The World Health Organization (WHO) warned this week that the level of resistance to drugs used to treat common infectious diseases is reaching crisis point.
If governments around the world do not make greater efforts to control disease and stem the spread of resistance there will be a return to the preantibiotic era and entire populations could be wiped our by “superbugs” for which no effective treatment exists, it said.
“We currently have effective medicines to cure almost every major infectious disease,” said Dr Gro Harlem Brundtland, director general of the WHO. “But we risk losing these valuable drugs—and our opportunity to eventually control many infectious diseases—because of increasing antimicrobial resistance.”
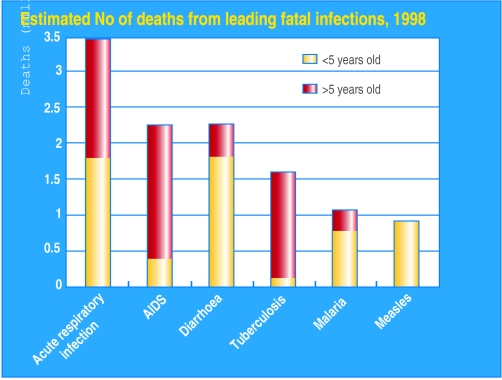
The WHO sounded the warning in its annual report on infectious diseases, Overcoming Antimicrobial Resistance. The report describes how all major infectious diseases—including tuberculosis, malaria, AIDS, pneumonia, and diarrhoeal diseases—are slowly becoming resistant to existing drugs.
In Estonia, Latvia, and parts of Russia and China more than 10% of patients with tuberculosis are infected with strains that are resistant to the two most powerful medicines used to treat the disease. In Thailand three of the most common antimalarial drugs are now useless because of resistance.
An estimated 30% of patients being treated for hepatitis B with the drug lamivudine show resistance to treatment after a year's treatment. The number of patients showing resistance to zidovudine and other drugs used to tackle HIV is growing.
“Unless we take action now we risk running out of drugs,” said Dr Rosemund Williams, coordinator of the WHO's anti-infective drug resistance surveillance and containment division and editor of the report.
“It is not just enough to get it right at home. We need to look at the global situation. Partnership is critical as many countries will not be able to tackle this problem on their own, but they will need help from richer countries.”
The spread of resistance is being fuelled by both underuse and overuse of drugs. In developing countries failure to control infections by not completing the full course of drugs allows the most resistant microbes to survive, multiply, and spread to others.
Conversely, in wealthier countries the overprescription of antibiotics to meet patients' demands and overuse of antimicrobials in food production is adding to the problem. Better surveillance, education of the public and the medical profession, and rapid diagnosis so that the first drug that is used destroys the microbe are all needed to prevent resistance, said Dr Williams. In addition, drug companies may need to be given incentives to encourage them to invest in developing new drugs.
• English health minister John Denham has granted inspectors new powers of “naming and shaming” hospitals that have above average levels of infection in a bid to reduce the incidence of hospital acquired infections.
The UK government's Antimicrobial Resistance Strategy is available at www.doh.gov.uk/arbstrat.htm. WHO information is available at www.who.int.
Figure.
Superbugs could make existing antibiotics useless by 2010