Diseases of the pleural space are common. In this review we discuss the pathophysiology, diagnosis, and treatment of pneumothorax, pleural effusion, and empyema.
Summary points
After a second spontaneous pneumothorax there is a 40% chance of recurrence; video assisted thoracoscopic bullectomy and pleurodesis is the treatment of choice
Needle decompression (second interspace, mid-clavicular line) is the best treatment for suspected tension pneumothorax
Ultrasonography is helpful in cases of pleural effusion
A chest drain should be inserted in cases of exudative (protein content greater than 3 g/l) pleural effusion that recur after aspiration, or in parapneumonic effusions when the pH is less than 7.2 or the glucose concentration is less than 3.33 mmol/l
A chest drain should be inserted for early empyema
Late presenting empyema should be treated by decortication if the patient is fit, but patients who are unfit for major surgery should receive thrombolytic instillation or thoracostomy
Methods
We searched Medline (1966 to 1999), standard textbooks of thoracic surgery, and life support manuals for articles that answered questions that in our experience non-specialists commonly ask of specialists in the diagnosis and management of pneumothorax, pleural effusion, and empyema.
The pleural space
The pleura is a thin serous layer, which covers the lungs (visceral pleura) and is reflected, by way of the lung hila, on to the chest wall and pericardium (parietal pleura). The pleural space thus created extends from the root of the neck, 3 cm above the mid-point of the clavicle, down behind the abdominal cavity, in the costodiaphragmatic recess, to the 12th rib overlying the kidney.1 Only a thin layer of pleural fluid separates the parietal and visceral pleura. The parietal layer secretes 2400 ml of fluid daily, which is resorbed by the visceral layer.2 Maintenance of negative intrapleural pressure is necessary for respiration.
Pneumothorax
Pneumothorax describes air within the pleural cavity. Pneumothorax may be spontaneous, secondary to an underlying disease such as emphysema or asthma, traumatic, or iatrogenic. “Spontaneous” pneumothoraces usually arise from rupture of small subpleural blebs.3 After the first spontaneous pneumothorax there is a 10% chance of recurrence,4 and after a second pneumothorax this increases to 40%.5
Clinical presentation
Patients with pneumothorax present with pleuritic pain or breathlessness, or both, which can be life threatening especially if the pneumothorax is under tension. On examination, expansion and breath sounds are reduced and the percussion note is hyperresonant. Tracheal shift away from the affected side indicates tension. Plain chest radiography shows lung collapse and air in the pleural space. There may be concomitant haemothorax caused by bleeding from adhesions between visceral and parietal pleura, which tear when the lung deflates.6
Management
Tension pneumothorax should be immediately decompressed by needle thoracocentesis through the second interspace in the mid-clavicular line.7 It is dangerous to await confirmation by radiography if tension is suspected.
A first pneumothorax without dyspnoea in a patient without chronic lung disease can be managed by observation. The presence of dyspnoea or underlying lung disease requires needle aspiration of the air.8 Patients with associated haemothorax, with recently decompressed tension pneumothoraces, on ventilators, or who have had unsuccessful conservative treatment should all be treated by chest drainage.8
Inserting chest drains
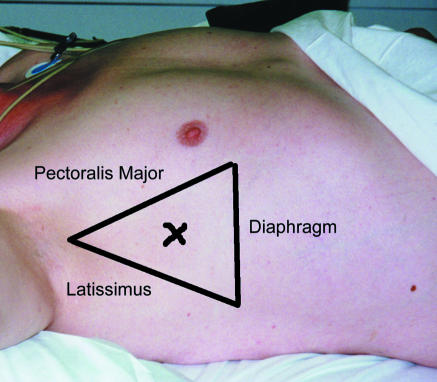
The insertion of chest drains has been discussed in many texts,7,9,10 but the importance of the insertion site and the blunt dissection and non-trocar technique merit emphasis. Insertion should be within the “triangle of safety” through the fifth interspace (fig 1). This is level with the nipple in a man, and the root of the breast in a woman. Insertion through lower spaces carries the risk of entering the abdomen. Insertion with sharp instruments carries a serious risk of injuring intrathoracic or abdominal viscera.
Figure 1.
“Triangle of safety”: X shows preferred site for drain insertion
Management of chest drains
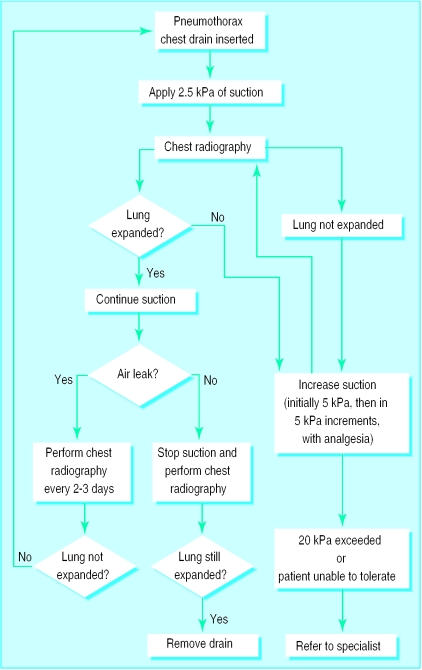
If management of chest drains is optimal, 87%-91% of spontaneous pneumothoraces can be managed without surgery.11,12 Upon insertion the drain should be connected to a one-way valve system. An underwater seal is most commonly used, but the Heimlich valve is useful outside the hospital or during transport. An underwater seal will swing with respiration. It is common practice to apply 2.5 to 5 kPa of suction to the outlet from the underwater seal bottle. This is only essential if the lung does not re-expand immediately or if there is an incompletely drained haemopneumothorax. In the presence of a noticeable air leak it is important to ensure that any suction apparatus can remove the volume of air leaked. If not it will prevent resolution of the pneumothorax and may place it under tension. Similarly, a drain with an air leak should never be clamped. The underwater seal may not swing when suction is used, but the difference between the height of the water in the bottle and the tube indicates the negative pressure being applied to the pleural cavity. Figure 2 shows the subsequent management of a chest drain.
Figure 2.
Management of intercostal drain in pneumothorax
Patients with a previous pneumothorax (on either side), emphysema, or who do not settle after one or two weeks of effective conservative management should be referred to a specialist centre.12 Pleurodesis through the chest drain using talc, tetracycline, or autologous blood may seal the leak.6,13,14
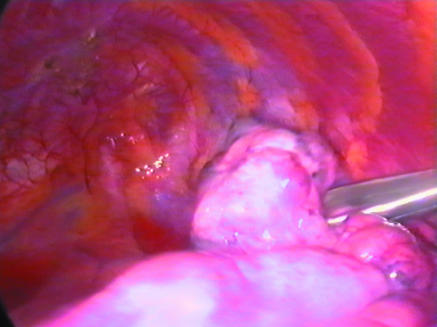
Patients who are fit are best treated by video assisted thoracoscopic surgery (fig 3), with sealing of the air leak and pleurectomy to prevent recurrence.15,16 This is effective in 93% of patients, with most treatment failures evident within 30 days.17 In patients who are unfit for surgery and who have persistent air leaks the underwater seal may be changed to a flutter bag allowing them to be mobilised and discharged.18
Figure 3.
Apical bulla seen during video assisted bullectomy and pleurodesis for pneumothorax
Pleural effusion
Pleural effusion describes fluid (transudative or exudative) within the pleural space. Transudates(protein concentration less than 3.0 g/dl) are secondary to underlying disease, such as heart failure, or medical disorders leading to hypoalbuminaemia (for example, cirrhosis, nephrotic syndrome, protein losing enteropathy). Usually there is evidence of the primary diagnosis. Exudates (protein concentration greater than 3.0 g/dl) are usually caused by infection (bacterial or mycobacterial), malignancy, collagen vascular disease, pancreatitis, or pulmonary embolism.19
Clinical presentation
Pleural effusions may be asymptomatic but if large produce breathlessness or pain, or both. Breath sounds are reduced on the affected side, and the percussion note is stony dull. Chest x ray film shows blunting of the lateral costophrenic angle if more than 200-500 ml of fluid is present. As the volume of fluid increases, the hemidiaphragm becomes obscured. The upper margin of the opacity tends to be concave—that is, higher laterally.
Differentiating consolidation of the lung from pleural effusion on x ray film may be difficult. The presence of air bronchograms indicates a consolidated lung. Pleural effusions, however, can be confirmed by ultrasonography or by noting the shift of fluid on lateral decubitus films. Ultrasonography is the method of choice as a drainage site can be marked (or the fluid drained) by the radiologist.20 It is important to note the presence of any other intrapulmonary masses, hilar lymphadenopathy, or pleural plaques, although these may not be visible until after the effusion has been drained.
Investigation and management
Having established radiologically that fluid is present, a sample must be obtained for biochemical, microbiological, and cytological analysis. If the patient is free of symptoms, a sample can be obtained with a 21 gauge needle and a 20 ml syringe. The patient is positioned sitting up and leaning forwards over a bed table. Under conditions of strict asepsis the effusion is tapped posteriorly in the mid-scapular line one interspace below the upper limit of the dullness to percussion but above the diaphragmatic reflection of the pleura.
If the patient has symptoms, the fluid should be drained off. The technique is similar to needle sampling but a 14 gauge intravenous cannula is used. The stylet is removed and the cannula connected to a closed pleural aspiration kit. All fluid is aspirated and sent for analysis. If more than 1.5 litres of fluid is obtained, fluid shifts can result in haemodynamic instability or pulmonary oedema. This is, however, rare in clinical practice.
Pleural fluid should be analysed for protein and glucose concentration, pH, bacteria—including acid fast bacilli—and cell content (three samples). If the fluid appears chylous, more specialised analysis is required.21 About 80% of the time, cytology (three samples) identifies a malignant effusion22; false positives are rare.23
Closed needle biopsy of the pleura is best performed early in the investigation of a pleural exudate, at the time of drainage of the effusion.24 This identifies 75% of cases of tuberculosis.25 The technique is also useful if malignancy is suspected,26 and, combined with cytology, 90% of cases will be diagnosed.27 If mesothelioma is suspected video assisted thoracoscopic surgery may be a more useful technique.28
If the effusion is a transudate secondary to systemic disease such as heart failure or nephrotic syndrome, it will not resolve until the disease is treated. It may be necessary to tap the effusion periodically to relieve symptoms; prolonged chest drainage results in significant protein and fluid losses.
Indications for insertion of chest drain
Patients with exudates not secondary to an underlying systemic disease that recur after aspiration, or parapneumonic effusions with a pH of less than 7.2 and a glucose concentration of less than 3.33 mmol/l, require an intercostal drain.29 The same technique and site is used as for pneumothorax.
Management of drain
Low suction (2.5-5 kPa) may be useful in the management of these drains, but unlike a pneumothorax it can be interrupted to allow mobilisation. The drain should remain in place until less than 100 ml of fluid is being drained per day. At this point the drain can be removed if the underlying cause has been treated. There is no need to clamp the drain. If, however, there is an underlying malignancy that has not been treated (or is untreatable) then chemical pleurodesis with talc, bleomycin,30 or tetracycline through the chest drain may be beneficial. The drain is removed when the lung is expanded and less than 100 ml of fluid is being drained per day. In some patients it takes many weeks for the drainage to settle, in which case the patient can be discharged home with the drain connected to a flutter bag. If the lung fails to expand (this may occur with mesothelioma or malignant effusions) a pleuroperitoneal shunt may be necessary.31
Empyema
Empyema describes pus within the pleural space. Causes of empyema may be parapneumonic, occur after trauma or surgery, or be associated with malignancy. Anaerobic bacteria, usually streptococci or Gram negative rods, are responsible for 76% of cases.32
Clinical presentation
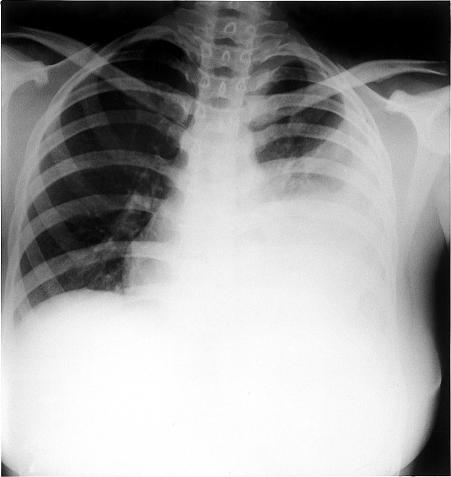
Presentation varies from fulminant sepsis to dull pain and shortness of breath. Empyema often occurs after an episode of pneumonia. Initial investigation by plain chest radiography may show features suggestive of pleural fluid and underlying consolidation (fig 4). Radiography may also show an abscess cavity with fluid, which can be confused with an intrapulmonary abscess. Computed tomography is usually required to differentiate the two. Ultrasonography is helpful in most cases of suspected empyema. It can confirm the presence of pleural fluid and determine if the fluid is suitable for needle aspiration or, if there is debris within the fluid, formal drainage.
Figure 4.
Chest x ray film of patient with empyema showing consolidation and pleural fluid
Management
Patients who present early, before the pus is loculated and a fibrinous peel has formed on the lung, are treated by simple drainage. Decortication is usually curative if the empyema is advanced beyond this or if simple drainage fails. The fibrinous peel is removed from the lung, allowing it to expand and obliterate the abscess cavity. This is a major operation requiring single lung anaesthesia, and many patients with cardiac or underlying lung disease will not tolerate it. In many centres video assisted thoracoscopic surgery is used routinely to accomplish decortication.33
Patients who are unfit for a major procedure may be treated by thrombolytic instillation or by thoracostomy, which drains the abscess via a small incision in the chest wall.34,35 Usually part of a rib is resected, and a large tube drain is placed in the cavity. Since the abscess cavity is walled off from the rest of the pleural space, it can be left open to atmospheric pressure. Usually a thick gauze dressing or a stoma bag is placed over the drain to catch the exudate. The abscess cavity gradually collapses down around the drain, which is periodically shortened. Antibiotics have little part to play. The cavity may take several months to close, so patients are usually managed at home.
Conclusion
Most patients with pneumothorax and pleural effusion can be managed by non-specialists using simple techniques. Needle thoracocentesis is the treatment of choice for tension pneumothorax. All doctors should be aware of this as tension pneumothorax can present anywhere—in the street, in patients' homes, or even at 36 000 feet.36
Patients with empyema may require prolonged specialist treatment. Although most patients can be treated expediently some will spend several months at home with a chest drain or thoracostomy and receive shared care from a district nurse, doctor, and cardiothoracic surgeon.
Acknowledgments
We thank David Mitton for help with the illustrations.
Footnotes
Competing interests: None declared.
References
- 1.Anon. Last's anatomy. London: Churchill Livingstone; 1990. [Google Scholar]
- 2.Wang N-S. Anatomy and physiology of the pleural space. Clin Chest Med. 1985;6:3–16. [PubMed] [Google Scholar]
- 3.Becker HP, Weidringer JW, Willy C, Hartel W, Blumel G. Light and scanning electron microscopy studies of the pleura. A contribution to the pathogenesis of spontaneous pneumothorax in young patients. Langenbecks Arch Chir. 1991;376:295–301. doi: 10.1007/BF00188271. . [In German.] [DOI] [PubMed] [Google Scholar]
- 4.Athanassiadi K, Kalavrouziotis G, Loutsidis A, Hatzimichalis A, Bellenis I, Exarchos N. Surgical treatment of spontaneous pneumothorax: ten-year experience. World J Surg. 1998;22:803–806. doi: 10.1007/s002689900473. [DOI] [PubMed] [Google Scholar]
- 5.Hart GJ, Stokes TC, Couch AH. Spontaneous pneumothorax in Norfolk. Br J Dis Chest. 1983;77:164–170. doi: 10.1016/0007-0971(83)90023-2. [DOI] [PubMed] [Google Scholar]
- 6.Alfageme I, Moreno L, Huertas C, Vargas A, Hernandez J, Beiztegui A. Spontaneous pneumothorax. Long-term results with tetracycline pleurodesis. Chest. 1994;106:347–350. doi: 10.1378/chest.106.2.347. [DOI] [PubMed] [Google Scholar]
- 7.Anon. Advanced trauma life support course for physicians. Chicago: American College of Surgeons; 1993. [Google Scholar]
- 8.Miller AC, Harvey JE. Guidelines for the management of spontaneous pneumothorax. Standards of Care Committee, British Thoracic Society [correction appears in BMJ 1993;307:308] BMJ. 1993;307:114–116. doi: 10.1136/bmj.307.6896.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peek GJ, Firmin RK, Arsiwala S. Chest tube insertion in the ventilated patient. Injury. 1995;26:425–426. doi: 10.1016/0020-1383(95)00055-e. [DOI] [PubMed] [Google Scholar]
- 10.Hyde J, Sykes T, Graham T. Reducing morbidity from chest drains. BMJ. 1997;314:914. doi: 10.1136/bmj.314.7085.914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chee CB, Abisheganaden J, Yeo JK, Lee P, Huan PY, Poh SC, et al. Persistent air-leak in spontaneous pneumothorax—clinical course and outcome. Resp Med. 1998;92:757–761. doi: 10.1016/s0954-6111(98)90008-7. [DOI] [PubMed] [Google Scholar]
- 12.Jain SK, Al-Kattan KM, Hamdy MG. Spontaneous pneumothorax: determinants of surgical intervention. J Cardiovasc Surg. 1998;39:107–111. [PubMed] [Google Scholar]
- 13.Rodriguez-Panadero F, Antony VB. Pleurodesis: state of the art. Eur Resp J. 1997;10:1648–1654. doi: 10.1183/09031936.97.10071648. [DOI] [PubMed] [Google Scholar]
- 14.Cagirici U, Sahin B, Cakan A, Kayabas H, Buduneli T. Autologous blood patch pleurodesis in spontaneous pneumothorax with persistent air leak. Scand Cardiovasc J. 1998;32:75–78. doi: 10.1080/14017439850140210. [DOI] [PubMed] [Google Scholar]
- 15.Passlick B, Born C, Haussinger K, Thetter O. Efficiency of video-assisted thoracic surgery for primary and secondary spontaneous pneumothorax. Ann Thorac Surg. 1998;65:324–327. doi: 10.1016/s0003-4975(97)01128-4. [DOI] [PubMed] [Google Scholar]
- 16.Waller DA, Yoruk Y, Morritt GN, Forty J, Dark JH. Videothoracoscopy in the treatment of spontaneous pneumothorax: an initial experience. Ann R Coll Surg Engl. 1993;75:237–240. [PMC free article] [PubMed] [Google Scholar]
- 17.Waller DA. Video assisted thoracoscopic surgery for spontaneous pneumothorax—a 7 year learning experience. Ann R Coll Surg Engl. 1999;81:387–392. [PMC free article] [PubMed] [Google Scholar]
- 18.Graham AN, Cosgrove AP, Gibbons JR, McGuigan JA. Randomised clinical trial of chest drainage systems. Thorax. 1992;47:461–462. doi: 10.1136/thx.47.6.461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jay SJ. Pleural effusions, 1: preliminary evaluation—recognition of the transudate. Postgrad Med. 1986;80:164–167. doi: 10.1080/00325481.1986.11699566. [DOI] [PubMed] [Google Scholar]
- 20.McLoud TC, Flower CD. Imaging the pleura: sonography, CT, and MR imaging. Am J Roentgenol. 1991;6:1145–1153. doi: 10.2214/ajr.156.6.2028857. [DOI] [PubMed] [Google Scholar]
- 21.Jay SJ. Pleural effusions, 2: definitive evaluation of the exudate. Postgrad Med. 1986;80:181–188. doi: 10.1080/00325481.1986.11699567. [DOI] [PubMed] [Google Scholar]
- 22.Light RW, Erozan YS, Ball WC., Jr Cells in pleural fluid. Their value in differential diagnosis. Arch Intern Med. 1973;132:854–860. [PubMed] [Google Scholar]
- 23.Dekker A, Bupp PA. Cytology of serous effusions. An investigation into the usefulness of cell blocks versus smears. Am J Clin Pathol. 1978;70:855–860. doi: 10.1093/ajcp/70.6.855. [DOI] [PubMed] [Google Scholar]
- 24.Kirsch CM, Kroe DM, Jensen WA, Kagawa FT, Wehner JH, Campagna AC. A modified Abrams needle biopsy technique. Chest. 1995;108:982–986. doi: 10.1378/chest.108.4.982. [DOI] [PubMed] [Google Scholar]
- 25.Salyer WR, Eggleston JC, Erozan YS. Efficacy of pleural needle biopsy and pleural fluid cytopathology in the diagnosis of malignant neoplasm involving the pleura. Chest. 1975;67:536–539. doi: 10.1378/chest.67.5.536. [DOI] [PubMed] [Google Scholar]
- 26.McLean AN, Bicknell SR, McAlpine LG, Peacock AJ. Investigation of pleural effusion: an evaluation of the new Olympus LTF semiflexible thoracofiberscope and comparison with Abram's needle biopsy. Chest. 1998;114:150–153. doi: 10.1378/chest.114.1.150. [DOI] [PubMed] [Google Scholar]
- 27.Larsen K, Axelsen F. Closed pleural biopsy and fluid cytology in the diagnosis of suspected pulmonary cancer with pleural involvement. Scand J Thorac Cardiovasc Surg. 1982;16:197–199. doi: 10.3109/14017438209101810. [DOI] [PubMed] [Google Scholar]
- 28.Boutin C, Rey F. Thoracoscopy in pleural malignant mesothelioma: a prospective study of 188 consecutive patients. Part 1: diagnosis. Cancer. 1993;72:389–393. doi: 10.1002/1097-0142(19930715)72:2<389::aid-cncr2820720213>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 29.Light RW, Rodriguez RM. Management of parapneumonic effusions. Clin Chest Med. 1998;19:373–382. doi: 10.1016/s0272-5231(05)70084-8. [DOI] [PubMed] [Google Scholar]
- 30.Noppen M, Degreve J, Mignolet M, Vincken W. A prospective, randomised study comparing the efficacy of talc slurry and bleomycin in the treatment of malignant pleural effusions. Acta Clinica Belgica. 1997;52:258–262. doi: 10.1080/17843286.1997.11718587. [DOI] [PubMed] [Google Scholar]
- 31.Petrou M, Kaplan D, Goldstraw P. Management of recurrent malignant pleural effusions. The complementary role of talc pleurodesis and pleuroperitoneal shunting. Cancer. 1995;75:801–805. doi: 10.1002/1097-0142(19950201)75:3<801::aid-cncr2820750309>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 32.Varkey B. Pleural effusions caused by infection. Postgrad Med. 1921;80:213–216. doi: 10.1080/00325481.1986.11699570. [DOI] [PubMed] [Google Scholar]
- 33.Cassina PC, Hauser M, Hillejan L, Greschuchna D, Stamatis G. Video-assisted thoracoscopy in the treatment of pleural empyema: stage-based management and outcome. J Thorac Cardiovasc Surg. 1999;117:234–238. doi: 10.1016/S0022-5223(99)70417-4. [DOI] [PubMed] [Google Scholar]
- 34.Chin NK, Lim TK. Controlled trial of intrapleural streptokinase in the treatment of pleural empyema and complicated parapneumonic effusions. Chest. 1997;111:275–279. doi: 10.1378/chest.111.2.275. [DOI] [PubMed] [Google Scholar]
- 35.Anon. Glenn's thoracic and cardiovascular surgery. Englewood Cliffs, NJ: Prentice-Hall; 1991. [Google Scholar]
- 36.Wallace WA. Managing in flight emergencies: a personal account. BMJ. 1995;311:374–375. doi: 10.1136/bmj.311.7001.374. [DOI] [PMC free article] [PubMed] [Google Scholar]