A healthy dentition and mouth is important to both quality of life and nutrition, and oral disease may affect systemic health, as discussed in later articles in this series.
Development of the dentition
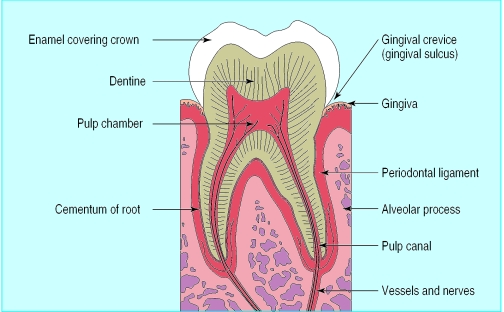
Teeth form mainly from neuroectoderm and comprise a crown of insensitive enamel surrounding sensitive dentine and a root that has no enamel covering. Teeth contain a vital pulp (nerve) and are supported by the periodontal ligament, through which roots are attached into sockets in the alveolar bone of the jaws (maxilla and mandible). The fibres of the periodontal ligament attach through cementum to the dentine surface. The alveolus is covered by the gingivae, or gums, which, when healthy, are pink, stippled, and tightly bound down and form a close fitting cuff with a small sulcus (gingival crevice) round the neck (cervical margin) of each tooth.
The primary (deciduous or milk) dentition comprises four incisors, two canines, and four molars in each jaw (total of 20 teeth). The normal permanent (adult) dentition comprises four incisors, two canines, four premolars, and six molars in each jaw (32 teeth).
Average times of tooth eruption
| Upper teeth | Lower teeth | |
| Primary teeth | ||
| Central incisors | 8-13 months | 6-10 months |
| Lateral incisors | 8-13 months | 10-16 months |
| Canines (cuspids) | 16-23 months | 16-23 months |
| First molars | 13-19 months | 13-19 months |
| Second molars | 25-33 months | 23-31 months |
| Permanent teeth | ||
| Central incisors | 7-8 years | 6-7 years |
| Lateral incisors | 8-9 years | 7-8 years |
| Canines (cuspids) | 11-12 years | 9-10 years |
| First premolars (bicuspids) | 10-11 years | 10-12 years |
| Second premolars (bicuspids) | 10-12 years | 11-12 years |
| First molars | 6-7 years | 6-7 years |
| Second molars | 12-13 years | 11-13 years |
| Third molars | 17-21 years | 17-21 years |
Tooth development begins in the fetus, at about 28 days in utero. Indeed, all the primary and some of the permanent dentition start to develop in the fetus. Mineralisation of the primary dentition begins at about 14 weeks in utero, and all primary teeth are mineralising by birth. The permanent incisors and first molars begin to mineralise at or close to the time of birth, while the other permanent teeth start to mineralise later. Tooth eruption occurs after formation and mineralisation of the crown are largely complete but before the roots are fully formed.
Neonatal teeth are uncommon and may be loose. They may damage the mother's nipple during suckling, in which case they might need to be removed.
• Tooth development begins in utero• Root formation finalises after eruption• Full primary dentition has 20 teeth• Full permanent dentition has 32 teeth
Teething
Eruption of primary teeth may be preceded by a bluish gingival swelling, usually a result of a transient haematoma and, rarely, an eruption cyst, which usually ruptures spontaneously. Tooth eruption may be associated with irritability, disturbed sleep, cheek flushing, drooling, and sometimes a small rise in temperature or a circumoral rash, but it does not cause diarrhoea or bronchitis (although these may occur coincidentally).
Delays in tooth eruption
A delay in eruption of up to 12 months may be of little or no importance in an otherwise healthy child. Localised delays often result from local factors such as a tooth in the path of eruption, insufficient space in the dental arch, or dental infection. Ectopic positioning and impaction most often affect the third molars, second premolars, and canines, possibly because these are the last teeth to erupt.
Causes of delayed tooth eruption
| Local | Uncommon or rare systemic causes |
| • Impacted teeth | • Down's syndrome |
| Iatrogenic | • Cleidocranial dysplasia |
| • Cytotoxic therapy | • Congenital hypopituitarism |
| • Radiotherapy | • Congenital hypothyroidism |
| • Gaucher's disease | |
| • Osteopetrosis | |
More generalised failure of eruption is rare but may be associated with a variety of systemic causes.
• Teething may cause irritability, drooling, and a small rise in body temperature• Failed eruption of single teeth is often caused by impaction
Early loss of teeth
Early tooth loss is usually because of extraction as a result of dental caries or, in adults, periodontal disease. Teeth, particularly incisors, may also be lost through trauma, such as from sports, assaults, or other injuries.
Main causes of early loss of teeth
Local causes
Caries • Periodontal disease • Trauma
| Systemic causes | Main systemic features |
| Genetic defects | |
| Down's syndrome | Learning disability, short stature |
| Papillon-Lefèvre syndrome | Palmar-plantar hyperkeratosis |
| Juvenile periodontitis and related disorders | Sometimes neutrophil defects |
| Ehlers-Danlos syndrome type VIII | Hypermobility |
| Chédiak-Higashi syndrome | Recurrent infections |
| Eosinophilic granuloma | Bone lesions |
| Immune defects | |
| Neutropenia | Recurrent infections |
| Neutrophil defects | Recurrent infections |
| Monocyte defects | Recurrent infections |
| Interleukin 1 abnormalities | Recurrent infections |
| HIV infection and AIDS | Recurrent infections |
| Enzyme defects | |
| Acatalasia (absent catalase) | Recurrent infections |
| Hypophosphatasia (low alkaline phosphatase) | Recurrent infections |
Unexplained early tooth loss in children or adults may be a feature of Down's syndrome, diabetes, immune defects, or non-accidental injury, or of rare conditions such as eosinophilic granuloma, hypophosphatasia, or Papillon-Lefèvre syndrome (palmoplantar hyperkeratosis).
• Most tooth loss is due to caries, periodontal disease, or trauma• Early tooth loss may have a systemic cause
Variations in tooth number
Teeth missing from the normal series may have failed to develop (hypodontia) or to erupt or have been lost prematurely.
Hypodontia is not uncommon and is probably of genetic origin. The teeth most often missing are the third molars, second premolars, and maxillary lateral incisors, and other teeth may be reduced in size. Several teeth may be absent in disorders such as Down's syndrome and ectodermal dysplasia.
Mixed dentition—It is not uncommon to see what seem to be two rows of teeth in the lower incisor region, when permanent teeth erupt before the primary incisors have exfoliated. This is particularly likely when there is inadequate space to accommodate the larger permanent teeth. The situation usually resolves as primary incisors are lost and the mandible grows.
Supplemental teeth—Extra teeth are uncommon. Of unknown cause, they are most often seen in the regions of the maxillary lateral incisors, premolars, and third molars. Additional teeth of abnormal form (supernumerary teeth) are also rare. They are usually small and conical in shape and are seen particularly in the maxillary midline, where they may remain unerupted and may cause a permanent incisor to impact. Additional teeth often occur alone in otherwise healthy individuals but occasionally occur in association with rare disorders such as cleidocranial dysplasia and Gardner's syndrome.
• Missing teeth may be due to failed eruption, tooth loss, or hypodontia• Hypodontia is genetic and is seen in Down's syndrome and ectodermal dysplasia• Supplemental or supernumerary teeth are genetic and occasionally occur with systemic disorders
Tooth size, shape, structure, and colour
A variety of local and generalised factors may act during tooth formation or mineralisation. Although tooth development in utero is generally well protected, it may be affected by maternal disease and intrauterine infection and by systemic disturbance during early life. Intrauterine infections that may affect tooth structure include rubella and cytomegalovirus. The classic hutchinsonian incisors and Moon's (or mulberry) molars of congenital syphilis are extremely uncommon in developed countries.
Between birth and 6 years of age, the permanent teeth, particularly those of cosmetic importance, may be damaged. Upper permanent incisors may show defects as a consequence of trauma to the primary predecessor. Local infection or trauma may cause a defect in a single tooth or group of teeth. Malformed lower premolars secondary to periapical infection of their primary predecessors are not uncommon and are termed Turner's teeth. More generalised defects may be seen in a range of systemic disorders (prematurity, infections, jaundice, malabsorption, and cytotoxic therapy) during tooth formation and mineralisation, the defect relating to the timing, severity, and duration of the disorder.
Teeth, especially the third molars, may vary in size, form, and structure because of genetic factors. Microdontia (teeth smaller than usual) is largely of genetic origin and usually affects the lateral incisors, which are conical or peg shaped. Teeth that are larger than normal (megadont) are uncommon. Double teeth may be seen occasionally. These seem to be the result of fusion of two teeth and occur most often in the primary dentition, when they are likely to be followed by extra tooth elements in the succeeding permanent dentition.
Causes of tooth discoloration
Extrinsic discolorations (typically brown or black)
Poor oral hygiene
Smoking
Food and drink (such as tea, coffee, red wine)
Drugs (such as iron, chlorhexidine, antimicrobials)
Chewing betel
Intrinsic discolorations
Localised
Trauma (yellow to brown)
Caries (white, brown, or black)
Restorative materials (such as black of amalgam)
Internal resorption (pink spot)
Generalised
Tetracyclines (brown)
Excessive fluoride (white or brown)
Rare causes Amelogenesis imperfecta (brown) Dentinogenesis imperfecta (brown or purple) Kernicterus or biliary atresia (green) Porphyria (red)
Superficial tooth discoloration is usually caused by poor oral hygiene or habits such as smoking, consuming certain foods and beverages (such as tea), or taking drugs such as iron, chlorhexidine, or long term oral antimicrobials. In some cultures chewing betel causes staining. Discoloration of a single tooth is usually because the tooth is non-vital, heavily filled, or carious.
Intrinsic staining of a brown or grey colour may be caused by tetracyclines given to pregnant or lactating women or to children under the age of 8 years. Excessive fluoride ingestion during early life may also result in enamel opacities, but, except in those parts of the world where water supplies contain very high levels of fluoride, these are usually extremely mild.
Enamel and dentine defects of genetic origin are rare but are occasionally severe and may take a variety of forms and vary in their inheritance. They can occur in isolation—as amelogenesis imperfecta (defective enamel) or dentinogenesis imperfecta (defective dentine)—or as part of a disorder such as epidermolysis bullosa dystrophica or osteogenesis imperfecta. In some genetic defects of dentine, for example, newly erupted teeth may seem brownish and translucent, an appearance seen in some patients with osteogenesis imperfecta.
• Developing teeth can be damaged by infection, jaundice, metabolic disorders, drugs, and irradiation• Tetracyclines given to pregnant or lactating mothers, or to children, can discolour teeth• Inherited disorders of enamel or dentine may cause malformation or discoloration• Most tooth discoloration is due to poor oral hygiene, diet, or habits
Anatomical variants
Patients sometimes become concerned after noticing various anatomical variants in the mouth.
Tori and exostoses are bony lumps that appear during tooth development and are especially common in Mongoloid and Negroid races. Torus mandibularis consists of bilateral, asymptomatic, benign bony lumps lingual to the lower premolars. Also common is torus palatinus, a slow growing, asymptomatic, benign bony lump in the midline of the palate. These lumps are usually left alone but are occasionally excised or reduced if they cause severe difficulties with dentures.
Sebaceous glands may be seen as creamy-yellow dots (Fordyce spots) along the border between the lip vermilion and the oral mucosa. Probably 50-80% of the population have them, but they are not usually clinically evident until after the age of 3 years, and they increase during puberty and then again in later adult life. They are totally benign, although occasional patients or physicians become concerned about them or misdiagnose them as, for example, thrush or lichen planus. No treatment is indicated other than reassurance.
Foliate papillae—The size and shape of the foliate papillae on the posterolateral margins of the tongue are variable. These papillae occasionally swell if irritated mechanically or if there is an upper respiratory infection. Located at a site with a high predilection for lingual cancer, they may give rise to anxiety about cancer.
Further reading
Scully C, Flint S, Porter SR. Oral diseases. London: Martin Dunitz, 1996
Scully C, Welbury RA. Colour atlas of oral diseases in children and adolescents. London: Mosby Wolfe, 1994
Figure.
Diagram of a tooth and supporting structures
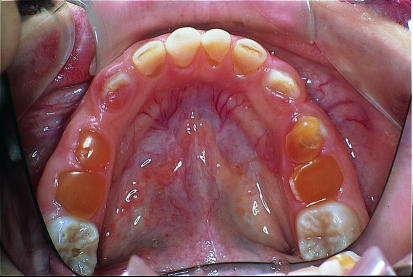
Figure.
Healthy dentition, increasingly seen as caries declines
Figure.
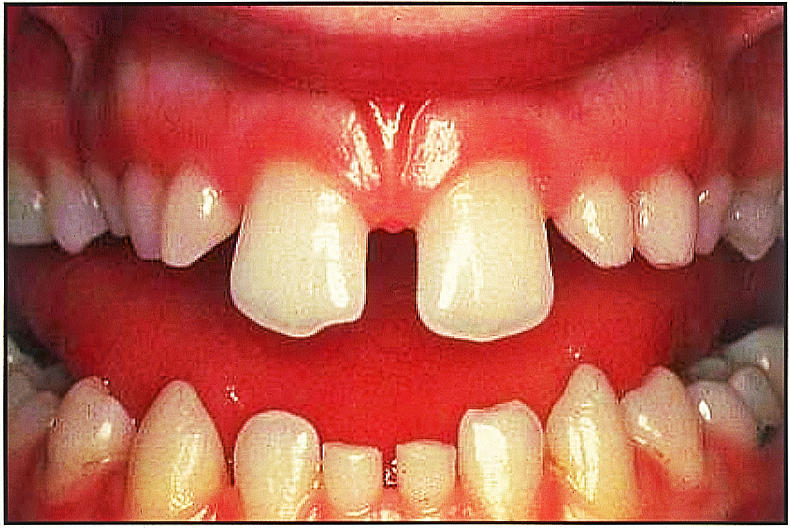
Hypodontia with many missing permanent teeth, including upper lateral incisors and lower central incisors. This appearance may be seen in ectodermal dysplasia
Figure.
Supernumerary teeth erupting palatal to upper central incisors. Such teeth often remain unerupted and may impede eruption of permanent incisors
Figure.

Dilacerated upper central incisor resulting from injury to primary predecessor during permanent tooth development. Severely malformed teeth such as this may require removal, but less severely affected teeth may be treated conservatively
Figure.
Microdont upper left lateral incisor. The tooth is small in size and conical in form
Figure.
Characteristic appearance of teeth of patient with osteogenesis imperfecta who also shows dentinogenesis imperfecta
Figure.
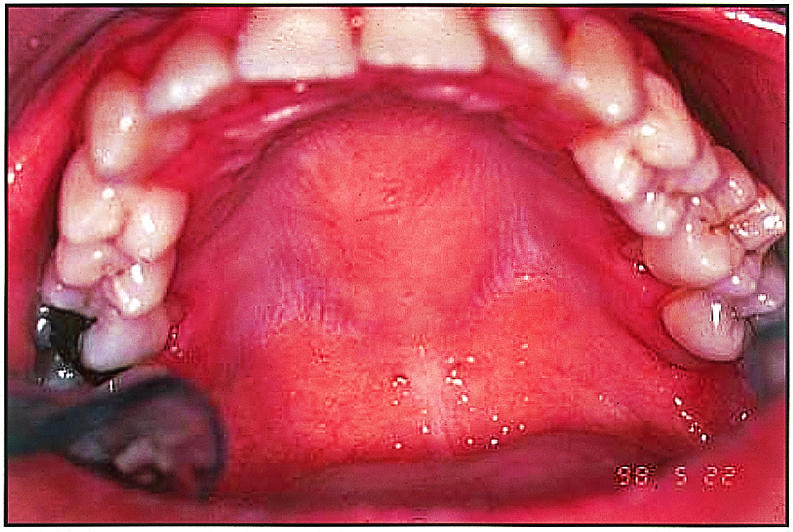
Torus palatinus, with large central torus on palate
Figure.
Fordyce's spots—sebaceous glands close to vermillion border between lip and buccal mucosa
Acknowledgments
Crispian Scully is grateful for the advice of Rosemary Toy, general practitioner, Rickmansworth, Hertfordshire.
Footnotes
Ruth Holt is senior lecturer, Graham Roberts is professor of paediatric dentistry, and Crispian Scully is dean at the Eastman Dental Institute for Oral Health Care Sciences, University College London, University of London (www.eastman.ucl.ac.uk).
The ABC of oral health is edited by Crispian Scully and will be published as a book in autumn 2000.