Abstract
Okur-Chung neurodevelopmental syndrome (OCNDS) is an ultra-rare disorder caused by variants in the CSNK2A1 gene. CSNK2A1 encodes for the alpha subunit of casein kinase 2 (CK2), a serine/threonine kinase critical in neural development. CK2 is implicated in many human pathologies, including viral infections, cancer, inflammation, cardiovascular, neurodegenerative, and psychiatric diseases. However, the mechanism of action for the CSNK2A1 variants observed in OCNDS is not fully understood, although studies suggest a loss of function or altered substrate specificity. There are no approved treatments for OCNDS, and current treatments focus on symptom management. The CSNK2A1 Foundation was established in 2018 and aims to find a cure for OCNDS and provide support to affected individuals. OCNDS presents with symptoms at varying severity, including developmental delay/intellectual disabilities, autism, disrupted sleep, speech delays/inability to speak, short stature, and, in ~25% of cases, epilepsy. The foundation has developed a research toolbox that is readily available to researchers worldwide and has awarded ~$1 million in grant funding. These efforts have provided valuable insights into CK2 biology and the natural history of OCNDS. However, additional efforts are needed to fully characterize the disease mechanism and investigate potential treatment interventions. Continued investigation into CK2 and its role in neural development holds promise for a better understanding of OCNDS and related disorders in the future. To accelerate research, we have developed a research roadmap highlighting key focus areas of landscape analysis/toolbox expansion, biomarker development, and therapeutic testing through a series of steps that are nonlinear; we expect these efforts to guide decision-making for therapeutic exploration whether that be drug repurposing, gene therapy, novel drug discovery, or a combination. In this perspective article, we describe OCNDS and the CSNK2A1 gene, highlight gaps in OCNDS research, discuss the research roadmap, and offer the founder’s perspective on our growth and future opportunities.
Keywords: CK2, CSNK2A1, OCNDS, Okur Chung, Roadmap, rare disease
Plain language summary
Patient organization perspective: a research roadmap for Okur-Chung Neurodevelopmental Syndrome
Okur-Chung Neurodevelopmental Syndrome (OCNDS) is an ultra-rare disorder caused by variants in the CSNK2A1 gene.
CSNK2A1 creates a subunit of CK2, a critical protein in brain development among other biological processes.
There are no approved treatments for OCNDS, and current suggested treatments focus on symptom management.
Individuals with OCNDS exhibit many symptoms at varying severity levels, including developmental delay/intellectual disabilities, autism, disrupted sleep, speech delays/inability to speak, short stature, and in approximately 25% of cases, epilepsy. We think that seizure prevalence may be underreported due to lack of extended EEG recordings for OCNDS patients and that seizures may preferentially occur at night as has been observed in other autism spectrum disorders.
The CSNK2A1 Foundation was established in 2018 and aims to find a cure for OCNDS and provide support to affected individuals. The CSNK2A1 Foundation’s research tools and efforts have provided valuable insights into the biology of OCNDS and the natural history of the disorder. However, additional efforts are needed to fully understand how OCNDS affects the body and investigate potential treatment approaches.
To accelerate OCNDS research, the foundation has developed a research roadmap that is presented in this perspective article. We describe OCNDS and the CSNK2A1 gene, highlight gaps in OCNDS research, discuss the research roadmap, and offer the founder’s perspective on our growth and future opportunities.
About Okur-Chung Neurodevelopmental Syndrome and CSNK2A1
Okur-Chung neurodevelopmental syndrome (OCNDS; OMIM #617062) was discovered in 2016 by Dr. Volkan Okur and Dr. Wendy Chung via whole exome sequencing with the first paper highlighting five cases published in Human Genetics on April 5, 1 which is the date now designated as International OCNDS Awareness Day each year. OCNDS is caused by mutations in the CSNK2A1 gene that encodes for the alpha catalytic subunit of casein kinase 2 (CK2), an ubiquitous serine/threonine kinase critical in neural development and a protein that has been implicated in various human pathologies, including cancer, inflammation, cardiovascular disease, neurodegenerative disease, psychiatric disorders, and viral infections. 2 There are no approved treatments for OCNDS, and current proposed treatments focus on symptom management. 3
Most mutations in CSNK2A1 are de novo; however, there have been a few cases of familial inheritance. Through these cases, we now know that OCNDS follows an autosomal dominant inheritance pattern. 4 OCNDS is characterized by developmental delay, language delay, intellectual disability, hypotonia, behavioral problems, seizures, and severe sleep issues among other symptoms (Figure 1). A critical gap in OCNDS phenotyping is the true prevalence of seizures. Although current clinical overviews indicate that approximately 25% of OCNDS patients experience seizures, parent reports and electroencephalogram (EEG) notes suggest that other OCNDS patients experience epileptiform activity, but only while sleeping. We estimate that seizure prevalence is underreported due to the lack of extended EEG recordings and that seizures may preferentially occur at night as has been observed in other autism spectrum disorders (ASDs). 5
Figure 1.
Symptoms of OCNDS.
OCNDS, Okur-Chung neurodevelopmental syndrome.
Based on Simons Foundation Autism Research Initiative (SFARI) profiling, CSNK2A1 is an ASD gene with the highest Gene Score of 1, 6 meaning that CSNK2A1 has been clearly implicated in ASD and has at least three de novo gene disrupting mutations reported in the literature. The symptom profile of OCNDS includes some typical ASD symptoms including stereotypic movements, learning disabilities, sensory challenges, sleep problems, and seizures. In an informal family survey performed by Simons Searchlight 7 in 2022, the top three issues reported by OCNDS families were (1) intellectual disability/developmental delay, (2) language delay/inability to speak, and (3) sleep issues, with 77% of families reporting sleep-related disruptions.
CK2 is an important player in a postsynaptic functional unit that affects cellular excitability and is a modulator of the circadian clock protein PER2. 8 In Drosophila, a dominant negative mutant of CK2 (CK2αTik) induced a severe period lengthening (~33 h), greater than the majority of known circadian mutant alleles, 9 further highlighting the important role that CK2 has in regulating circadian rhythm. Sleep difficulties are often overlooked in individuals with ASDs due to the severity of other symptoms and due to current treatment guidelines for managing challenging behaviors in ASD rarely addressing sleep. 10 Although there is an abundance of evidence that significant sleep problems are common in individuals with ASD and that poor sleep quality/duration can exacerbate ASD behavioral symptoms,10–12 there have not been sufficient interventions to improve symptoms and quality of life, representing a critical need for individuals with OCNDS that have an ASD diagnosis.
CK2 has been studied for over 70 years, but never in the context of OCNDS until its discovery in 2016. CK2 is a complex consisting of four subunits, two α or α′ subunits and two β subunits, all encoded by distinct genes. 13 A different neurodevelopmental disorder discovered in 2017 is associated with mutations in CSNK2B, encoding for the regulatory β subunit of CK2, called Poirier-Bienvenu neurodevelopmental syndrome. 14 Both the α and β subunits are indispensable for embryonic development in animals.15–17 CK2α is far more abundant in the brain than in any other tissue 18 and plays a critical role in regulating neuronal excitability and synaptic transmission. 2 Currently, the mechanism of action for CSKN2A1 variants is unclear, representing a major gap in the field and creating a roadblock to treatment development for OCNDS. Current literature suggests potential loss of function, shift in substrate specificity, and/or dominant negative mechanisms depending on the variant.19,20
Over 200 patients have registered with the CSNK2A1 Foundation, 21 with another ~40 known globally. Currently, the only method of diagnosing OCNDS is via molecular genetic testing. We expect the number of individuals with OCNDS to be much higher and that the number of registered individuals will increase as access to sequencing technologies improves. CSNK2A1 variants have been discovered along the entire kinase domain in OCNDS patients, with the majority classified as missense mutations. 22 In the foundation’s registry, we have recorded 82 distinct variants and 22 distinct deletions. 21 Recent work analyzed the activity of 16 distinct CSNK2A1 mutations toward a consensus peptide and found activity to be significantly reduced. 20 Furthermore, differences in subcellular localization between variants were observed implying that the position of the mutation may differentially impact CK2 mechanisms and, thus, symptom presentation in patients. However, given another study demonstrating a shift a substrate specificity 19 and the potential for other mechanisms not yet tested, this is one of the many existing questions that drive our current roadmap (Figure 2). Potential strategies to better understand the functional consequences of these variants include generating an OCNDS-specific portal similar to the GRIN Portal 23 to generate a database of known variants, provide additional information and data visualization from the foundation’s registry and natural history (NH) study, and support updates to interpretation/classification. Furthermore, we could pursue efforts similar to GRIN through a Center for Functional Evaluation of Rare Variants 24 or provide directed funds toward a project to assess variants in a standardized manner 25 [e.g., utilizing Xenopus laevis (frog) oocytes and a set of relevant measurements such as electrophysiological properties and protein expression].
Figure 2.
CSNK2A1 Foundation’s research roadmap for OCNDS.
OCNDS, Okur-Chung neurodevelopmental syndrome.
Gaps in OCNDS research
To address our key unanswered questions and other gaps in our understanding of OCNDS, we have identified key needs including increased funding, basic science studies, research toolbox model characterization, a data sharing mechanism for scientists, expansion of our Scientific Advisory Board (SAB), an International Statistical Classification of Diseases and Related Health Problems (ICD-10) code, formal clinical consensus guidelines, and increased awareness of OCNDS by clinicians and researchers. Some of these needs have recently been addressed – for example, we noticed key gaps in our SAB for expertise in preclinical gene therapy and neurology. We have recently added Dr. Rachel Bailey and Dr. Kim Goodspeed to fill these gaps alongside our existing members Dr. Wendy Chung, Dr. Volkan Okur, Dr. Tika Benveniste, and Kyle Retterer. We envision expanding our SAB further in 2025 to add someone with experience in the development of clinical outcomes in rare diseases.
|
Key unanswered questions
1. Do mutations in CK2 act via a haploinsufficiency, dominant negative, or other mechanism? Do mutations in different regions of the gene act via distinct mechanisms? 2. How do mutations in CSNK2A1 affect human cells? 3. Can we define a biomarker for OCNDS (e.g., via phosphoproteomics to assess CK2 target selection and abundance, EEG marker for sleep and/or seizure activity, or other)? 4. Can we accurately model OCNDS in a mouse? If so, can we rescue the phenotype(s) using gene editing techniques or drug repurposing? 5. What is the best therapeutic avenue to treat OCNDS? 6. What does adulthood typically look like for individuals with OCNDS? |
From a clinical position, we do not have an ICD-10 code, an important system used to track and report diseases, injuries, and disorders. 26 These ICD codes allow for easy retrieval of health information to compare across hospitals and time periods; importantly, this provides the power to better understand the types of medical specialties diagnosing OCNDS and the ability to track health outcomes following therapeutic administration. Furthermore, OCNDS is currently only diagnosed via molecular genetic testing limiting the ability to find new patients as many parts of the world do not have access. As such, obtaining an ICD-10 code will be a focused effort for the foundation in the next few years to help us find and connect with new patients. We are grateful to be partnered with the Orphan Disease Center at the University of Pennsylvania 27 as this partnership has provided us access to a genetic counseling master’s student intern in early 2024 who will help us advocate for OCNDS to be added to all epilepsy and autism sequencing panels at different companies.
Furthermore, we do not have formal clinical consensus guidelines for OCNDS. The closest guidance to date is a GeneReview publication from 2022 highlighting current clinical characteristics, suggestive findings, and management. 3 Generating real-world evidence both prospectively and retrospectively through initiatives, such as medical record collection, our contact registry, and NH study, will highlight gaps in care as well as disparities including delayed diagnoses that will assist the foundation in advocating for federal policy changes and an ICD-10 code in the future. We have made significant efforts to increase awareness of OCNDS through publications such as a NORD Rare Disease Report in the NORD database, 28 social media posts, and attending conferences to network with other professionals and engage new clinicians that may be seeing a patient with OCNDS. We will prioritize engagement in three main categories through the next year (Figure 3): scientific community, patient/caregiver community, and other stakeholders although we expect to introduce more focused clinician engagement in the coming years as we identify more patients.
Figure 3.
CSNK2A1 Foundation’s 2024 engagement plans.
Roadmap and key initiatives
We focus our efforts on initiatives that will bring the most value to the OCNDS community as quickly as possible. Thus, our efforts to date have focused on the development of a research toolbox and establishing an experienced SAB. The full phenotypic range of OCNDS is currently unknown, and major questions regarding disease progression remain unanswered. Our current work highlighted in the roadmap is focused on three major initiatives: (1) landscape analysis and toolbox expansion, (2) biomarker development, and (3) therapeutic testing. Ultimately, these efforts will help us decide the most promising avenue to pursue for treatment whether that be drug repurposing, gene therapy, novel drug discovery, or a combination. Most importantly, we truly value the patient/caregiver voice; we gather information on their unique experiences, include the most impactful symptoms at the forefront of our research efforts, and utilize the Parent Advisory Board’s feedback on our educational initiatives and partnerships.
Landscape analysis and toolbox expansion
Over the past 5 years, efforts have focused on engaging researchers studying CSNK2A1 and related scientific topics and learning more about the biology of OCNDS. To that end, in 2021, the OCNDS Scientific Roundtable was launched bringing together researchers and clinicians to share unpublished data and obtain feedback from colleagues working in related fields. This has stimulated collaborative publications and grant submissions and continues to be a source of novel ideas. Critically, we have ensured that the scientific tools developed for OCNDS research, including disease models, are readily available to interested researchers. A crucial initiative over the coming years is fully characterizing the existing models in our research toolbox. To accomplish this, we have dedicated funds to projects focused on the characterization of three mouse models harboring distinct CSNK2A1 variants found in patients in the Rebholz lab (INSERM, Paris, France) and four patient-derived induced pluripotent stem cell (iPSC) lines in the Huentelman lab (TGen, Phoenix, AZ, USA). The foundation is pursuing multiple research avenues simultaneously and has recently announced the funding of a Drosophila (fly) model to screen a library of FDA-approved compounds in the Chow lab (University of Utah). Furthermore, we are actively enrolling individuals in the Simons Searchlight Natural History Study that collects high-quality, standardized data about individuals with OCNDS over their lifetime. These data will be important to compare how well our models mimic the human experience. Our contact registry has grown to over 200 individuals, which has helped us better understand the OCNDS mutational spectrum and will assist in the future for genotype–phenotype analyses, a basic science study we have highlighted in our roadmap. Additionally, as part of our toolbox and engagement efforts, we stay informed of relevant quality of life resources to share with our community to address current issues with OCNDS as best as possible. While it is important to look ahead using a roadmap for research, we recognize the importance of ongoing support and remain committed to assisting the community as effectively as possible in the interim period.
Biomarker development
We are driven to learn more about OCNDS biology to investigate if an OCNDS biological marker (‘biomarker’) exists. Specifically, a defined feature that can be measured as an indicator that someone has OCNDS and/or a feature that relays whether an individual is responding to specific therapies. To find a biomarker, we have funded the establishment of mouse models that have CSNK2A1 mutations that have been observed in OCNDS patients and we are measuring multiple biological variables including behaviors that are often observed in individuals with autism (e.g. repetitive movements, anxiety, learning, and memory) as well as other features including epileptiform activity, body size, and gastrointestinal phenotypes. Through the SFARI biorepository, we have nine patient-derived iPSC lines. We think of iPSCs as chameleon cells that can transform into different cell types just like they would during early human development. These iPSCs provide a unique opportunity to model human brain development both in a ‘normal’ context and in the presence of OCNDS-causing mutations. As OCNDS is a neurodevelopmental disorder, it is critical that we utilize iPSCs to assess the development of central nervous system cell types to determine when and how ‘normal’ development is disrupted. This is also vital to pursuing therapeutic options in the future as there may be a specific ‘window of opportunity’ for intervention to have the maximum possible effect on symptom reduction and/or prevention in patients.
Therapeutic testing
As previously mentioned, we have awarded a grant to Dr. Chow to screen over 1500 FDA-approved compounds in an OCNDS fly model. We also established our first partnership with a biotechnology company in 2023 – Unravel Biosciences. Unravel is dedicated to identifying therapeutic opportunities based on computational analysis of gene expression profiles. They will utilize their computational platform to identify molecular differences in OCNDS mouse and human samples and compare them to non-OCNDS samples. Unravel will leverage their drug screening platform to identify potential therapeutics predicted to be functional within and across mouse and human models of OCNDS. This work is ongoing in parallel to our mouse and iPSC model characterization. Once we have established mice and/or cells with potential biomarker(s), we can explore testing compounds identified via the fly screen, Unravel’s platform, or other studies. In the future, we plan to fund ‘proof of concept’ studies (i.e., research studies that provide evidence to demonstrate that something is feasible) for gene editing therapeutic approaches.
These key focus areas guide our roadmap that describes our view of the therapeutic development process using our existing toolbox. We have broken the roadmap down into the following categories: disease models, basic science, NH, preclinical research, Phase I/II trials, Phase III trials, and long-term monitoring (Figure 2). We want to emphasize that although our roadmap is displayed as a semi-linear model, many of these steps can take place in parallel. Importantly, NH and long-term monitoring continue to inform categories of disease models, basic science, preclinical research, and human studies. To further summarize, this roadmap is a continuous process with each ‘step’ having the ability to inform another ‘step’.
Natural history
In our roadmap, NH is a longitudinal component and not part of a linear model; while NH informs many parts of disease models, basic science, preclinical research, and clinical endpoints, it also serves as a tool to track key data across all phases of research and stages of a disease. Furthermore, NH will be useful when therapeutic options are available to gather insights into risks, benefits, side effects, and disease comorbidities. Thus, NH is a constant presence in our roadmap spanning all steps. We included foundation surveys under the NH category, which can be a helpful starting point for researchers to decide which projects to pursue. We hope to establish a disease concept model (a framework that describes the lived experience of OCNDS families) to help define relevant outcome measures for future studies. We are also interested in piloting retrospective EEG studies using patient data to assess if any EEG signatures exist. Furthermore, we can compare EEG data to other rare epilepsies to assess potential similarities and combine efforts with other groups when possible. Notably, NH from Ciitizen 29 has been used as the primary data source for a successful investigational new drug (IND) filing with the FDA. 30 Given this success, it may be possible in the future to replace the placebo arm with NH data in clinical trials when small populations lead to challenges enrolling enough patients.
Disease models
Our toolbox expansion has led to OCNDS models across various model systems including mice, patient-derived cells, zebrafish, Xenopus (frog), and fly. Furthermore, we currently have 23 blood samples stored with SFARI. 6 Collectively, our models and NH study form our Research Toolbox (Table 1). A valuable consideration when generating models for rare diseases is what variants to model. We chose the most observed variant (K198R) alongside others that occur at distinct parts of the gene. To visualize the most recently published representation of existing variants, refer to Figure 2 of Unni et al. 22 These samples are readily available for studies, and we have active funded projects focused on model characterization that will guide future research initiatives.
Table 1.
Research toolbox.
| Research tool | Details | Source |
|---|---|---|
| Human dermal fibroblasts | Four lines, female Gene: CSNK2A1 p.Lys198Arg (2) p.Arg47Gly p.Asp156Glu |
Translational Genomics Research Institute Center for Rare Childhood Disorders. Contact: Sampath Rangasamy, PhD, srangasamy@tgen.org |
| Human induced pluripotent stem cells | Nine lines, gene: CSNK2A1
p.Lys198Arg (2) p.Arg47Gly p.Asp156Glu Arg312Trp p.Arg47Gln (2) p.Tyr50Ser CNV deletion 378136-547319 |
Simons Foundation SFARI Base (https://www.sfari.org/resource/ips-cells/) Derived from peripheral blood mononuclear cells |
| Mouse models |
CSNK2A1 K198R CSNK2A1 R312W CSNK2A1 R47G Csnk2a1 Constitutive Knockout |
Jackson Labs (Stock # 067399-JAX) Heike Rebholz, PhD, heike.rebholz@inserm.fr Taconic (Stock #: TF0094) |
| Natural history data | Medical history Medications Sleep habits questionnaire Seizure history Vineland Adaptive Behavior Scales 3rd edition and more |
Simons Searchlight (https://www.simonssearchlight.org/) |
We are committed to working with institutions and researchers that share reagents, biospecimens, cells lines, animal models, and data. In addition to the tools noted in the table, other assets currently in development or storage include various plasmids for injections into zebrafish or Xenopus models as well as a Drosophila model.
Basic science research
This type of study investigates how a disease works at the molecular, cellular, and organism level and is a critical step toward developing a therapeutic approach. Through research into CK2 target proteins, the mechanism of action across CK2 mutations, genotype–phenotype analyses, and OCNDS model characterization, we are hopeful that researchers will identify biomarkers to measure treatment response(s) and discover relevant therapeutic avenues for OCNDS.
Preclinical research
Our preclinical efforts focus on drug repurposing and gene therapy approaches. Ongoing efforts include our partnership with Unravel, a grant to Dr. Chow to test FDA-approved compounds in an OCNDS fly model, and future efforts will include our mouse and iPSC models. Gene editing approaches are very early stage with data from zebrafish studies at TGen to be released in 2024.
Phase I/II/III clinical trials
We currently do not have any OCNDS-specific therapeutic intervention clinical trials ongoing; however, when we do have the opportunity, we will diligently advocate to be a part of the clinical trial design including the protocol and patient-facing materials. We are promoting participation in ongoing research studies investigating aspects of multiple rare disorders that have autism and/or epilepsy and will continue to engage with researchers conducting these types of studies so that OCNDS is considered for inclusion.
Long-term monitoring
Our community is now participating in medical record collection platforms, such as Ciitizen, 29 to gather data directly from electronic health records that may be missed in a formal NH study. Furthermore, we partner with TREND Community 31 to gather secure and anonymous information from our OCNDS private caregiver Facebook group. TREND is a digital health analytics company that specializes in extracting actionable insights from conversations related to rare, chronic, and emerging diseases. For example, TREND can capture sentiments about specific medications or help to discover novel symptoms. One such insight gained as we launched this partnership in October is a suspected underreporting of seizure activity in OCNDS patients. By collecting medical records, insights from TREND, and longitudinal NH data combined with the characterization of patient-derived models, we will gain insights for future clinical phenotyping and contribute to understanding the mechanisms behind the heterogeneity of symptoms observed in patients.
Our integrated roadmap highlights our current plans, and we are excited to see it used to accelerate OCNDS research. Importantly, this roadmap is a ‘snapshot’ in time, and as we learn more, we will revisit and revise our roadmap to ensure that we pursue the most promising projects for the community.
Founder perspective
Like many parents who are also patient advocacy group founders, my daughter Juliet was born affected by a rare disorder, OCNDS. However, at the time of her birth in 2010, OCNDS had not yet been discovered. She was not reaching her milestones, and we searched for 6 years for a diagnosis. In 2016, we received a call from our neurologist that changed our lives forever – she told us that Juliet was the sixth individual in the world to be diagnosed with OCNDS through whole exome sequencing. Just 4 months prior, the first study identifying this brand-new syndrome was published by Dr. Wendy Chung and Dr. Volkan Okur. I looked up OCNDS on the Internet for more information. There was nothing – no support group, no foundation, no website. This was my first lesson in rare disease 101: just because you have a diagnosis, it does not mean you have all the answers. I knew we had to do better for Juliet and our community. We had to create something for individuals to easily understand their diagnosis and empower them to be their own advocates. In addition, we are living in an unprecedented time in science. Diseases once thought to be untreatable are now being treated. After speaking with researchers and academics, it became abundantly clear that OCNDS is treatable.
Dr. Chung told me the cold, hard fact about most rare diseases, which is that patients and their families shouldered the burden of building an army to drive rare disease research. At that time, no one was studying OCNDS. To make a difference, she told me that I needed to build an army. Her instructions were clear for our first year – start a foundation, hold an in-person family conference, start a patient registry, make models (including mice and iPSC cells), fund basic research, and find at least 60 other families. We started the foundation about 18 months later because we wanted to be thoughtful about our approach and hit the ground running. In the organization’s inaugural year, we started to build our army: we held an in-person family meeting, made our first mouse model, funded the first OCNDS biochemistry study, and found many more patients. Since then, we assembled a team of scientists across the globe who worked on CK2 before it was associated with OCNDS, funded basic science, built a robust research toolbox, hosted 10 scientific roundtables with over 25 scientists from across the globe regularly participating, and held 3 scientific conferences. Furthermore, we have awarded almost $1 million in grants to date.
One glaring problem we noticed from the beginning was barriers to participation in everything: in research, in connecting with the community, in diagnosis, in care, and in treatment. Roughly 13% of the world speaks English. We have found over 200 patients in 33 countries, speaking 21 languages. We strive to remove barriers to participation across all areas, but we have limited funding, so we have focused our efforts on removing the language barrier. We created a printable one-page document, translated into 21 languages, containing the most common questions about OCNDS to make it easy for families to share the information with friends, providers, teachers, and doctors. Currently, little is known about OCNDS, so this document serves as a lifeline to families struggling with the daily challenges of OCNDS. The one-pager helps families easily understand the diagnosis and provides recommendations for care. We also partner with Wordly 32 to provide live-caption translation for our family Zoom calls and our webinars so that families can participate in their native languages.
Our successes can be attributed to our collaborative approach. Our approach is supported by our foundation’s four pillars: Board of Directors, SAB, Parent Advisory Board, and our OCNDS Community (Figure 4). This collaboration supports our ability to accelerate the path to treatment and ensures that the patient’s voice is at the center of all our decisions. The prospect of hiring a full-time Science Program Director once seemed far-fetched; however, the need for a visionary leader to steer our research program and hasten the path to treatment became evident in 2022. In April of 2023, Dr. Gabrielle Rushing joined us as our Science Program Director, and in her first year, she has already left an indelible mark, propelling us closer to our goal. In less than 8 months, she has already applied for seven highly competitive grants ranging in awards from $5000 to $1.6 million, some of which were collaborative submissions with other OCNDS researchers. She surveyed the OCNDS landscape, added two members to our SAB, and created the OCNDS research roadmap as described in this publication. We simply did not have the capacity or expertise to do what Dr. Rushing is doing.
Figure 4.
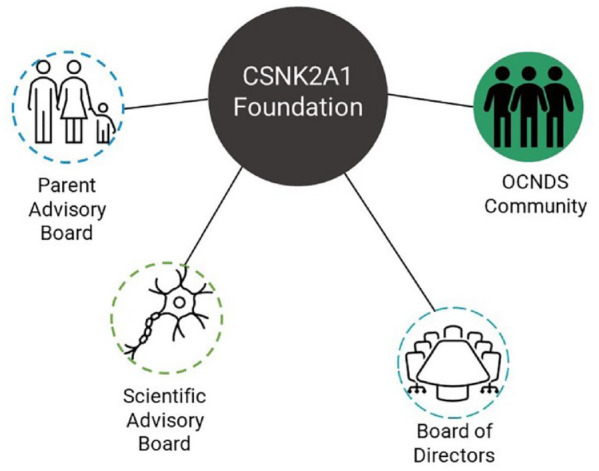
CSNK2A1 Foundation’s four pillars.
Reflecting on 2016 (Figure 5), a time when my only resource was a lone publication detailing the initial five cases of OCNDS, and I had to look up every other word to comprehend its content, we have made significant progress. Today, we have a contact registry with over 200 OCNDS individuals, a comprehensive website featuring a dedicated page summarizing 27 publications focused on OCNDS, our inaugural full-time hire, nearly $1 million in research grants awarded, and a robust research toolbox guiding our new research roadmap. With these developments, we stand at the forefront of discovering innovative treatment options for OCNDS families.
Figure 5.
Timeline of CSNK2A1 Foundation’s major milestones.
Summary
The foundation is committed to generating a comprehensive array of research tools and resources, empowering stakeholders to excel in their endeavors, fostering collaboration, and accelerating our understanding and treatment options for OCNDS. Our goal is to expedite the research process without imposing additional burdens on researchers. By concurrently exploring multiple approaches and models, we aim to shorten the timeline for developing therapeutic solutions for OCNDS. In addition, our commitment extends to investments in attending forward-thinking events, co-writing grant applications with research groups, regularly engaging the OCNDS community, and collaborating with others as much as possible. Embracing the philosophy that ‘If you want to go fast, go alone. If you want to go far, go together,’ prominently featured on our foundation webpage, we emphasize the importance of flexibility and collective efforts. We are firm believers in following the science and will continue to adapt our roadmap as we learn. This will keep the foundation moving as fast as possible – we will listen, we will learn, and we will adapt to ensure the best possible future for OCNDS families.
Acknowledgments
The authors thank the CSNK2A1 Foundation Parent Advisory Board for their thoughtful insights on the research roadmap. The authors thank Ashley Pounders, MSN, FNP-C for reviewing the manuscript.
Footnotes
ORCID iD: Gabrielle V. Rushing  https://orcid.org/0000-0002-6114-883X
https://orcid.org/0000-0002-6114-883X
Contributor Information
Gabrielle V. Rushing, CSNK2A1 Foundation, 1929 Van Ness Avenue, San Francisco, CA 94109, USA.
Jennifer Sills, CSNK2A1 Foundation, San Francisco, CA, USA.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Author contributions: Gabrielle V. Rushing: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Validation; Visualization; Writing – original draft; Writing – review & editing.
Jennifer Sills: Methodology; Project administration; Resources; Supervision; Visualization; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Okur V, Cho MT, Henderson L, et al. De novo mutations in CSNK2A1 are associated with neurodevelopmental abnormalities and dysmorphic features. Hum Genet 2016; 135: 699–705. [DOI] [PubMed] [Google Scholar]
- 2. Castello J, Ragnauth A, Friedman E, et al. CK2 – an emerging target for neurological and psychiatric disorders. Pharmaceuticals 2017; 10: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Okur-Chung Neurodevelopmental Syndrome – GeneReviews® – NCBI Bookshelf, 2022, https://www.ncbi.nlm.nih.gov/books/NBK581083/ (accessed 25 October 2023).
- 4. Belnap N, Price-Smith A, Ramsey K, et al. Inherited CSNK2A1 variants in families with Okur-Chung neurodevelopmental syndrome. Clin Genet 2023; 104: 607–609. [DOI] [PubMed] [Google Scholar]
- 5. Lamb GV, Green RJ, Olorunju S. Tracking epilepsy and autism. Egypt J Neurol Psychiatry Neurosurg 2019; 55: 55. [Google Scholar]
- 6. SFARI Gene – Welcome. SFARI Gene, 2024, https://gene.sfari.org/ (accessed 14 July 2023).
- 7. CSNK2A1. Simons searchlight, https://www.simonssearchlight.org/research/what-we-study/csnk2a1/ (accessed 19 December 2023).
- 8. Tsuchiya Y, Akashi M, Matsuda M, et al. Involvement of the protein kinase CK2 in the regulation of mammalian circadian rhythms. Sci Signal 2009; 2: ra26. [DOI] [PubMed] [Google Scholar]
- 9. Smith EM, Lin J-M, Meissner R-A, et al. Dominant-negative CK2α induces potent effects on Circadian Rhythmicity. PLoS Genet 2008; 4: e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cohen S, Conduit R, Lockley SW, et al. The relationship between sleep and behavior in autism spectrum disorder (ASD): a review. J Neurodev Disord 2014; 6: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Distefano G, Calderoni S, Apicella F, et al. Impact of sleep disorders on behavioral issues in preschoolers with autism spectrum disorder. Front Psychiatry 2023; 14: 1181466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Veatch OJ, Sutcliffe JS, Warren ZE, et al. Shorter sleep duration is associated with social impairment and comorbidities in ASD. Autism Res Off J Int Soc Autism Res 2017; 10: 1221–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Niefind K, Guerra B, Ermakowa I, et al. Crystal structure of human protein kinase CK2: insights into basic properties of the CK2 holoenzyme. EMBO J 2001; 20: 5320–5331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Poirier K, Hubert L, Viot G, et al. CSNK2B splice site mutations in patients cause intellectual disability with or without myoclonic epilepsy. Hum Mutat 2017; 38: 932–941. [DOI] [PubMed] [Google Scholar]
- 15. Lou DY, Dominguez I, Toselli P, et al. The alpha catalytic subunit of protein kinase CK2 is required for mouse embryonic development. Mol Cell Biol 2008; 28: 131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Seldin DC, Lou DY, Toselli P, et al. Gene targeting of CK2 catalytic subunits. Mol Cell Biochem 2008; 316: 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Buchou T, Vernet M, Blond O, et al. Disruption of the regulatory beta subunit of protein kinase CK2 in mice leads to a cell-autonomous defect and early embryonic lethality. Mol Cell Biol 2003; 23: 908–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ceglia I, Flajolet M, Rebholz H. Predominance of CK2α over CK2α’ in the mammalian brain. Mol Cell Biochem 2011; 356: 169–175. [DOI] [PubMed] [Google Scholar]
- 19. Caefer DM, Phan NQ, Liddle JC, et al. The Okur-Chung Neurodevelopmental Syndrome Mutation CK2K198R leads to a rewiring of kinase specificity. Front Mol Biosci 2022; 9: 850661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dominguez I, Cruz-Gamero JM, Corasolla V, et al. Okur-Chung neurodevelopmental syndrome-linked CK2α variants have reduced kinase activity. Hum Genet 2021; 140: 1077–1096. [DOI] [PubMed] [Google Scholar]
- 21. CSNK2A1 Foundation. Understanding Okur-Chung neurodevelopmental syndrome, https://www.csnk2a1foundation.org/ (accessed 18 December 2023).
- 22. Unni P, Friend J, Weinberg J, et al. Predictive functional, statistical and structural analysis of CSNK2A1 and CSNK2B variants linked to neurodevelopmental diseases. Front Mol Biosci 2022; 9: 851547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. GRIN Portal. An Interactive Website for families, clinicians, and researchers dedicated to comprehending GRIN-related disorders, 2024, https://grin-portal.broadinstitute.org/ (accessed 5 March 2024).
- 24. CFERV. GRIN2B Foundation, 2019, http://grin2b.com/cferv/ (accessed 5 March 2024).
- 25. Myers SJ, Yuan H, Perszyk RE, et al. Classification of missense variants in the N-methyl-d-aspartate receptor GRIN gene family as gain- or loss-of-function. Hum Mol Genet 2023; 32: 2857–2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. ICD Code Roadmap. Everylife foundation for rare diseases, 2021, https://everylifefoundation.org/icd-code-roadmap/ (accessed 18 December 2023).
- 27. Orphan Disease Center. https://www.orphandiseasecenter.med.upenn.edu/ (accessed 18 December 2023).
- 28. Rushing GV, Chung W. Okur-Chung Neurodevelopmental Syndrome – symptoms, causes, treatment | NORD, 2023, https://rarediseases.org/rare-diseases/okur-chung-neurodevelopmental-syndrome/ (accessed 15 December 2023).
- 29. Ciitizen. When you control your health data, you control your options. Ciitizen, https://www.ciitizen.com/ (accessed 19 December 2023).
- 30. Invitae Corporation. Invitae’s real-world citizen data utilized in Praxis Precision Medicines’ PRAX-222 IND filing, 2022, https://www.prnewswire.com/news-releases/invitaes-real-world-ciitizen-data-utilized-in-praxis-precision-medicines-prax-222-ind-filing-301627677.html (accessed 15 December 2023).
- 31. TREND Community | Turning Anecdotes Into Evidence™. https://trend.community/ (accessed 19 December 2023).
- 32. #1 AI Translation Platform | Meetings & Events | Wordly.ai. https://www.wordly.ai/ (accessed 19 December 2023).






