tolerance to endotracheal tubes and significantly reduce the average awakening and extubation times.
There has been limited research on the combined use of DEX and nalbuphine for pain and its anti-inflammatory effects in laparoscopic radical gastrectomy for gastric cancer[23,24]. The results of this study show that 1 h after surgery, patients in the A group had significantly lower levels of serum IL-6, TNF-α, and IL-10 compared to the B group. This suggests that DEX, in combination with nalbuphine, is more effective in reducing inflammatory marker levels than nalbuphine alone. Although the effect of nalbuphine on visceral pain is evident when combined with general anesthesia, its ability to suppress inflammatory cytokine levels still has room for improvement[25]. Nalbuphine can bind to μ and κ receptors and exert sedative and analgesic effects by activating κ receptors in the bone marrow[26,27]. DEX can significantly inhibit the release of glutamate and catecholamines, reducing glutamate toxicity and excitability, thereby reducing the degree of stress and inflammatory response in the body[28]. Moreover, the combined use of both drugs can more effectively inhibit the transmission of pain signals, enhance analgesic effects, and consequently alleviate the degree of the inflammatory response.
This study showed that cough in the B group was generally more severe than in the A group (P < 0.05). This indicated that DEX + nalbuphine can effectively improve patients’ coughing degree. Studies have confirmed[29,30] that the combination of nalbuphine and DEX anesthesia can reduce the degree of stress response in patients during endotracheal intubation and increase the patient’s tolerance to mechanical stimulation of the endotracheal tube, thus playing a role in improving coughing.
CONCLUSION
The use of DEX and nalbuphine in patients undergoing laparoscopic radical gastrectomy for gastric cancer help reducing the inflammatory response, cough severity, and agitation and helps maintain hemodynamic stability.
Footnotes
Institutional review board statement: This study was reviewed and approved by the institutional review board of The Second Affiliated Hospital of Shandong First Medical University.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: There are no conflicts of interest to report.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Christodoulidis G, Greece S-Editor: Chen YL L-Editor: A P-Editor: Guo X
Contributor Information
Guo-Guang Zhao, Department of Anesthesiology, The Second Affiliated Hospital of Shandong First Medical University, Tai’an 271000, Shandong Province, China.
Chao Lou, Department of Anesthesiology, The Second Affiliated Hospital of Shandong First Medical University, Tai’an 271000, Shandong Province, China.
Rong-Lei Gao, Department of Anesthesiology, The Second Affiliated Hospital of Shandong First Medical University, Tai’an 271000, Shandong Province, China.
Fu-Xing Lei, Department of Anesthesiology, The Second Affiliated Hospital of Shandong First Medical University, Tai’an 271000, Shandong Province, China.
Jing Zhao, Department of Dermatology, The Second Affiliated Hospital of Shandong First Medical University, Tai’an 271000, Shandong Province, China. 15662019899@163.com.
Data sharing statement
The data are available from the corresponding author.
References
- 1.Liu R, Suo S, Wang Y, Wang M. Effects of Dexmedetomidine and Propofol on Postoperative Analgesia and the Cellular Immune Function of Patients Undergoing Radical Gastrectomy for Gastric Cancer. Contrast Media Mol Imaging. 2022;2022:7440015. doi: 10.1155/2022/7440015. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Liao YQ, Min J, Wu ZX, Hu Z. Comparison of the effects of remimazolam and dexmedetomidine on early postoperative cognitive function in elderly patients with gastric cancer. Front Aging Neurosci. 2023;15:1123089. doi: 10.3389/fnagi.2023.1123089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Imaging CMM. Retracted: Effects of Dexmedetomidine and Propofol on Postoperative Analgesia and the Cellular Immune Function of Patients Undergoing Radical Gastrectomy for Gastric Cancer. Contrast Media Mol Imaging. 2023;2023:9854737. doi: 10.1155/2023/9854737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fan Q, Luo J, Zhou Q, Zhang Y, Zhang X, Li J, Jiang L, Lan L. Esketamine opioid-free intravenous anesthesia versus opioid intravenous anesthesia in spontaneous ventilation video-assisted thoracic surgery: a randomized controlled trial. Front Oncol. 2023;13:1145953. doi: 10.3389/fonc.2023.1145953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Govêia CS, Miranda DB, Oliveira LVB, Praxedes FB, Moreira LG, Guimarães GMN. Dexmedetomidine reduces postoperative cognitive and behavioral dysfunction in adults submitted to general anesthesia for non-cardiac surgery: meta-analysis of randomized clinical trials. Braz J Anesthesiol. 2021;71:413–420. doi: 10.1016/j.bjane.2021.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avery P, Morton S, Raitt J, Lossius HM, Lockey D. Rapid sequence induction: where did the consensus go? Scand J Trauma Resusc Emerg Med. 2021;29:64. doi: 10.1186/s13049-021-00883-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shehabi Y, Serpa Neto A, Howe BD, Bellomo R, Arabi YM, Bailey M, Bass FE, Kadiman SB, McArthur CJ, Reade MC, Seppelt IM, Takala J, Wise MP, Webb SA SPICE III Study Investigators. Early sedation with dexmedetomidine in ventilated critically ill patients and heterogeneity of treatment effect in the SPICE III randomised controlled trial. Intensive Care Med. 2021;47:455–466. doi: 10.1007/s00134-021-06356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qin C, Jiang Y, Lin C, Li A, Liu J. Perioperative dexmedetomidine administration to prevent delirium in adults after non-cardiac surgery: A systematic review and meta-analysis. J Clin Anesth. 2021;73:110308. doi: 10.1016/j.jclinane.2021.110308. [DOI] [PubMed] [Google Scholar]
- 9.Guo Q, Ma M, Yu H, Han Y, Zhang D. Dexmedetomidine enables copper homeostasis in cerebral ischemia/reperfusion via ferredoxin 1. Ann Med. 2023;55:2209735. doi: 10.1080/07853890.2023.2209735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Xin Y, Chu T, Liu C, Xu A. Dexmedetomidine attenuates perioperative neurocognitive disorders by suppressing hippocampal neuroinflammation and HMGB1/RAGE/NF-κB signaling pathway. Biomed Pharmacother. 2022;150:113006. doi: 10.1016/j.biopha.2022.113006. [DOI] [PubMed] [Google Scholar]
- 11.Chinese Medical Association Oncology Branch; Journal of Chinese Medical Association. Clinical Guidelines for Diagnosis and Treatment of Gastric Cancer (2021 Edition) Zhonghua Yixue Zazhi. 2022;102:1169–1189. [Google Scholar]
- 12.Huang X, Lin D, Sun Y, Wu A, Wei C. Effect of Dexmedetomidine on Postoperative Sleep Quality: A Systematic Review. Drug Des Devel Ther. 2021;15:2161–2170. doi: 10.2147/DDDT.S304162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spinetta R, Petrillo F, Reibaldi M, Tortori A, Mazzoni M, Metrangolo C, Gelormini F, Ricardi F, Giordano A. Intravitreal DEX Implant for the Treatment of Diabetic Macular Edema: A Review of National Consensus. Pharmaceutics. 2023;15 doi: 10.3390/pharmaceutics15102461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng W, Tian X, Fan J, Jiang X, He W. Application of Dexmedetomidine in Surgical Anesthesia for Gastric Cancer and Its Effects on IL-1β, IL-6, TNF-α and CRP. Cell Mol Biol (Noisy-le-grand) 2023;69:177–181. doi: 10.14715/cmb/2023.69.3.26. [DOI] [PubMed] [Google Scholar]
- 15.Wan W, Hou Z, Qiu Q. Postoperative analgesic effect of dexmedetomidine combined with TPVB applied to open gastrectomy for gastric cancer. Immunopharmacol Immunotoxicol. 2023;45:234–239. doi: 10.1080/08923973.2022.2136573. [DOI] [PubMed] [Google Scholar]
- 16.Ma XF, Lv SJ, Wei SQ, Mao BR, Zhao XX, Jiang XQ, Zeng F, Du XK. Influences of dexmedetomidine on stress responses and postoperative cognitive and coagulation functions in patients undergoing radical gastrectomy under general anesthesia. World J Gastrointest Surg. 2023;15:1169–1177. doi: 10.4240/wjgs.v15.i6.1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gao X, Wang XL. Dexmedetomidine promotes ferroptotic cell death in gastric cancer via hsa_circ_0008035/miR-302a/E2F7 axis. Kaohsiung J Med Sci. 2023;39:390–403. doi: 10.1002/kjm2.12650. [DOI] [PubMed] [Google Scholar]
- 18.Parvizi A, Haddadi S, Faghih Habibi A, Nemati S, Akhtar N, Ramezani H. Dexmedetomidine Efficacy in Quality of Surgical Field During Endoscopic Sinus Surgery. Iran J Otorhinolaryngol. 2019;31:281–288. [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Z, Shen Z, Wang H, Zhang L, Dong R. Effect of dexmedetomidine on the cognitive function of patients undergoing gastric cancer surgery by regulating the PI3K/AKT signaling pathway. Oncol Lett. 2020;19:1151–1156. doi: 10.3892/ol.2019.11224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang GR, Wu Q, Liu WP, Jing YM. Effect of Oxycodone hydrochloride combined with Dexmedetomidine on quality of recovery and stress response after general anesthesia in patients who had Laparoscopic Cholecystectomy. Pak J Med Sci. 2021;37:1408–1413. doi: 10.12669/pjms.37.5.3959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang M, Wang J, Li X, Xu X, Zhao Q, Li Y. A predictive model for postoperative cognitive dysfunction in elderly patients with gastric cancer: a retrospective study. Am J Transl Res. 2022;14:679–686. [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Z, Shao DH, Ma XD, Mao ZM. Dexmedetomidine aggravates hypotension following mesenteric traction during total gastrectomy: a randomized controlled trial. Ann Saudi Med. 2020;40:183–190. doi: 10.5144/0256-4947.2020.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Go SI, Kim JH, Kang JH. Treatment of Opioid Withdrawal Syndrome Triggered by Oxycodone/Naloxone with Dexmedetomidine. J Hosp Palliat Care. 2023;26:18–21. doi: 10.14475/jhpc.2023.26.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang W, Ma Y, Liu Y, Wang P, Liu Y. Effects of Dexmedetomidine Anesthesia on Early Postoperative Cognitive Dysfunction in Elderly Patients. ACS Chem Neurosci. 2022;13:2309–2314. doi: 10.1021/acschemneuro.2c00173. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Sun X, Liang J, Wang X, Cao X. Observation of analgesic effect of dexmedetomidine combined with ketorolac tromethamine in laparoscopic surgery under ERAS. Panminerva Med. 2020;62:280–281. doi: 10.23736/S0031-0808.19.03662-0. [DOI] [PubMed] [Google Scholar]
- 26.Kiski D, Malec E, Schmidt C. Use of dexmedetomidine in pediatric cardiac anesthesia. Curr Opin Anaesthesiol. 2019;32:334–342. doi: 10.1097/ACO.0000000000000731. [DOI] [PubMed] [Google Scholar]
- 27.Wang K, Wu M, Xu J, Wu C, Zhang B, Wang G, Ma D. Effects of dexmedetomidine on perioperative stress, inflammation, and immune function: systematic review and meta-analysis. Br J Anaesth. 2019;123:777–794. doi: 10.1016/j.bja.2019.07.027. [DOI] [PubMed] [Google Scholar]
- 28.Rekatsina M, Theodosopoulou P, Staikou C. Effects of Intravenous Dexmedetomidine Versus Lidocaine on Postoperative Pain, Analgesic Consumption and Functional Recovery After Abdominal Gynecological Surgery: A Randomized Placebo-controlled Double Blind Study. Pain Physician. 2021;24:E997–E1006. [PubMed] [Google Scholar]
- 29.Singh A, Brenna CTA, Broad J, Kaustov L, Choi S. The Effects of Dexmedetomidine on Perioperative Neurocognitive Outcomes After Cardiac Surgery: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Ann Surg. 2022;275:864–871. doi: 10.1097/SLA.0000000000005196. [DOI] [PubMed] [Google Scholar]
- 30.Liu Z, Jin Y, Feng C, Liu G, Wang Y, Zhao X, Liu G. Renoprotective Effect of Intraoperative Dexmedetomidine in Renal Transplantation. Comput Math Methods Med. 2022;2022:9275406. doi: 10.1155/2022/9275406. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available from the corresponding author.