ABSTRACT
Context:
The COVID-19 epidemic has had a substantial influence on the mental health of chronic disease patients. However, there is a scarcity of research on them in Bangladesh.
Aims:
This study aims to explore the prevalence of and identify the risk factors for depression, anxiety, and stress symptoms during the COVID-19 pandemic among people with chronic diseases in Bangladesh.
Materials and Methods:
This cross-sectional study involving face-to-face and telephone interviews was carried out among Bangladeshi people diagnosed with chronic diseases between September and November 2020. The total sample size was 878, and a convenient sampling technique was used. Logistic regression analysis was performed to investigate potential influencing factors for depression, anxiety, and stress.
Results:
The mean age of respondents was 50.10 years. Among them, 35.0%, 36.0%, and 29.0% suffered from depression, anxiety, and stress symptoms, respectively. In multivariable logistic regression, depression had a significant positive association with higher age (≥60 years), lower income, rural residency, and loss of close family members due to COVID-19. Anxiety had a significant positive association with higher age (≥40 years), lower education, lower income, rural residency, and loss of close family members due to COVID-19. Stress had a significant positive association with higher age (≥40 years), no income, rural residency, and loss of close family members due to COVID-19.
Conclusion:
It is urgent to consider the risk of developing mental health distress among chronic disease patients, especially aged people, by health service providers and generate effective programs for emergency situations.
Keywords: Anxiety, chronic disease, COVID-19, depression, stress
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) has been substantially influencing the lifestyle of people globally.[1,2] There have been 222,812,592 confirmed cases up to September 8, 2021, and 4,601,142 have succumbed to this disease or complications resulting from COVID-19.[3] Particularly, older individuals and those with chronic diseases, such as diabetes mellitus (DM), hypertension, chronic respiratory disease, malignancy, and cardiovascular disease, seem to be most vulnerable.[4,5,6] Evidence from China and Italy also indicates that the presence of comorbid chronic illnesses may increase the risk of death from COVID-19.[4,5,6] The COVID-19 pandemic triggered a combination of both physical and mental suffering and unwell-being since its first outbreak.[7] Extreme quarantine measures and fear have made it difficult for individuals to access routine medical care, especially in low- and middle-income countries (LMICs).[8] Thus, it is reasonable to anticipate that patients with chronic diseases will face mental health issues like anxiety, depression, and stress.[9]
The number of people affected by these symptoms tends to be higher than those affected by the infection.[10] Limited knowledge about COVID-19, duration of home confinement, lack of access to healthcare systems, lack of physical activity, social isolation, and uncertainty regarding the economic scenario can be significant psychological stressors [11,12,13] and cause adverse lifestyle changes.[14] Existing literature points to a significant association between mental health conditions and chronic diseases like DM, cardiovascular diseases, and pneumonia.[15,16] The presence of depressive comorbidity with DM in Bangladesh varies from 34% to 60%, depending on age, gender, and diabetes type.[17,18,19] Amid the uncertainty and disruption of the COVID-19 pandemic in Bangladesh, mental health and chronic disease comorbidity may increase.
Apart from physical health, it is common that mental health remains neglected and explored later during a pandemic, especially for LMICs like Bangladesh. In Bangladesh, due to a lack of awareness and indifferent attitude, mental health is considered a stigma; people generally ignore its importance and adverse health impacts.[20] The sudden outbreak of the COVID-19 pandemic and related uncertainty and fear may push the majority of the Bangladeshi population into a higher mental health risk.
Family doctors or primary care physicians play a vital role in reducing the risk of mental health issues in Bangladesh. This is especially crucial considering the country’s inadequate mental health care services availability. Hence, considering their close proximity to the community and their understanding of cultural variables, primary care physicians can play a significant role in treating psychiatric issues triggered by COVID-19.[21]
To the best of our knowledge, few studies have been conducted in Bangladesh exploring the mental health status of people with chronic diseases during COVID-19. Exploratory studies of mental health conditions and associated factors during this time are essential to mitigate future negative mental health outcomes. We hypothesized that the prevalence of mental health distress is high among Bangladeshi residents with chronic diseases during this pandemic. Therefore, this study aims to explore the prevalence of and identify the risk factors for depression, anxiety, and stress symptoms during the COVID-19 pandemic among chronically diseased people in Bangladesh.
Materials and Methods
Study design and study participants
We performed a descriptive cross-sectional study from September and November 2020. Most of the data for this study were collected through face-to-face interviews at public tertiary hospitals in Bangladesh using convenient sampling.[22] However, a small proportion of study participants were interviewed over the phone using snowball sampling procedures.
The inclusion criteria were: (i) Bangladeshi adults (aged ≥18 years) of either sex, (ii) Diagnosed with chronic diseases like DM, hypertension, chronic respiratory cases, malignancy, and cardiovascular disease (diagnosed by registered doctors’ prescription and identified from different tertiary level hospitals in Bangladesh), (iii) understanding the study purpose, and (iv) voluntary participation in our study.
Sample size calculation and technique
Convenient and snowball techniques were used for data collection, and the sample size was calculated by using the following formula:
z2× p × (1 − p)/d2
Here, we considered z = 1.96 and d = 0.05 confidence interval as 95%; the sample proportion was assumed to be 0.5 since this value provided the maximum sample size.[23] Hence, the required sample size was 384. However, using design effect 2.3, the sample size was calculated to be 878. We considered the design effect for this study to increase the sample size and minimize the errors.
Study procedure
The Bangla questionnaire’s validity was verified according to Sousa and Rojjanasrirat’s (2011) guidelines.[24] Two translators, one an expert in the subject matter and the other familiar with Bangla and English, translated the questionnaire. The two translations were reviewed by a four-person committee, who completed the initial Bangla version. Then, the committee finalized the initial draft of the Bangla version. A pre-test was conducted with 10-15 members of the participants to assess the questionnaire’s acceptability and clarity. Following the pre-test, a few minor adjustments were made, but these surveys were not included in the final analysis.
Further, two bilingual translators, who had not seen the English version of the DASS-21, translated the questionnaire backward. The reverse translation was approved by the same panel of experts. A pre-test was then conducted with this pre-final version with 10-15 chronic disease patients to check the item’s suitability, meaning, and difficulty. No item was, however, required to be modified after the pre-testing.
Regarding face-to-face data collection, it took approximately 10-15 minutes to complete the survey, and for telephone interviews, the survey took approximately 15-20 minutes to complete.
Measures
In this study, the structured questionnaire containing questions regarding sociodemographic data and COVID-19-related factors was used for data collection. Sociodemographic variables included age, gender, marital status, education level, occupation, family type, monthly income, and residence. COVID-19-related factors included lost earnings (yes/no) and recently lost close family members (yes/no).
Depression Anxiety Stress Scale 21 (DASS 21)
The Depression Anxiety Stress Scale 21 (DASS-21) is a validated screening instrument for evaluating mental health status and was also used in previous surveys to ascertain the psychological status of the COVID-19 pandemic.[25,26,27] The DASS has a strong construct, concurrent validity, and internal consistency reliability. Therefore, DASS 21 was used to assess depression, anxiety, and stress in this study. The scale includes 21 items divided evenly into three sub-scales of stress, anxiety, and depression with seven items each, and scored on a four-point Likert scale ranging from 0 (“never”) to 3 (“always”). The sub-scale of depression consists of questions 3, 5, 10, 13, 16, 17, and 21, and the cut-off scores were: normal (0–4), mild depression (5–6), moderate depression (7–10), severe depression (11–13), and extremely severe depression (14 and above). The sub-scale of anxiety consists of questions 2, 4, 7, 9, 15, 19, and 20, and the cut-off scores were: normal (0–3), mild anxiety (4–5), moderate anxiety (6–7), severe anxiety (8–9), and extremely severe anxiety (10 and above). The sub-scale of stress consists of questions 1, 6, 8, 11, 12, 14, and 18, and the cut-off scores were: normal (0–7), mild stress (8–9), moderate stress (10–12), severe stress (13–16), and extremely severe stress (17 and above). The validated Bangla version of the DASS 21[28] was used in this study due to its strong psychometric properties and ability to quickly assess stress, anxiety, and depression in Bangladeshi individuals. Alim et al.[28] mentioned Cronbach’s alpha of the total score was 0.989, demonstrating the scale to be reliable. Cronbach’s alpha for depression, anxiety, and stress subscales were 0.987, 0.957, and 0.964, respectively. The correlation was significant at the 0.01 level (2-tailed).
Ethical consideration
Ethics approval was obtained from the Institutional Review Board/Ethical Review Committee (IRB/ERC) of North South University (2020/OR-NSU/IRB-No. 0801), Bangladesh. For face-to-face interviews, consent was obtained from the study participants before the interview. Participants were well briefed on the process, study intent, and data confidentiality. Data were collected anonymously, and their participation was completely voluntary. Participants could withdraw from the study at any time, and no incentives were offered to participate in this study. However, before conducting the telephone interview, all respondents were given proper information about the interview process, and they verbally agreed to participate. They were also informed that their participation was voluntary and that they could withdraw from the interview at any time. The information they provided was kept confidential to ensure their privacy. All instructions were given to them in Bengali. After listening to or reading about the study’s purposes, its nature, and risks and benefits, participants gave their consent to participate in the survey. Those who did not provide their consent were not required to participate in the survey.
Data analysis
Data were analyzed using Statistical Package for Social Sciences (SPSS), IBM Statistics version 25. Descriptive analyses (frequency and percentages) to describe the sociodemographic characteristics and factors related to COVID-19 were performed. Logistic regression analysis was performed to investigate potential influencing factors for depression, anxiety, and stress. The results of regression analyses were reported by the odds ratio (OR) with a 95% confidence interval (CI). The association of variables was deemed statistically significant if the P value was below 0.05.
Results
A total of 878 participants completed the survey, and the mean age was 50.10 years (SD: 13.73). Most of them were female (53.0%), aged 40-59 years (50.3%), and married (87.2%). More than half of the participants had completed secondary level education (52.6%), and 50.8% of the participants’ monthly income was BDT 1,000-30,000. About one-third (35.4%) had a joint family, 46.2% were rural residents, 46.6% lost earnings during COVID-19, and 14.1% had lost close family members during COVID-19 [Table 1].
Table 1.
Sociodemographic characteristics of the study participants (n=878)
| Characteristics | Number | Percentage |
|---|---|---|
| Age | ||
| 18-39 years | 188 | 21.4 |
| 40-59 years | 442 | 50.3 |
| 60 and above years | 248 | 28.2 |
| Mean (SD) | 50.10 (13.73) years | |
| Gender | ||
| Male | 413 | 47.0 |
| Female | 465 | 53.0 |
| Education | ||
| Class 11 and above completed | 171 | 19.5 |
| Class 6-10 completed | 462 | 52.6 |
| Class 5 and below (0-5) | 245 | 27.9 |
| Marital status | ||
| Unmarried | 37 | 4.2 |
| Divorced | 4 | 0.5 |
| Widowed | 71 | 8.1 |
| Married | 766 | 87.2 |
| Family type | ||
| Nuclear | 567 | 64.6 |
| Joint | 311 | 35.4 |
| Monthly income (in BDT) | ||
| >30,000 | 102 | 11.6 |
| 1000-30000 | 446 | 50.8 |
| No income | 330 | 37.6 |
| Residence | ||
| Urban | 472 | 53.8 |
| Rural | 406 | 46.2 |
| Lost your earning COVID-19 | ||
| No | 469 | 53.4 |
| Yes | 409 | 46.6 |
| Lost close family members COVID-19 | ||
| No | 754 | 85.9 |
| Yes | 124 | 14.1 |
Among the study participants, 35.0%, 36.0%, and 29.0% suffered from depression, anxiety, and stress symptoms, respectively [Figure 1]. Depression was categorized as follows: normal 43.2%, mild 12.5%, moderate 21.9%, severe 8.3%, and extremely severe 14.1%. Anxiety was categorized as follows: normal 41.9%, mild 9.0%, moderate 11.7%, severe 9.8%, and extremely severe 27.6%, and stress was categorized as normal 53.3%, mild 12.2%, moderate 15.4%, severe 14.8%, and extremely severe 4.3% [Table 2].
Figure 1.
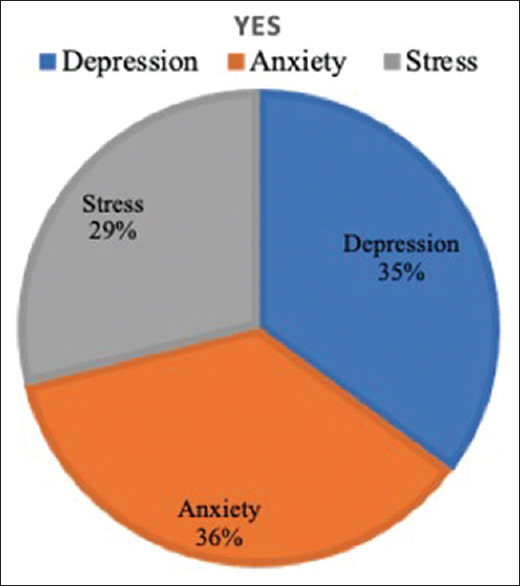
Mental health status among the study participants
Table 2.
Frequency distribution of depression, anxiety, and stress in participants
| Category | Score for depression | Depression n (%) | Score for anxiety | Anxiety n (%) | Score for stress | Stress n (%) |
|---|---|---|---|---|---|---|
| Normal | 0-4 | 379 (43.2) | 0-3 | 368 (41.9) | 0-7 | 468 (53.3) |
| Mild | 5-6 | 110 (12.5) | 4-5 | 79 (9) | 8-9 | 107 (12.2) |
| Moderate | 7-10 | 192 (21.9) | 6-7 | 103 (11.7) | 10-12 | 135 (15.4) |
| Severe | 11-13 | 73 (8.3) | 8-9 | 86 (9.8) | 13-16 | 130 (14.8) |
| Extremely severe | 14+ | 124 (14.1) | 10+ | 242 (27.6) | 17+ | 38 (4.3) |
In multivariable logistic regression, depression had significant positive association with aged ≥60 years [adjusted OR (95% CI); 1.65 (1.04-2.59)], monthly income (1,000-30,000 BDT) [2.16 (1.30-3.57)], no monthly income [3.13 (1.79-5.47)], rural resident [1.78 (1.27-2.47)] and participant recently lost their close family member due to COVID-19 [5.17 (3.07-8.70)]; however, significant negative association was observed with participants from joint family [0.71 (0.52-9.98)] [Table 3]. Anxiety had significant positive association with aged 40-59 years [adjusted OR (95% CI); 1.76 (1.20-2.59)], aged ≥60 years [2.28 (1.44-3.60)], education (primary level) [1.75 (1.05-2.93)], monthly income (1,000-30,000 BDT) [1.91 (1.16-3.14)], no monthly income [2.43 (1.40-4.22)], rural resident [1.83 (1.31-2.56)] and participant recently lost close family member due to COVID-19 [4.66 (2.81-7.75)] [Table 3]. Stress had a significant positive association with those aged 40-59 years [adjusted OR (95% CI); 1.59 (1.08-2.33)], aged ≥60 years [2.20 (1.40-3.47)], no monthly income [2.25 (1.28-3.94),] rural resident [1.75 (1.26-2.43)] and participant recently lost a close family member due to COVID-19 [4.61 (2.89-7.34)] [Table 3].
Table 3.
Association between the demographic characteristics and mental health status
| Variables | Depression n (%) | ORs (95% CI) | Anxiety n (%) | ORs (95% CI) | Stress n (%) | ORs (95% CI) |
|---|---|---|---|---|---|---|
| Age group (in years) | ||||||
| 18-39® | 97 (19.4) | 84 (16.5) | 69 (16.8) | |||
| 40-59 | 245 (49.1) | 1.25 (0.85-1.83) | 260 (51.0) | 1.76 (1.20-2.59)*** | 205 (50.0) | 1.59 (1.08-2.33)*** |
| ≥60 | 157 (31.5) | 1.65 (1.04-2.59)*** | 166 (32.5) | 2.28 (1.44-3.60)*** | 136 (33.2) | 2.20 (1.40-3.47)*** |
| Gender | ||||||
| Male® | 236 (47.3) | 244 (47.8) | 201 (49.0) | 1 | ||
| Female | 263 (52.7) | 0.85 (0.54-1.34) | 266 (52.2) | 0.70 (0.44-1.11) | 209 (51.0) | 0.84 (0.54-1.32) |
| Education | ||||||
| Secondary complete or higher (11 and above) | 80 (16.0) | 1 | 80 (15.7) | 67 (16.3) | 1 | |
| Secondary incomplete (6-10) | 274 (54.9) | 1.42 (0.94-2.16) | 267 (52.4) | 1.42 (0.94-2.15) | 229 (55.9) | 1.45 (0.95-2.20) |
| Primary complete or below (0-5) | 145 (29.1) | 1.25 (0.75-2.09) | 163 (32.0) | 1.75 (1.05-2.93)*** | 114 (27.8) | 1.13 (0.67-1.88) |
| Marital status | ||||||
| Unmarried® | 72 (14.4) | 1 | 66 (12.9) | 1 | 56 (13.7) | 1 |
| Married | 427 (85.6) | 0.76 (0.47-1.20) | 444 (87.1) | 1.04 (0.65-1.66) | 354 (87.2) | 0.91 (0.58-1.43) |
| Family type | ||||||
| Nuclear® | 328 (65.7) | 1 | 329 (64.5) | 1 | 267 (65.1) | 1 |
| Joint | 171 (34.3) | 0.71 (0.52-9.98)*** | 181 (35.5) | 0.79 (0.57-1.08) | 143 (34.9) | 0.78 (0.57-1.07) |
| Monthly income | ||||||
| >30,000® | 35 (7.0) | 1 | 39 (7.6) | 1 | 33 (8.0) | 1 |
| 1,000-30,000 | 253 (50.7) | 2.16 (1.30-3.57)*** | 259 (50.8) | 1.91 (1.16-3.14)*** | 198 (48.3) | 1.50 (0.91-2.50) |
| No income | 211 (42.3) | 3.13 (1.79-5.47)*** | 212 (41.6) | 2.43 (1.40-4.22)*** | 179 (43.7) | 2.25 (1.28-3.94)*** |
| Occupation | ||||||
| Homemaker® | 232 (46.5) | 1 | 243 (47.6) | 1 | 186 (45.4) | 1 |
| Service/business | 188 (37.7) | 1.00 (0.60-1.68) | 188 (36.9) | 0.80 (0.47-1.35) | 157 (38.3) | 1.02 (0.61-1.70) |
| Student/retired/other | 79 (15.8) | 0.69 (0.40-1.20) | 79 (15.5) | 0.63 (0.36-1.10) | 67 (16.3) | 0.71 (0.41-1.22) |
| Residence | ||||||
| Urban® | 242 (48.5) | 1 | 241 (47.3) | 1 | 199 (48.5) | 1 |
| Rural | 257 (51.5) | 1.78 (1.27-2.47)*** | 269 (52.7) | 1.83 (1.31-2.56)*** | 211 (51.5) | 1.75 (1.26-2.43)*** |
| Lost your earning during COVID-19 | ||||||
| No® | 262 (52.5) | 1 | 270 (52.9) | 1 | 222 (54.1) | 1 |
| Yes | 237 (47.5) | 0.95 (0.68-1.31) | 240 (47.1) | 0.81 (0.58-1.13) | 188 (45.9) | 0.84 (0.61-1.17) |
| Recently lost close family members during COVID-19 | ||||||
| No® | 397 (79.6) | 1 | 411 (80.6) | 1 | 319 (77.8) | 1 |
| Yes | 102 (20.4) | 5.17 (3.07-8.70) | 99 (19.4) | 4.66 (2.81-7.75) | 91 (22.2) | 4.61 (2.89-7.34)*** |
***P<0.001; ®=Reference
Discussion
This study investigated the mental health status of people with chronic diseases in Bangladesh during the COVID-19 pandemic. In the present study, more than one-third of the patients suffered from depression (35.0%) and anxiety (36.0%), and one-fourth from stress (29.0%). The prevalence of anxiety in this study was higher than that of depression and stress; this is in keeping with current literature in which anxiety rates are frequently higher than depression and stress.[29,30,31] A study carried out by Kaur et al.[32] showed that the prevalence of depression, anxiety, and stress symptoms were 11.5%, 30.5%, and 12.5%, respectively, in patients with chronic diseases, which was consistent with our study findings. Conversely, several studies among patients with chronic diseases had found higher rates than our study.[30,31] People with chronic diseases present higher levels of psychological symptoms due to the sudden occurrence, lack of good prognosis, and definitive treatment during pandemic situations.[33,34]
Chronic disease occurs mostly in the age range between 35 years or more.[35,36] In the present study, older age (≥60 years) was significantly associated with depression, anxiety, and stress, whereas participants aged 40-59 years had only anxiety and stress. Depression, anxiety, and stress are the most common psychological impacts of chronic diseases within these age groups[37] and can negatively affect the patient’s quality of life. Besides, it may be due to the fact that old age increases the risk of COVID-19-related infection and mortality.[38]
Moreover, no significant relationship was observed between depression, anxiety, and stress, with variables sex, marital status, occupation, and loss of earnings.[39] Additionally, we found the patients with primary education and below had a high level of anxiety. This is probably because of job insecurity, a low level of self-awareness or knowledge of their health.[40]
Depression was negatively associated with joint family type, which is inconsistent with other studies.[41,42] Joint families have been found to provide emotional and interpersonal support, which may have contributed to better experiences and lower levels of depression.[43] In this study, no or lower level of income significantly predicted depression, anxiety, and stress. Studies found that lower family income may lead to more stress responses, anxiety, and depression.[44,45] The reason behind that could be household poverty,[46] limited resources,[47] health care expenditure,[48] and so on.
Multivariate Logistic regression analysis suggested that persons living in urban areas were less likely to suffer from depression, anxiety, and stress than rural areas. This might be explained by the fact that urban areas have better economic, cultural, and educational resources and better access to health, hygiene, and sanitary conditions than rural areas.[49] However, the death of a beloved leads to psychological problems, such as stress.[50] Studies found that the death of a family member may psychologically affect the other family members because they cannot perform the last rites and attend the funeral, which turns into intense grief and stress.[51]
Further, the emergence of the pandemic has hindered efforts to diagnose, treat, and monitor chronic illnesses, particularly in older adults and individuals with comorbidities that can be life-threatening. Additionally, people with multiple chronic diseases need regular check-ups or hospital visits to manage their risk factors. But, due to the COVID-19 pandemic, these in-person interactions have become challenging. To reduce the risk of transmission, healthcare providers have adapted to new methods of providing care through telemedicine.[52] People with chronic diseases and who have mental health issues often feel more secure knowing that their primary care physician is available via teleservice. Therefore, it is recommended that primary care physicians make use of this facility to consult with a mental health specialist via telemedicine and digital mode.
Nonetheless, this study has some limitations. Our data was generated by participants’ subjective reports of their experiences and emotions and subjected to response bias. The self-reporting of depression, anxiety, or stress symptoms is not equivalent to a structured diagnostic interview[53] and cannot be used to classify a mental health disorder as a depressive disorder. Besides, the present study does not provide any qualitative information regarding preventive measures and coping strategies for people with chronic diseases, which are warranted in future studies.
Despite these limitations, this study provides novel information regarding the psychological states of Bangladeshi people with chronic diseases in the context of COVID-19. This is among the first few studies in Bangladesh’s context on the mental health impacts of the COVID-19 pandemic among people with chronic diseases. This study included people with chronic diseases from all divisions across Bangladesh, and the recruitment methods captured the diverse backgrounds of the study participants. The findings of this study might be helpful for concerned authorities to plan and adopt appropriate interventions to ensure sound mental health for people with chronic diseases in the context of COVID-19.
Conclusion
This study explores the psychological symptoms among people with chronic diseases during the COVID-19 pandemic. The results of this study could be valuable in detecting mental health problems and identifying individuals with chronic disease conditions who are at a higher risk and may benefit from interventions. Further, due to the insufficient mental health resources available in the country and the restricted community access during the COVID-19 pandemic, it has become necessary for family and primary care physicians to manage psychological issues along with physical illnesses. Further, primary care physicians may take appropriate measures to combat mental health issues among people with chronic diseases, possibly by reaching out via telemedicine sessions. Therefore, it is imperative for primary care physicians to possess sufficient knowledge and skill in addressing frequent mental health concerns that arise in the context of infectious disease outbreaks, such as COVID-19. Additionally, a longitudinal study is necessary to investigate the relationships between mental health issues and COVID-19-related factors in more detail, and the findings could be used to enhance the health of individuals with chronic diseases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We sincerely thank the participants who participated in this research.
References
- 1.Kapasia N, Paul P, Roy A, Saha J, Zaveri A, Mallick R, et al. Impact of lockdown on learning status of undergraduate and postgraduate students during COVID-19 pandemic in West Bengal, India. Child Youth Serv Rev. 2020;116:105194. doi: 10.1016/j.childyouth.2020.105194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Temsah MH, Al-Sohime F, Alamro N, Al-Eyadhy A, Al-Hasan K, Jamal A, et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J Infect Public Health. 2020;13:877–82. doi: 10.1016/j.jiph.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldometer Coronavirus Update (Live) 2021. [[Last accessed on 8 Sep 2021]]. Available from: https://www.worldometers.info/coronavirus/?utm_campaign=homeAdUOA?Si .
- 4.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–6. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 5.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–8. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int J Infect Dis. 2020;94:91–5. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hasan N, Bao Y. Impact of “e-Learning crack-up” perception on psychological distress among college students during COVID-19 pandemic: A mediating role of “fear of academic year loss”. Child Youth Serv Rev. 2020;118:105355. doi: 10.1016/j.childyouth.2020.105355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pellino G, Spinelli A. How coronavirus disease 2019 outbreak is impacting colorectal cancer patients in Italy: A long shadow beyond infection. Dis Colon Rectum. 2020;63:720–2. doi: 10.1097/DCR.0000000000001685. [DOI] [PubMed] [Google Scholar]
- 9.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown?A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–6. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tran BX, Vu GT, Latkin CA, Pham HQ, Phan HT, Le HT, et al. Characterize health and economic vulnerabilities of workers to control the emergence of COVID-19 in an industrial zone in Vietnam. Saf Sci. 2020;129:104811. doi: 10.1016/j.ssci.2020.104811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu Z, Lin X, Chiwanda Kaminga A, Xu H. Impact of the COVID-19 epidemic on lifestyle behaviors and their association with subjective well-being among the general population in mainland China: Cross-sectional study. J Med Internet Res. 2020;22:e21176. doi: 10.2196/21176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rozario SS, Masho SW. The associations between mental health status, hypertension, and hospital inpatient visits in women in the United States. Am J Hypertens. 2018;31:804–10. doi: 10.1093/ajh/hpy065. [DOI] [PubMed] [Google Scholar]
- 16.Mukeshimana M, Chironda G. Depression and associated factors among the patients with type 2 diabetes in Rwanda. Ethiop J Health Sci. 2019;29:709–18. doi: 10.4314/ejhs.v29i6.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rahman M, Rahman MA, Flora MS, Rakibuz-Zaman M. Depression and associated factors in diabetic patients attending an urban hospital of Bangladesh. Int J Collab Res Intern Med Public Health. 2011;3:65–76. [Google Scholar]
- 18.Roy T, Lloyd CE, Parvin M, Mohiuddin KG, Rahman M. Prevalence of co-morbid depression in out-patients with type 2 diabetes mellitus in Bangladesh. BMC Psychiatry. 2012;12:123. doi: 10.1186/1471-244X-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Islam SM, Rawal LB, Niessen LW. Prevalence of depression and its associated factors in patients with type 2 diabetes: A cross-sectional study in Dhaka, Bangladesh. Asian J Psychiatr. 2015;17:36–41. doi: 10.1016/j.ajp.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 20.Shah P. Psychological well-being: A challenge in Covid-19 regime. The Financial Express. [[Last accessed on 16 Mar 2021]]. Available from: https://thefinancialexpress.com.bd/views/psychological-well-being-a-challenge-in-covid-19-regime-1586186005 .
- 21.Victor GS, Ahmed S. The importance of culture in managing mental health response to pandemics. In: Huremovic D, editor. Psychiatry of Pandemics. New York: Springer; 2019. pp. 55–64. [Google Scholar]
- 22.Haque MMA, Jahan Y, Khair Z, Moriyama M, Rahman MM, Sarker MHR, et al. Perceptions about telemedicine among populations with chronic diseases amid COVID-19: Data from a cross-sectional survey. Int J Environ Res Public Health. 2022;19:4250. doi: 10.3390/ijerph19074250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peltzer K, Pengpid S. Anxiety and depressive features in chronic disease patients in Cambodia, Myanmar and Vietnam. S Afr J Psychiatr. 2016;22:940. doi: 10.4102/sajpsychiatry.v22i1.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J Eval Clin Pract. 2011;17:268–74. doi: 10.1111/j.1365-2753.2010.01434.x. [DOI] [PubMed] [Google Scholar]
- 25.Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–8. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–65. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alim SAHM, Kibria SME, Uddin MZ, Nessa M, Wahab MA. Translation of DASS 21 into Bangla and validation among medical students. Bang J Psychiatry. 2014;28:67–70. [Google Scholar]
- 29.Tann SS, Yabiku ST, Okamoto SK, Yanow J. TRIADD: The risk for alcohol abuse, depression, and diabetes multimorbidity in the American Indian and Alaska Native populations. Am Indian Alsk Native Ment Health Res. 2007;14:1–23. doi: 10.5820/aian.1401.2007.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Khuwaja AK, Lalani S, Dhanani R, Azam IS, Rafique G, White F. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol Metab Syndr. 2010;2:72. doi: 10.1186/1758-5996-2-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tovilla-Zárate C, Juárez-Rojop I, Peralta Jimenez Y, Jiménez MA, Vázquez S, Bermúdez-Ocaña D, et al. Prevalence of anxiety and depression among outpatients with type 2 diabetes in the Mexican population. PLoS One. 2012;7:e36887. doi: 10.1371/journal.pone.0036887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kaur G, Tee GH, Ariaratnam S, Krishnapillai AS, China K. Depression, anxiety and stress symptoms among diabetics in Malaysia: A cross sectional study in an urban primary care setting. BMC Fam Pract. 2013;14:69. doi: 10.1186/1471-2296-14-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dehghan A, Memarian R. Abundance of stress, anxiety and depression in multiple sclerosis patients. Alborz Univ Med J. 2013;2:82–8. [Google Scholar]
- 34.Dong XC, Li JM, Bai JY, Liu ZQ, Zhou PH, Gao L, et al. [Epidemiological characteristics of confirmed COVID-19 cases in Tianjin. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:638–41. doi: 10.3760/cma.j.cn112338-20200221-00146. [DOI] [PubMed] [Google Scholar]
- 35.Khan N, Rahman M, Mitra D, Afsana K. Prevalence of multimorbidity among Bangladeshi adult population: A nationwide cross-sectional study. BMJ Open. 2019;9:e030886. doi: 10.1136/bmjopen-2019-030886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jahan Y, Rahman MM, Faruque ASG, Chisti MJ, Kazawa K, Matsuyama R, et al. Awareness development and usage of mobile health technology among individuals with hypertension in a rural community of Bangladesh: Randomized controlled trial. J Med Internet Res. 2020;22:e19137. doi: 10.2196/19137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Seo J, Choi B, Kim S, Lee H, Oh D. The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: Results of a 2009 Korean community health survey of 156,747 participants. BMC Public Health. 2017;17:844. doi: 10.1186/s12889-017-4798-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC) Older Adults at greater risk of requiring hospitalization or dying if diagnosed with COVID-19. [[Last accessed on 16 Jan 2021]]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html .
- 39.Alsaadi T, El Hammasi K, Shahrour TM, Shakra M, Turkawi L, Mudhafar A, et al. Prevalence of depression and anxiety among patients with multiple sclerosis attending the MS clinic at Sheikh Khalifa Medical City, UAE: Cross-sectional study. Mult Scler Int 2015. 2015:487159. doi: 10.1155/2015/487159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liang L, Ren H, Cao R, Hu Y, Qin Z, Li C, et al. The effect of COVID-19 on youth mental health. Psychiatr Q. 2020;91:841–52. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bansal SB, Dixit S, Shivram G, Pandey D, Saroshe S. A study to compare various aspects of members of joint and nuclear family. J Evol Med Dent Sci. 2014;1:641–8. [Google Scholar]
- 42.Munda SK, Soreng S. Attitude towards joint family: A comparative study. International Journal of Research in all Subjects in Multi Languages. 2019;7:43–5. [Google Scholar]
- 43.Tiwari GK, Tiwari RP, Pandey R, Ray B, Dwivedi A, Sharma DN, et al. The life outcomes of children during COVID-19: Exploring the protective roles of the joint and nuclear families in India. Authorea. 2020 [Google Scholar]
- 44.Ali M, Ahsan GU, Khan R, Khan HR, Hossain A. Immediate impact of stay-at-home orders to control COVID-19 transmission on mental well-being in Bangladeshi adults: Patterns, explanations, and future directions. BMC Res Notes. 2020;13:494. doi: 10.1186/s13104-020-05345-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu M, Xu W, Yao Y, Zhang L, Guo L, Fan J, et al. Mental health status of students'parents during COVID-19 pandemic and its influence factors. Gen Psychiatr. 2020;33:e100250. doi: 10.1136/gpsych-2020-100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lewis G, Bebbington P, Brugha T, Farrell M, Gill B, Jenkins R, et al. Socio-economic status, standard of living, and neurotic disorder. Int Rev Psychiatry. 2003;15:91–6. doi: 10.1080/0954026021000045994. [DOI] [PubMed] [Google Scholar]
- 47.Hodgkinson S, Godoy L, Beers LS, Lewin A. Improving mental health access for low-income children and families in the primary care setting. Pediatrics. 2017;139:e20151175. doi: 10.1542/peds.2015-1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hailemichael Y, Hanlon C, Tirfessa K, Docrat S, Alem A, Medhin G, et al. Mental health problems and socioeconomic disadvantage: A controlled household study in rural Ethiopia. Int J Equity Health. 2019;18:121. doi: 10.1186/s12939-019-1020-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74:281–2. doi: 10.1111/pcn.12988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. 2020;51:102076. doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, et al. Impact of COVID-19 on routine care for chronic diseases: A global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14:965–7. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shear K, Frank E, Houck PR, Reynolds CF., 3rd Treatment of complicated grief: A randomized controlled trial. JAMA. 2005;293:2601–8. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Levis B, Yan XW, He C, Sun Y, Benedetti A, Thombs BD. Comparison of depression prevalence estimates in meta-analyses based on screening tools and rating scales versus diagnostic interviews: A meta-research review. BMC Med. 2019;17:65. doi: 10.1186/s12916-019-1297-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


