Abstract
Background and Objective
Staffing shortages and health inequities are persistent barriers in the Philippines toward achieving universal health care. To ensure an adequate and responsive health workforce, there is a need to evaluate the Human Resources for Health (HRH) status across health facilities, particularly those in underserved communities. Hence, this study aims to determine the staffing requirements and workload pressure among primary care facilities in selected geographically isolated and disadvantaged areas (GIDAs) in the Philippines.
Methods
The study utilized the workload indicators of staffing need (WISN) methodology from the World Health Organization to determine the staffing and workload situation among three health worker cadres (physicians, nurses, and midwives) in the study sites. Particularly, six primary care facilities (four rural health units and two community hospitals) located in Surigao del Norte were involved in the study. WISN-related data (health service statistics, available working time, and health professionals’ workload components) were collected through records review, focus group discussions, and key informant interviews. The WISN software was used to analyze the staffing levels and workload pressure in the selected facilities.
Results
A total of 40 health workers, including physicians (n = 5, 13%), nurses (n = 21, 52%), and midwives (n = 14, 35%) participated in the study. The findings noted varying levels of staffing and workload pressures among the three cadres in selected primary care facilities, which were influenced by several factors. Particularly, health facilities with additional human resources obtained from deployment programs indicated adequate staffing and low to normal workload pressures. However, further analysis revealed potential HRH maldistribution and reliance on the temporary nature of the staff augmentation program in delivering primary care services, which need to be addressed to optimize health workforce planning. Service workload may also have been impacted by the temporary closure of health facilities due to disasters. Among the few cadres that reported staffing shortage and high workload pressure, these were due to higher service demands, increased task delegation, and inadequate service coordination. Hence, context-specific challenges and situational factors in GIDAs need to be considered when determining the staffing and workload requirements.
Conclusion
There is a need to improve the capacities of health facilities and local government units (LGUs) to engage in evidence-based HRH planning through the WISN methodology. Doing so could improve staffing and workload distribution among health care facilities in the country. Moreover, interorganizational collaboration (DOH, LGUs, and health facilities) should be strengthened to improve delineation and prevent duplication/omission of health services, rationalize HRH distribution and augmentation, and streamline the priority health services based on the local contextual factors.
Keywords: geographically isolated and disadvantaged areas, health workforce planning, human resources for health, primary health care, workload indicators of staffing need
INTRODUCTION
To attain universal health coverage (UHC), all people should have access to the right number of health workers with the right skills in the right place and time. Hence, adequate levels and equitable allocation of Human Resources for Health (HRH) are vital for an effective and responsive health system.1 As the world moves forward to achieve UHC in the post-pandemic era, the World Health Organization (WHO) recommends the reorientation of health systems through the primary care approach.2 However, several countries, including the Philippines, have persistently faced HRH shortages and maldistribution. For instance, less than 25% of the country’s municipalities/cities have met the WHO standards on population-based HRH levels, with more than 50% of health worker cadres (i.e., physicians, nurses, midwives) residing in Metro Manila and other Luzon regions.3
There is a need for evidence-based health workforce planning across all levels of service delivery, particularly in primary care. This would ensure that adequate HRH can be mobilized to address the changing health needs and to deliver quality services to various communities. However, the traditional method of population-to-staff ratios, which has been employed by most healthcare facilities to determine HRH requirements, does not take into consideration the local or complex variations in service demands and other activities performed by health workers.4 Thus, the WHO recommends the use of data-driven tools to better guide HRH planning and decision-making.
Studies conducted so far were carried out to help strengthen HRH adequacy and distribution for delivering primary care services in the country. First, the Skills Mix project (Phase 1) was conducted by Dones et al.5 involving cities/municipalities from 13 areas/island groups. The qualitative study aimed to identify factors influencing the required number of health workers in urban and rural communities. Their findings showed that determining the optimal health workforce in primary care facilities requires an understanding of various socioeconomic, geographic, political, and other contextual nuances in the communities; and that the existing health worker-to-population ratios are not appropriate for all settings. Then, the HRH2030 Philippines Project6 was conducted across nine regions, which aimed to establish the staffing requirements for primary care facilities in the country. This was the first project to adopt the WHO Workload Indicators of Staffing Need (WISN) methodology, an evidence-based management tool for determining the required number of health workers per cadre in a particular facility, as well as the current level of workload pressure among its personnel.7 Its results enabled the Department of Health (DOH) to provide recommendations on the minimum/ maximum staffing requirements for primary care facilities in the country.8 Particularly, they suggested having 1 to 2 physicians, 2 to 4 nurses, and 2 to 4 midwives in each rural health unit (RHU). Additionally, barangay health stations (BHS) were encouraged to have 1 to 2 midwives and 2 to 3 nurses.
Since the WISN methodology was introduced in the Philippines in 2019, there were no follow-up studies conducted thereafter to further utilize this tool in improving HRH distribution in the country. Moreover, the qualitative findings of the Skills Mix project (Phase 1)5 need to be triangulated by quantitative methods to ensure that staffing requirements can be comprehensively determined across primary care facilities. The results of the HRH2030 Philippines Project6 need to be validated as well, given the difference in the local healthcare situation during the pre-pandemic period. Notably, the sudden increase in health service demands during the COVID-19 pandemic has exposed the country’s perennial problems of HRH shortage and maldistribution. The pandemic has also accelerated the resignation and migration of Filipino health workers from the local health system.9 As the country navigates through the post-pandemic period, there is a need to review the staffing levels across health facilities in the country so that appropriate HRH support can be provided, especially in the country’s underserved or marginalized communities. Assessing the adequacy of the health workforce in the primary care facilities of geographically isolated and disadvantaged areas (GIDAs) is crucial, as these communities experience physical and socioeconomic limitations in accessing health services.10 Given these contexts, it is also necessary to establish if the DOH staffing recommendations8 are met or applicable in primary care facilities serving GIDAs.
This study is part of the first project to reassess the staffing and workload pressures among health workers in primary care facilities in the Philippines, after the Skills Mix (Phase 1) in 2017 and HRH2030 Philippines project in 2019. Particularly, the study focuses on the cadres of physicians, nurses, and midwives working in GIDAs. Consequently, the results could contribute relevant knowledge for improving HRH management in primary care settings, which is a vital component in achieving UHC.
MATERIALS AND METHODS
Research Design
This research is part of a project commissioned by the DOH to determine the required skill mix for delivering health services among the healthcare provider networks (HCPNs) of selected regions in the Philippines. Specifically, this study aimed to assess the staffing and workload pressures of three health worker cadres (physicians, nurses, and midwives) across primary care facilities in GIDAs. We used a mixed methods case study design, gathering quantitative and qualitative information to comprehensively analyze relevant data from the different health facilities.11 The WISN methodology was adopted to determine the staffing/workload situation through quantitative variables (i.e., available working time, health service statistics, and workload components performed by the health workers). Moreover, participants were encouraged to describe their staffing and workload situation, including possible factors and local circumstances influencing these aspects.
Setting and Participants
This study reports the WISN findings in Surigao del Norte, one of the Universal Health Care Integration Sites (UHC-IS) in the country.12 The province was chosen since it was included in the Skills Mix Phase 1 project,5 and comprises several types of geographically isolated and disadvantaged areas, such as island barangays, indigenous people-populated communities, armed conflict areas, and disaster-prone sites. More specifically, one city and municipality from Surigao del Norte mainland and one municipality from Siargao Island were included in this study. In total, six primary care facilities were involved: four rural health units (RHUs) and two community hospitals.
Physicians, nurses, and midwives were the target cadres in this study, being the groups that commonly reported staffing concerns in the Skills Mix Phase 1 project.5 The research team utilized purposive sampling to recruit participants from each cadre, including health workers with plantilla (regular/ permanent) positions (e.g., municipal health officers, public health nurses, rural health midwives), as well as employees hired through the DOH HRH Deployment Program (e.g., nurses, midwives). Currently, this deployment program is only implemented among 4th to 6th class municipalities and GIDAs, such as those in Surigao del Norte. The DOH-deployed workers were on duty four times per week in their assigned barangay health stations (BHSs) and once per week in the RHU, sharing the community health service workload with the nurses and midwives.
Data Collection
Data collection was conducted from July to August 2023. Prior to study commencement, ethical approval was obtained from the DOH Single Joint Research Ethics Board (Ref. No.: SJREB-2023-44). Endorsement from the DOH Center for Health Department-Caraga was also sought to facilitate correspondence with the study sites. Despite the involvement of official instances, participation in the study was purely voluntary. The project team contacted each facility via e-mail and phone to set potential schedules for in-person data collection. The team also provided the invited participants with information sheets further discussing relevant study information and addressing related questions. After securing their informed consent, data collection was facilitated at the study site.
Following the WISN methodology, records review, key informant interviews (KIIs), and focus group discussions (FGDs) were utilized to gather relevant data for determining the staffing level and workload pressure in each facility. First, a task inventory checklist based on the HRH2030 Philippines project6 was utilized to gather data on the workload components (health service, support, and additional activities) of each cadre, in line with the set professional standards (Appendices 1-3). These data were gathered through KIIs and FGDs with each cadre in every facility. Moreover, participants were encouraged to describe the facility staffing, difficulties/challenges in carrying out health-related or administrative activities, and factors in the locality that affected their workload. Two research team members facilitated the KIIs/FGDs, and the sessions were audio-recorded with the participants’ permission.
The records review obtained information related to the personnel’s available working time and the facilities’ annual service statistics in 2022, as the WISN methodology utilizes data from the previous year (one calendar year is required) to calculate the optimal staffing levels in a healthcare institution.7 Table 1 summarizes the definition of the WISN variables and the related data gathered in the study.
Table 1.
WISN variables and related data gathered
| WISN Variable | Definition | Data gathered |
|---|---|---|
| Available working time | No. of hours available for a health worker to report for duty in a year, taking into account all types of absences |
|
| Workload components | Work activities that take up the health workers’ daily activity time. These are classified as health service, support, and additional activities. | |
| Health service activities | Activities done by all members of the staff category for which annual statistics are collected | Refer to Appendices 1-3
|
| Support activities | Activities done by all members of the cadre for which annual statistics are not collected | Refer to Appendices 1-3
|
| Additional activities | Activities done only by certain (not all) members of the cadre for which annual statistics are not collected | Refer to Appendices 1-3
|
| Workload statistics | Annual service statistics of the healthcare facility, which represent the accomplished health-related activities of the workers |
|
| Activity standards | The time needed for a skilled, well-trained, and motivated worker to perform an activity based on professional standards in the local context |
|
Challenges/Limitations in Data Collection
The team encountered some challenges and limitations in data collection. For instance, a major challenge was the incomplete or untallied raw data in the health service records. Due to the effects of Typhoon Odette (International name: Rai) in the latter part of 2021, some local facilities were damaged and had to undergo repairs before becoming operational again in 2022. This calamity led to the three-month closure of some health facilities, which might have significantly contributed to the reduction in the recorded service statistics, and in turn may have affected the WISN computation of their staffing/workload pressure. While the participating staff mentioned that they continued conducting community health visits during such time, there were no recorded numbers of the patients they cared for or the services they delivered, which also decreased their service statistics. Moreover, other facilities did not have up-to-date records of some health services they provided (e.g., number of internal referrals, wound suturing/care, administered/dispensed medications). Leaves availed of by each cadre were also not aggregated and instead kept on their individual monthly time records in most facilities. These situations led to manual searching and counting of logbook records in various areas (RHU, city health office, local HR departments, provincial DOH office) and further interviews with the participants to estimate and validate the relevant data as much as possible.
There were some participants who were scheduled for data collection were not able to join due to several circumstances (i.e., training, meetings with other offices, unavailability in another schedule, and poor internet connection hindering participation in a potential online interview). Nevertheless, we ensured that each cadre was represented in every facility so that the gathered information were triangulated.
Data Analysis
Descriptive statistics, including frequency and percentage, were used to summarize the health worker profiles. The gathered data (available working time, workload components, activity standards, service statistics) were first encoded into a spreadsheet for cross-checking and validation by the team members, and then entered into the WISN software13 to generate per-facility and per-cadre reports in web archive transformation (.wat) files. The audio-recorded interviews were also transcribed and analyzed via content analysis to provide additional context on the staffing and workload situation of the health workers in the selected facilities. Since the purpose of this process was to identify the staffing and work distribution of the cadres, it did not aim to interpret the meaning of their experiences which is typical for qualitative research.
The WISN software provides two values: difference and ratio.13 The WISN difference is obtained by subtracting the current number of staff in each cadre from the required number based on WISN calculations. Results could indicate balance (0), surplus (+1 or above), or shortage (-1 or below) in staffing. Meanwhile, the WISN ratio shows the degree of workload pressure experienced by each cadre in providing services to their constituents. This is calculated by dividing the current number of staff from the required number of staff, and the results could denote very high (0.10 to 0.49), high (0.50 to 0.89), normal (0.90 to 1.19), low (1.20 to 1.59), very low (1.60 to 1.80) and extremely low (1.81 and up) workload pressures among health workers.
RESULTS
Profile of Healthcare Facilities and Cadres
Table 2 describes the profile of the primary care facilities, including the number of existing health workers and the characteristics of the population they serve. All RHUs have birthing clinics for providing maternal and newborn care to their constituents. However, these facilities were closed for about three months (January to March 2022) as they were being renovated in the aftermath of Typhoon Odette. All RHUs also received workforce augmentation through the DOH HRH Deployment Program, wherein nurses and midwives were assigned to specific barangays to implement health promotion, risk reduction, and treatment-related activities. Two community hospitals (CH-1 and CH-2) were located nearby two RHUs (RHU-3 and RHU-4). One hospital (CH-1) was licensed as an infirmary, but the other one (CH-2) was only authorized to operate as a polyclinic. Hence, the latter was limited to offering outpatient services, but attempted to extend its services by providing basic management of medical, surgical, and pediatric conditions, and temporary (< 24 hours) patient admission.
Table 2.
Profile of Primary Care Facilities and Health Worker Cadres
| Facility | No. of hired health workers | Study participants | Characteristics | |
|---|---|---|---|---|
| RHU-1 | Physician = 1 |
|
||
| Municipal Health Officer | 1 | 1 | ||
| Nurses = 17 | ||||
| Public Health Nurse | 1 | 1 | ||
| Casual/Job order | 7 | 1 | ||
| HRH Deployed | 9 | 3 | ||
| Midwives = 9 | ||||
| Rural Health Midwife | 8 | 3 | ||
| HRH Deployed | 1 | - | ||
| RHU-2 | Physician = 1 |
|
||
| Municipal Health Officer | 1 | 1 | ||
| Nurses = 16 | ||||
| Public Health Nurse | 1 | 1 | ||
| Casual/Job order | 1 | - | ||
| HRH Deployed | 14 | 2 | ||
| Midwives = 11 | ||||
| Rural Health Midwife | 7 | 3 | ||
| Casual/Job order | 3 | - | ||
| HRH Deployed | 1 | - | ||
| RHU-3 | Physician = 1 |
|
||
| Municipal Health Officer | 1 | 1 | ||
| Nurses = 17 | ||||
| Public Health Nurse | 1 | 1 | ||
| HRH Deployed | 16 | 2 | ||
| Midwives = 6 | ||||
| Rural Health Midwife | 5 | 3 | ||
| Casual/Job order | 1 | - | ||
| RHU-4 | Physician = 1 |
|
||
| Doctors-to-the-Barrios (DTTB) deployed | 1 | - | ||
| Nurses = 8 | ||||
| Public Health Nurse | 1 | - | ||
| HRH Deployed | 7 | 4 | ||
| Midwives = 5 | ||||
| Rural Health Midwife | 4 | 3 | ||
| HRH Deployed | 1 | 1 | ||
| CH-1 | Physicians = 2 |
|
||
| OIC-Chief of Hospital | 1 | 1 | ||
| Casual/Job order | 1 | - | ||
| Nurses = 6 | ||||
| Permanent | 1 | 1 | ||
| Casual/Job order | 5 | 2 | ||
| Midwives = 2 | ||||
| Permanent | 1 | 1 | ||
| Casual/Job order | 1 | - | ||
| CH-2 | Physicians = 2 |
|
||
| OIC-Chief of Hospital | 1 | - | ||
| Casual/Job order | 1 | 1 | ||
| Nurses = 6 | ||||
| Permanent | 1 | 1 | ||
| Casual/Job order | 5 | 2 | ||
| Participant summary (N = 40) | Frequency | Percentage (%) | ||
| Physicians (n = 5, 13%) | ||||
| LGU-hired (regular) | 4 | 80.0 | ||
| Casual/job order | 1 | 20.0 | ||
| Nurses (n = 21, 52%) | ||||
| Regular/LGU-hired | 5 | 24.0 | ||
| Casual/Job order | 5 | 24.0 | ||
| HRH/DOH-hired | 11 | 52.0 | ||
| Midwives (n = 14, 35%) | ||||
| Regular/LGU-hired | 13 | 93.0 | ||
| HRH/DOH-hired | 1 | 7.0 | ||
A total of 40 health workers, including physicians (n = 5, 13%), nurses (n = 21, 52%), and midwives (n = 14, 35%) participated in the study. More specifically, one physician was assigned to each RHU, functioning as the Municipal Health Officer (MHO) and clinic physician at the same time. However, the physician in RHU-4 (a newly assigned Doctors-to-the-Barrios employee) was not present during data collection due to training and was unable to join in an online interview because of internet connectivity limitations. In each of the two community hospitals, two physicians were assigned, one as a permanent employee and the other hired on a contractual basis. Meanwhile, the nurse participants from RHUs and community hospitals included those holding plantilla positions (24%), casual/job orders (24%), and DOH-deployed (52%). Majority of the participant midwives held regular positions in the LGU (93%), while one community hospital did not have midwives in its plantilla.
Healthcare facilities generally followed the prescribed 40-hour weekly or 160-hour monthly work reporting. In the RHUs, this was usually arranged as eight hours, five days per week. Meanwhile, hospitals reported having a 12-hour per shift arrangement to cover the staff duties for 24 hours. Table 3 shows the sample computation of the AWT for the physician (1,816 hours), nurses (1,832 hours), and midwives (1,760 hours).
Table 3.
Sample Computation of Available Working Time (AWT) of Physicians, Nurses, and Midwives in a Rural Health Unit
| Cadre | Working days per week | Working hours per day | Annual leave | Public holidays | Sick leave | Special no notice leave | Training days | AWT in weeks | AWT in days | AWT in hours |
|---|---|---|---|---|---|---|---|---|---|---|
| Physicians | 5 | 8 | 9 | 20 | 0 | 0 | 4 | 45.4 | 227 | 1,816 |
| Nurses | 5 | 8 | 5 | 20 | 2 | 1 | 3 | 45.8 | 229 | 1,832 |
| Midwives | 5 | 8 | 5 | 20 | 2 | 1 | 11 | 44.2 | 221 | 1,768 |
Staffing Requirements
Table 4 shows the summary of the computed optimal number of staff per facility. Results of the WISN difference indicated the presence of balance, shortage, or surplus among the existing workforce in the selected facilities. Meanwhile, Figure 1 illustrates the percentage breakdown of staffing levels across the three cadres. Three RHUs (50%) were adequately staffed having one physician per facility. Meanwhile, one RHU (RHU-1) and two community hospitals (CH-1 and CH-2) needed one more physician to provide quality health services to their constituents.
Table 4.
WISN Results on the Status of Staffing and Workload Pressure among Selected Primary Care Facilities
| Facility | Cadre | Existing staff | Calculated staff | WISN Difference | Staffing level | WISN Ratio | Workload pressure |
|---|---|---|---|---|---|---|---|
| RHU-1 | Physician | 1 | 2 | -0.38 | Shortage | 0.72 | High |
| Nurse | 17 | 12 | 4.53 | Surplus | 1.36 | Low | |
| Midwife | 9 | 11 | -1.59 | Shortage | 0.85 | High | |
| RHU-2 | Physician | 1 | 1 | 0.43 | Balance | 1.75 | Very low |
| Nurse | 16 | 19 | -3.08 | Shortage | 0.84 | High | |
| Midwife | 11 | 9 | 2.45 | Surplus | 1.29 | Low | |
| RHU-3 | Physician | 1 | 1 | 0 | Balance | 1.00 | Normal |
| Nurse | 17 | 12 | 4.71 | Surplus | 1.38 | Low | |
| Midwife | 6 | 4 | 1.95 | Surplus | 1.48 | Low | |
| RHU-4 | Physician | 1 | 1 | -0.06 | Balance | 0.94 | Normal |
| Nurse | 8 | 6 | 1.84 | Surplus | 1.30 | Low | |
| Midwife | 5 | 4 | 0.72 | Surplus | 1.17 | Normal | |
| CH-1 | Physician | 2 | 3 | -0.24 | Shortage | 0.89 | High |
| Nurse | 6 | 6 | 0.14 | Balance | 1.02 | Normal | |
| Midwife | 2 | 1 | 1.83 | Surplus | 11.76 | Extremely low | |
| CH-2 | Physician | 2 | 3 | -0.23 | Shortage | 0.90 | Normal |
| Nurse | 4 | 2 | 1.96 | Surplus | 1.96 | Extremely low |
Figure 1.
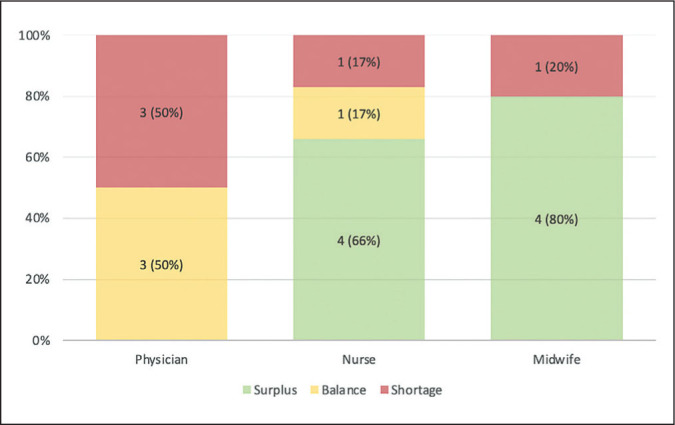
Staffing levels among health workers in primary care facilities
The presence of DOH-deployed nurses in the RHUs significantly augmented the number of staff available to provide primary care to the residents. Hence, three RHUs showed a surplus in the total number of nursing staff. In contrast, one facility that covers a larger population (RHU-2), indicated a shortage in the number of available nurses. Nevertheless, it was noted that there was only one public health nurse (PHN) assigned per RHU and the rest were either designated to the birthing clinic (casual/job order) or deployed in individual barangays (DOH-hired). Meanwhile, one community hospital (CH-1) had a balance in their nursing workforce, while the other one (CH-2) revealed a surplus in their staff.
Four out of five facilities (80%) showed a surplus in the existing number of midwives. The exception is RHU-1, which was noted to have a shortage of midwifery staff due to a higher workload in maternal and child health services (MCH) in the communities.
Workload Pressure
The WISN ratio indicated the degree of workload pressures among primary care workers, ranging from extremely low, very low, low, normal, and high. Table 4 also shows the WISN ratio in the six facilities, with Figure 2 displaying the percentage breakdown across the three cadres. Physicians in four facilities had very low to normal workload pressures (67%); however, those working in two facilities with staff shortages (RHU-1 and CH-1) exhibited high workload pressures (33%). For nurses, extremely low to normal workload pressures were obtained in five facilities (83%), especially those with DOH-deployed staff; except for one facility with higher service demands (RHU-2), which indicated high workload pressures (17%). Lastly, midwives in four health facilities had workload pressures ranging from extremely low to normal (80%); although one facility (RHU-1) with higher MCH service demands recorded high workload pressure among its midwives (20%).
Figure 2.
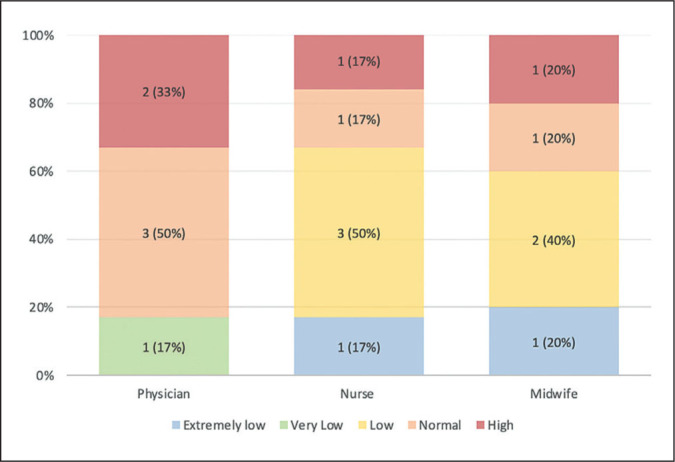
Workload pressure among health workers in primary care facilities.
Qualitative findings from the interviews with primary care workers
The KIIs and FGDs revealed relevant information about the health facilities’ local context and staffing arrangements for providing primary care services. Particularly, health worker-related factors that the healthcare provision in the study settings included: task-delegation/shifting, task-sharing, expansion of scope of practice, and temporary staff augmentation. Meanwhile, facility or community-related factors that impact staffing/workload involved: facility closures (due to disasters), financial and resource limitations, service delivery challenges in GIDAs, and data monitoring problems. These findings are presented per cadre to describe the specific staffing and workload situation across health worker levels.
Physicians
RHU physicians mainly carried out clinic consultations and patient admission/discharge in the birthing clinics. However, the three-month closure of some RHU facilities led to the referral of most medical and MCH services to the City Health Office. Instead, some physicians facilitated barangay visits to deliver primary care services to their constituents, but such activities were not properly documented/tallied. Some physicians were also assigned to facilitate LGU-sponsored medical missions and outreach programs throughout the whole year. In one facility (RHU-2), the MHO was often pulled out to fulfill clinical duties at the City Health Office, as the latter’s clinic physicians were often scheduled for training, medical missions, and administrative functions. This reduced the MHO’s availability to provide services to the communities covered by the RHU. Some physicians also prepared standing orders for managing common illnesses in the RHU and admitting patients in the birthing clinics, which enabled nurses and midwives to deliver care when doctors were unavailable or engaged in other tasks (e.g., trainings or meetings). Through their RHU online group chat, physicians were also able to advise the staff on the health interventions they could provide. However, there were also some instances wherein medical procedures like suturing skin lacerations were delegated to nurses with previous experience doing the procedure. Moreover, tasks related to report writing and program supervision were usually delegated to the PHNs with physicians only being consulted for approval.
In community hospitals, one physician was on duty for 15 straight days covering 24 hours of shift. They also reported having a relatively higher number of patient consultations whenever the physician in the nearby RHU was unavailable or if there was an increased number of cases requiring prolonged observation or admission, such as diarrhea with dehydration, dengue fever, and respiratory conditions in exacerbation. Nevertheless, the bulk of their clinical duties were during office hours (8 AM to 5 PM), which included facilitating outpatient consultations, admission, ward rounds, and discharge. Aside from these, they would be on-call for emergencies and other pertinent referrals while in the hospital. Notably, there were instances, wherein nurses and midwives in the afternoon/night shift were allowed to carry out medical procedures (e.g., order laboratory examinations, administer commonly available medications, suture skin lacerations) in which case they would refer them to the physician later.
Nurses
There was only one public health nurse assigned to each RHU. Hence, some PHNs reported struggling to perform both clinical and administrative tasks. In one facility (RHU-2), the PHN spent much of the time synthesizing and writing reports for all barangays, which could take one to two days to complete. This is in addition to them assuming other roles (e.g., assisting midwives in the birthing clinics when there is understaffing, dispensing medications, managing the RHU when the physician is unavailable). Hence, most of them reported having to work even on weekends to finish their outputs. To somewhat reduce the PHN burden, the DOH-deployed nurses rotationally report to the RHU once per week. In another facility (RHU-3), the PHN was not assigned to the clinical operations, but rather handled the RHU mental health programs [e.g., adolescent, mental health gap action program (mhGAP), community-based drug rehabilitation], in an attempt to maximize the availability of DOH-deployed nurses. Most PHNs noted that when the DOH deployment program ceases, it will be overwhelmingly difficult to deliver health services to the whole community, especially in the far-flung barangays.
The DOH-deployed nurses contributed to the implementation of standard DOH services in their assigned areas (one nurse per BHS or one nurse per two BHSs with smaller communities), in addition to providing mass health education, attending barangay council meetings, and community organizing. In 2022, most of their workload was allotted to COVID-19 mass vaccinations, performing various approaches (e.g., house-to-house, mobile clinics, and fixed posts) to provide primary and booster immunizations to the eligible population. They were also assisted by barangay health workers (BHWs) in their respective communities, who obtained vital signs, anthropometric measurements, patient interviews, and household profiling/monitoring. BHWs were also trained by the nurses to improve their competencies in delivering community health services. However, the deployed nurses reported some challenges in their workload, such as traveling to distant or unpaved areas (via boat or motorcycle), which reduces the time for healthcare services when moving from one location to another; staying in the island communities for four straight days, which extended their duty beyond eight hours per day as people continuously sought them; frequent retraining of BHWs, as they were often replaced by the LGU; referring patients in the RHU despite limitations in the mobile/internet signal in their areas; and providing health education to individuals/groups with low health literacy.
Nurses in one community hospital (CH-1) reported having expanded roles, performing other activities such as suturing lacerations (substituting for physicians) and facilitating labor and deliveries (instead of midwives). Two nurses were assigned per shift, who were responsible for managing the ward, outpatient department, emergency room, and delivery room at the same time. In addition to administrative and clinical roles, the nurse supervisor also assumed the duties of pollution control officer and health emergency management staff of the hospital. By contrast, the other community hospital (CH-2) reported having a light workload, because of the low demand for health services in their area. The facility also had limited resources; hence, residents preferred to go directly to the largest hospital on the island for health services. Despite being licensed as a polyclinic, the nurses still covered a 24-hour shift to provide care to common and emergency cases, since the referral hospital is 45 minutes away from the municipality.
Midwives
Midwives were mainly responsible for implementing MCH services in the community, including prenatal/ postnatal care, normal deliveries, child immunization, and all forms of family planning. They manned the birthing clinics, which also served as the sites for the provision of MCH services. Due to the three-month closure of the birthing facilities, midwives had a relatively lower workload in the first quarter of 2022. Nonetheless, they delivered the health services through community visits, which were not regularly accounted for. There were also other health service activities that they performed, which were not reflected in the prescribed workload components (Appendix 3), such as contributing to the implementation of the National Tuberculosis Program (i.e., dispensing antitubercular medications, patient education, follow-up, and monitoring), which according to them, took a significant amount of time of their work.
While they were also responsible for facilitating the services in the BHSs, the deployment of DOH-hired nurses to each barangay enabled them to share and shift their tasks to this cadre. In one RHU (RHU-3), rehabilitation programs for malnourished children were also delegated to barangay nutrition scholars or rural sanitary inspectors. Nevertheless, midwives were still responsible for monitoring, tallying, and writing reports of the healthcare activities for the barangays, which they reported to have taken most of their time. Notably, one birthing clinic (RHU-4) in Siargao Island did not have a license to operate (LTO) from the DOH due to some unmet requirements. Hence, they mostly transferred deliveries to the main referral hospital on the island, although they catered to patients having imminent deliveries. The community hospital (CH-2) that was only licensed as a polyclinic did not have midwives, as they cannot deliver services related to labor and delivery. Meanwhile, in one community hospital (CH-1), midwives assisted in delivering MCH services, although they were also assigned to the ward, functioning as nurse assistants to augment the health workforce.
Among the three cadres, midwives generally had the longest tenure in health facilities. However, as experienced health service providers, there were some instances when they performed the roles of other cadres, including the administration of intravenous medications and prescription of medications for various illnesses. Meanwhile, one of their reported challenges is the increasing age of the staff, making it difficult at times to arrange schedules for night shifts in the birthing clinics, which sometimes affected the nurses who would need to assume their clinical duties.
DISCUSSION
The study revealed various levels of staffing and workload pressures among selected primary care facilities of GIDAs in Surigao del Norte. Notably, situational and community factors influenced the health service delivery among these facilities, which need to be considered when interpreting the study findings. In particular, half of the facilities had an adequate number of physicians, with corresponding very low to normal workload pressures. Owing to higher service demands, acute medical cases, and larger populations being catered to, the other half of the facilities had medical staff shortages and high workload pressures. In most RHUs with DOH-deployed workers, the pool of nursing and midwifery staff had surpluses and workload pressures ranged from extremely low to normal. However, closure of some health facilities, inadequate service records, and resource/legal limitations in providing health services have also impacted such quantitative findings. Moreover, due to larger patient volumes and increased task-shifting toward nurses and midwives, a few facilities had their staff showing high workload pressures. These findings show the potential utility of the WISN methodology, together with the identification of contextual determinants of staffing and workload, in guiding HRH distribution and service delivery among primary care facilities in GIDAs or communities with comparable characteristics to the study setting.
The findings indicated that there was only one physician in each RHU, which was found to be adequate for three (out of four) RHUs. However, the increased population in one facility also led to higher patient consultations, which made up most of the working time of the physician. Hence, the DOH recommendation of having a maximum of two physicians in the RHU8 is warranted in this situation. The addition of a rural health physician could enable the MHO to function as a public health manager and facilitate the supervision of the DOH and local health programs. While hiring additional HRH may not be immediately possible due to resource limitations in most LGUs,14 appropriate workload distribution should be done between RHU physicians and nurses to ensure that the delegation of managerial roles toward nurses is only conducted when it is necessary, as the latter is also fulfilling their own clinical and supervisory tasks. In contrast, the nearby community hospitals experienced shortages in their number of physicians. Despite being in close proximity to RHUs, physicians in community hospitals managed increased patient volumes when their counterparts in the RHU were unavailable or when there were surges in communicable diseases requiring hospitalization. This implies the need to strengthen the implementation of health promotion and disease prevention programs in the RHUs. Better delineation and coordination of services offered by the two facilities should also be done so that outpatient consultations for endemic conditions could be managed by the RHU, as this could reduce the service workload of physicians in the community hospitals.
The WISN results indicated surpluses in nursing staff in most primary care facilities because of the DOH-deployed workers, but further analysis revealed that there was only one regular PHN in each RHU. Hence, these nurses reported being overworked as they tried to balance their health service and support/additional activities. While the current staffing is considered inadequate compared with the DOH recommendations (2 to 4 nurses per RHU; 2 to 3 nurses per BHS),8 the RHUs came up with compensatory scheme by requesting the deployed DOH staff to report to their facility once per week and assist the PHN in clinic activities. Notably, the surpluses should not imply that the number of DOH-deployed nurses in GIDAs be reduced; rather, the nuances in their workload should be considered when determining staffing. These include challenges in accessing islands and mountainous areas, moving around to visit distant households when performing door-to-door activities, organizing the community to act on health-related issues, and providing frontline access to health services beyond their working hours.14 Moreover, the current findings call for improved collaboration between the DOH and LGUs in tailoring the activities that would maximize the presence of deployed staff in barangays and decrease the patient burden in the main RHUs. Through focused consultations between the two agencies, the local needs of the population served can be better understood, and the staffing arrangements for deployed personnel can be rationalized.
Based on the 2022 WISN data, midwives in primary care facilities seemed overstaffed and had extremely low to normal workload pressures. However, several factors should be taken into account. First, most birthing clinics in Surigao were destroyed by Typhoon Odette, which led to their closure/repair for several months and reduced service workload. Moreover, the community health visits they conducted during such time were not properly documented. Second, one RHU admitted to having no license to operate as a birthing clinic, which led to referral of most deliveries to the hospital instead. Despite its temporary closure, one RHU still had an increased demand for MCH services, with WISN results showing midwifery staff shortage and high workload pressure. These findings imply that the actual service workload of midwives in the selected facilities could be potentially higher than the computed numbers, if they were able to operate on a fuller scale. After the COVID-19 pandemic and the re-opening of the birthing clinics in some RHUs, midwives reported an increasing surge of patients back to the RHU in 2023. Hence, WISN assessment should be revisited every one to two years to consider contextual factors affecting the appropriateness of current staffing levels in each facility.15 Another possible reason for the current results is that midwives were assigned to work with DOH-deployed nurses in implementing health programs in the barangays, which led to task-sharing in some services, such as immunization, pre/postnatal care, and family planning. Without the augmentation from the DOH, midwives would be assigned to manage up to three BHSs, on top of their duties in the birthing facilities. This is an important consideration in staffing decisions pertaining to this cadre, as DOH-deployed personnel are only temporarily assigned in LGUs,16 and will transfer an immense workload burden to midwives and nurses once they leave.
The DOH should sustain the HRH deployment program in GIDAs, as the findings showed that task-sharing of DOH-hired workers reduced the service workload among the LGU-hired staff and promoted better healthcare access to the community residents. However, the current program has only remained a stopgap measure for HRH recruitment and retention, as employees are never assured of being rehired after one year of service. Existing policies should be reviewed to provide better security of tenure for these workers, together with possible reassignment to other areas with higher service demands.16 The WISN methodology, by providing data on staffing requirements and workload pressures, could be used to guide such HRH distribution. The DOH is in the best position to lead initiatives and build coalitions with several agencies to reinforce the competencies of nurses and midwives, particularly those deployed in disadvantaged communities. Strengthening the capabilities of these cadres to deliver quality health services in the continuum of health promotion, disease prevention, treatment, and rehabilitation would maximize the presence of deployed health workers in the community, and eventually reduce the service workload in main RHUs, community hospitals, and higher-level facilities.17
Close collaboration among RHUs, community hospitals, and LGU administration in GIDAs is also crucial to promote delineation and prevent duplication/omission in health service delivery. This could facilitate improved distribution of HRH among facilities managed by the same LGUs and maximize their share of the health service workload. For instance, a staffing-related challenge noted by the midwives, especially the older staff, is the need to cover the 24/7 shift in the birthing clinics. Thus, despite the low service demands in some instances, they were required to report for duty. A possible recommendation to address this is for each facility to regularly monitor/track the pregnant women in their community, so that appropriate arrangements can be made to operate on an on-call or as-needed basis.18 For instance, midwives may cover the birthing clinic operations for 16 hours, and the remaining eight hours in the night shift can be on-call. Moreover, community hospitals also have their night shifts, which are manned by nurses/midwives who can also render MCH services to patients. By having flexible staff scheduling, more midwives might be available to share the workload of the lone RHU nurse during the day, when most health services are delivered. Meanwhile, clear referral guidelines should also be developed between primary care facilities serving the same areas, so that services that can be delivered in the RHU do not need to be referred to the community hospital.8 This could also help in reducing the high workload pressure of physicians in primary hospitals, as shown in the study results. Moreover, LGUs could utilize the WISN methodology among their health facilities to facilitate the reassignment or temporary borrowing of health workers toward facilities with greater service demands,19 leading to better staff and workload distribution.
The importance of continuous support from the LGU in the delivery of primary care services cannot be overemphasized. For instance, the findings showed that one community hospital (CH-2) was only licensed as a polyclinic due to resource constraints. This led to its inability to admit patients, attend to deliveries, and provide a higher level of care than the nearby RHU, resulting in referrals to bigger hospitals that tend to be easily congested. Nurses in this facility were also noted to have extremely low workload pressure because of limited health resources, despite covering the 24/7 shift. Unfortunately, the financial capacity of LGUs in GIDAs is limited due to their lower Internal Revenue Allotment (IRA).6 A recent development in the country’s UHC initiatives is the creation of the Special Health Fund (SHF) through subsidies from the national government, PhilHealth payments, and other financial donations to aid LGUs in improving health service delivery.20 The SHF could be utilized to remunerate additional health workers until the LGUs have incrementally created plantilla positions based on existing standards. Currently, further proposals are being made to improve the SHF guidelines/oversight to ensure good governance in its creation and implementation. Hence, LGUs, in collaboration with the UHC coordinating council, should ensure the appropriate and transparent facilitation of SHF-related processes in addressing the health needs of their constituents.
The findings also indicated that significant task-shifting occurred across cadres, especially from physicians to nurses and midwives, to deliver primary care services. However, this also entailed that nurses and midwives performed some activities that were beyond their professional scope and training. Consistent with the findings of the HRH2030 Philippines project,8 these findings suggest the need to revise the scope of practice of health worker cadres. This could improve the delivery of basic healthcare services, especially in GIDAs and underserved communities, and could contribute to the realization of UHC in the country. Nevertheless, revising the scope of practice of healthcare professionals is a long-term goal that warrants legislative and political support. For instance, the proposed amendment or repealing of the Philippine Nursing Act suggests the provision of resources to train advanced practice nurses (APNs) who would have expanded and collaborative roles in providing health services to patients, including in the absence/ unavailability of physicians. Recent reviews highlighted the positive impact of APNs in primary care, being associated with reduced healthcare costs, increased client satisfaction, lower hospitalization rates, and comparable patient outcomes with medical practitioner-led care.21,22 Review and revision of the scope of midwifery practice in the country is also vital, as midwives are the frontline implementers of DOH programs in the community. Midwives are expected to carry out multifaceted tasks in primary care, but there is insufficient capability development to enhance their program management skills.23
Another vital human resource that can be maximized to augment the primary health workforce in GIDAs is the barangay health workers. Notably, the Philippines is one of the first countries to implement the BHW program, following the recommendations of the Alma Ata Declaration in 1978.24 The application of health-related knowledge/skills and integration with community members by experienced BHWs are essential competencies that could greatly reduce the service workload of professional health workers. However, political decisions in LGUs could influence the high turnover among BHWs, leading to reorientation/training sessions by nurses/midwives that reduce their available time allotted for health service activities. Despite their valuable contribution to primary care, BHWs are considered volunteers, receive below-minimum-wage honoraria, and have no security of tenure. Currently, there are proposed legislations to establish a registry of qualified and trained BHWs and raise their status to that of government employees (House Bill No. 6481, Senate Bill No. 68), which could strengthen the involvement of BHWs in delivering primary care services. The DOH25 and Technical Skills Development Authority (TESDA)26 have also formulated training manuals for BHWs, highlighting their roles as educators, community organizers, and health service providers. These materials can be utilized by LGUs to facilitate the preparation and certification of BHWs in providing frontline health access at the grassroots level and improving the workload distribution in primary health facilities.
Notably, the results implied the potential application of WISN in improving health workforce planning, particularly among primary care facilities in the country. However, based on the team’s experience in conducting the study, there is a need to improve the recording system of health facilities and align them with the standard workloads set by the DOH and its expert working groups.6 Such configurations should be incorporated into the health information systems, especially in the UHC integration sites. This is to ensure an accurate assessment of the service delivery by the health facilities, which would enable an updated measurement of their staffing and workload gaps. To widen the utilization of the WISN methodology across the country, it is important for the DOH to conduct more trainings across the country through the regional CHDs. Currently, the DOH has an introductory WISN course27 in its eLearning platform; however, more information is needed to appropriately guide stakeholders on how to conduct a per-facility WISN assessment to address their staffing needs. As the country has entered the post-pandemic period, our local health systems need to be empowered to ensure that they are able to meet the health demands of the population through an adequately distributed HRH. Ultimately, evidence-based decisions on staffing and workload distribution can benefit both health workers and patients, as the country continuously aims to achieve universal health coverage.
Study Limitations
The study has some limitations in terms of sample size owing to funding constraints and the number of healthcare facilities in the study locale, which might limit its generalizability. Nonetheless, the study sites were chosen as they share most characteristics of rural communities and GIDAs in the country, such as islands, far-flung areas, conflict-affected sites, disaster-prone settings, and populations of economically marginalized and indigenous communities.
As previously mentioned, a significant challenge encountered during data retrieval was the untallied or incomplete service records in some facilities, which could have influenced the computed WISN difference and ratio. Notably, the study gathered qualitative information to triangulate the results, as numerical data might not be sufficient to fully capture the staffing and workload situation in health facilities. As with studies involving qualitative data collection, the potential for recall bias among the participants cannot be totally ruled out. To minimize this, researchers employed probing techniques and participant checking. Apart from addressing the data monitoring/recording problems in healthcare facilities in the country, future WISN studies should cover more facilities and participants. This will increase the representativeness of various communities in the archipelago and will reinforce the external validity of the findings to other healthcare settings.
CONCLUSION
This study evaluated the staffing and workload pressures among health workers in primary care facilities in the Philippines, particularly those catering to GIDAs and rural communities in the province of Surigao del Norte. Despite the WISN results showing that the majority of the primary care facilities had adequate staffing levels and low to normal workload pressures among three cadres (physicians, nurses, and midwives), understanding the community and situational factors influencing these results is crucial to ensure responsive HRH planning and distribution. Contextual analysis showed that the HRH deployment program of the DOH contributed to the reduction of workload burden in some facilities, although HRH maldistribution and reliance on the program’s temporary nature needed to be addressed. Situational limitations, such as temporary closures, recordkeeping problems, and health service delivery restrictions among primary care facilities should also be considered when interpreting the current findings. These should guide future studies in the country utilizing the WISN methodology to determine staffing levels across healthcare facilities. Notably, inadequate service coordination among health units, higher service demands from the community, and increased task shifting across cadres contributed to some health workers indicating staff shortage and workload burden. Apart from understanding the health needs of the population, several context-specific challenges in service delivery should also be considered when determining the staffing and workload requirements in GIDAs.
Continuous and wide-scale implementation of the WISN methodology could contribute to providing evidence-based HRH decisions to improve staffing and workload distribution across health facilities and workers in the country. Lastly, sustained collaboration among the DOH, LGUs, and health facilities is also imperative to rationalize HRH distribution and augmentation, improve delineation and prevent duplication/omission of health services, and streamline the priority health services based on the local contextual factors.
Acknowledgments
This study is under the project entitled “Determining the Required Skill Mix to Deliver Primary Health Care Services: Phase 2 (Validation),” which was commissioned by the Department of Health and the Philippine Council for Health Research and Development, under the Advancing Health through Evidence-Assisted Decisions with Health Policy and Systems Research (AHEAD-HPSR) Program 2022. The project team extends its gratitude to Asst. Prof. Julienne Ivan Soberano and Asst. Prof. Ryan de Torres who assisted the study team in gathering relevant data from the participants. Lastly, we thank all the participating primary care facilities and health workers in Surigao del Norte.
APPENDICES
Appendix 1. Workload components and activity standards for physicians in primary care facilities
| Workload Group 1: Health service activities | Activity standards (based on HRH2030) |
| Consultations | 18 minutes/ patient |
| Minor Surgical Procedures | 30 minutes/ patient |
| Ward Rounds | 10 minutes/ in-patient |
| Family Planning | 30 minutes/ patient |
| Referral | 9 minutes/ patient |
| Admission | 2 minutes/ patient |
| Discharge | 8 minutes/ patient |
| Peri-mortem care | 41 minutes/ patient |
| Workload Group 2: Support activities | Activity standards |
| Health education | 30 minutes/ week |
| Departmental meetings | 2 hours/ month |
| Continuing professional development | 8 days/ year |
| Outreach programs (medical missions) | 8 hours/ month |
| Endorsement meetings | 1 hour/ day |
| Issuance of documents and medicolegal management | 8 hours/ month |
| Workload Group 3: Support activities | Activity standards |
| Staff supervision | 30 minutes/day |
| Trainee supervision | 2 hours/week |
| Administrative functions | 1 hour/week |
| Interpretation and action on surveillance | 2 hours/week |
| Barangay visits | 8 hours/week |
Appendix 2. Workload components and activity standards for nurses in primary care facilities
| Workload Group 1: Health service activities | Activity standards (based on HRH2030) |
| Patient assessment | 13 minutes/patient |
| Nursing diagnosis and management | 34 minutes/patient |
| Minor surgical procedures | 37 minutes/patient |
| Wound care | 29 minutes/patient |
| Assistance in normal spontaneous delivery | 44 minutes/patient |
| Administration of medication | 20 minutes/patient |
| Immunization | 12 minutes/patient |
| External referral with escort | 132 minutes/patient |
| Internal referral | 12 minutes/patient |
| Admission of patients | 24 minutes/patient |
| Inpatient nursing care | 34 minutes/patient |
| Ward rounds | 18 minutes/ in-patient |
| Discharge of patients | 14 minutes/patient |
| Post-mortem care | 20 minutes/patient |
| Workload Group 2: Support activities | Activity standards |
| Health education | 30 minutes/day |
| Reporting patient census | 30 minutes/day |
| Community outreach programs | 8 hours/month |
| Group counselling | 30 minutes/week |
| Documentation | 34 minutes/ day |
| Home visits | 8 hours/week |
| Attendance to trainings/seminars | 2 hours/ month |
| Attendance to meetings | 34 minutes/ day |
| Workload Group 3: Support activities | Activity standards |
| Surveillance | 1 hour/month |
| Assist in municipal health planning | 3 hours/ month |
| Supervision and monitoring of staff | 1 hour/day |
| Staff scheduling | 1 hour/week |
| Mentoring of students | 1 hour/week |
| Management meetings | 2 hours/month |
| Supervisor’s monthly reports | 1 hour/month |
| Performance evaluation | 2 hours/year |
| Nursing audit | 2 hours/month |
| Committee work | 3 hours/month |
Appendix 3. Workload components and activity standards for midwives in primary care facilities
| Workload Group 1: Health service activities | Activity standards (based on HRH2030) |
| Prenatal care | 35 minutes/patient |
| Postpartum care | 35 minutes/patient |
| Family planning: male condoms | 10 minutes/ patient |
| Family planning: injectables | 23 minutes/ patient |
| Family planning: intrauterine device | 53 minutes/ patient |
| Family planning: natural | 33 minutes/patient |
| Family planning: implants | 35 minutes/ patient |
| Family planning: pills | 15 minutes/ patient |
| Normal spontaneous delivery | 99 minutes/patient |
| Newborn care | 35 minutes/patient |
| Labor management | 168 minutes/patient |
| Child care/well-baby clinic | 18 minutes/patient |
| Integrated Management of Childhood Illness (IMCI) | 22 minutes/patient |
| Visual inspection with acetic acid | 25 minutes/patient |
| Pap Smear | 20 minutes/patient |
| Rehabilitation of malnourished children | 20 minutes/patient |
| Referral | 19 minutes/patient |
| Immunization | 15 minutes/patient |
| Workload Group 2: Support activities | Activity standards |
| Health education | 30 minutes/day |
| Home visits | 8 hours/month |
| Staff meetings | 2 hours/month |
| Continuous professional development | 2 hours/month |
| Medical missions | 8 hours/month |
| Housekeeping (5S Practice) | 40 minutes/day |
| Mentoring of students | 2 hours/week |
| Workload Group 3: Support activities | Activity standards |
| Supervision | 1 hour/day |
| Management meetings | 1 hour/month |
| Report writing | 2 hours/month |
| Mass circumcision | 8 hours/year |
Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
All authors declared no conflicts of interest.
REFERENCES
- 1.Witter S, Hamza MM, Alazemi N, Alluhidan M, Alghaith T, Herbst CH. Human resources for health interventions in high- and middle-income countries: findings of an evidence review. Hum Resour Health. 2020. Jun 8;18(1):43. doi: 10.1186/s12960-020-00484-w. PMID: 32513184; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Universal health coverage [Internet]. 2023. [cited 2023 Apr]. Available from: https://www.who.int/news-room/fact-sheets/detail/universal-health-coverage-(uhc)
- 3.Abrigo MRM, Ortiz DAP. Who are the health workers and where are they? Revealed preferences in location decision among health care professionals in the Philippines. Philipp Inst Dev Stud [Internet]. 2019. [cited 2023 Apr]; 6–17. Available from: https://pidswebs.pids.gov.ph/CDN/PUBLICATIONS/pidsdps1932.pdf
- 4.Kunjumen T, Okech M, Diallo K, Mcquide P, Zapata T, Campbell J. Global experiences in health workforce policy, planning and management using the Workload Indicators of Staffing Need (WISN) method, and way forward. Hum Resour Health. 2022. Jan 28;19 (Suppl 1):152. doi: 10.1186/s12960-021-00695-9. PMID: 35090485; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dones LBP, Abad PJB, Medina V, Cordero A. Determining the required skill mix to deliver primary health care services across various rural and urban communities. 2017. Unpublished report.
- 6.Department of Health-Philippines, United States Aid for International Development . Determining staffing levels for primary care services using workload indicators of staffing need in selected regions of the Philippines [Internet]. 2019. [cited 2023 Apr]. Available from: https://hrh2030program.org/wp-content/uploads/2020/08/2.1_HRH2030PH_WISN-SDN-Phase-1-Report.pdf
- 7.World Health Organization . Workload Indicators of Staffing Need (WISN) User Manual [Internet]. 2010. [cited 2023 Apr]. Available from: https://www.who.int/publications/i/item/9789241500197
- 8.Aytona MG, Politico MR, McManus L, Ronquillo K, Okech M. Determining staffing standards for primary care services using workload indicators of staffing needs in the Philippines. Hum Resour Health. 2022. Jan 28;19(Suppl 1):129. doi: 10.1186/s12960-021-00670-4. PMID: 35090487; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alibudbud R. When the “heroes” “don’t feel cared for”: The migration and resignation of Philippine nurses amidst the COVID-19 pandemic. J Glob Health. 2022. May 23;2:03011. doi: 10.7189/jogh.12.03011. PMID: 35604059; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Department of Health-Philippines . Guidelines on identifying geographically isolated and disadvantaged areas and strengthening their health systems. [Internet]. 2020. [cited 2023 Apr]. Available from: https://law.upd.edu.ph/wp-content/uploads/2020/06/DOH-AO-No-2020-0023.pdf
- 11.Creswell J, Plano Clark V. Designing and conducting mixed methods research, 3rd ed. Thousand Oaks: Sage; 2018. p.116. [Google Scholar]
- 12.Department of Health-Philippines . Official list of Universal Health Care Integration Sites (UHC IS) as of 30 September 2020 [Internet]. 2020. [cited 2023 Apr]. Available from: https://www.nnc.gov.ph/phocadownloadpap/userupload/Ro5-webpub/DOH%20Department%20Memo%20No.%202020-041458site%20%20SHF.pdf
- 13.World Health Organization . Workload indicators of staffing need (WISN) software manual [Internet]. 2014. [cited 2023 Apr]. Available from: https://iris.who.int/bitstream/handle/10665/44414/9789241500197_users_eng.pdf
- 14.Tejero LMS, Leyva EWA, Abad PJB, Montorio D, Santos ML. Production, recruitment, and retention of health workers in rural areas in the Philippines. Acta Med Philipp. 2022. May;56(8):31–42. doi: 10.47895/amp.vi0.1510.[ [DOI] [Google Scholar]
- 15.Stankovic S, Santric Milicevic M. Use of the WISN method to assess the health workforce requirements for the high-volume clinical biochemical laboratories. Hum Resour Health. 2022. Jan 28;19(Suppl 1):143. doi: 10.1186/s12960-021-00686-w. PMID: 35090473; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abrigo MRM, Opiniano GA, Tam ZC. Process evaluation of the Department of Health Human Resources for Health deployment program. Philipp Inst Dev Stud [Internet]. 2021. [cited 2023 Aug]; 5–42. Available from: https://pidswebs.pids.gov.ph/CDN/PUBLICATIONS/pidsdps2107.pdf [Google Scholar]
- 17.World Health Organization . Strengthening nursing and midwifery: investments in education, jobs, leadership and service delivery. [Internet]. 2021. [cited 2023 Aug]. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA74/A74_ACONF3-en.pdf
- 18.Department of Health-Philippines . Additional clarification on the requirement of a license to operate (LTO) a birthing facility pursuant to Administrative Order No. 2012-0012 known as “Rules and regulations governing the new classification of hospitals and other health facilities in the Philippines” [Internet]. 2015. [cited] 2023 Sep]. Available from: https://hfsrb.doh.gov.ph/wp-content/uploads/2021/05/11122015-2015-0392.pdf
- 19.Nguyen TTH, Phung HT, Bui ATM. Applying the workload indicators of staffing needs method in nursing health workforce planning: evidences from four hospitals in Vietnam. Hum Resour Health. 2022. Jan 28;19(Suppl 1):124. doi: 10.1186/s12960-021-00668-y. PMID: 35090478; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Health, Department of Budget and Management, Department of Finance, Department of Interior and Local Government, PhilHealth Insurance Corporation . Joint Memorandum Circular 2021-0001: Guidelines on the allocation, utilization, and monitoring of, and accountability for the special health fund [Internet]. 2021. [cited 2023 Nov]. Available from: https://www.dbm.gov.ph/wp-content/uploads/Issuances/2021/Joint-Memorandum-Circular/JMC-2021-0001_Guidelines-on-SHF.pdf
- 21.Htay M, Whitehead D. The effectiveness of the role of advanced nurse practitioners compared to physician-led or usual care: a systematic review. Int J Nurs Stud Adv. 2021. Nov;3:100034. doi: 10.1016/j.ijnsa.2021.100034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McMenamin A, Turi E, Schlak A, Poghosyan L. A systematic review of outcomes related to nurse practitioner-delivered primary care for multiple chronic conditions. Med Care Res Rev. 2023. Dec;80(6): 563–81. doi: 10.1177/10775587231186720. PMID: 37438917; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Canila CC, Hipolito JH. Assessing the state of professional practice of midwifery in the Philippines. Phil J Health Res Dev. 2018;22(2):1–11. [Google Scholar]
- 24.Mallari E, Lasco G, Sayman DJ, Amit AML, Balabanova D, McKee M, et al. Connecting communities to primary care: a qualitative study on the roles, motivations and lived experiences of community health workers in the Philippines. BMC Health Serv Res. 2020. Sep 11;20(1):860. doi: 10.1186/s12913-020-05699-0. PMID: 32917203; PMCID: . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Department of Health-Philippines . Barangay health workers’ reference manual [Internet]. 2022. [cited 2023 Aug]. Available from: https://tciurbanhealth.org/courses/philippines-toolkit-demand-generation/lessons/engaging-barangay-health-workers/topic/bhw-reference-manual/
- 26.Technical Education and Skills Development Authority-Philippines . Barangay health services NC II [Internet]. 2019. [cited 2023 Aug]. Available from: https://tesda.gov.ph/Downloadables/Barangay%20Health%20Services%20NC%20II.pdf
- 27.Department of Health-Philippines . WISN for planning: an introduction to WISN [Internet]. 2023. [cited 2023 Apr]. Available from: https://learn.doh.gov.ph/


