Key Points
Question
What are the safety, pharmacokinetic, and survival outcomes of B-cell maturation antigen (BCMA)/CD19 dual-targeting chimeric antigen receptor (CAR) T-cell therapy in individuals with high-risk newly diagnosed multiple myeloma who receive it as a frontline treatment?
Findings
In this single-arm, open-label phase 1 cohort study including 19 patients in the efficacy analysis, all patients (100%) achieved stringent complete responses and minimal residual disease negativity. The treatment showed a favorable safety profile in the 22 patients in the safety analysis, with 6 patients (27%) experiencing mild to moderate cytokine release syndrome and no patients with immune effector cell–associated neurotoxicity syndrome.
Meaning
These results suggest that the BCMA/CD19 dual-targeting CAR T-cell therapy, GC012F, is a safe treatment associated with positive health and survival outcomes for patients with high-risk newly diagnosed multiple myeloma eligible for transplant following initial induction therapy.
Abstract
Importance
Patients with high-risk newly diagnosed multiple myeloma (NDMM) often have poor outcomes with standard treatments, necessitating novel effective frontline therapies to enhance clinical outcomes. GC012F, a B-cell maturation antigen/CD19 dual-targeting chimeric antigen receptor (CAR) T-cell therapy, has been developed on the novel FasTCAR platform. Notably, its use as a frontline therapy for patients with high-risk NDMM who are eligible for transplant has not been thoroughly explored.
Objective
To examine the safety, pharmacokinetics, and patient health and survival outcomes associated with GC012F in individuals with NDMM.
Design, Setting, and Participants
Patients were enrolled in this single-arm, open-label phase 1 cohort study between June 28, 2021, and June 1, 2023 (the data cutoff date). All patients included in this study were treated at a single center, Shanghai Changzheng Hospital. The patients in the efficacy evaluation were followed up for a minimum period of 3 months.
Intervention
Patients underwent 2 cycles of induction therapy, followed by GC012F infusion (at 1 × 105 cells/kg, 2 × 105 cells/kg, or 3 × 105 cells/kg).
Main Outcomes and Measures
The primary goals were to assess the safety, efficacy, and pharmacokinetics of GC012F at various dose levels.
Results
Of 22 patients receiving GC012F treatment, 6 experienced mild to moderate cytokine release syndrome (grade 1-2) and none experienced neurotoxic effects. Nineteen patients were included in the efficacy evaluation, and all 19 patients showed stringent complete responses and achieved minimal residual disease negativity. The treatment’s effectiveness was consistent across different dose levels. GC012F demonstrated a rapid response, with a median time to first stringent complete response of 84 days (range, 26-267 days) and achieving minimal residual disease negativity within 28 days (range, 23-135 days). The CAR T-cell expansion was robust, with a median peak copy number of 60 652 copies/μg genomic DNA (range, 8754-331 159 copies/μg genomic DNA), and the median time to median peak copy number was 10 days (range, 9-14 days).
Conclusions and Relevance
The findings of this single-arm, open-label phase 1 cohort study suggest that GC012F may be a safe treatment associated with positive health and survival outcomes for patients with high-risk NDMM eligible for transplant. Owing to the small sample size, further studies with larger cohorts and longer follow-up durations are needed.
This single-arm, open-label phase 1 cohort study examines the safety, patient health, and survival outcomes of GC012F in individuals with high-risk newly diagnosed multiple myeloma.
Introduction
Despite advances in frontline standard therapy, patients with newly diagnosed multiple myeloma (NDMM) exhibiting high-risk features often experience poor clinical outcomes, even among those eligible for transplantation.1,2 The absence of a standardized definition for high-risk multiple myeloma has hindered the identification of an optimal treatment approach.
B-cell maturation antigen (BCMA)/CD19 dual-targeting chimeric antigen receptor (CAR) T-cell therapy is a novel approach demonstrating potential efficacy in the treatment of patients with relapsed and refractory multiple myeloma (RRMM).3,4,5,6 However, relapses remain frequent, particularly in patients with high-risk disease. Hence, the simultaneous targeting of different surface antigens of BCMA and CD19, with CD19 cells having a strong myeloma-propagating capability,7 is an effective strategy to prevent relapse of multiple myeloma.
GC012F is an autologous anti-BCMA/CD19 bispecific CAR T-cell therapy developed using the FasTCAR platform that enabled next-day manufacturing. The findings of our previous study suggest it is safe and efficacious in patients with RRMM. Herein, we present a preliminary analysis assessing the safety, pharmacokinetics, and survival outcomes of GC012F in patients with high-risk NDMM following induction therapy.
Methods
This single-arm, open-label phase 1 cohort study was conducted at Shanghai Changzheng Hospital. The protocol received approval from the Institutional Review Board and the Independent Ethics Committees of Shanghai Changzheng Hospital. All patients who were enrolled in this study provided written informed consent. Eligible participants met at least 1 high-risk feature (eMethods in Supplement 1). Patients were enrolled between June 28, 2021, and June 1, 2023 (data cutoff date).
After lymphodepletion with fludarabine and cyclophosphamide, the GC012F CAR T cells were administered at 3 dose levels:
1 × 105 cells/kg;
2 × 105 cells/kg; and
3 × 105 cells/kg.
Patients achieving minimal residual disease (MRD) negativity8 with complete response (CR) could be maintained on lenalidomide from month 6 based on investigators’ discretion (eAppendix in Supplement 1). The primary end points included adverse events (AEs)9; overall response rate (ORR)10; CR and stringent CR (sCR) rates; MRD-negative rate; duration of response (DOR); and progression-free survival (PFS). Secondary end points included overall survival (OS); time to first response; time to best response; and pharmacokinetic and biomarkers.
Categorical variables were compared using the Fisher exact test. Continuous variables were compared using the Mann-Whitney U test (for 2 groups) or the Kruskal-Wallis test (for 3 or more groups). The Clopper-Pearson method was used to construct 95% CIs. Time-to-event data were estimated using the Kaplan-Meier method. Data were analyzed with R statistical software, version 3.5.1 (R Project for Statistical Computing) or SPSS 22 (IBM). Statistical significance was defined as a 2-tailed P < .05.
Results
Patients’ Disposition and Characteristics
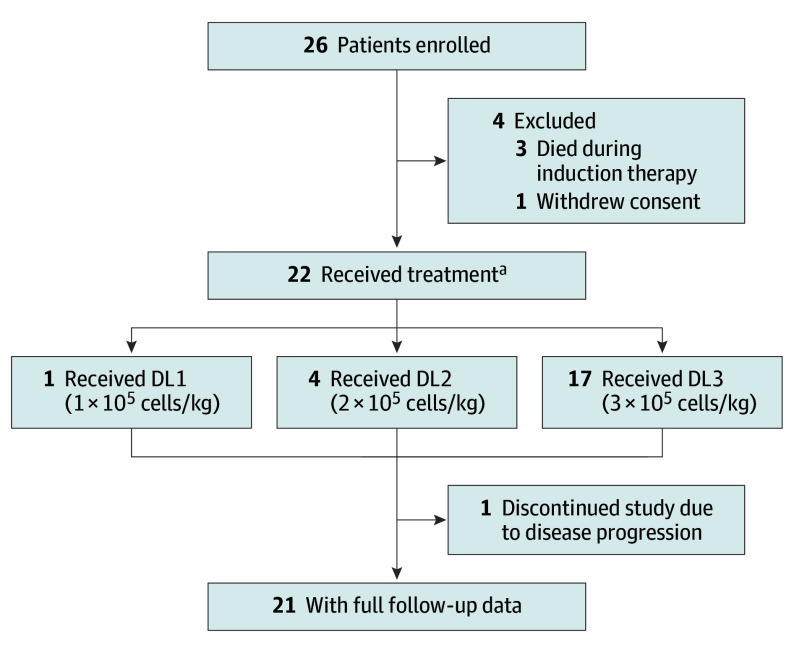
Of 26 enrolled patients, 22 individuals received infusion and were included in the safety analysis. Nineteen patients were evaluable at the median follow-up of 16 months (range, 3.6-23.6 months) and included in the efficacy analysis (Figure 1; median [range] age of cohort, 59 [43-69] years; 12 [63%] male; Table). All patients exhibited at least 2 high-risk features and received 2 cycles of induction therapy (eTables 1-3 in Supplement 1).
Figure 1. CONSORT Diagram.
Data cutoff of the interim analysis was June 1, 2023. Median duration of follow-up was 16.0 months (range, 3.6-23.6 months).
Abbreviations: DL, dose level.
aA total of 22 patients were in the safety analysis, and 19 had at least 1 evaluable record in the efficacy analysis.
Table. Baseline Characteristics of Patients by Infusion Dose Using Full Analysis Set.
| Characteristica | No. (%) | |||
|---|---|---|---|---|
| DL1 (n = 1) | DL2 (n = 4) | DL3 (n = 14) | Total (N = 19) | |
| Age, median (range), y | 65 | 64 (51-69) | 57 (43-64) | 59 (43-69) |
| Male | 0 | 3 (75) | 9 (64) | 12 (63) |
| Time since diagnosis, median (range), mob | 4.7 | 3.6 (3.2-4.5) | 3.8 (2.0-5.4) | 3.7 (2.0-5.4) |
| Monoclonal globulin | ||||
| IgG | 0 | 1 (25) | 7 (50) | 8 (42) |
| IgA | 0 | 1 (25) | 5 (36) | 6 (32) |
| IgD | 0 | 2 (50) | 0 | 2 (11) |
| Light chain | 1 (100) | 0 | 2 (14) | 3 (16) |
| DS disease stage | ||||
| I | 0 | 0 | 0 | 0 |
| II | 0 | 0 | 0 | 0 |
| III | 1 (100) | 4 (100) | 14 (100) | 19 (100) |
| ISS disease stage | ||||
| I | 0 | 0 | 2 (14) | 2 (11) |
| II | 1 (100) | 1 (25) | 9 (64) | 11 (58) |
| III | 0 | 3 (75) | 3 (21) | 6 (32) |
| R-ISS disease stage | ||||
| I | 0 | 0 | 2 (14) | 2 (11) |
| II | 1 (100) | 2 (50) | 11 (79) | 14 (74) |
| III | 0 | 2 (50) | 1 (7) | 3 (16) |
| R2-ISS disease stage | ||||
| I | 0 | 0 | 0 | 0 |
| II | 0 | 0 | 2 (14) | 2 (11) |
| III | 1 (100) | 2 (50) | 11 (79) | 14 (74) |
| IV | 0 | 1 (25) | 1 (7) | 2 (11) |
| Not sure | 0 | 1 (25) | 0 | 1 (5) |
| ECOG performance-status score | ||||
| 0 | 0 | 0 | 3 (21) | 3 (16) |
| 1 | 1 (100) | 1 (25) | 8 (57) | 10 (53) |
| 2 | 0 | 3 (75) | 3 (21) | 6 (32) |
| High tumor burdenc | 0 | 2 (50) | 3 (21) | 5 (26) |
| Plasmacytomas in multiple myeloma | ||||
| Any | 1 (100) | 3 (75) | 8 (57) | 12 (63) |
| Paraskeletal plasmacytoma | 1 (100) | 1 (25) | 7 (50) | 9 (47) |
| Extramedullary disease | 0 | 2 (50) | 1 (7) | 3 (16) |
| High-risk cytogenetics | 1 (100) | 1 (25) | 7 (50) | 9 (47) |
| amp(1q21) | 1 (100) | 1 (25) | 5 (36) | 7 (37) |
| del(17p) | 0 | 1 (25) | 1 (7) | 2 (11) |
| t(4;14) | 0 | 0 | 1 (7) | 1 (5) |
| t(14;16) | 0 | 0 | 0 | 0 |
| ≥2 High-risk cytogenetics | 0 | 1 (25) | 0 | 1 (5) |
| Missing | 0 | 1 (25) | 0 | 1 (5) |
| Previous systemic therapy regimen (2 cycles) | ||||
| VRd (2 cycles) | 1 (100) | 3 (75) | 14 (100) | 18 (95) |
| PAD (1 cycle) + VRd (1 cycle) | 0 | 1 (25) | 0 | 1 (5) |
Abbreviations: amp, amplification ≥4 copies; del, deletion; DL, dose level; DS, Durie-Salmon System; ECOG, Eastern Cooperative Oncology Group; Ig, immunoglobulin; ISS, International Staging System; PAD, bortezomib, epirubicin, dexamethasone; R-ISS, Revised International Staging System; R2-ISS, Second Revision of the International Staging System; t, translocation; VRd, bortezomib, lenalidomide, dexamethasone.
Baseline characteristics of the patients were assessed at the time of diagnosis.
Time between initial diagnosis and GC012F infusion.
At least 60% or more bone marrow plasma cells.
Safety
AEs were evaluated in 22 patients, with the most common treatment-emergent AE being hematologic toxic effects (eTable 4 in Supplement 1). Grade 3 or higher AEs included lymphopenia (14 patients [64%]), leukopenia (10 patients [45%]), and neutropenia (9 patients [41%]). Nonhematologic treatment-emergent AEs were mainly grades 1 or 2, with the most common being increased lactate dehydrogenase (9 patients [41%]), hypocalcemia (9 patients [41%]), and hypoalbuminemia (9 patients [41%]).
Low-grade cytokine release syndrome (CRS) occurred in 6 patients (27%) (eFigure 1, eTable 4 in Supplement 1). The median time to CRS onset was 7 days (range, 6-9 days) with a median duration of 1 day (range, 1-4 days). No neurotoxic effects were observed. All patients developed B-cell aplasia (eTable 5 in Supplement 1). No patients had treatment-related tumor lysis syndrome; or replication-competent retrovirus.
Efficacy
The ORR was 100%, with best response being sCR in all 19 patients (Figure 2). All evaluable patients demonstrated MRD negativity at 1 month, 6 months, and 12 months after infusion (eTable 6 in Supplement 1). The median time to the first sCR was 84 days (range, 26-267 days), and for the first MRD negativity, it was 28 days (range, 23-135 days).
Figure 2. Clinical Responses to GC012F Infusion.

Swimmer’s plot of clinical responses over time. The data analysis was conducted using full analysis set. CR indicates complete response; DL, dose level; MRD, minimal residual disease; PD, progressive disease; PR, partial response; sCR, stringent complete response; VGPR, very good partial response.
The median time to the first sCR was 84 days (range, 26-267 days), and for the first MRD negativity, it was 28 days (range, 23-135 days).
ORRs across subgroups were generally similar to those in the overall cohort (eFigure 2, eTables 7-8 in Supplement 1). However, 1 patient achieved sCR with MRD negativity during the first assessment but unfortunately progressed 3 months after infusion (Figure 2; subsequent therapies provided in eFigure 3 in Supplement 1). Median values for DOR, PFS, and OS had not yet been reached.
Pharmacokinetics and Biomarkers
GC012F expansion was observed in the peripheral blood of 22 patients. The median peak copy number (Cmax) was 60 652 copies/μg genomic DNA (gDNA) (range, 8754-331 159 copies/μg gDNA), and the median time to Cmax (Tmax) was 10 days (range, 9-14 days). Median persistence was 29 days (range, 26-196 days). The median area under the curve (AUC0-28) was 289 685 (range, 80 181-3 985 420), with no difference observed across dose levels (P = .77) (eFigure 4 in Supplement 1). Cmax and AUC0-28 were not significantly associated with CRS; however, Cmax was higher among patients with treated CRS compared with untreated CRS (137 404 vs 30 691 copies/μg gDNA; P = .01) and those without CRS (137 404 vs 62 131 copies/μg gDNA; P = .04) (eFigure 5-7 in Supplement 1). The expansion of GC012F was not significantly associated with DOR, PFS, and OS (eFigure 8 in Supplement 1).
Discussion
In this single-arm, open-label phase 1 cohort study of BCMA/CD19 dual-targeted CAR T in patients with high-risk NDMM, GC012F showed a good safety profile with a low-grade CRS rate. All patients had favorable outcomes with MRD negativity and sCR. A potentially durable response is indicated with medians of DOR, PFS, and OS not reached.
Only 1 patient, who met all 5 high-risk criteria, progressed after a 3-month follow-up, with rib mass but no measurable disease in blood and urine. We postulate that plasmacytoma signals from the tumor microenvironment, tumor antigen escape mechanisms, and systemic inflammatory consequences of infusion might have influenced the efficacy of CAR T-cell therapy.
In the present study, GC012F resulted in early MRD negativity at 1 month using a more stringent threshold of 10−6. This was sustained at 6 and 12 months, favorable in comparison with previous studies.11 Although bone marrow may still be hypocellular at the early time point after CAR T therapy, Lin Y et al recently reported that bone marrow MRD negative at month 1, regardless of cellularity status in bone marrow, correlated with CR/sCR response and prolonged PFS.12
GC012F also showed a favorable safety profile without dose-limiting toxic effects. Cytopenia was the most common grade 3 or higher AE exhibiting a rapid recovery, faster than in the cohort of patients with RRMM.13 Moreover, CRS occurred at a lower rate than in patients with RRMM (27% vs 86%).13 The infrequent occurrence of CRS can be attributed to the reduced tumor burden following induction therapy and the lower levels of key cytokines, in contrast to that observed in published trials for RRMM.14,15
Limitations
Owing to the small sample size, further studies with larger cohorts and longer follow-up durations are warranted to determine the benefit of GC012F as an early intervention after induction therapy in this patient population.
Conclusions
In this single-arm, open-label phase 1 cohort study, dual-targeting of BCMA/CD19 in patients with NDMM who were eligible for transplant using GC012F (FasTCAR) showed favorable safety and promising efficacy. Further studies with larger cohorts and longer follow-up durations are warranted to determine the benefits of GC012F as an early intervention after induction therapy in this patient population.
eAppendix. List of Investigators
eMethods. Additional Methodological Information
eFigure 1. Median Cytokine Concentrations over Time
eFigure 2. Subgroup analysis of ORR
eFigure 3. Timeline of Clinical Events for the Patient with PD
eFigure 4. CAR T cell Expansion and Persistence
eFigure 5. The Cmax by the Occurrence of CRS
eFigure 6. AUC0–28 Based on the Occurrence of CRS
eFigure 7. The Cmax Based on the Occurrence of CRS (Treated and Untreated)
eFigure 8. Association of CAR T cell expansion with DoR, PFS, and OS
eTable 1. Baseline High-Risk Features in the Cohort
eTable 2. Baseline Characteristics of Patients by the Number of High-risk Features
eTable 3. Prior Treatments
eTable 4. Adverse Events
eTable 5. Infections and Related AEs
eTable 6. Responses Based on Infusion Dose
eTable 7. Responses by the Number of High-risk Features
eTable 8. Responses in Patients with Paraskeletal Plasmacytoma and Extramedullary Disease
Data Sharing Statement
References
- 1.D’Agostino M, Cairns DA, Lahuerta JJ, et al. Second revision of the International Staging System (R2-ISS) for overall survival in multiple myeloma: a European Myeloma Network (EMN) report within the HARMONY project. J Clin Oncol. 2022;40(29):3406-3418. doi: 10.1200/JCO.21.02614 [DOI] [PubMed] [Google Scholar]
- 2.Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised international staging system for multiple myeloma: a report from International Myeloma Working Group. J Clin Oncol. 2015;33(26):2863-2869. doi: 10.1200/JCO.2015.61.2267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du J, Wei R, Jiang S, et al. CAR-T cell therapy targeting B cell maturation antigen is effective for relapsed/refractory multiple myeloma, including cases with poor performance status. Am J Hematol. 2022;97(7):933-941. doi: 10.1002/ajh.26583 [DOI] [PubMed] [Google Scholar]
- 4.Martin T, Usmani SZ, Berdeja JG, et al. Ciltacabtagene autoleucel, an anti-B-cell maturation antigen chimeric antigen receptor T-cell therapy, for relapsed/refractory multiple myeloma: CARTITUDE-1 2-year follow-up. J Clin Oncol. 2023;41(6):1265-1274. doi: 10.1200/JCO.22.00842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.San-Miguel J, Dhakal B, Yong K, et al. Cilta-cel or standard care in lenalidomide-refractory multiple myeloma. N Engl J Med. 2023;389(4):335-347. doi: 10.1056/NEJMoa2303379 [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez-Otero P, Ailawadhi S, Arnulf B, et al. Ide-cel or standard regimens in relapsed and refractory multiple myeloma. N Engl J Med. 2023;388(11):1002-1014. doi: 10.1056/NEJMoa2213614 [DOI] [PubMed] [Google Scholar]
- 7.Hosen N. Multiple myeloma-initiating cells. Int J Hematol. 2013;97(3):306-312. doi: 10.1007/s12185-013-1293-0 [DOI] [PubMed] [Google Scholar]
- 8.Flores-Montero J, Sanoja-Flores L, Paiva B, et al. Next generation flow for highly sensitive and standardized detection of minimal residual disease in multiple myeloma. Leukemia. 2017;31(10):2094-2103. doi: 10.1038/leu.2017.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee DW, Santomasso BD, Locke FL, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transplant. 2019;25(4):625-638. doi: 10.1016/j.bbmt.2018.12.758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328-e346. doi: 10.1016/S1470-2045(16)30206-6 [DOI] [PubMed] [Google Scholar]
- 11.Kaiser MF, Hall A, Walker K, et al. Daratumumab, cyclophosphamide, bortezomib, lenalidomide, and dexamethasone as induction and extended consolidation improves outcome in ultra-high-risk multiple myeloma. J Clin Oncol. 2023;41(23):3945-3955. doi: 10.1200/JCO.22.02567 [DOI] [PubMed] [Google Scholar]
- 12.Bansal R, Baksh M, Larsen JT, et al. Prognostic value of early bone marrow MRD status in CAR-T therapy for myeloma. Blood Cancer J. 2023;13(1):47. doi: 10.1038/s41408-023-00820-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Du J, Fu W, Jiang H, et al. Updated results of a phase I, open-label study of BCMA/CD19 dual-targeting FasT CAR-T GC012F for patients with relapsed/refractory multiple myeloma (RRMM). J Clin Oncol. 2023;41(16_suppl). doi: 10.1200/JCO.2023.41.16_suppl.8005 [DOI] [Google Scholar]
- 14.Yan Z, Cao J, Cheng H, et al. A combination of humanised anti-CD19 and anti-BCMA CAR T cells in patients with relapsed or refractory multiple myeloma: a single-arm, phase 2 trial. Lancet Haematol. 2019;6(10):e521-e529. doi: 10.1016/S2352-3026(19)30115-2 [DOI] [PubMed] [Google Scholar]
- 15.Hay KA, Hanafi LA, Li D, et al. Kinetics and biomarkers of severe cytokine release syndrome after CD19 chimeric antigen receptor-modified T-cell therapy. Blood. 2017;130(21):2295-2306. doi: 10.1182/blood-2017-06-793141 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. List of Investigators
eMethods. Additional Methodological Information
eFigure 1. Median Cytokine Concentrations over Time
eFigure 2. Subgroup analysis of ORR
eFigure 3. Timeline of Clinical Events for the Patient with PD
eFigure 4. CAR T cell Expansion and Persistence
eFigure 5. The Cmax by the Occurrence of CRS
eFigure 6. AUC0–28 Based on the Occurrence of CRS
eFigure 7. The Cmax Based on the Occurrence of CRS (Treated and Untreated)
eFigure 8. Association of CAR T cell expansion with DoR, PFS, and OS
eTable 1. Baseline High-Risk Features in the Cohort
eTable 2. Baseline Characteristics of Patients by the Number of High-risk Features
eTable 3. Prior Treatments
eTable 4. Adverse Events
eTable 5. Infections and Related AEs
eTable 6. Responses Based on Infusion Dose
eTable 7. Responses by the Number of High-risk Features
eTable 8. Responses in Patients with Paraskeletal Plasmacytoma and Extramedullary Disease
Data Sharing Statement